Social Support, but Not Perceived Food Environment, Is Associated with Diet Quality in French-Speaking Canadians from the PREDISE Study
Abstract
1. Introduction
2. Materials and Methods
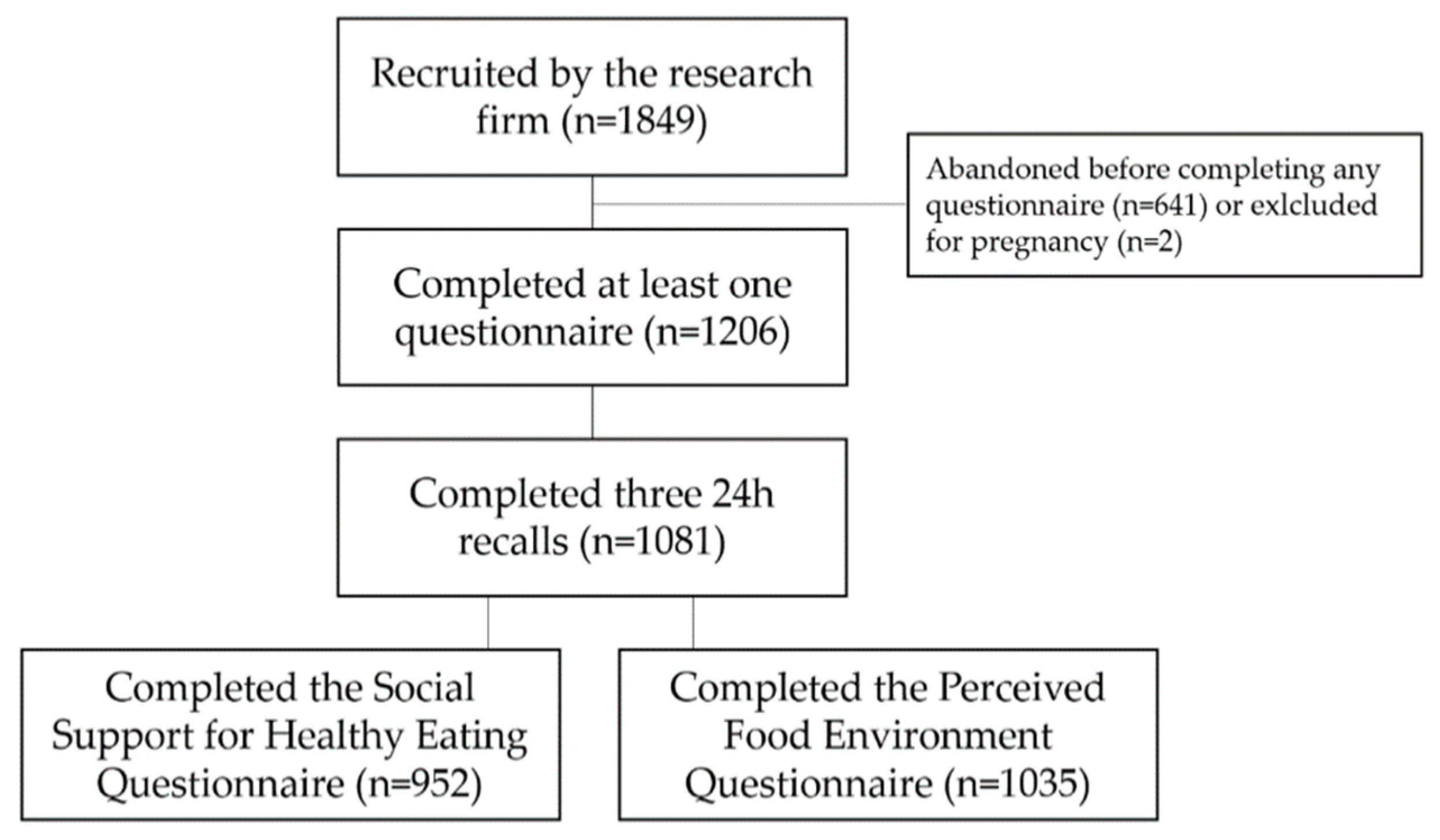
2.1. Participants and Procedures
2.2. Measures
2.3. Ethics
2.4. Statistical Analyses
3. Results
3.1. Objective 1: Social Support for Healthy Eating
3.2. Objective 2: Perceived Food Environment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- McLeroy, K.R.; Bibeau, D.; Steckler, A.; Glanz, K. An ecological perspective on health promotion programs. Health Educ. Quart. 1988, 15, 351–377. [Google Scholar] [CrossRef] [PubMed]
- Rothschild, M. Carrots, sticks, and promises: A conceptual framework for the management of public health and social issue behaviors. J. Mark. 1999, 63, 24–37. [Google Scholar] [CrossRef]
- Brug, J. Determinants of healthy eating: Motivation, abilities and environmental opportunities. Fam. Pract. 2008, 25 (Suppl. 1), i50–i55. [Google Scholar] [CrossRef] [PubMed]
- Kamphuis, C.B.; Giskes, K.; de Bruijn, G.J.; Wendel-Vos, W.; Brug, J.; van Lenthe, F.J. Environmental determinants of fruit and vegetable consumption among adults: A systematic review. Brit. J. Nutr. 2006, 96, 620–635. [Google Scholar] [PubMed]
- Giskes, K.; Kamphuis, C.B.; van Lenthe, F.J.; Kremers, S.; Droomers, M.; Brug, J. A systematic review of associations between environmental factors, energy and fat intakes among adults: Is there evidence for environments that encourage obesogenic dietary intakes? Public Health Nutr. 2007, 10, 1005–1017. [Google Scholar] [CrossRef] [PubMed]
- Giskes, K.; van Lenthe, F.; Avendano-Pabon, M.; Brug, J. A systematic review of environmental factors and obesogenic dietary intakes among adults: Are we getting closer to understanding obesogenic environments? Obes. Rev. 2011, 12, e95–e106. [Google Scholar] [CrossRef] [PubMed]
- Caspi, C.E.; Sorensen, G.; Subramanian, S.V.; Kawachi, I. The local food environment and diet: A systematic review. Health Place 2012, 18, 1172–1187. [Google Scholar] [CrossRef]
- Marifran, M.; Gibb, H.J. Linking health communication with social support. In Health as Communication Nexus: A Service-Learning Approach; Dubuque, I., Ed.; Kendall Hunt Publishing Company: Dubuque, IA, USA, 2011. [Google Scholar]
- Sahyoun, N.R.; Zhang, X.L. Dietary quality and social contact among a nationally representative sample of the older adult population in the united states. J. Nutr. Health Aging 2005, 9, 177–183. [Google Scholar]
- Locher, J.L.; Ritchie, C.S.; Roth, D.L.; Baker, P.S.; Bodner, E.V.; Allman, R.M. Social isolation, support, and capital and nutritional risk in an older sample: Ethnic and gender differences. Soc. Sci. Med. 2005, 60, 747–761. [Google Scholar] [CrossRef]
- Conklin, A.I.; Forouhi, N.G.; Surtees, P.; Khaw, K.T.; Wareham, N.J.; Monsivais, P. Social relationships and healthful dietary behaviour: Evidence from over-50s in the epic cohort, UK. Soc. Sci. Med. 2014, 100, 167–175. [Google Scholar] [CrossRef]
- De Bourdeaudhuij, I.; te Velde, S.; Brug, J.; Due, P.; Wind, M.; Sandvik, C.; Maes, L.; Wolf, A.; Perez Rodrigo, C.; Yngve, A.; et al. Personal, social and environmental predictors of daily fruit and vegetable intake in 11-year-old children in nine european countries. Eur. J. Clin. Nutr. 2008, 62, 834–841. [Google Scholar] [CrossRef] [PubMed]
- Draper, C.E.; Grobler, L.; Micklesfield, L.K.; Norris, S.A. Impact of social norms and social support on diet, physical activity and sedentary behaviour of adolescents: A scoping review. Child Care Health Dev. 2015, 41, 654–667. [Google Scholar] [CrossRef] [PubMed]
- Uchino, B.N. Understanding the links between social support and physical health: A life-span perspective with emphasis on the separability of perceived and received support. Perspect. Psychol. Sci. 2009, 4, 236–255. [Google Scholar] [CrossRef] [PubMed]
- Chair, S.Y.; Wong, K.B.; Tang, J.Y.; Wang, Q.; Cheng, H.Y. Social support as a predictor of diet and exercise self-efficacy in patients with coronary artery disease. Contemp. Nurse 2015, 51, 188–199. [Google Scholar] [CrossRef] [PubMed]
- Powers, T.A.; Koestner, R.; Gorin, A.A. Autonomy support from family and friends and weight loss in college women. Fam. Syst. Health 2008, 26, 404–416. [Google Scholar] [CrossRef]
- Greaves, C.J.; Sheppard, K.E.; Abraham, C.; Hardeman, W.; Roden, M.; Evans, P.H.; Schwarz, P. Systematic review of reviews of intervention components associated with increased effectiveness in dietary and physical activity interventions. BMC Public Health 2011, 11, 119. [Google Scholar] [CrossRef]
- Pieroth, R.; Rigassio Radler, D.; Guenther, P.M.; Brewster, P.J.; Marcus, A. The relationship between social support and diet quality in middle-aged and older adults in the united states. J. Acad. Nutr. Diet. 2017, 117, 1272–1278. [Google Scholar] [CrossRef]
- Ferranti, E.P.; Dunbar, S.B.; Higgins, M.; Dai, J.; Ziegler, T.R.; Frediani, J.K.; Reilly, C.; Brigham, K.L. Psychosocial factors associated with diet quality in a working adult population. Res. Nurs. Health 2013, 36, 242–256. [Google Scholar] [CrossRef]
- Lawrence, W.; Schlotz, W.; Crozier, S.; Skinner, T.C.; Haslam, C.; Robinson, S.; Inskip, H.; Cooper, C.; Barker, M. Specific psychological variables predict quality of diet in women of lower, but not higher, educational attainment. Appetite 2011, 56, 46–52. [Google Scholar] [CrossRef]
- Cheadle, A.; Psaty, B.M.; Curry, S.; Wagner, E.; Diehr, P.; Koepsell, T.; Kristal, A. Community-level comparisons between the grocery store environment and individual dietary practices. Prev. Med. 1991, 20, 250–261. [Google Scholar] [CrossRef]
- Bodor, J.N.; Rose, D.; Farley, T.A.; Swalm, C.; Scott, S.K. Neighbourhood fruit and vegetable availability and consumption: The role of small food stores in an urban environment. Public Health Nutr. 2008, 11, 413–420. [Google Scholar] [CrossRef] [PubMed]
- Zenk, S.N.; Lachance, L.L.; Schulz, A.J.; Mentz, G.B.; Kannan, S.; Ridella, W. Neighborhood retail food environment and fruit and vegetable intake in a multiethnic urban population. Am. J. Health Promot. 2009, 23, 255–264. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, A.; Cook, A.J.; Jiao, J.; Seguin, R.A.; Vernez Moudon, A.; Hurvitz, P.M.; Drewnowski, A. Access to supermarkets and fruit and vegetable consumption. Am. J. Public Health 2014, 104, 917–923. [Google Scholar] [CrossRef] [PubMed]
- Morland, K.; Wing, S.; Roux, A.D. The contextual effect of the local food environment on residents’ diets: The atherosclerosis risk in communities study. Am. J. Public Health 2002, 92, 1761–1768. [Google Scholar] [CrossRef] [PubMed]
- Izumi, B.T.; Zenk, S.N.; Schulz, A.J.; Mentz, G.B.; Wilson, C. Associations between neighborhood availability and individual consumption of dark-green and orange vegetables among ethnically diverse adults in detroit. J. Am. Diet. Assoc. 2011, 111, 274–279. [Google Scholar] [CrossRef] [PubMed]
- Thornton, L.E.; Bentley, R.J.; Kavanagh, A.M. Fast food purchasing and access to fast food restaurants: A multilevel analysis of viclanes. Int. J. Behav. Nutr. Phys. Act. 2009, 6, 28. [Google Scholar] [CrossRef] [PubMed]
- Hillier, A.; Cannuscio, C.C.; Karpyn, A.; McLaughlin, J.; Chilton, M.; Glanz, K. How far do low-income parents travel to shop for food? Empirical evidence from two urban neighborhoods. Urban Geogr. 2011, 32, 712–729. [Google Scholar] [CrossRef]
- Dibsdall, L.A.; Lambert, N.; Bobbin, R.F.; Frewer, L.J. Low-income consumers’ attitudes and behaviour towards access, availability and motivation to eat fruit and vegetables. Public Health Nutr. 2003, 6, 159–168. [Google Scholar] [CrossRef]
- Williams, L.; Ball, K.; Crawford, D. Why do some socioeconomically disadvantaged women eat better than others? An investigation of the personal, social and environmental correlates of fruit and vegetable consumption. Appetite 2010, 55, 441–446. [Google Scholar] [CrossRef]
- Lucan, S.C.; Mitra, N. Perceptions of the food environment are associated with fast-food (not fruit-and-vegetable) consumption: Findings from multi-level models. Int. J. Public Health 2012, 57, 599–608. [Google Scholar] [CrossRef]
- Mujahid, M.S.; Diez Roux, A.V.; Morenoff, J.D.; Raghunathan, T. Assessing the measurement properties of neighborhood scales: From psychometrics to ecometrics. Am. J. Epidemiol. 2007, 165, 858–867. [Google Scholar] [CrossRef] [PubMed]
- Sharkey, J.R.; Johnson, C.M.; Dean, W.R. Food access and perceptions of the community and household food environment as correlates of fruit and vegetable intake among rural seniors. BMC Geriatr. 2010, 10, 32. [Google Scholar] [CrossRef] [PubMed]
- Gustafson, A.A.; Sharkey, J.; Samuel-Hodge, C.D.; Jones-Smith, J.; Folds, M.C.; Cai, J.; Ammerman, A.S. Perceived and objective measures of the food store environment and the association with weight and diet among low-income women in north carolina. Public Health Nutr. 2011, 14, 1032–1038. [Google Scholar] [CrossRef] [PubMed]
- Carbonneau, E.; Bradette-Laplante, M.; Lamarche, B.; Provencher, V.; Begin, C.; Robitaille, J.; Desroches, S.; Vohl, M.C.; Corneau, L.; Lemieux, S. Social support for healthy eating: Development and validation of a questionnaire for the french-canadian population. Public Health Nutr. 2018, 21, 2360–2366. [Google Scholar] [CrossRef] [PubMed]
- Carbonneau, E.; Robitaille, J.; Lamarche, B.; Corneau, L.; Lemieux, S. Development and validation of the perceived food environment questionnaire in a French-Canadian population. Public Health Nutr. 2017, 20, 1914–1920. [Google Scholar] [CrossRef]
- Lafrenière, J.; Lamarche, B.; Laramée, C.; Robitaille, J.; Lemieux, S. Relative validity of a web-based, self-administered, 24-h dietary recall to evaluate adherence to Canadian dietary guidelines. Nutrition 2018, 57, 252–256. [Google Scholar] [CrossRef]
- Jacques, S.; Lemieux, S.; Lamarche, B.; Laramee, C.; Corneau, L.; Lapointe, A.; Tessier-Grenier, M.; Robitaille, J. Development of a web-based 24-h dietary recall for a French-Canadian population. Nutrients 2016, 8, 724. [Google Scholar] [CrossRef]
- Carbonneau, E.; Lamarche, B.; Lafreniere, J.; Robitaille, J.; Provencher, V.; Desroches, S.; Corneau, L.; Lemieux, S. Are French Canadians able to accurately self-rate the quality of their diet? Insights from the PREDISE study. Appl. Physiol. Nutr. Metab. 2018, 44, 293–300. [Google Scholar] [CrossRef]
- Lafrenière, J.; Lamarche, B.; Laramée, C.; Robitaille, J.; Lemieux, S. Validation of a newly automated web-based 24-hour dietary recall using fully controlled feeding studies. BMC Nutr. 2017, 3, 34. [Google Scholar] [CrossRef]
- Lafreniere, J.; Laramee, C.; Robitaille, J.; Lamarche, B.; Lemieux, S. Assessing the relative validity of a new, web-based, self-administered 24 h dietary recall in a French-Canadian population. Public Health Nutr. 2018, 21, 2744–2752. [Google Scholar] [CrossRef]
- Garriguet, D. Diet Quality in Canada; Statistics Canada: Ottawa, ON, Canada, 2009. [Google Scholar]
- Health Canada. Eating Well with Canada’s Food Guide. Available online: https://www.canada.ca/en/health-canada/services/canada-food-guide/about/history-food-guide/eating-well-with-canada-food-guide-2007.html (accessed on 10 September 2018).
- Institut de la Statistique du Québec. Seuils du Faible Revenu, MFR-Seuils Avant Impôt, Selon la Taille du Ménage, Québec, 2012–2015. Available online: http://www.stat.gouv.qc.ca/statistiques/conditions-vie-societe/revenu/faible-revenu/seuilsmfr_qcavi_.htm (accessed on 24 July 2018).
- Bradette-Laplante, M.; Carbonneau, E.; Provencher, V.; Begin, C.; Robitaille, J.; Desroches, S.; Vohl, M.C.; Corneau, L.; Lemieux, S. Development and validation of a nutrition knowledge questionnaire for a Canadian population. Public Health Nutr. 2017, 20, 1184–1192. [Google Scholar] [CrossRef] [PubMed]
- Brassard, D.; Laramee, C.; Corneau, L.; Begin, C.; Bélanger, M.; Couillard, C.; Desroches, S.; Houle, J.; Langlois, M.F.; Provencher, V.; et al. Poor adherence to dietary guidelines among French-speaking adults in the province of Quebec, Canada—The PREDISE study. Can. J. Cardiol. 2018, 34, 1665–1673. [Google Scholar] [CrossRef] [PubMed]
- Brassard, D.; Laramée, C.; Provencher, V.; Vohl, M.-C.; Robitaille, J.; Lemieux, S.; Lamarche, B. Consumption of low nutritive value foods and cardiometabolic risk factors among French-speaking adults from Quebec, Canada: The PREDISE study. Nutr. J. 2019, 18, 49. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.T.-K.; Roberts, S.B.; Howarth, N.C.; McCrory, M.A. Effect of screening out implausible energy intake reports on relationships between diet and bmi. Obes. Res. 2005, 13, 1205–1217. [Google Scholar] [CrossRef] [PubMed]
- Garriguet, D. Nutrition: Findings from the Canadian Community Health Survey: Overview of Canadians’ Eating Habits; Canada, S., Ed.; Statistics Canada: Ottawa, ON, Canada, 2004. [Google Scholar]
- Canadian Foundation for Dietetic Research. Tracking Nutrition Trends 2013; CFDR: Toronto, ON, Canada, 2013. [Google Scholar]
- Bove, C.F.; Sobal, J. Foodwork in newly married couples. Food Cult. Soc. 2006, 9, 69–89. [Google Scholar] [CrossRef]
- Ball, K.; Crawford, D.; Mishra, G. Socio-economic inequalities in women’s fruit and vegetable intakes: A multilevel study of individual, social and environmental mediators. Public Health Nutr. 2006, 9, 623–630. [Google Scholar] [CrossRef]
- Williams, L.; Thornton, L.; Crawford, D. Optimising women’s diets. An examination of factors that promote healthy eating and reduce the likelihood of unhealthy eating. Appetite 2012, 59, 41–46. [Google Scholar] [CrossRef]
- Evans, G.L.; McNeil, L.H.; Laufman, L.; Bowman, S.L. Determinants of low-fat eating behaviors among midlife african american women. J. Nutr. Educ. Behav. 2009, 41, 327–333. [Google Scholar] [CrossRef]
- Williams, G.C.; McGregor, H.A.; Sharp, D.; Levesque, C.; Kouides, R.W.; Ryan, R.M.; Deci, E.L. Testing a self-determination theory intervention for motivating tobacco cessation: Supporting autonomy and competence in a clinical trial. Health Psychol. 2006, 25, 91–101. [Google Scholar] [CrossRef]
- Fortier, M.S.; Sweet, S.N.; O’Sullivan, T.L.; Williams, G.C. A self-determination process model of physical activity adoption in the context of a randomized controlled trial. Psychol. Sport Exerc. 2007, 8, 741–757. [Google Scholar] [CrossRef]
- McSpadden, K.E.; Patrick, H.; Oh, A.Y.; Yaroch, A.L.; Dwyer, L.A.; Nebeling, L.C. The association between motivation and fruit and vegetable intake: The moderating role of social support. Appetite 2016, 96, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Dehghan, M.; Akhtar-Danesh, N.; Merchant, A.T. Factors associated with fruit and vegetable consumption among adults. J. Hum. Nutr. Diet. 2011, 24, 128–134. [Google Scholar] [CrossRef] [PubMed]
- Swan, E.; Bouwman, L.; Hiddink, G.J.; Aarts, N.; Koelen, M. Profiling healthy eaters. Determining factors that predict healthy eating practices among dutch adults. Appetite 2015, 89, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Beydoun, M.A.; Wang, Y. Do nutrition knowledge and beliefs modify the association of socio-economic factors and diet quality among us adults? Prev. Med. 2008, 46, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Thrasher, J.F.; Campbell, M.K.; Oates, V. Behavior-specific social support for healthy behaviors among african american church members: Applying optimal matching theory. Health Educ. Behav. 2004, 31, 193–205. [Google Scholar] [CrossRef] [PubMed]
- Jackson, T. Relationships between perceived close social support and health practices within community samples of american women and men. J. Psychol. 2006, 140, 229–246. [Google Scholar] [CrossRef]
- Scholz, U.; Ochsner, S.; Hornung, R.; Knoll, N. Does social support really help to eat a low-fat diet? Main effects and gender differences of received social support within the health action process approach. Appl. Psychol. Health Well-Being 2013, 5, 270–290. [Google Scholar] [CrossRef]
- Pearce, J.; Hiscock, R.; Blakely, T.; Witten, K. The contextual effects of neighbourhood access to supermarkets and convenience stores on individual fruit and vegetable consumption. J. Epidemiol. Community Health 2008, 62, 198–201. [Google Scholar] [CrossRef]
- Brug, J.; Kremers, S.P.; Lenthe, F.; Ball, K.; Crawford, D. Environmental determinants of healthy eating: In need of theory and evidence. Proc. Nutr. Soc. 2008, 67, 307–316. [Google Scholar] [CrossRef]
- Giskes, K.; Van Lenthe, F.J.; Brug, J.; Mackenbach, J.P.; Turrell, G. Socioeconomic inequalities in food purchasing: The contribution of respondent-perceived and actual (objectively measured) price and availability of foods. Prev. Med. 2007, 45, 41–48. [Google Scholar] [CrossRef]
- Mackenbach, J.D.; Nelissen, K.G.M.; Dijkstra, S.C.; Poelman, M.P.; Daams, J.G.; Leijssen, J.B.; Nicolaou, M. A systematic review on socioeconomic differences in the association between the food environment and dietary behaviors. Nutrients 2019, 11, 2215. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Olendzki, B.C.; Pagoto, S.L.; Hurley, T.G.; Magner, R.P.; Ockene, I.S.; Schneider, K.L.; Merriam, P.A.; Hebert, J.R. Number of 24-hour diet recalls needed to estimate energy intake. Ann. Epidemiol. 2009, 19, 553–559. [Google Scholar] [CrossRef] [PubMed]
- Freedman, L.S.; Commins, J.M.; Moler, J.E.; Arab, L.; Baer, D.J.; Kipnis, V.; Midthune, D.; Moshfegh, A.J.; Neuhouser, M.L.; Prentice, R.L.; et al. Pooled results from 5 validation studies of dietary self-report instruments using recovery biomarkers for energy and protein intake. Am. J. Epidemiol. 2014, 180, 172–188. [Google Scholar] [CrossRef] [PubMed]
- Gouvernement du Québec. Panorama des Régions du Québec—Édition 2017; Institut de la statistique du Québec: Québec, QC, Canada, 2017. [Google Scholar]
| Characteristics | n (%) |
| Female | 471 (49.5) |
| Age (years) | |
| 18–34 | 348 (36.6) |
| 35–49 | 283 (29.7) |
| 50–65 | 321 (33.7) |
| Ethnicity | |
| Caucasian | 868 (91.2) |
| Highest level of education | |
| High school or less | 216 (22.7) |
| College | 290 (30.5) |
| University | 436 (45.8) |
| Missing value or prefer not to answer | 10 (1.1) |
| Occupation | |
| Worker | 604 (63.5) |
| Retired | 127 (13.3) |
| Student | 114 (12.0) |
| No job | 36 (3.8) |
| Other | 49 (5.2) |
| Missing value or prefer not to answer | 22 (2.3) |
| Marital status | |
| Married or living under common law | 604 (63.4) |
| Other status | 284 (29.8) |
| Missing value or prefer not to answer | 64 (6.7) |
| Living arrangement (living with…) | |
| Partner only | 243 (25.5) |
| Partner and children | 367 (38.6) |
| Children only | 55 (5.8) |
| Family member (other than a partner and children) | 125 (13.1) |
| Roommate | 22 (2.3) |
| Alone | 127 (13.3) |
| Missing value or prefer not to answer | 13 (1.4) |
| Smoking status | |
| Current smoker | 120 (12.6) |
| Non-smoker or former smoker | 830 (87.2) |
| Missing value | 2 (0.2) |
| Supportive Actions at Home | Non-Supportive Actions at Home | Supportive Actions Outside of Home | Non-Supportive Actions Outside of Home | |||||
|---|---|---|---|---|---|---|---|---|
| Mean ± SD | p | Mean ± SD | p | Mean ± SD | p | Mean ± SD | p | |
| Whole sample | 3.2 ± 0.9 | n/a | 1.6 ± 0.5 | n/a | 2.6 ± 0.8 | n/a | 1.6 ± 0.5 | n/a |
| Sex | 0.0343 | 0.0001 | 0.0008 | 0.79 | ||||
| Women | 3.1 ± 0.9 | 1.7 ± 0.6 | 2.7 ± 0.8 | 1.6 ± 0.5 | ||||
| Men | 3.2 ± 0.9 | 1.6 ± 0.5 | 2.6 ± 0.8 | 1.6 ± 0.5 | ||||
| Age | 0.0179 * | <0.0001 * | 0.0004 * | <0.0001 * | ||||
| 18–34 year | 3.2 ± 0.9 | 1.7 ± 0.5 | 2.8 ± 0.7 | 1.8 ± 0.6 | ||||
| 35–49 year | 3.2 ± 0.9 | 1.7 ± 0.5 | 2.7 ± 0.8 | 1.6 ± 0.4 | ||||
| 50–65 year | 3.0 ± 1.0 | 1.5 ± 0.5 | 2.5 ± 0.8 | 1.6 ± 0.5 | ||||
| Education | 0.19 † | 0.11 † | 0.0405 † | 0.48 † | ||||
| High school or less | 3.1 ± 0.9 | 1.7 ± 0.5 | 2.6 ± 0.9 | 1.7 ± 0.5 | ||||
| College or university | 3.2 ± 0.9 | 1.6 ± 0.5 | 2.7 ± 0.8 | 1.6 ± 0.5 | ||||
| Income | 0.0219 † | 0.49 † | 0.07 † | 0.20 † | ||||
| <low-income cut-off | 3.0 ± 1.0 | 1.6 ± 0.6 | 2.6 ± 0.9 | 1.7 ± 0.7 | ||||
| >low-income cut-off | 3.2 ± 0.9 | 1.6 ± 0.5 | 2.7 ± 0.8 | 1.6 ± 0.5 | ||||
| Living with | <0.0001 * | <0.0001 * | 0.26 * | 0.0124 * | ||||
| Partner only | 3.4 a± 0.7 | 1.6 a ± 0.5 | 2.6 ± 0.8 | 1.6 a,b ± 0.5 | ||||
| Partner and children | 3.3 a,b ± 0.7 | 1.8 b ± 0.5 | 2.6 ± 0.8 | 1.6 c ± 0.5 | ||||
| Children only | 3.1 b,c ± 0.7 | 1.7 a,b ± 0.5 | 2.8 ± 0.9 | 1.7 a,b,c ± 0.6 | ||||
| Family member | 3.3 a,b,c ± 0.8 | 1.7 a,b ± 0.5 | 2.6 ± 0.8 | 1.8 b ± 0.6 | ||||
| Roommate | 3.0 c ± 0.8 | 1.6 a,b ± 0.5 | 2.8 ± 0.8 | 1.7 a,b,c ± 0.4 | ||||
| Alone | 2.0 d ± 1.1 | 1.2 c ± 0.3 | 2.6 ± 0.8 | 1.5 a,c ± 0.4 | ||||
| C-HEI Score | ||
|---|---|---|
| B | (95% CI) | |
| Independent variables | ||
| Supportive actions at home | 1.50 | (0.46, 2.54) |
| Non-supportive actions at home | −3.06 | (−4.95, −1.18) |
| Supportive actions outside of home | 0.71 | (−0.46, 1.87) |
| Non-supportive actions outside of home | 0.73 | (−1.20, 2.65) |
| Covariates | ||
| Sex (1 = female, 2 = male) | −5.62 | (−7.45, −3.80) |
| Age groups (1 = 18–34 year, 2 = 35–49 year, 3 = 50–65 year) | 0.87 | (−0.18, 1.92) |
| Education (1 = high school or less, 2 = college or university) | 2.05 | (−0.04, 4.15) |
| Household annual income (1 = under low-income cut-off, 2 = over low-income cut-off) | 1.19 | (−1.46, 3.85) |
| Marital status (1 = other status, 2 = married or living in common-law) | −0.36 | (−2.47, 1.74) |
| Smoking status (1 = non-smoker/former smoker, 2 = current smoker) | −6.93 | (−9.47, −4.40) |
| Nutrition knowledge (continuous score from 0 to 100) | 0.13 | (0.06, 0.19) |
| Reporting status (1 = under-reporter, 2 = plausible reporter, 3 = over-reporter) | 2.66 | (0.82, 4.51) |
| C-HEI Score | ||||
|---|---|---|---|---|
| High School or Less * | College or University ** | |||
| B | (95% CI) | B | (95% CI) | |
| Independent variables | ||||
| Supportive actions at home | 1.37 | (−0.69, 3.44) | 1.55 | (0.32, 2.77) |
| Non-supportive actions at home | −6.09 | (9.92, −2.25) | −2.24 | (−4.42, −0.06) |
| Supportive actions outside of home | 1.10 | (−1.19, 3.38) | 0.77 | (−0.60, 2.13) |
| Non-supportive actions outside of home | 0.90 | (−3.33, 5.13) | 0.55 | (−1.66, 2.76) |
| Covariates | ||||
| Sex (1 = female, 2 = male) | −5.01 | (−9.02, −1.00) | −5.82 | (−7.89, −3.76) |
| Age groups (1 = 18–34 year, 2 = 35–49 year, 3 = 50–65 year) | 1.37 | (−0.80, 3.53) | 0.84 | (−0.37, 2.05) |
| Household annual income (1 = under low-income cut-off, 2 = over low-income cut-off) | 1.18 | (−3.38, 5.75) | 1.39 | (−1.90, 4.67) |
| Marital status (1 = other status, 2 = married or living in common-law) | −3.26 | (−7.29, 0.78) | 0.34 | (−2.16, 2.85) |
| Smoking status (1 = non-smoker/former smoker, 2 = current smoker) | −5.20 | (−9.69, −0.72) | −7.66 | (−10.75, −4.57) |
| Nutrition knowledge (continuous score from 0 to 100) | 0.30 | (0.17, 0.43) | 0.07 | (−0.01, 0.14) |
| Reporting status (1 = under-reporter, 2 = plausible reporter, 3 = over-reporter) | 2.21 | (−1.05, −5.47) | 2.94 | (0.70, 5.19) |
| Accessibility to Healthy Foods | ||
|---|---|---|
| Mean ± SD | p | |
| Whole sample | 3.8 ± 0.5 | n/a |
| Sex | 0.61 | |
| Women | 3.8 ± 0.5 | |
| Men | 3.8 ± 0.5 | |
| Age | 0.23 * | |
| 18–34 year | 3.8 ± 0.6 | |
| 35–49 year | 3.9 ± 0.5 | |
| 50–65 year | 3.8 ± 0.5 | |
| Income | 0.0007 † | |
| <low-income cut-off | 3.7 ± 0.6 | |
| >low-income cut-off | 3.9 ± 0.5 | |
| Education | 0.0027 † | |
| High school or less | 3.7 ± 0.6 | |
| College or university | 3.9 ± 0.5 | |
| C-HEI Score | ||
|---|---|---|
| B | (95% CI) | |
| Independent variables | ||
| Perceived accessibility to healthy foods | 0.01 | (−1.51, 1.53) |
| Travel time from home to the main retailer (by car; 1 = Less than 10 min, 2 = 10 min or more) | 1.31 | (−0.62, 3.24) |
| Covariates | ||
| Sex (1 = female, 2 = male) | −5.50 | (−7.22, −3.78) |
| Age groups (1 = 18–34 year, 2 = 35–49 year, 3 = 50–65 year) | 0.68 | (−0.32, 1.69) |
| Education (1 = high school or less, 2 = college or university) | 2.21 | (0.18, 4.25) |
| Household annual income (1 = under low-income cut-off, 2 = over low-income cut-off) | 1.74 | (−0.77, 4.24) |
| Marital status (1 = other status, 2 = married or living in common-law) | 0.50 | (−1.39, 2.39) |
| Smoking status (1 = non-smoker/former smoker, 2 = current smoker) | −6.71 | (−9.14, −4.27) |
| Nutrition knowledge (continuous score from 0 to 100) | 0.13 | (0.06, 0.19) |
| Reporting status (1 = under-reporter, 2 = plausible reporter, 3 = over-reporter) | 2.33 | (0.54, 4.11) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carbonneau, E.; Lamarche, B.; Robitaille, J.; Provencher, V.; Desroches, S.; Vohl, M.-C.; Bégin, C.; Bélanger, M.; Couillard, C.; Pelletier, L.; et al. Social Support, but Not Perceived Food Environment, Is Associated with Diet Quality in French-Speaking Canadians from the PREDISE Study. Nutrients 2019, 11, 3030. https://doi.org/10.3390/nu11123030
Carbonneau E, Lamarche B, Robitaille J, Provencher V, Desroches S, Vohl M-C, Bégin C, Bélanger M, Couillard C, Pelletier L, et al. Social Support, but Not Perceived Food Environment, Is Associated with Diet Quality in French-Speaking Canadians from the PREDISE Study. Nutrients. 2019; 11(12):3030. https://doi.org/10.3390/nu11123030
Chicago/Turabian StyleCarbonneau, Elise, Benoît Lamarche, Julie Robitaille, Véronique Provencher, Sophie Desroches, Marie-Claude Vohl, Catherine Bégin, Mathieu Bélanger, Charles Couillard, Luc Pelletier, and et al. 2019. "Social Support, but Not Perceived Food Environment, Is Associated with Diet Quality in French-Speaking Canadians from the PREDISE Study" Nutrients 11, no. 12: 3030. https://doi.org/10.3390/nu11123030
APA StyleCarbonneau, E., Lamarche, B., Robitaille, J., Provencher, V., Desroches, S., Vohl, M.-C., Bégin, C., Bélanger, M., Couillard, C., Pelletier, L., Bouchard, L., Houle, J., Langlois, M.-F., Corneau, L., & Lemieux, S. (2019). Social Support, but Not Perceived Food Environment, Is Associated with Diet Quality in French-Speaking Canadians from the PREDISE Study. Nutrients, 11(12), 3030. https://doi.org/10.3390/nu11123030






