Effectiveness of Individual Nutrition Education Compared to Group Education, in Improving Anthropometric and Biochemical Indices among Hypertensive Adults with Excessive Body Weight: A Randomized Controlled Trial
Abstract
1. Introduction
2. Material and Methods
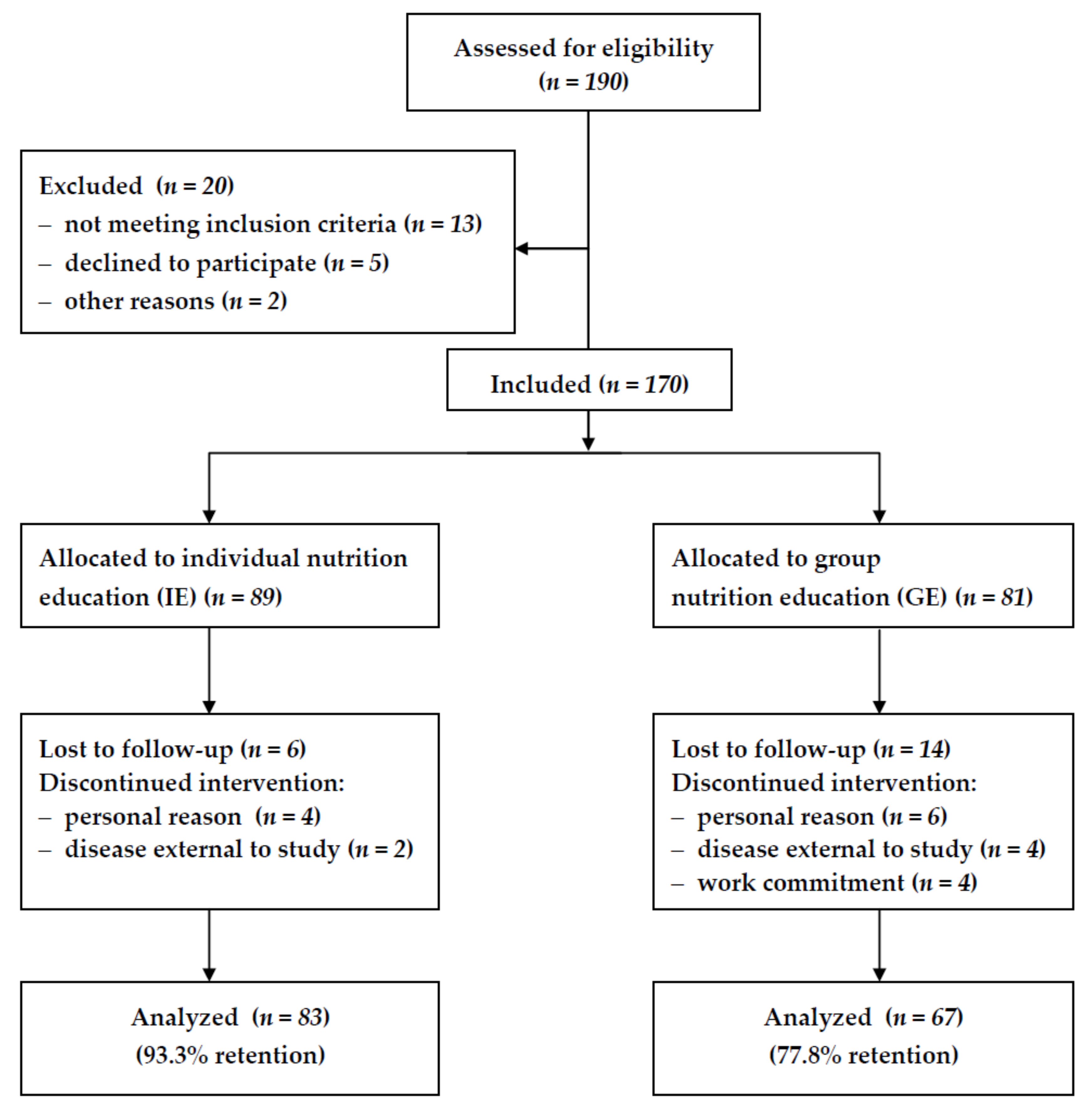
2.1. Subjects
2.2. Experimental Design
2.3. Anthropometric Measurements
2.4. Blood Pressure
2.5. Biochemical Markers
2.6. Statistical Analysis
3. Results
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Mills, K.T.; Bundy, J.D.; Kelly, T.N.; Reed, J.E.; Kearney, P.M.; Reynolds, K.; Chen, J.; He, J. Global disparities of hypertension prevalence and control: A systematic analysis of population-based studies from 90 countries. Circulation 2016, 134, 441–450. [Google Scholar] [CrossRef]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E., Jr.; Collins, K.J.; Himmelfarb, C.D.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018, 71, 1269–1324. [Google Scholar]
- NCD Risk Factor Collaboration. Worldwide trends in blood pressure from 1975 to 2015: A pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet 2017, 389, 37–55. [Google Scholar] [CrossRef]
- World Health Organization (WHO). World Health Organization 2013 A Global Brief on Hypertension. Silent Killer, Global Public Health Crisis; WHO/DCO/WHD/2013.2; WHO Press, World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Stevens, V.J.; Obarzanek, E.; Cook, N.R.; Lee, I.M.; Appel, L.J.; West, D.S.; Milas, N.C.; Mattfeldt-Beman, M.; Belden, L.; Bragg, C.; et al. Long-term weight loss and changes in blood pressure: Results of the trials of hypertension prevention, phase II. Ann. Intern. Med. 2001, 134, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Elmer, P.; Obarzanek, E.; Vollmer, W.; Simons-Morton, D.; Stevens, V.; Young, D.; Lin, P.; Champagne, C.; Harsha, D.; Svetkey, L.; et al. Effects of comprehensive lifestyle modification on diet, weight, physical fitness, and blood pressure control: 18-month results of a randomized trial. Ann. Intern. Med. 2006, 144, 485–495. [Google Scholar] [CrossRef] [PubMed]
- Ettehad, D.; Emdin, C.A.; Kiran, A.; Anderson, S.G.; Callender, T.; Emberson, J.; Chalmers, J.; Rodgers, A.; Rahimi, K. Blood pressure lowering for prevention of cardiovascular disease and death: A systematic review and meta-analysis. Lancet 2016, 387, 957–967. [Google Scholar] [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; Rosei, E.A.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef]
- Slawson, D.L.; Fitzgerald, N.; Morgan, K.T. Position of the Academy of Nutrition and Dietetics: The role of nutrition in health promotion and chronic disease prevention. J. Acad. Nutr. Diet. 2013, 113, 972–979. [Google Scholar] [CrossRef]
- Rees, K.; Takeda, A.; Martin, N.; Ellis, L.; Wijesekara, D.; Vepa, A.; Das, A.; Hartley, L.; Stranges, S. Mediterranean-Style diet for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst. Rev. 2019, 3, CD009825. [Google Scholar] [CrossRef]
- Pallazola, V.A.; Davis, D.M.; Whelton, S.P.; Cardoso, R.; Latina, J.M.; Michos, E.D.; Sarkar, S.; Blumenthal, R.S.; Arnett, D.K.; Stone, N.J.; et al. A clinician’s guide to healthy eating for cardiovascular disease prevention. Mayo Clin. Proc. Inn. Qual. Out. 2019, 3, 251–267. [Google Scholar]
- Sacks, F.M.; Svetkey, L.P.; Vollmer, W.M.; Appel, L.J.; Bray, G.A.; Harsha, D.; Obarzanek, E.; Conlin, P.R.; Miller, E.R.; Simons-Morton, D.G.; et al. DASH-Sodium Collaborative Research Group. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH). Diet. N. Engl. J. Med. 2001, 344, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Swain, J.F.; McCarron, P.B.; Hamilton, E.F.; Sacks, F.M.; Appel, L.J. Characteristics of the diet patterns tested in the OptimalMacronutrient Intake Trial to Prevent Heart Disease (OmniHeart): Options for a Heart-Healthy. Diet. J. Am. Diet. Assoc. 2008, 108, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, D.J.A.; Jones, P.J.; Frohlich, J.; Lamarche, B.; Ireland, C.; Nishi, S.K.; Srichaikul, K.; Galange, P.; Pellini, C.; Faulkner, D.; et al. The effect of a dietary portfolio compared to a DASH-type diet on blood pressure. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 1132e1139. [Google Scholar] [CrossRef] [PubMed]
- Nissensohn, M.; Vinas, B.R.; Sanchez-Villegas, A.; Piscopo, S.; Serra-Majem, L. The effect of the Mediterranean diet on hypertension: A systematic review and meta-analysis. J. Nutr. Educ. Behav. 2016, 48, 42–53. [Google Scholar] [CrossRef]
- Pettersen, B.J.; Anousheh, R.; Fan, J.; Jaceldo-Siegl, K.; Fraser, G.E. Vegetarian diets and blood pressure among white subjects: Results from the Adventist Health Study-2 (AHS-2). Public Health Nutr. 2012, 15, 1909–1916. [Google Scholar] [CrossRef]
- Spahn, J.M.; Reeves, R.S.; Keim, K.S.; Laquatra, I.; Kellogg, M.; Jortberg, B.; Clark, N.A. State of the evidence regarding behavior change theories and strategies in nutrition counseling to facilitate health and food behavior change. J. Am. Diet. Assoc. 2010, 110, 879–891. [Google Scholar] [CrossRef]
- Patnode, C.D.; Evans, C.V.; Senger, C.A.; Redmond, N.; Lin, J.S. Behavioral Counseling to Promote a Healthful Diet and Physical Activity for Cardiovascular Disease Prevention in Adults Without Known Cardiovascular Disease Risk Factors: Updated Systematic Review for the U.S. Preventive Services Task Force; Evidence Synthesis No. 152; AHRQ Publication No. 15-05222-EF-1; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2017. [Google Scholar]
- Gajewska, D.; Niegowska, J.; Kucharska, A. Compliance to DASH diet by patients with essential hypertension. Pol. J. Food Nutr. Sci. 2010, 60, 71–76. [Google Scholar]
- Kucharska, A.; Gajewska, D.; Kiedrowski, M.; Sińska, B.; Czerw, A.; Juszczyk, G.; Augustynowicz, A.; Bobiński, K.; Deptała, A.; Niegowska, J. The impact of individualized nutritional therapy according to DASH diet on blood pressure, body mass and selected biochemical parameters in overweight/obese patients with primary arterial hypertension: A prospective randomized study. Kardiol. Pol. 2018, 76, 158–165. [Google Scholar] [CrossRef]
- World Health Organisation (WHO). Obesity: Preventing and Managing the Global Epidemic; Report of a WHO Consultation; Technical Report Series No 894; WHO: Geneva, Switzerland, 2000. [Google Scholar]
- Lukaski, H.C. Evolution of bioimpedance: A circuitous journey from estimation of physiological function to assessment of body composition and a return to clinical research. Eur. J. Clin. Nutr. 2013, 67, S2–S9. [Google Scholar] [CrossRef]
- Kylea, U.G.; Bosaeusb, I.; De Lorenzoc, A.D.; Deurenbergd, P.; Eliae, M.; Gómez, J.M.; Heitmann, B.L.; Kent-Smithh, L.; Melchiori, J.-C.; Pirlichj, M.; et al. Bioelectrical impedance analysis-part II: Utilization in clinical practice. Clin. Nutr. 2004, 23, 1430–1453. [Google Scholar] [CrossRef]
- Matthews, D.R.; Hosker, J.; Rudenski, A.S.; Naylor, B.A.; Treacher, D.F.; Turner, R.C. Homeostasis model assessment: Insulin resistance and β-cell function from fasting plasma glucose and insulin concentration in man. Diabetologia 1985, 28, 412–419. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2018. [Google Scholar]
- Aldana, S.G.; Greenlaw, R.L.; Diehl, H.A.; Salberg, A.; Merrill, R.M.; Ohmine, S.; Thomas, C. The behavioral and clinical effects of therapeutic lifestyle change on middle-aged adults. Prev. Chronic Dis. 2006, 3, 1. [Google Scholar]
- Renjilian, D.A.; Perri, M.G.; Nezu, A.M.; McKelvey, W.F.; Shermer, R.L.; Anton, S.D. Individual versus group therapy for obesity: Effects of matching participants to their treatment preferences. J. Consult. Clin. Psychol. 2001, 69, 717–721. [Google Scholar] [CrossRef] [PubMed]
- Befort, C.A.; Donnelly, J.E.; Sullivan, D.K.; Ellerbeck, E.F.; Perri, M.G. Group versus individual phone-based obesity treatment for rural women. Eat. Behav. 2010, 11, 11. [Google Scholar] [CrossRef]
- Kalavainen, M.P.; Korppi, M.O.; Nuutinen, O.M. Clinical efficacy of group-based treatment for childhood obesity compared with routinely given individual counselling. Int. J. Obes. 2007, 31, 1500–1508. [Google Scholar] [CrossRef]
- Phimarn, W.; Paktipat, P.; Pansiri, K.; Klabklang, P.; Duangjanchot, P.; Tongkul, A. Effect of weight control counselling in overweight and obese young adults. Indian J. Pharm. Sci. 2017, 79, 35–41. [Google Scholar] [CrossRef]
- Kloek, C.J.J.; Tol, J.; Veenhof, C.; van der Wulp, I.; Swinkels, I.C.S. Dutch general practitioners’ weight management policy for overweight and obese patients. BMC Obes. 2014, 1, 2. [Google Scholar] [CrossRef]
- Brotons, C.; Ciurana, R.; Piñeiro, R.; Kloppe, P.; Godycki-Cwirko, M.; Sammut, M.R. Dietary advice in clinical practice: The views of general practitioners in Europe. Am. J. Clin. Nutr. 2003, 77, 1048S–1051S. [Google Scholar]
- Wynn, K.; Trudeau, J.D.; Taunton, K.; Gowans, M.; Scott, I. Nutrition in primary care. Current practices, attitudes, and barriers. Can. Fam. Physician 2010, 56, e109–e116. [Google Scholar]
- Nicholas, L.G.; Pond, C.D.; Roberts, D.C.K. Dietitian–general practitioner interface: A pilot study on what influences the provision of effective nutrition management. Am. J. Clin. Nutr. 2003, 77, 1039S–1042S. [Google Scholar] [CrossRef]
- Dahl, B.R.; Reed, M.H. Effect on a nutrition education program on the reduction of serum cholesterol level in Veterans Administration patients. J. Am. Diet. Assoc. 1995, 95, 702–705. [Google Scholar] [CrossRef]
- Hinderliter, A.L.; Sherwood, A.; Craighead, L.W.; Lin, P.-H.; Watkins, L.; Babyak, M.A.; Blumentha, J.A. The long-term effects of lifestyle change on blood pressure: One-year follow-up of the ENCORE study. Am. J. Hypertens. 2014, 27, 734–741. [Google Scholar] [CrossRef] [PubMed]
- Stone, N.J. Nonpharmacologic management of mixed dyslipidemia associated with diabetes mellitus and the metabolic syndrome: A review of the evidence. Am. J. Cardiol. 2008, 102, 14L–18L. [Google Scholar] [CrossRef] [PubMed]
- Vogeser, M.; König, D.; Frey, I.; Predel, H.-G.; Parhofer, K.G.; Berg, A. fasting serum insulin and the homeostasis model of insulin resistance (HOMA-IR) in the monitoring of lifestyle interventions in obese persons. Clin. Biochem. 2007, 40, 964–968. [Google Scholar] [CrossRef]
- Yamaoka, K.; Tango, K. Efficacy of lifestyle education to prevent type 2 diabetes. A meta-analysis of randomized controlled trials. Diab. Care 2005, 28, 2780–2786. [Google Scholar] [CrossRef]
- Beto, J.A.; Schury, K.A.; Bansal, V.K. Strategies to promote adherence to nutritional advice in patients with chronic kidney disease: A narrative review and commentary. Int. J. Nephrol. Renovasc. Dis. 2016, 9, 21–33. [Google Scholar] [CrossRef]
- De Camargo, K.R.; Coeli, C.M. Theory in practice: Why “good medicine” and “scientific medicine” are not necessarily the same thing. Adv. Health Sci. Educ. 2006, 11, 77–89. [Google Scholar] [CrossRef]
- Trivedi, R.B.; Ayotte, B.; Edelman, D.; Bosworth, H.B. The association of emotional well-being and marital status with treatment adherence among patients with hypertension. J. Behav. Med. 2008, 31, 489–497. [Google Scholar] [CrossRef]
- Miller, N.H.; Hill, M.; Kottke, T.; Ockene, I.S. The multilevel compliance challenge: Recommendations for a call to action: A statement for healthcare professionals. Circulation 1997, 95, 1085–1090. [Google Scholar] [CrossRef]
- Desroches, S.; Lapointe, A.; Ratté, S.; Gravel, K.; Légaré, F.; Turcotte, S. Interventions to enhance adherence to dietary advice for preventing and managing chronic diseases in adults. Cochrane Database Syst. Rev. 2013, 28. [Google Scholar] [CrossRef]


| Parameter | All (n) | Q1 | Q2 | Q3 |
|---|---|---|---|---|
| Age (years) | 60.7 ± 9.3 (150) | 55 | 60 | 68 |
| Weight (kg) | 91.0 ± 15.3 (150) | 80.0 | 90.0 | 100.5 |
| WC (cm) | 104.7 ± 11.3 (150) | 97.0 | 104.0 | 112.0 |
| BMI (kg/m2) | 32.8 ± 4.3 (150) | 29.2 | 32.3 | 35.1 |
| Fat mass (%) | 35.6 ± 8.9 (150) | 28.7 | 35.1 | 42.0 |
| SBP (mmHg) | 130.1 ± 6.3 (150) | 126.0 | 130.0 | 136.0 |
| DBP (mmHg) | 84.3 ± 3.7 (150) | 84.0 | 82.0 | 88.0 |
| FPG (mmol/L) | 5.4 ± 0.7 (149) | 5.0 | 5.5 | 5.8 |
| FIRI (μU/mL) | 15.8 ± 10.1 (149) | 10.2 | 13.6 | 18.7 |
| OGTT (mmol/L) | 6.9 ± 3.0 (141) | 4.8 | 6.3 | 9.1 |
| Homa-IR | 3.8 ± 2.6 (150) | 2.3 | 3.4 | 4.7 |
| TC (mmol/L) | 5.2 ± 1.1 (146) | 4.4 | 5.1 | 5.8 |
| HDL-C (mmol/L) | 1.4 ± 0.3 (145) | 1.2 | 1.3 | 1.6 |
| LDL-C (mmol/L) | 3.4 ± 0.9 (145) | 2.7 | 3.2 | 3.9 |
| TG (mmol/L) | 1.8 ± 0.9 (146) | 1.1 | 1.6 | 2.2 |
| Individual Education (IE) | Group Education (GE) | p Value 2 | |||||
|---|---|---|---|---|---|---|---|
| Before (n) | After | p Value 1 | Before (n) | After | p Value 1 | ||
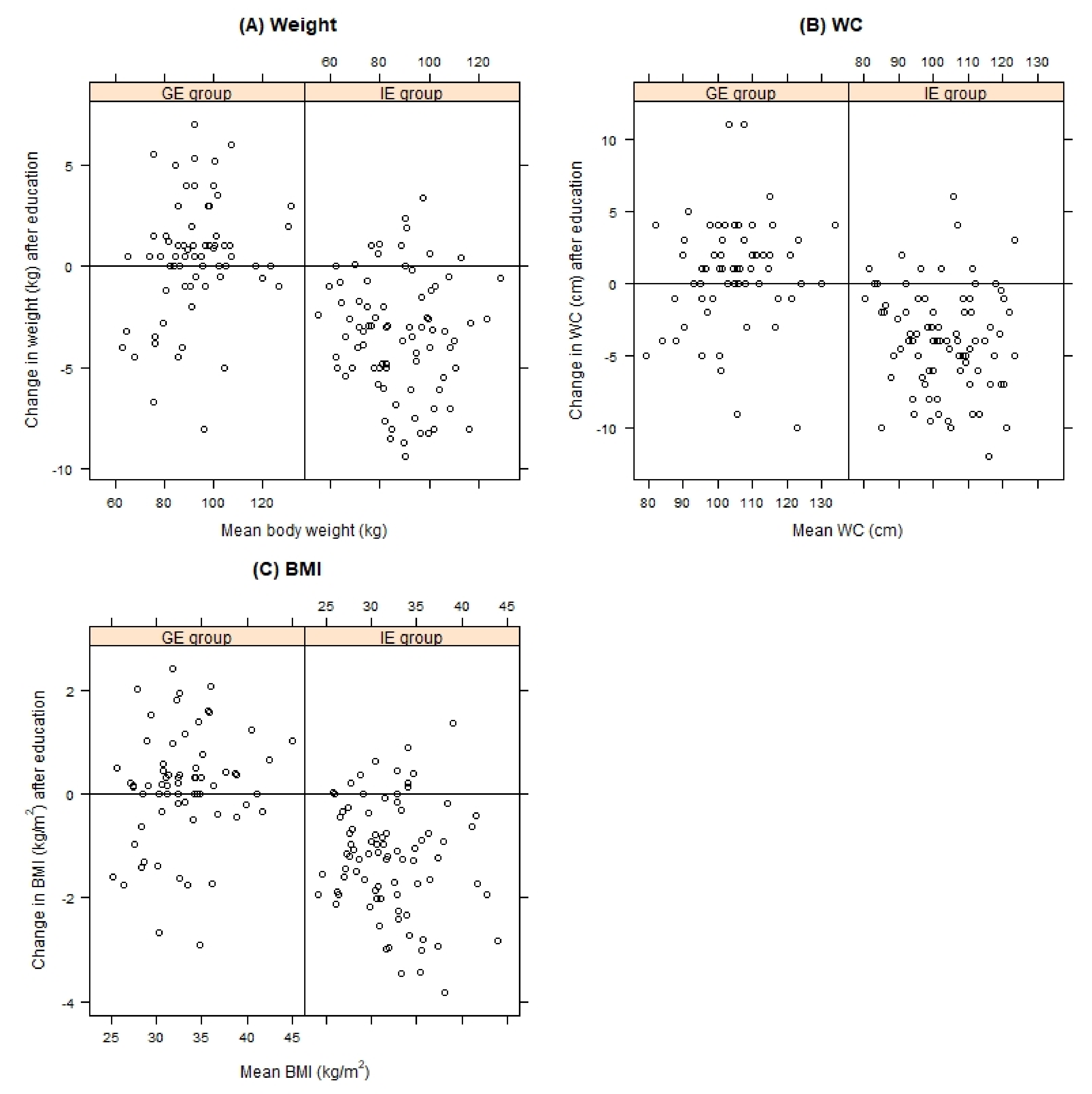
| Weight (kg) | 89.7 ± 16.1 (82) | 86.4 ± 15.9 | < 0.001 | 92.4 ± 14.5 (66) | 92.8 ± 15.3 | 0.282 | < 0.001 |
| WC (cm) | 105.2 ± 11.5 (82) | 101.2 ± 11.1 | < 0.001 | 104.0 ± 11.1 (67) | 104.7 ± 11.6 | 0.139 | < 0.001 |
| BMI (kg/m2) | 32.6 ± 4.5 (83) | 31.4 ± 4.3 | < 0.001 | 33.0 ± 4.2 (66) | 33.1 ± 4.4 | 0.378 | < 0.001 |
| Fat mass (%) | 34.9 ± 7.6 (63) | 34.0 ± 8.1 | 0.069 | 36.3 ± 10.0 (65) | 36.4 ± 10.6 | 0.905 | 0.100 |
| SBP (mmHg) | 130.1 ± 6.2 (81) | 125.6 ± 5.0 | < 0.001 | 130.3 ± 6.5 (66) | 130.9 ± 6.2 | 0.174 | < 0.001 |
| DBP (mmHg) | 85 ± 3.6 (81) | 82.1 ± 2.9 | < 0.001 | 83.4 ± 3.8 (66) | 85.0 ± 3.7 | 0.001 | < 0.001 |
| FPG (mmol/L) | 5.5 ± 0.7 (74) | 5.4 ± 0.7 | 0.117 | 5.3 ± 0.7 (66) | 5.5 ± 1.1 | 0.034 | 0.011 |
| FIRI (μU/mL) | 17.6 ± 13.1 (65) | 15.8 ± 10.3 | 0.082 | 14.1 ± 6.4 (50) | 16.4 ± 10.6 | 0.016 | 0.005 |
| OGTT (mmol/L) | 7.4 ± 3.0 (64) | 7.1 ± 2.4 | 0.248 | 6.3 ± 2.8 (53) | 7.2 ± 3.1 | 0.041 | 0.030 |
| Homa-IR | 4.4 ± 3.2 (65) | 3.8 ± 2.7 | 0.041 | 3.4 ± 1.7 (50) | 4.1 ± 2.8 | 0.003 | < 0.001 |
| TC (mmol/L) | 5.1 ± 1.1 (69) | 5.0 ± 1.0 | 0.085 | 5.3 ± 1.0 (60) | 5.2 ± 0.9 | 0.150 | 0.748 |
| HDL-C (mmol/L) | 1.4 ± 0.3 (69) | 1.4 ± 0.3 | 0.255 | 1.4 ± 0.3 (60) | 1.4 ± 0.3 | 0.151 | 0.546 |
| LDL-C (mmol/L) | 3.3 ± 1.0 (69) | 3.2 ± 0.9 | 0.213 | 3.5 ± 0.9 (59) | 3.3 ± 0.8 | 0.012 | 0.485 |
| TG (mmol/L) | 1.9 ± 0.9 (69) | 1.7 ± 0.8 | 0.018 | 1.6 ± 0.8 (59) | 1.7 ± 0.8 | 0.703 | 0.144 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gajewska, D.; Kucharska, A.; Kozak, M.; Wunderlich, S.; Niegowska, J. Effectiveness of Individual Nutrition Education Compared to Group Education, in Improving Anthropometric and Biochemical Indices among Hypertensive Adults with Excessive Body Weight: A Randomized Controlled Trial. Nutrients 2019, 11, 2921. https://doi.org/10.3390/nu11122921
Gajewska D, Kucharska A, Kozak M, Wunderlich S, Niegowska J. Effectiveness of Individual Nutrition Education Compared to Group Education, in Improving Anthropometric and Biochemical Indices among Hypertensive Adults with Excessive Body Weight: A Randomized Controlled Trial. Nutrients. 2019; 11(12):2921. https://doi.org/10.3390/nu11122921
Chicago/Turabian StyleGajewska, Danuta, Alicja Kucharska, Marcin Kozak, Shahla Wunderlich, and Joanna Niegowska. 2019. "Effectiveness of Individual Nutrition Education Compared to Group Education, in Improving Anthropometric and Biochemical Indices among Hypertensive Adults with Excessive Body Weight: A Randomized Controlled Trial" Nutrients 11, no. 12: 2921. https://doi.org/10.3390/nu11122921
APA StyleGajewska, D., Kucharska, A., Kozak, M., Wunderlich, S., & Niegowska, J. (2019). Effectiveness of Individual Nutrition Education Compared to Group Education, in Improving Anthropometric and Biochemical Indices among Hypertensive Adults with Excessive Body Weight: A Randomized Controlled Trial. Nutrients, 11(12), 2921. https://doi.org/10.3390/nu11122921






