A Randomised Trial to Optimise Gestational Weight Gain and Improve Maternal and Infant Health Outcomes through Antenatal Dietary, Lifestyle and Exercise Advice: The OPTIMISE Randomised Trial
Abstract
1. Introduction
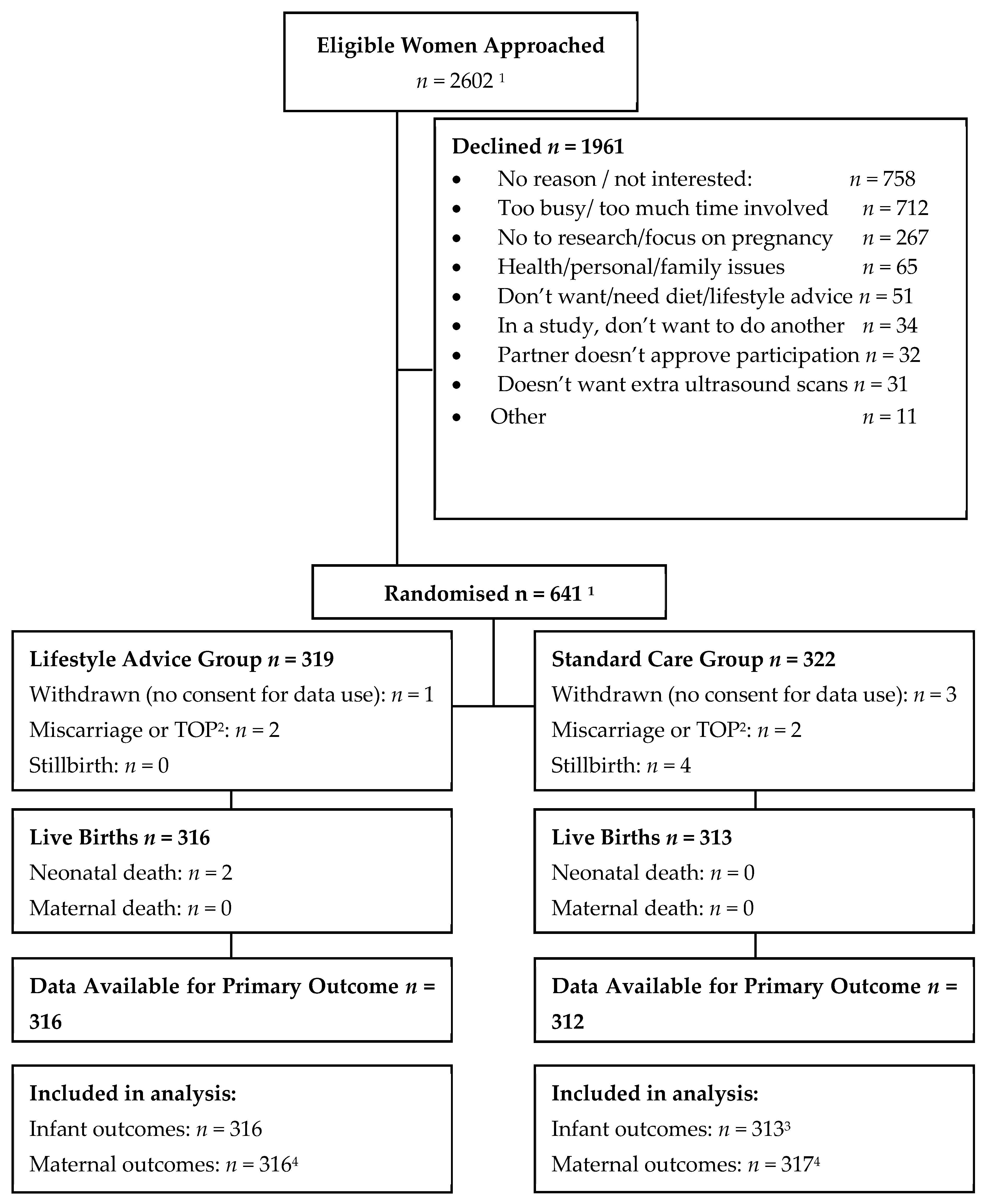
2. Materials and Methods
2.1. Trial Design
2.2. Outcome Measures
2.2.1. Secondary Infant Outcomes
2.2.2. Maternal Antepartum, Labour and Birth Outcomes
2.2.3. Maternal Weight Change
2.2.4. Maternal Diet and Physical Activity
2.2.5. Maternal Quality of Life
2.3. Sample Size Estimate
2.4. Analysis and Reporting of Results
3. Results
3.1. Participant Characteristics
3.2. Pre-Specified Infant Outcomes
3.3. Maternal Diet Quality
3.4. Pre-Specified Maternal Antepartum Outcomes
3.5. Pre-Specified Maternal Labour and Birth Outcomes
3.6. Effect Modification by Maternal Pre-Pregnancy BMI
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organisation. 2008–2013 Action Plan for the Global Strategy for the Prevention and Control of Noncommunicable Diseases: Prevent and Control Cardiovascular Diseases, Cancers, Chronic Respiratory Diseases and Diabetes; World Health Organisation WHO: Geneva, Switzerland, 2008. [Google Scholar]
- Walls, H.L.; Magliano, D.J.; Stevenson, C.E.; Backholer, K.; Mannan, H.R.; Shaw, J.E.; Peeters, A. Projected progression of the prevalence of obesity in australia. Obesity (Silver Spring) 2012, 20, 872–878. [Google Scholar] [CrossRef] [PubMed]
- Ball, K.; Crawford, D.; Ireland, P.; Hodge, A. Patterns and demographic predictors of 5-year weight change in a multi-ethnic cohort of men and women in Australia. Public Health Nutr. 2003, 6, 269–281. [Google Scholar] [CrossRef] [PubMed]
- Adamson, L.; Brown, W.; Byles, J.; Chojenta, C.; Dobson, A.; Fitzgerald, D.; Hockey, R.; Loxton, D.; Powers, J.; Spallek, M.; et al. Women’s Weight: Findings from the Australian Longitudinal Study on Women’s Health, Report prepared for the Australian Government Department of Health. Available online: https://www.alswh.org.au/images/content/pdf/major_reports/ALSWH%202018%20Major%20Report_Caring%20final.pdf (accessed on 30 June 2013).
- Cameron, A.J.; Welborn, T.A.; Zimmet, P.Z.; Dunstan, D.W.; Owen, N.; Salmon, J.; Dalton, M.; Jolley, D.; Shaw, J.E. Overweight and obesity in Australia: The 1999–2000 Australian diabetes, obesity and lifestyle study (ausdiab). Med. J. Aust. 2003, 178, 427–432. [Google Scholar] [CrossRef] [PubMed]
- Mannan, M.; Doi, S.A.R.; Mamun, A.A. Association between weight gain during pregnancy and postpartum weight retention and obesity: A bias-adjusted meta-analysis. Nutr. Rev. 2013, 71, 343–352. [Google Scholar] [CrossRef] [PubMed]
- Gunderson, E.P.; Abrams, B. Epidemiology of gestational weight gain and body weight changes after pregnancy. Epidemiol. Rev. 2000, 22, 261–274. [Google Scholar] [CrossRef] [PubMed]
- Schmitt, N.M.; Nicholson, W.K.; Schmitt, J. The association of pregnancy and the development of obesity—Results of a systematic review and meta-analysis on the natural history of postpartum weight retention. Int. J. Obes. (Lond.) 2007, 31, 1642–1651. [Google Scholar] [CrossRef]
- Institute of Medicine. Subcommittee on Nutritional Status and Weight Gain in Pregnancy. In Nutrition during Pregnancy; National Academy Press: Washington, DC, USA, 1990. [Google Scholar]
- Institute of Medicine. Subcommittee on Nutritional Status and Weight Gain in Pregnancy. In Weight Gain during Pregnancy: Reexamining the Guidelines; National Academies Press: Washington, DC, USA, 2009. [Google Scholar]
- Dodd, J.M.; Grivell, R.M.; Nguyen, A.M.; Chan, A.; Robinson, J.S. Maternal and perinatal health outcomes by body mass index category. Aust. N. Z. J. Obstet. Gynaecol. 2011, 51, 136–140. [Google Scholar] [CrossRef]
- Callaway, L.K.; Prins, J.B.; Chang, A.M.; McIntyre, H.D. The prevalence and impact of overweight and obesity in an australian obstetric population. Med. J. Aust. 2006, 184, 56–59. [Google Scholar] [CrossRef]
- Cedergren, M. Effects of gestational weight gain and body mass index on obstetric outcome in sweden. Int. J. Gynecol. Obstet. 2006, 93, 269–274. [Google Scholar] [CrossRef]
- Cedergren, M.I. Optimal gestational weight gain for body mass index categories. Obstet. Gynecol. 2007, 110, 759–764. [Google Scholar] [CrossRef]
- Rooney, B.L.; Schauberger, C.W. Excess pregnancy weight gain and long-term obesity: One decade later. Obstet. Gynecol. 2002, 100, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Rooney, B.L.; Schauberger, C.W.; Mathiason, M.A. Impact of perinatal weight change on long-term obesity and obesity-related illnesses. Obstet. Gynecol. 2005, 106, 1349–1356. [Google Scholar] [CrossRef] [PubMed]
- Amorim, A.R.; Rössner, S.; Neovius, M.; Lourenço, P.M.; Linné, Y. Does excess pregnancy weight gain constitute a major risk for increasing long-term bmi? Obesity (Silver Spring) 2007, 15, 1278–1286. [Google Scholar] [CrossRef] [PubMed]
- Ma, D.; Szeto, I.M.; Yu, K.; Ning, Y.; Li, W.; Wang, J.; Zheng, Y.; Zhang, Y.; Wang, P. Association between gestational weight gain according to prepregnancy body mass index and short postpartum weight retention in postpartum women. Clin. Nutr. 2015, 34, 291–295. [Google Scholar] [CrossRef] [PubMed]
- Nehring, I.; Schmoll, S.; Beyerlein, A.; Hauner, H.; von Kries, R. Gestational weight gain and long-term postpartum weight retention: A meta-analysis. Am. J. Clin. Nutr. 2011, 94, 1225–1231. [Google Scholar] [CrossRef] [PubMed]
- Retnakaran, R.; Qi, Y.; Sermer, M.; Connelly, P.W.; Hanley, A.J.; Zinman, B. Glucose intolerance in pregnancy and future risk of pre-diabetes or diabetes. Diabetes Care 2008, 31, 2026–2031. [Google Scholar] [CrossRef] [PubMed]
- Hedderson, M.M.; Gunderson, E.P.; Ferrara, A. Gestational weight gain and risk of gestational diabetes mellitus. Obstet. Gynecol. 2010, 115, 597–604. [Google Scholar] [CrossRef]
- Shah, B.R.; Retnakaran, R.; Booth, G.L. Increased risk of cardiovascular disease in young women following gestational diabetes mellitus. Diabetes Care 2008, 31, 1668–1669. [Google Scholar] [CrossRef]
- Jonsdottir, L.S.; Arngrimsson, R.; Geirsson, R.T.; Sigvaldason, H.; Sigfusson, N. Death rates from ischemic heart disease in women with a history of hypertension in pregnancy. Acta. Obstet. Gynecol. Scand. 1995, 74, 772–776. [Google Scholar] [CrossRef]
- Fraser, A.; Tilling, K.; Macdonald-Wallis, C.; Hughes, R.; Sattar, N.; Nelson, S.M.; Lawlor, D.A. Associations of gestational weight gain with maternal body mass index, waist circumference, and blood pressure measured 16 y after pregnancy: The avon longitudinal study of parents and children (alspac). Am. J. Clin. Nutr. 2011, 93, 1285–1292. [Google Scholar] [CrossRef]
- Mamun, A.A.; Kinarivala, M.; O’Callaghan, M.J.; Williams, G.M.; Najman, J.M.; Callaway, L.K. Associations of excess weight gain during pregnancy with long-term maternal overweight and obesity: Evidence from 21y postpartum follow-up. Am. J. Clin. Nutr. 2010, 91, 1336–1341. [Google Scholar] [CrossRef] [PubMed]
- Rooney, B.L.; Mathiason, M.A.; Schauberger, C.W. Predictors of obesity in childhood, adolescence, and adulthood in a birth cohort. Matern. Child Health J. 2011, 15, 1166–1175. [Google Scholar] [CrossRef] [PubMed]
- Oken, E.; Taveras, E.M.; Kleinman, K.P.; Rich-Edwards, J.W.; Gillman, M.W. Gestational weight gain and child adiposity at age 3 years. Am. J. Obstet. Gynecol. 2007, 196, 322–328. [Google Scholar] [CrossRef] [PubMed]
- Wrotniak, B.H.; Shults, J.; Butts, S.; Stettler, N. Gestational weight gain and risk of overweight in the offspring at age 7 y in a multicenter, multiethnic cohort study. Am. J. Clin. Nutr. 2008, 87, 1818–1824. [Google Scholar] [CrossRef] [PubMed]
- Cnattingius, S.; Villamor, E.; Lagerros, Y.T.; Wikstrom, A.K.; Granath, F. High birth weight and obesity—A vicious circle across generations. Int. J. Obes. (Lond.) 2012, 36, 1320–1324. [Google Scholar] [CrossRef] [PubMed]
- Schack-Nielsen, L.; Michaelsen, K.F.; Gamborg, M.; Mortensen, E.L.; Sorensen, T.I.A. Gestational weight gain in relation to offspring body mass index and obesity from infancy through adulthood. Int. J. Obesity 2010, 34, 67–74. [Google Scholar] [CrossRef]
- Lawlor, D.A.; Lichtenstein, P.; Fraser, A.; Långström, N. Does maternal weight gain in pregnancy have long-term effects on offspring adiposity? A sibling study in a prospective cohort of 146,894 men from 136,050 families. Am. J. Clin. Nutr. 2011, 94, 142–148. [Google Scholar] [CrossRef]
- Fraser, A.; Tilling, K.; Macdonald-Wallis, C.; Sattar, N.; Brion, M.J.; Benfield, L.; Ness, A.; Deanfield, J.; Hingorani, A.; Nelson, S.M.; et al. Association of maternal weight gain in pregnancy with offspring obesity and metabolic and vascular traits in childhood. Circulation 2010, 121, 2557–2564. [Google Scholar] [CrossRef]
- Gaillard, R.; Welten, M.; Oddy, W.H.; Beilin, L.J.; Mori, T.A.; Jaddoe, V.W.V.; Huang, R.-C. Associations of maternal prepregnancy body mass index and gestational weight gain with cardio-metabolic risk factors in adolescent offspring: A prospective cohort study. BJOG 2016, 123, 207–216. [Google Scholar] [CrossRef]
- O’Brien, C.M.; Grivell, R.M.; Dodd, J.M. Systematic review of antenatal dietary and lifestyle interventions in women with a normal body mass index. Acta. Obstet. Gynecol. Scand. 2016, 95, 259–269. [Google Scholar] [CrossRef]
- Dodd, J.M.; Deussen, A.R.; Louise, J. Optimising gestational weight gain and improving maternal and infant health outcomes through antenatal dietary, lifestyle and physical activity advice: The optimise randomised controlled trial protocol. BMJ Open 2018, 8, e019583. [Google Scholar] [CrossRef] [PubMed]
- Australian Guide to Healthy Eating. Australian Guide to Healthy Eating. Available online: https://www.eatforhealth.gov.au/guidelines/australian-guide-healthy-eating (accessed on 1 January 2014).
- Dodd, J.M.; Cramp, C.; Sui, Z.; Yelland, L.N.; Deussen, A.R.; Grivell, R.M.; Moran, L.J.; Crowther, C.A.; Turnbull, D.; McPhee, A.J.; et al. The effects of antenatal dietary and lifestyle advice for women who are overweight or obese on maternal diet and physical activity: The limit randomised trial. BMC Med. 2014, 12, 161. [Google Scholar] [CrossRef] [PubMed]
- Dodd, J.M.; Turnbull, D.A.; McPhee, A.J.; Deussen, A.R.; Grivell, R.M.; Yelland, L.N.; Crowther, C.A.; Wittert, G.; Owens, J.A.; Robinson, J.S. Antenatal lifestyle advice for women who are overweight or obese: The limit randomised trial. BMJ 2014, 348, g1285. [Google Scholar] [CrossRef] [PubMed]
- Bennett, P.; Murphy, S. Psychology and Health Promotion; Open University Press: Buckingham, UK, 1997. [Google Scholar]
- SA Perinatal Practice Guidelines. Diabetes Mellitus and Gestational Diabetes. Available online: https://www.sahealth.sa.gov.au/wps/wcm/connect/146238004ee2144cb404bdd150ce4f37/Diabetes+Mellitus+and+GDM_+PPG_v5_0+%281%292.pdf?MOD=AJPERES&CACHEID=ROOTWORKSPACE-146238004ee2144cb404bdd150ce4f37-mSkq58x (accessed on 10 October 2013).
- Australian and New Zealand Neonatal Network (ANZNN). Available online: https://anznn.net/dataresources/datadictionaries (accessed on 10 October 2013).
- Sarnat, H.B.; Sarnat, M.S. Neonatal encephalopathy following fetal distress. A clinical and electroencephalographic study. Arch. Neurol. 1976, 33, 696–705. [Google Scholar] [CrossRef] [PubMed]
- Brown, M.A.; Hague, W.M.; Higgins, J.; Lowe, S.; McCowan, L.; Oats, J.; Peek, M.J.; Rowan, J.A.; Walters, B.N.; Austalasian Society of the Study of Hypertension in Pregnancy. The detection, investigation and management of hypertension in pregnancy: Full consensus statement. Aust. N. Z. J. Obstet. Gynaecol. 2000, 40, 139–155. [Google Scholar] [CrossRef]
- Willett, W.C.; Reynolds, R.D.; Cottrell-Hoehner, S.; Sampson, L.; Browne, M.L. Validation of a semi-quantitative food frequency questionnaire: Comparison with a 1-year diet record. J. Am. Diet. Assoc. 1987, 87, 43–47. [Google Scholar]
- Ibiebele, T.I.; Parekh, S.; Mallitt, K.A.; Hughes, M.C.; O’Rourke, P.K.; Webb, P.M.; Grp, A.O.C.S.; Study, A.C. Reproducibility of food and nutrient intake estimates using a semi-quantitative ffq in Australian adults. Public Health Nutr. 2009, 12, 2359–2365. [Google Scholar] [CrossRef]
- Wendel-Vos, G.C.; Schuit, A.J.; Saris, W.H.; Kromhout, D. Reproducibility and relative validity of the short questionnaire to assess health-enhancing physical activity. J. Clin. Epidemiol. 2003, 56, 1163–1169. [Google Scholar] [CrossRef]
- Ware, J.E.; Sherbourne, C.D. The mos 36 item short form health survey (sf36) conceptual framework and item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef]
- Marteau, T.M.; Bekker, H. The development of a six-item short-form of the state scale of the spielberger state-trait anxiety inventory (stai). Br. J. Clin. Psychol. 1992, 31, 301–306. [Google Scholar] [CrossRef] [PubMed]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of postnatal depression: Development of the 10 item edinburgh postnatal depression scale (edps). Brit. J. Psych. 1987, 154, 782–786. [Google Scholar] [CrossRef] [PubMed]
- Scheil, W.; Scott, J.; Catcheside, B.; Sage, L.; Kennare, R. Pregnancy Outcome in South Australia 2014; Pregnancy Outcome Unit, SA Health, Ed.; Government of South Australia: Adelaide, Australia, 2016.
- White, I.R.; Royston, P.; Wood, A.M. Multiple imputation using chained equations: Issues and guidance for practice. Stat. Med. 2011, 30, 377–399. [Google Scholar] [CrossRef] [PubMed]
- Althuizen, E.; van der Wijden, C.L.; van Mechelen, W.; Seidell, J.C.; van Poppel, M.N. The effect of a counselling intervention on weight changes during and after pregnancy: A randomised trial. BJOG 2013, 120, 92–99. [Google Scholar] [CrossRef] [PubMed]
- Asbee, S.M.; Jenkins, T.R.; Butler, J.R.; White, J.; Elliot, M.; Rutledge, A. Preventing excessive weight gain during pregnancy through dietary and lifestyle counseling a randomized controlled trial. Obstet. Gynecol. 2009, 113, 305–311. [Google Scholar] [CrossRef]
- Huang, T.T.; Yeh, C.Y.; Tsai, Y.C. A diet and physical activity intervention for preventing weight retention among taiwanese childbearing women: A randomised controlled trial. Midwifery 2011, 27, 257–264. [Google Scholar] [CrossRef]
- Hui, A.; Back, L.; Ludwig, S.; Gardiner, P.; Sevenhuysen, G.; Dean, H.; Sellers, E.; McGavock, J.; Morris, M.; Bruce, S.; et al. Lifestyle intervention on diet and exercise reduced excessive gestational weight gain in pregnant women under a randomised controlled trial. BJOG 2012, 119, 70–77. [Google Scholar] [CrossRef]
- Hui, A.L.; Back, L.; Ludwig, S.; Gardiner, P.; Sevenhuysen, G.; Dean, H.J.; Sellers, E.; McGavock, J.; Morris, M.; Jiang, D.; et al. Effects of lifestyle intervention on dietary intake, physical activity level, and gestational weight gain in pregnant women with different pre-pregnancy body mass index in a randomized control trial. BMC Pregnancy Childbirth 2014, 14, 331. [Google Scholar] [CrossRef]
- Hui, A.L.; Ludwig, S.M.; Gardiner, P.; Sevenhuysen, G.; Murray, R.; Morris, M.; Shen, G.X. Community-based exercise and dietary intervention during pregnancy: A pilot study. Can. J. Diabetes 2006, 30, 169–175. [Google Scholar] [CrossRef]
- Laitinen, K.; Poussa, T.; Isolauri, E.; Nutrition, Allergy, Mucosal Immunology and Intestinal Microbiota Group. Probiotics and dietary counselling contribute to glucose regulation during and after pregnancy: A randomised controlled trial. Br. J. Nutr. 2009, 101, 1679–1687. [Google Scholar] [CrossRef]
- Phelan, S.; Phipps, M.G.; Abrams, B.; Darroch, F.; Schaffner, A.; Wing, R.R. Randomized trial of a behavioral intervention to prevent excessive gestational weight gain: The fit for delivery study. Am. J. Clin. Nutr. 2011, 93, 772–779. [Google Scholar] [CrossRef]
- Polley, B.A.; Wing, R.R.; Sims, C.J. Randomized controlled trial to prevent excessive weight gain in pregnant women. Int. J. Obes. Relat. Metab. Disord. 2002, 26, 1494–1502. [Google Scholar] [CrossRef] [PubMed]
- Dodd, J.M.; Louise, J.; Deussen, A.R.; Grivell, R.M.; Dekker, G.; McPhee, A.J.; Hague, W. Effect of metformin in addition to dietary and lifestyle advice for pregnant women who are overweight or obese: The grow randomised, double-blind, placebo-controlled trial. Lancet. Diabetes Endocrinol. 2019, 7, 15–24. [Google Scholar] [CrossRef]
- International Weight Management in Pregnancy Collaborative Group. Effect of diet and physical activity based interventions in pregnancy on gestational weight gain and pregnancy outcomes: Meta-analysis of individual participant data from randomised trials. BMJ 2017, 358, j3119. [Google Scholar]
- Dodd, J.M. Pregnancy: Managing obesity during pregnancy-what are the options? Nat. Rev. Endocrinol. 2015, 11, 691–692. [Google Scholar] [CrossRef]
| Characteristic | Lifestyle Advice (n = 316) ** | Standard Care (n = 317) ** | Overall (n = 633) ** |
|---|---|---|---|
| Maternal age in (years) * | 31.60 (4.63) | 31.45 (4.63) | 31.53 (4.76) |
| Gestational age at entry (weeks) + | 16.21 (14.43, 18.14) | 16.29 (14.71, 18.14) | 16.29 (14.57, 18.14) |
| Body mass index at entry (kg/m2) + | 22.17 (20.81, 23.70) | 22.20 (20.90, 23.46) | 22.20 (20.87, 23.60) |
| Height at trial entry + | 165.18 (7.18) | 164.74 (7.18) | 164.96 (7.17) |
| Weight at trial entry + | 60.56 (6.92) | 60.22 (6.92) | 60.39 (6.88) |
| Public patient # | 312 (98.73) | 315 (99.37) | 627 (99.05) |
| Ethnicity # | |||
| Caucasian | 212 (67.09) | 215 (67.82) | 427 (67.46) |
| Asian | 50 (15.82) | 45 (14.20) | 95 (15.01) |
| Indian, Pakistani, Sri Lankan | 22 (6.96) | 29 (9.15) | 51 (8.06) |
| Other | 32 (10.13) | 28 (8.83) | 60 (9.47) |
| Nulliparous # | 189 (59.81) | 186 (58.68) | 375 (59.24) |
| Smoker # | 15 (4.75) | 13 (4.10) | 28 (4.42) |
| SEIFA IRSD 1 Quintile # ^ | |||
| Q1 (most disadvantaged) | 48 (15.19) | 58 (18.30) | 106 (16.75) |
| Q2 | 78 (24.68) | 93 (29.34) | 87 (13.74) |
| Q3 | 48 (15.19) | 39 (12.30) | 156 (24.64) |
| Q4 | 80 (25.32) | 76 (23.97) | 156 (24.64) |
| Q5 (least disadvantaged) | 62 (19.62) | 51 (16.09) | 113 (17.85) |
| Outcome | Lifestyle Advice (n = 316) ** | Standard Care (n = 313) ** | Unadjusted Estimate (95% CI) | Unadjusted p Value | Adjusted Estimate (95% CI) c | Adjusted p Value |
|---|---|---|---|---|---|---|
| Birthweight > 4 kg a | 24 (7.59) | 26 (8.31) | 0.91 (0.54, 1.56) | 0.739 | 0.91 (0.54, 1.55) | 0.732 |
| Birthweight (g) b | 3291.97 (586.20) | 3370.92 (511.24) | −78.96 (−164.95, 7.03) | 0.072 | −78.39 (−164.00, 7.22) | 0.073 |
| Birthweight z-score b | −0.01 (0.87) | 0.04 (0.89) | −0.05 (−0.18, 0.09) | 0.503 | −0.04 (−0.18, 0.09) | 0.532 |
| Gestational age at delivery (weeks) b | 39.12 (2.38) | 39.46 (1.63) | −0.33 (−0.65, −0.02) | 0.040 | −0.34 (−0.66, -0.02) | 0.039 |
| Large for gestational age a | 22 (6.96) | 25 (8.00) | 0.87 (0.50, 1.51) | 0.621 | 0.88 (0.51, 1.52) | 0.641 |
| Small for gestational age a | 21 (6.65) | 25 (8.01) | 0.83 (0.47, 1.45) | 0.512 | 0.84 (0.48, 1.47) | 0.545 |
| Birthweight below 2.5kg a | 20 (6.33) | 15 (4.82) | 1.31 (0.69, 2.52) | 0.411 | 1.32 (0.69, 2.54) | 0.399 |
| Birthweight > 4.5 kg d | 0 (0.00) | 2 (0.64) | 0.246 | |||
| Neonatal intensive/special care nursery admission a | 27 (8.54) | 34 (10.89) | 0.78 (0.49, 1.27) | 0.323 | 0.80 (0.50, 1.30) | 0.368 |
| Neonatal death d | 2 (0.63) | 0 (0.00) | 0.499 | |||
| Hypoglycaemia a | 10 (3.16) | 23 (7.41) | 0.43 (0.21, 0.88) | 0.022 | 0.44 (0.21, 0.91) | 0.026 |
| Hyperbilirubinaemia a | 23 (7.28) | 15 (4.80) | 1.52 (0.81, 2.85) | 0.196 | 1.53 (0.82, 2.87) | 0.181 |
| Shoulder dystocia a | 9 (2.85) | 13 (4.16) | 0.68 (0.30, 1.58) | 0.373 | 0.69 (0.30, 1.59) | 0.386 |
| Nerve palsy a, d | 0 (0.00) | 0(0.00) | -- | -- | ||
| Bone fracture a, d | 0 (0.00) | 1 (0.32) | -- | 0.497 | -- | |
| Birth trauma a, d | 1 (0.32) | 2 (0.64) | -- | 0.622 | -- |
| Outcome | Lifestyle Advice (n = 316) ** | Standard Care (n = 313) ** | Unadjusted Estimate (95% CI) | Unadjusted p Value | Adjusted Estimate (95% CI) f | Adjusted p Value |
|---|---|---|---|---|---|---|
| Healthy Eating Index b, e | <0.001 * | < 0.001 * | ||||
| Trial Entry | 72.94 (9.22) | 73.56 (7.89) | −0.62 (−1.96, 0.72) | 0.362 | −0.66 (−1.99, 0.68) | 0.334 |
| 28 Weeks | 74.35 (7.65) | 72.11 (8.21) | 2.25 (1.01, 3.48) | <0.001 | 2.21 (0.98, 3.45) | < 0.001 |
| 36 Weeks | 74.10 (8.77) | 72.50 (8.43) | 1.60 (0.25, 2.95) | 0.020 | 1.57 (0.22, 2.91) | 0.023 |
| Total Energy (kJ) b, e | 0.017 * | 0.017 * | ||||
| Trial Entry | 8917.75 (3182.65) | 8899.67 (3796.04) | 18.07 (−525.98, 562.13) | 0.948 | 20.93 (−516.71, 558.57) | 0.939 |
| 28 Weeks | 9358.47 (3782.64) | 8692.51 (2829.24) | 665.95 (141.52, 1190.38) | 0.013 | 668.81 (155.43, 1182.19) | 0.011 |
| 36 Weeks | 8809.72 (3233.50) | 8697.78 (3132.76) | 111.93 (−381.78, 605.65) | 0.657 | 114.79 (−375.44, 605.03) | 0.646 |
| Glycaemic Index b, e | 0.183 * | 0.183 * | ||||
| Trial Entry | 47.23 (4.85) | 47.54 (4.88) | −0.31 (−1.07, 0.45) | 0.427 | −0.26 (−1.01, 0.49) | 0.496 |
| 28 Weeks | 47.22 (3.70) | 48.13 (4.46) | −0.91 (−1.55, −0.27) | 0.005 | −0.86 (−1.50, −0.23) | 0.008 |
| 36 Weeks | 47.18 (4.73) | 47.79 (4.57) | −0.61 (−1.34, 0.12) | 0.099 | −0.56 (−1.28, 0.16) | 0.124 |
| Glycaemic Load b, e | 0.113 * | 0.113 * | ||||
| Trial Entry | 110.53 (48.61) | 115.02 (67.51) | −4.50 (−13.76, 4.76) | 0.341 | −4.06 (−13.15, 5.02) | 0.381 |
| 28 Weeks | 117.43 (55.86) | 114.87 (45.96) | 2.56 (−5.43, 10.54) | 0.530 | 2.99 (−4.89, 10.87) | 0.457 |
| 36 Weeks | 109.28 (46.41) | 113.87 (51.31) | -4.59 (-12.14, 2.95) | 0.233 | −4.16 (−11.62, 3.31) | 0.275 |
| Metabolic Equivalent Task Score b, e | 0.998 * | 0.998 * | ||||
| Trial Entry | 9809.81 (4176.78) | 9744.88 (4427.83) | 64.93 (−607.56, 737.42) | 0.850 | 82.27 (−581.63, 746.16) | 0.808 |
| 28 Weeks | 9085.84 (4076.53) | 9028.78 (4440.41) | 57.06 (−614.93, 729.06) | 0.868 | 74.40 (−588.00, 736.81) | 0.826 |
| 36 Weeks | 7863.59 (4848.39) | 7786.89 (4609.72) | 76.70 (−664.65, 818.05) | 0.839 | 94.04 (−637.23, 825.32) | 0.801 |
| Outcome | Lifestyle Advice (n = 316) ** | Standard Care (n = 313) ** | Unadjusted Estimate (95% CI) | Unadjusted p Value | Adjusted Estimate (95% CI) f | Adjusted p Value |
|---|---|---|---|---|---|---|
| Total Gestational Weight Gain (kg) b | 11.32 (3.96) | 11.70 (3.78) | −0.39 (−0.99, 0.21) | 0.205 | −0.37 (−0.97, 0.23) | 0.227 |
| Average Weekly Gestational Gain (kg) b | 0.57 (0.21) | 0.60 (0.21) | −0.03 (−0.06, 0.01) | 0.114 | −0.03 (−0.06, 0.01) | 0.132 |
| Institute of Medicine Category: total gestational weight gain d | 0.168 | 0.177^ | ||||
| Below | 160 (50.71) | 162 (51.68) | 0.85 (0.60, 1.21) | 0.362 | 0.85 (0.60, 1.21) | 0.366 |
| Within | 128 (40.57) | 110 (35.16) | (reference) | (reference) | ||
| Above | 28 (8.72) | 41 (13.16) | 0.57 (0.32, 1.03) | 0.062 | 0.58 (0.32, 1.04) | 0.066 |
| Institute of Medicine Category: weekly gestational weight gain d | 0.386 | 0.444^ | ||||
| Below | 61 (19.25) | 46 (14.78) | 1.40 (0.84, 2.31) | 0.196 | 1.36 (0.82, 2.26) | 0.235 |
| Within | 105 (33.12) | 111 (35.47) | (reference) | (reference) | ||
| Above | 151 (47.63) | 156 (49.75) | 1.03 (0.71, 1.48) | 0.895 | 1.02 (0.70, 1.48) | 0.916 |
| Pregnancy Hypertension a | 5 (1.58) | 4 (1.30) | 1.22 (0.33, 4.51) | 0.764 | 1.87 (0.52, 6.70) | 0.338 |
| Pre-Eclampsia/Eclampsia a | 6 (1.90) | 9 (2.91) | 0.65 (0.24, 1.81) | 0.414 | 0.70 (0.25, 1.96) | 0.502 |
| Clinical Diagnosis of Gestational Diabetes Mellitus a, † | 39 (12.43) | 39 (12.46) | 1.00 (0.64, 1.55) | 0.995 | 1.02 (0.66, 1.59) | 0.929 |
| Antenatal Hospital Admission a | 43 (13.61) | 52 (16.61) | 0.82 (0.56, 1.19) | 0.294 | 0.81 (0.56, 1.18) | 0.272 |
| Antenatal Length Stay c | 0.83 (4.18) | 0.42 (1.49) | 1.98 (1.00, 3.92) | 0.049 | 1.99 (1.03, 3.85) | 0.042 |
| Antepartum Haemorrhage a | 4 (1.27) | 7 (2.24) | 0.57 (0.17, 1.91) | 0.360 | 0.62 (0.18, 2.10) | 0.443 |
| Preterm Prelabour Ruptured Membranes a | 5 (1.58) | 4 (1.28) | 1.24 (0.34, 4.57) | 0.748 | 1.17 (0.32, 4.32) | 0.814 |
| Outcome | Lifestyle Advice (n = 316) ** | Standard Care (n = 313) ** | Unadjusted Estimate (95% CI) | Unadjusted p Value | Adjusted Estimate (95% CI) | Adjusted p Value |
|---|---|---|---|---|---|---|
| Chorioamnionitis a | 3 (0.95) | 5 (1.60) | 0.59 (0.14, 2.46) | 0.470 | 0.56 (0.14, 2.28) | 0.418 |
| Induction of Labour a | 74 (23.42) | 109 (34.96) | 0.67 (0.52, 0.86) | 0.002 | 0.66 (0.52, 0.85) | 0.001 |
| Antibiotics during Labour a | 147 (46.52) | 137 (43.75) | 1.06 (0.89, 1.26) | 0.486 | 1.04 (0.88, 1.23) | 0.629 |
| Caesarean Section a | 73 (23.17) | 74 (23.79) | 0.97 (0.73, 1.29) | 0.855 | 0.95 (0.72, 1.26) | 0.713 |
| Emergency Caesarean Section a | 41 (13.03) | 45 (14.46) | 0.90 (0.61, 1.33) | 0.603 | 0.89 (0.60, 1.31) | 0.560 |
| Preterm Birth a | 23 (7.28) | 20 (6.40) | 1.14 (0.64, 2.03) | 0.663 | 1.14 (0.64, 2.03) | 0.669 |
| Postpartum Haemorrhage a | 53 (16.84) | 45 (14.43) | 1.17 (0.81, 1.68) | 0.408 | 1.16 (0.80, 1.67) | 0.431 |
| Perineal Trauma a | 184 (58.23) | 189 (60.26) | 0.97 (0.85, 1.10) | 0.604 | 0.98 (0.86, 1.11) | 0.728 |
| 3rd/4th Degree Perineal Trauma a | 9 (2.85) | 5 (1.60) | 1.78 (0.60, 5.25) | 0.296 | 1.69 (0.57, 4.97) | 0.344 |
| Wound Infection a | 4 (1.27) | 3 (0.99) | 1.29 (0.29, 5.70) | 0.740 | 1.45 (0.33, 6.39) | 0.624 |
| Postnatal Length Stay c | 1.87 (1.47) | 1.88 (1.54) | 0.99 (0.89, 1.11) | 0.906 | 1.00 (0.89, 1.12) | 0.951 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dodd, J.M.; Deussen, A.R.; Louise, J. A Randomised Trial to Optimise Gestational Weight Gain and Improve Maternal and Infant Health Outcomes through Antenatal Dietary, Lifestyle and Exercise Advice: The OPTIMISE Randomised Trial. Nutrients 2019, 11, 2911. https://doi.org/10.3390/nu11122911
Dodd JM, Deussen AR, Louise J. A Randomised Trial to Optimise Gestational Weight Gain and Improve Maternal and Infant Health Outcomes through Antenatal Dietary, Lifestyle and Exercise Advice: The OPTIMISE Randomised Trial. Nutrients. 2019; 11(12):2911. https://doi.org/10.3390/nu11122911
Chicago/Turabian StyleDodd, Jodie M., Andrea R. Deussen, and Jennie Louise. 2019. "A Randomised Trial to Optimise Gestational Weight Gain and Improve Maternal and Infant Health Outcomes through Antenatal Dietary, Lifestyle and Exercise Advice: The OPTIMISE Randomised Trial" Nutrients 11, no. 12: 2911. https://doi.org/10.3390/nu11122911
APA StyleDodd, J. M., Deussen, A. R., & Louise, J. (2019). A Randomised Trial to Optimise Gestational Weight Gain and Improve Maternal and Infant Health Outcomes through Antenatal Dietary, Lifestyle and Exercise Advice: The OPTIMISE Randomised Trial. Nutrients, 11(12), 2911. https://doi.org/10.3390/nu11122911





