Comparison and Characterization of Prenatal Nutrition Counseling among Large-for-Gestational Age Deliveries by Pre-Pregnancy BMI
Abstract
1. Introduction
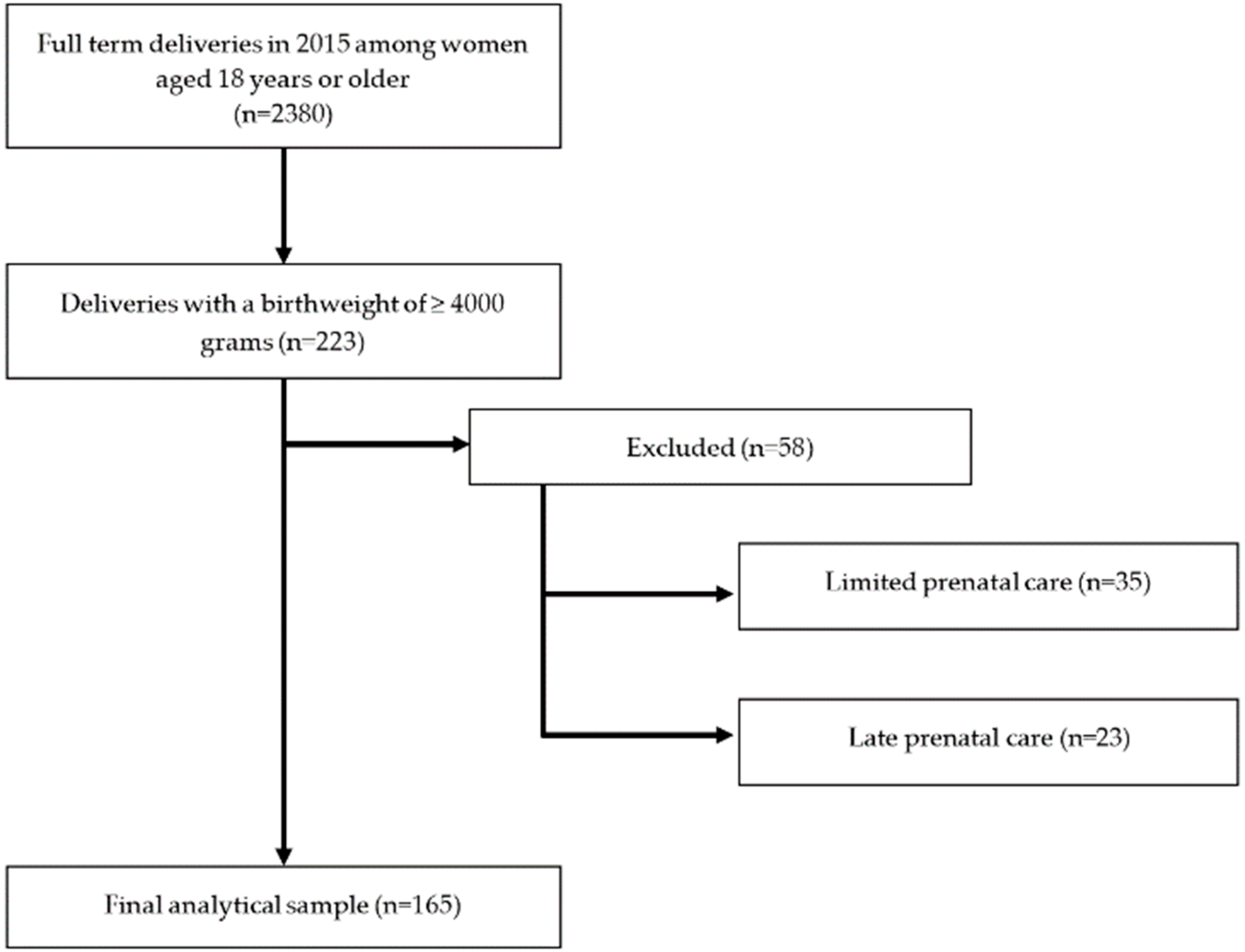
2. Materials and Methods
2.1. Methods
2.2. Data and Definitions
2.3. Statistical Analyses
3. Results
3.1. Demographics
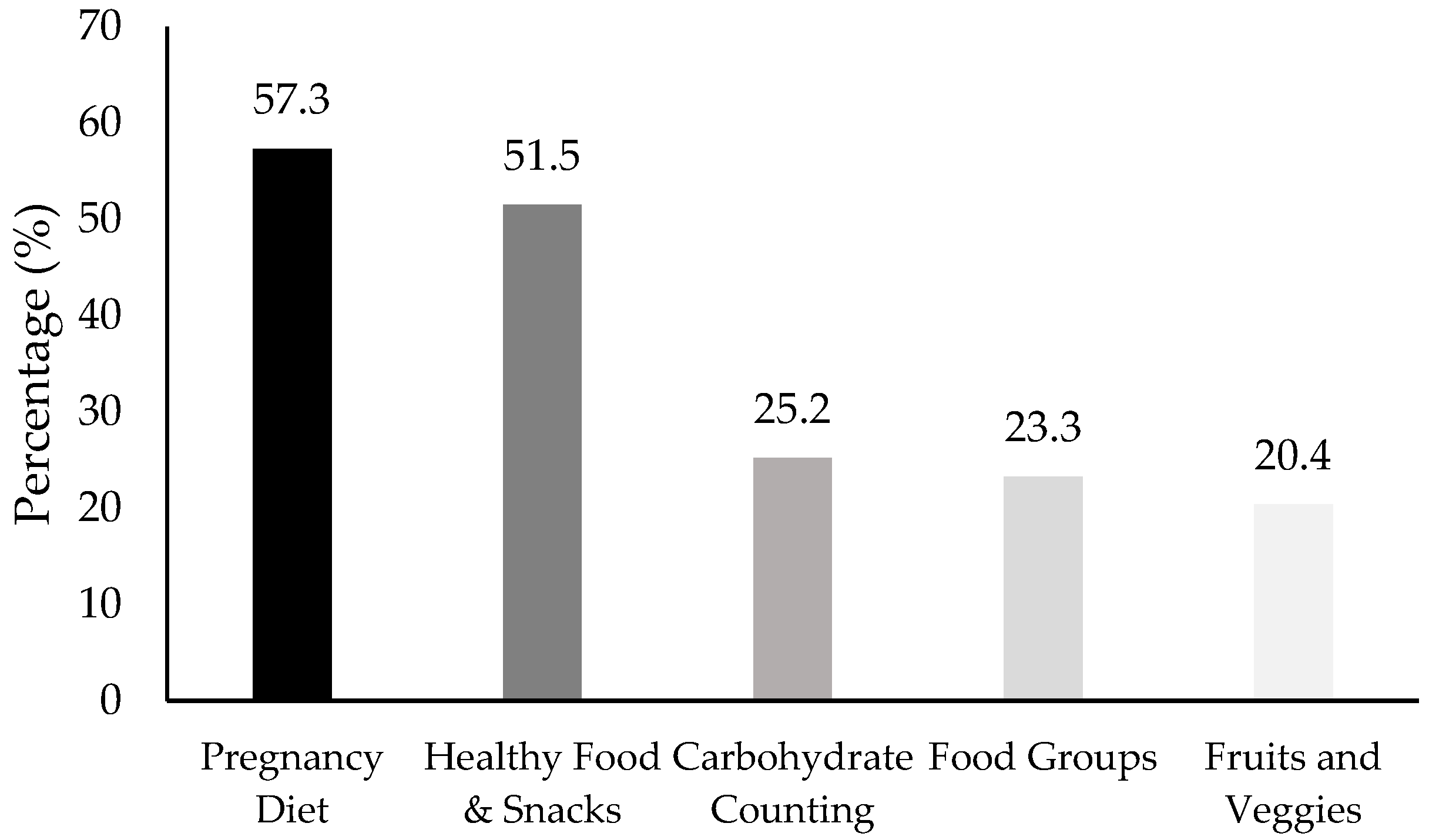
3.2. Prenatal Nutrition Counseling
3.3. Maternal and Fetal Health Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- American Academy of Pediatrics. The American College of Obstetricians and Gynecologists Guidelines for Perinatal Care, 7th ed.; American Academy of Pediatrics: Elk Grove Village, IL, USA, 2012; ISBN 9781581107340. [Google Scholar]
- World Health Organization Nutrition Counselling during Pregnancy. Available online: http://www.who.int/elena/titles/nutrition_counselling_pregnancy/en/ (accessed on 15 October 2018).
- Faucher, M.A.; Barger, M.K. Gestational weight gain in obese women by class of obesity and select maternal/newborn outcomes: A systematic review. Women Birth 2015, 28, e70–e79. [Google Scholar] [CrossRef] [PubMed]
- Guelinckx, I.; Devlieger, R.; Beckers, K.; Vansant, G. Maternal obesity: Pregnancy complications, gestational weight gain and nutrition. Obes. Rev. 2008, 9, 140–150. [Google Scholar] [CrossRef] [PubMed]
- Iwama, N.; Sugiyama, T.; Metoki, H.; Kusaka, H.; Maki, J.; Nishigori, H.; Yaegashi, N.; Sagawa, N.; Hiramatsu, Y.; Toyoda, N. Maternal body mass index is a better indicator of large-for-gestational-age infants compared with a 75-g oral glucose tolerance test in early pregnancy: The JAGS trial. Diabetes Res. Clin. Pract. 2017, 132, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Galtier-dereure, F.; Boegner, C.; Bringer, J. Obesity and pregnancy: Complications and cost 1–3. Am. J. Clin. Nutr. 2000, 71, 1242–1248. [Google Scholar] [CrossRef] [PubMed]
- Gore, S.A.; Brown, D.M.; West, D.S. The Role of Postpartum Weight Retention in Obesity Among Women: A Review of the Evidence. Ann. Behav. Med. 2003, 26, 149–159. [Google Scholar] [CrossRef] [PubMed]
- Bodnar, L.M.; Siminerio, L.L.; Himes, K.P.; Hutcheon, J.A.; Lash, T.L.; Parisi, S.M.; Abrams, B. Maternal obesity and gestational weight gain are risk factors for infant death. Obesity 2016, 24, 490–498. [Google Scholar] [CrossRef] [PubMed]
- Hyden, M. When benefits outweigh costs: Integrating dietitian services improves patient outcomes. MGMA Connex. 2014, 14, 34–36. [Google Scholar]
- Ferraro, Z.M.; Boehm, K.; Gaudet, L.; Adamo, K.B. Counselling About Gestational Weight Gain and Healthy Lifestyle During Pregnancy: Canadian Maternity Care Providers’ Self-Evaluation. Can. J. Diabetes 2013, 37, S267. [Google Scholar] [CrossRef][Green Version]
- Morris, J.; Nikolopoulos, H.; Berry, T.; Jain, V.; Vallis, M.; Piccinini-Vallis, H.; Bell, R.C. Healthcare providers’ gestational weight gain counselling practises and the influence of knowledge and attitudes: A cross-sectional mixed methods study. BMJ Open 2017, 7, e018527. [Google Scholar] [CrossRef]
- Stotland, N.; Tsoh, J.Y.; Gerbert, B. Prenatal Weight Gain: Who is Counseled? J. Women’s Health 2012, 21, 695–701. [Google Scholar] [CrossRef]
- Vinturache, A.E.; Winn, A.; Tough, S.C. Recall of Prenatal Counselling Among Obese and Overweight Women from a Canadian Population: A Population Based Study. Matern. Child Health J. 2017, 21, 2092–2101. [Google Scholar] [CrossRef] [PubMed]
- Lucas, C.; Charlton, K.E.; Yeatman, H. Nutrition Advice During Pregnancy: Do Women Receive it and Can Health Professionals Provide it? Matern. Child Health J. 2014, 18, 2465–2478. [Google Scholar] [CrossRef] [PubMed]
- Whitaker, K.M.; Wilcox, S.; Liu, J.; Blair, S.N.; Pate, R.R. Provider advice and women’s intentions to meet weight gain, physical activity, and nutrition guidelines during pregnancy. Matern. Child Health J. 2017, 20, 2309–2317. [Google Scholar] [CrossRef] [PubMed]
- Dodd, J.M.; McPhee, A.J.; Turnbull, D.; Yelland, L.N.; Deussen, A.R.; Grivell, R.M.; Crowther, C.A.; Wittert, G.; Owens, J.A.; Robinson, J.S. The effects of antenatal dietary and lifestyle advice for women who are overweight or obese on maternal diet and physical activity: The LIMIT randomised trial. BMC Med. 2014, 12, 161. [Google Scholar] [CrossRef] [PubMed]
- Dodd, J.M.; Turnbull, D.; Mcphee, A.J.; Deussen, A.R.; Grivell, R.M.; Yelland, L.N.; Crowther, C.A.; Wittert, G.; Owens, J.A.; Robinson, J.S.; et al. Antenatal lifestyle advice for women who are overweight or obese: LIMIT randomised trial Maternal dietary patterns and preterm delivery: Results from large prospective cohort study. BMJ 2014, 348, 11–14. [Google Scholar] [CrossRef] [PubMed]
- Yeo, S.; Crandell, J.L.; Jones-Vessey, K. Adequacy of Prenatal Care and Gestational Weight Gain. J. Women’s Health 2016, 25, 117–123. [Google Scholar] [CrossRef]
- Peccei, A.; Blake-Lamb, T.; Rahilly, D.; Hatoum, I.; Bryant, A. Intensive Prenatal Nutrition Counseling in a Community Health Setting. Obstet. Gynecol. 2017, 130, 423–432. [Google Scholar] [CrossRef]
- Asbee, S.M.; Jenkins, T.R.; Butler, J.R.; White, J.; Elliot, M.; Rutledge, A. Preventing excessive weight gain during pregnancy. Obstet. Gynecol. 2009, 113, 305–312. [Google Scholar] [CrossRef]
- Tanentsapf, I.; Heitmann, B.L.; Adegboye, A.R. Systematic review of clinical trials on dietary interventions to prevent excessive weight gain during pregnancy among normal weight, overweight and obese women. BMC Pregnancy Childbirth 2011, 11, 81. [Google Scholar] [CrossRef]
- Polley, B.A.; Wing, R.R.; Sims, C.J. Randomized controlled trial to prevent excessive weight gain in pregnant women. Int. J. Obes. 2002, 26, 1494. [Google Scholar] [CrossRef]
- Phelan, S.; Phipps, M.G.; Darroch, F.; Grantham, K.; Schaffner, A.; Wing, R.R. Does behavioral intervention in pregnancy reduce postpartum weight retention? Twelve-month outcomes of the Fit for Delivery randomized trial. Am. J. Clin. Nutr. 2014, 99, 302–311. [Google Scholar] [CrossRef] [PubMed]
- Laraia, B.A.; Bodnar, L.M.; Siega-Riz, A.M. Pregravid body mass index is negatively associated with diet quality during pregnancy. Public Health Nutr. 2007, 10, 920–926. [Google Scholar] [CrossRef] [PubMed]
- Kunath, J.; Gunther, J.; Rauh, K.; Hoffman, J.; Stecher, L.; Rosenfeld, E.; Kick, L.; Ulm, K.; Hauner, H. Effects of a lifestyle intervention during pregnancy to prevent excessive gestational weight gain in routine care—The cluster-randomised GeliS trial. BMC Med. 2019, 17, 5. [Google Scholar] [CrossRef] [PubMed]
- Ilmonen, J.; Isolauri, E.; Poussa, T.; Laitinen, K. Impact of dietary counselling and probiotic intervention on maternal anthropometric measurements during and after pregnancy: A randomized placebo-controlled trial. Clin. Nutr. 2011, 30, 156–164. [Google Scholar] [CrossRef] [PubMed]
- Parat, S.; Nègre, V.; Baptiste, A.; Valensi, P.; Bertrand, A.M.; Chollet, C.; Dabbas, M.; Altman, J.J.; Lapillonne, A.; Tréluyer, J.M.; et al. Prenatal education of overweight or obese pregnant women to prevent childhood overweight (the ETOIG study): An open-label, randomized controlled trial. Int. J. Obes. 2019, 43, 362–373. [Google Scholar] [CrossRef]
- Girard, A.W.; Olude, O. Nutrition Education and Counselling Provided during Pregnancy: Effects on Maternal, Neonatal and Child Health Outcomes. Paediatr. Perinat. Epidemiol. 2012, 26, 191–204. [Google Scholar] [CrossRef]
- Di Carlo, C.; Iannotti, G.; Sparice, S.; Chiacchio, M.P.; Greco, E.; Tommaselli, G.A.; Nappi, C. The role of a personalized dietary intervention in managing gestational weight gain: A prospective, controlled study in a low-risk antenatal population. Arch. Gynecol. Obstet. 2014, 289, 765–770. [Google Scholar] [CrossRef]
- Haeck, C.; Lefebvre, P. A simple recipe: The effect of a prenatal nutrition program on child health at birth. Labour Econ. 2016, 41, 77–89. [Google Scholar] [CrossRef]
- Rush, D. Nutritional services during pregnancy and birthweight: A retrospective matched pair analysis. Can. Med. Assoc. J. 1981, 125, 567–574. [Google Scholar]
| PNC | No PNC | p-Value | |
|---|---|---|---|
| Age, years (mean ± SD) | 30.4 ± 5.4 | 30.4 ± 6.1 | 0.995 |
| Race/Ethnicity, % (n) | 0.518 | ||
| Non-Hispanic White | 7.8% (8) | 4.8% (3) | |
| Hispanic White | 73.8% (76) | 85.5% (53) | |
| Black/African American | 10.7% (11) | 4.8% (3) | |
| Asian | 4.9% (5) | 3.2% (2) | |
| Other | 2.9% (3) | 1.6% (1) | |
| Marital Status, % (n) | 0.528 | ||
| Married | 41.7% (43) | 46.8% (29) | |
| Single | 58.3% (60) | 53.2% (33) | |
| Gestational Age (mean ± SD) | |||
| First PNC | 13.3 ± 5.9 | 13.4 ± 5.9 | 0.989 |
| Delivery | 39.8 ± 1.2 | 40.3 ± 0.9 | 0.003 |
| # of Prenatal Visits (mean ± SD) | 14.2 ± 6.0 | 12.1 ± 2.9 | 0.003 |
| Gradivity (mean ± SD) | 4.0 ± 2.2 | 3.8 ± 2.1 | 0.547 |
| Parity (mean ± SD) | 3.4 ± 1.8 | 3.3 ± 1.7 | 0.851 |
| Delivery Mode, % (n) | 0.004 | ||
| Vaginal | 52.9% (54) | 75.8% (47) | |
| Cesarean Section | 47.1% (48) | 24.2% (15) | |
| Body Mass Index, kg/m2 (mean ± SD) | |||
| Pre-pregnancy | 31.4 ± 6.7 | 29.0 ± 5.3 | 0.014 |
| Delivery | 36.2 ± 6.5 | 33.6 ± 5.0 | 0.009 |
| Pre-Pregnancy BMI, % (n) | 0.025 | ||
| Normal weight | 16.5% (17) | 22.6% (14) | |
| Overweight | 23.3% (24) | 38.7% (24) | |
| Obese | 60.2% (62) | 38.7% (24) | |
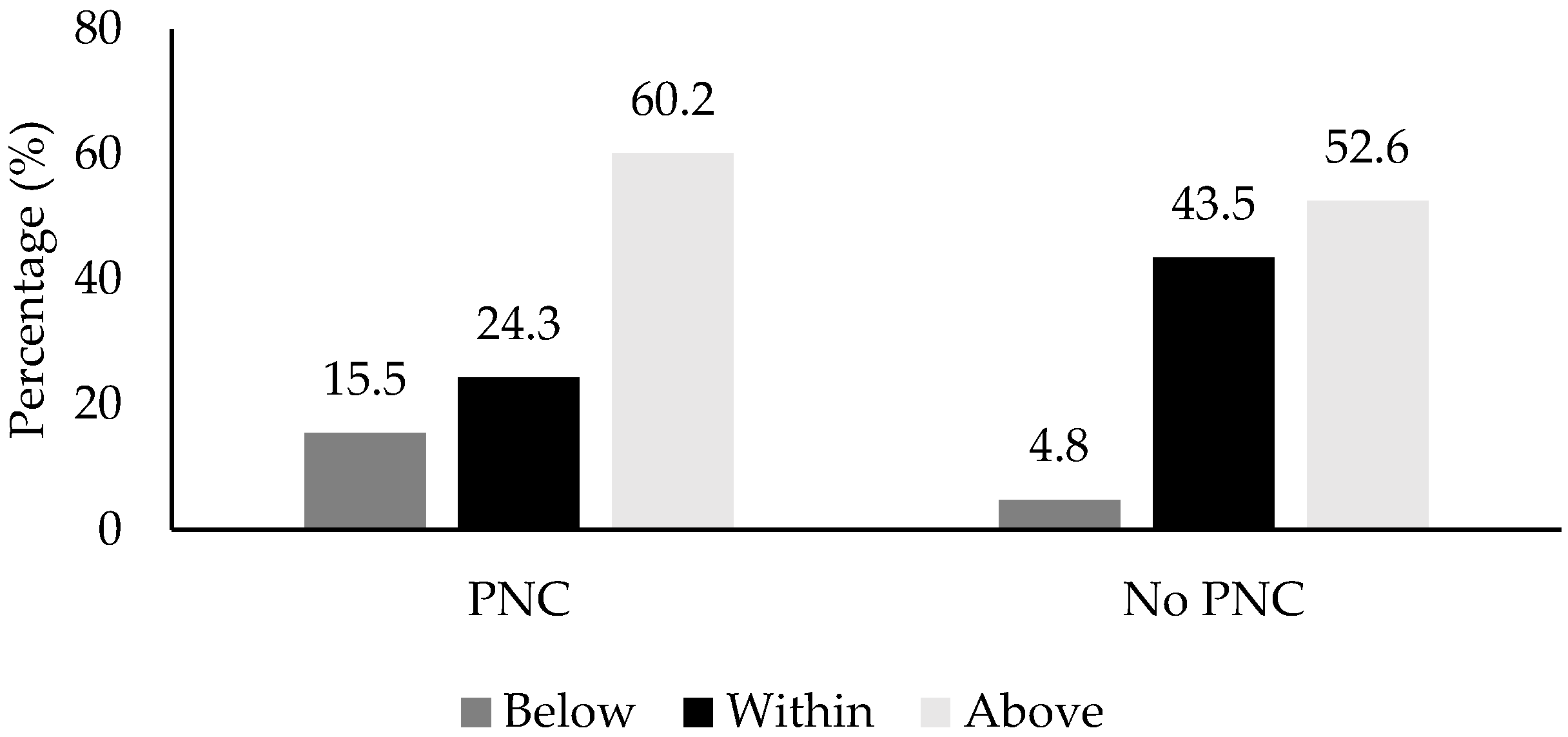
| IOM Recommendations, % (n) a | 0.012 | ||
| Below | 15.5% (16) | 4.8% (3) | |
| Within | 24.3% (25) | 43.5 (27) | |
| Above | 60.2% (62) | 51.6 (32) |
| PNC | No PNC | p-Value | Adjusted p-Value | |
|---|---|---|---|---|
| Infant Sex, % (n) | 0.981 | |||
| Male | 61.9% (60) | 61.7% (37) | ||
| Female | 38.1% (37) | 38.3% (23) | ||
| Birth Weight, g (mean ± SD) | 4313.8 ± 285.0 | 4196.8 ± 175.4 | 0.004 | 0.018 |
| Head Circumference, cm (mean ± SD) | 36.1 ± 1.3 | 36.1 ± 1.3 | 0.808 | 0.995 |
| Delivery Length, cm (mean ± SD) | 53.4 ± 3.7 | 52.7 ± 4.3 | 0.323 | 0.313 |
| 5-min Apgar Score (mean ± SD) | 7.9 ± 1.4 | 8.2 ± 1.2 | 0.153 | 0.220 |
| 10-min Apgar Score (mean ± SD) | 8.9 ± 0.7 | 8.9 ± 0.6 | 0.850 | 0.734 |
| Variable | OR | 95% CI | RR | 95% CI |
|---|---|---|---|---|
| PNC by BMI (kg/m2) Category | ||||
| Obese vs. Overweight | 2.58 | 1.24–5.40 | 1.44 | 1.06–1.97 |
| Obese vs. Normal weight | 2.13 | 0.91–4.98 | 1.32 | 0.93–1.86 |
| Overweight vs. Normal weight | 0.82 | 0.33–2.04 | 0.91 | 0.60–1.40 |
| PNC by IOM Recommendations | ||||
| Above vs. Within | 0.48 | 0.24–0.95 | 0.73 | 0.53–1.00 |
| Above vs. Below | 0.36 | 0.10–1.34 | 0.78 | 0.61–1.00 |
| Within vs. Below | 0.17 | 0.05–0.67 | 0.57 | 0.41–0.81 |
| Fetal Biometry, Mean ± SD | PNC | No PNC | p-Value |
|---|---|---|---|
| Second Trimester | |||
| Gestational Age, wks * | 21.1 ± 0.3 | 21.1 ± 0.4 | 0.905 |
| Estimated Fetal Weight, g | 471.4 ± 8.3 | 467.0 ± 10.6 | 0.750 |
| Biparietal Diameter, mm | 49.3 ± 3.4 | 55.6 ± 4.4 | 0.259 |
| Occipital Frontal Diameter, mm | 67.6 ± 1.1 | 67.7 ± 1.4 | 0.955 |
| Head Circumference, mm | 186.0 ± 0.9 | 189.2 ± 1.1 | 0.023 |
| Abdominal Circumference, mm | 167.1 ± 1.7 | 168.4 ± 2.2 | 0.639 |
| Femur Length, mm | 35.8 ± 2.1 | 38.9 ± 2.7 | 0.354 |
| Third Trimester | |||
| Gestational Age, wks * | 33.3 ± 0.5 | 33.7 ± 0.5 | 0.559 |
| Estimated Fetal Weight, g | 2789.4 ± 80.2 | 2815.6 ± 72.4 | 0.809 |
| Biparietal Diameter, mm | 84.9 ± 0.6 | 85.5 ± 0.7 | 0.54 |
| Occipital Frontal Diameter, mm | 112.0 ± 0.7 | 112.7 ± 0.8 | 0.541 |
| Head Circumference, mm | 315.5 ± 1.7 | 316.8 ± 2.9 | 0.617 |
| Abdominal Circumference, mm | 322.9 ± 3.4 | 322.3 ± 3.7 | 0.902 |
| Femur Length, mm | 66.3 ± 0.4 | 65.4 ± 0.5 | 0.15 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vander Wyst, K.B.; Quintana, G.; Balducci, J.; Whisner, C.M. Comparison and Characterization of Prenatal Nutrition Counseling among Large-for-Gestational Age Deliveries by Pre-Pregnancy BMI. Nutrients 2019, 11, 3018. https://doi.org/10.3390/nu11123018
Vander Wyst KB, Quintana G, Balducci J, Whisner CM. Comparison and Characterization of Prenatal Nutrition Counseling among Large-for-Gestational Age Deliveries by Pre-Pregnancy BMI. Nutrients. 2019; 11(12):3018. https://doi.org/10.3390/nu11123018
Chicago/Turabian StyleVander Wyst, Kiley B., Guadalupe Quintana, James Balducci, and Corrie M. Whisner. 2019. "Comparison and Characterization of Prenatal Nutrition Counseling among Large-for-Gestational Age Deliveries by Pre-Pregnancy BMI" Nutrients 11, no. 12: 3018. https://doi.org/10.3390/nu11123018
APA StyleVander Wyst, K. B., Quintana, G., Balducci, J., & Whisner, C. M. (2019). Comparison and Characterization of Prenatal Nutrition Counseling among Large-for-Gestational Age Deliveries by Pre-Pregnancy BMI. Nutrients, 11(12), 3018. https://doi.org/10.3390/nu11123018





