The Use of Tablet-Based Multiple-Pass 24-Hour Dietary Recall Application (MP24Diet) to Collect Dietary Intake of Children under Two Years Old in the Prospective Cohort Study in Indonesia
Abstract
1. Introduction
2. Methods
2.1. Study Context
2.2. Development of the Electronic Data Collection Tool for 24-h Dietary Recall
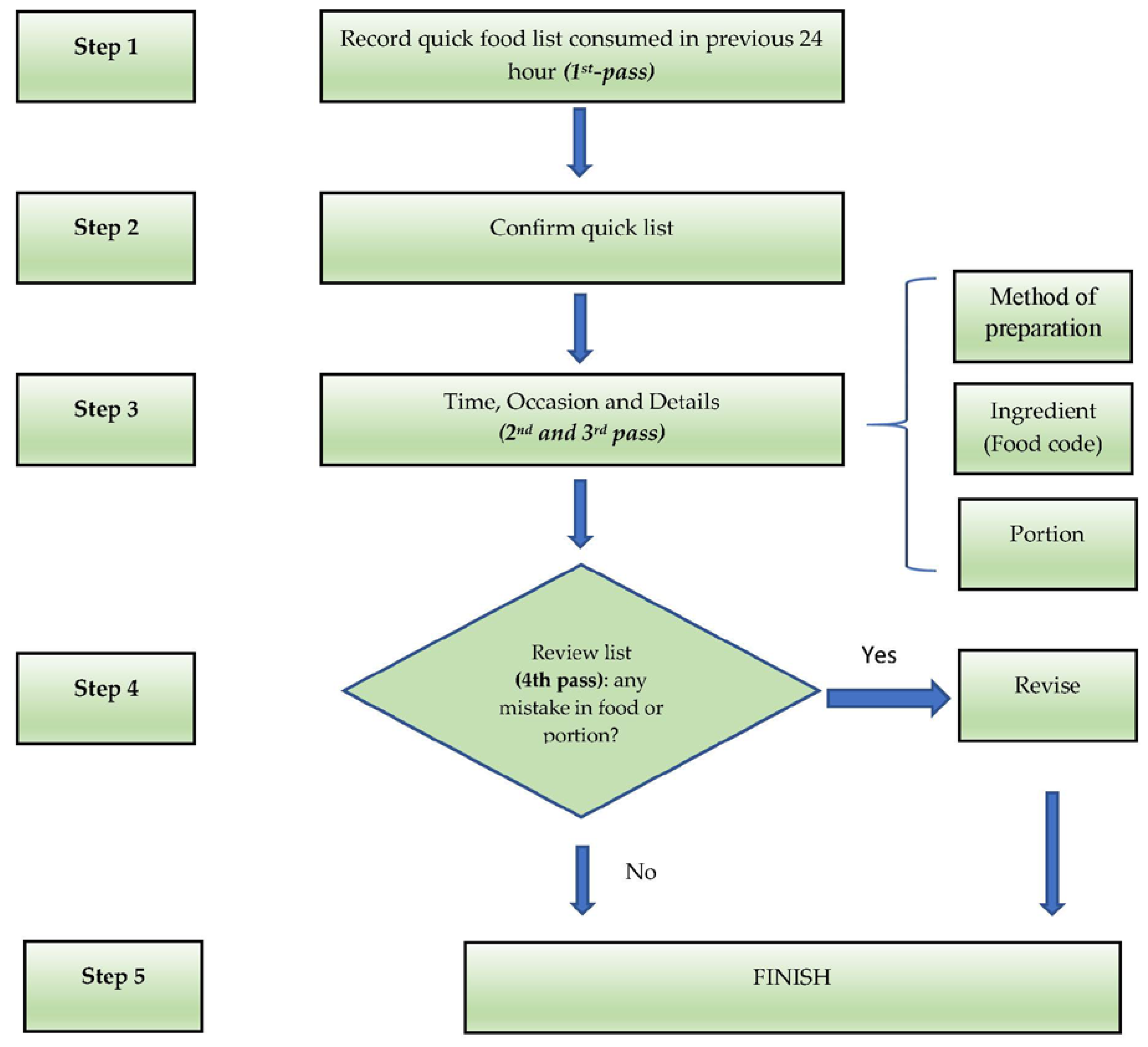
2.3. Steps in Data Collection Using the Application
2.4. Portion Size Estimation
2.5. Calculation of Energy and Nutrient Intakes
2.6. Paper-Based 24-h Dietary Recall
2.7. Realistic Energy Ranges for the Children
2.8. Training of Enumerators
2.9. Ethical Approval
2.10. Data Analysis
2.11. Statistical Analysis
3. Results
4. Discussions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Pries, A.M.; Filteau, S.; Ferguson, E.L. Snack food and beverage consumption and young child nutrition in low- and middle-income countries: A systematic review. Matern. Child Nutr. 2019, 15, e12729. [Google Scholar] [CrossRef] [PubMed]
- Style, S.; James Beard, B.; Harris-Fry, H.; Sengupta, A.; Jha, S.; Shrestha, B.P.; Rai, A.; Paudel, V.; Thondoo, M.; Pulkki-Brannstrom, A.M.; et al. Experiences in running a complex electronic data capture system using mobile phones in a large-scale population trial in southern Nepal. Glob. Health Action 2017, 10, 1330858. [Google Scholar] [CrossRef] [PubMed]
- Tomlinson, M.; Solomon, W.; Singh, Y.; Doherty, T.; Chopra, M.; Ijumba, P.; Tsai, A.C.; Jackson, D. The use of mobile phones as a data collection tool: A report from a household survey in South Africa. BMC Med. Inform. Decis. Mak. 2009, 9, 51. [Google Scholar] [CrossRef] [PubMed]
- Harris-Fry, H.; Beard, B.J.; Harrisson, T.; Paudel, P.; Shrestha, N.; Jha, S.; Shrestha, B.P.; Manandhar, D.S.; Costello, A.; Saville, N.M. Smartphone tool to collect repeated 24 h dietary recall data in Nepal. Public Health Nutr. 2018, 21, 260–272. [Google Scholar] [CrossRef] [PubMed]
- Caswell, B.L.; Talegawkar, S.A.; Dyer, B.; Siamusantu, W.; Klemm, R.D.W.; Palmer, A.C. Assessing child nutrient intakes using a tablet-based 24-hour recall tool in rural Zambia. Food Nutr. Bull. 2015, 36, 467–480. [Google Scholar] [CrossRef] [PubMed]
- Gibson, R.S.; Ferguson, E.L. An Interactive 24-Hour Recall for Assessing the Adequacy of Iron and Zinc Intakes in Developing Countries; International Life Sciences Institute: Washington, DC, USA, 2008. [Google Scholar]
- Daniel, C.R.; Kapur, K.; McAdams, M.J.; Dixit-Joshi, S.; Devasenapathy, N.; Shetty, H.; Hariharan, S.; George, P.S.; Mathew, A.; Sinha, R. Development of a field-friendly automated dietary assessment tool and nutrient database for India. Br. J. Nutr. 2014, 111, 160–171. [Google Scholar] [CrossRef] [PubMed]
- Park, M.K.; Park, J.Y.; Nicolas, G.; Paik, H.Y.; Kim, J.; Slimani, N. Adapting a standardised international 24 h dietary recall methodology (GloboDiet software) for research and dietary surveillance in Korea. Br. J. Nutr. 2015, 113, 1810–1818. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Keats, S.; Mallipu, A.; Menon, R.; Poonawala, A.; Sutrisna, A.; Tumilowicz, A. The Baduta Programme in East Java, Indonesia. Available online: https://www.gainhealth.org/resources/reports-and-publications/gain-working-paper-series-1-baduta-programme-indonesia (accessed on 22 November 2019).
- Mhila, G.; DeRenzi, B.; Mushi, C.; Wakabi, T.; Steele, M.; Dhaldialla, P.; Roos, D.; Sims, C.; Jackson, J.; Lesh, N. Using mobile applications for community-based social support for chronic patients. In Proceedings of the 6th Health Informatics in Africa Conference (HELINA), Abidjan, Cote d’Ivoire, 16–18 April 2009; Pan Africa Health Informatics Association: Abidjan, Cote d’Ivoire, 2009. [Google Scholar]
- Schakel, S.F.; Buzzard, I.M.; Gebhardt, S.E. Procedures for estimating nutrient values for food composition databases. J. Food Compos. Anal. 1997, 10, 102–114. [Google Scholar] [CrossRef]
- Dewey, K.G.; Brown, K.H. Update on technical issues concerning complementary feeding of young children in developing countries and implications for intervention programs. Food Nutr. Bull. 2003, 24, 5–28. [Google Scholar] [CrossRef] [PubMed]
- McCrory, M.A.; Hajduk, C.L.; Roberts, S.B. Procedures for screening out inaccurate reports of dietary energy intake. Public Health Nutr. 2002, 5, 873–882. [Google Scholar] [CrossRef] [PubMed]
- Fahmida, U.; Santika, O.; Kolopaking, R.; Ferguson, E. Complementary feeding recommendations based on locally available foods in Indonesia. Food Nutr. Bull. 2014, 35, S174–S179. [Google Scholar] [CrossRef] [PubMed]
- Foster, E.; Bradley, J. Methodological considerations and future insights for 24-hour dietary recall assessment in children. Nutr. Res. 2018, 51, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Archer, E.; Hand, G.A.; Blair, S.N. Validity of U.S. Nutritional surveillance: National health and nutrition examination survey caloric energy intake data, 1971–2010. PLoS ONE 2013, 8, e76632. [Google Scholar] [CrossRef] [PubMed]
- Steinfeldt, L.; Anand, J.; Murayi, T. Food reporting patterns in the USDA automated multiple-pass method. Procedia Food Sci. 2013, 2, 145–156. [Google Scholar] [CrossRef]
- Coates, J.C.; Colaiezzi, B.A.; Bell, W.; Charrondiere, U.R.; Leclercq, C. Overcoming dietary assessment challenges in low-income countries: Technological solutions proposed by the international dietary data expansion (INDDEX) project. Nutrients 2017, 9, 289. [Google Scholar] [CrossRef] [PubMed]
- Timon, C.M.; van den Barg, R.; Blain, R.J.; Kehoe, L.; Evans, K.; Walton, J.; Flynn, A.; Gibney, E.R. A review of the design and validation of web- and computer-based 24-h dietary recall tools. Nutr. Res. Rev. 2016, 29, 268–280. [Google Scholar] [CrossRef] [PubMed]
- Departemen Kesehatan Republik Indonesia, Republic of Indonesia. Laporan Hasil Riset Kesehatan Dasar Indonesia (Riskesdas) 2013; Republic of Indonesia: Jakarta, Indonesia, 2013.
- Rangan, A.M.; O’Connor, S.; Giannelli, V.; Yap, M.L.; Tang, L.M.; Roy, R.; Louie, J.C.Y.; Hebden, L.; Kay, J.; Allman-Farinelli, M. Electronic dietary intake assessment (e-DIA): Comparison of a mobile phone digital entry app for dietary data collection with 24-hour dietary recalls. JMIR mHealth uHealth 2015, 3, e98. [Google Scholar] [CrossRef] [PubMed]
- Baer, D.J.; Paul, D.R.; Rhodes, D.G.; Clemens, J.C.; Kuczynski, K.J.; Ingwersen, L.A.; Cleveland, L.E.; Sebastian, R.S.; Staples, R.C.; Murayi, T.; et al. The US department of agriculture automated multiple-pass method reduces bias in the collection of energy intakes. Am. J. Clin. Nutr. 2008, 88, 324–332. [Google Scholar] [CrossRef]
- Daelmans, B.; Ferguson, E.; Lutter, C.K.; Singh, N.; Pachón, H.; Creed-Kanashiro, H.; Woldt, M.; Mangasaryan, N.; Cheung, E.; Mir, R.; et al. Designing appropriate complementary feeding recommendations: Tools for programmatic action. Matern. Child Nutr. 2013, 9, 116–130. [Google Scholar] [CrossRef] [PubMed]
| Breastfed Infants (kcal) | Non–Breastfed Infants (kcal) | |
|---|---|---|
| 6–8 months old | 100 to 600 | 400 to 800 |
| 9–11 months old | 200 to 750 | 500 to 900 |
| 12–23 months old | 500 to 1100 | 600 to 1200 |
| Characteristics of Mother | Cohort | Cross-Sectional | p-Value 1 | ||
|---|---|---|---|---|---|
| Number | (%) | Number | (%) | ||
| Age of Mother (year) | |||||
| ≤15 | 1 | 0.1 | 2 | 0.1 | 0.006 |
| 15–19 | 58 | 8.5 | 111 | 4.0 | |
| 20–29 | 337 | 49.7 | 1298 | 47.4 | |
| 30–39 | 261 | 38.5 | 1154 | 42.1 | |
| >40 | 21 | 3.1 | 175 | 6.4 | |
| Highest Level of Education | |||||
| Never attended any school | 15 | 2.2 | 38 | 1.4 | 0.102 |
| Completed primary school | 161 | 23.7 | 479 | 17.7 | |
| Completed junior high school | 215 | 31.7 | 661 | 24.4 | |
| Completed senior high school | 238 | 35.1 | 1111 | 41.1 | |
| Academy/D1/D2/D3 | 49 | 7.2 | 415 | 15.3 | |
| Main Occupation | |||||
| Housewife | 532 | 78.5 | 2,049 | 74.8 | 0.024 |
| Government employee | 42 | 6.2 | 282 | 10.3 | |
| Entrepreneur/trader | 46 | 6.8 | 179 | 6.5 | |
| Factory labor | 34 | 5.0 | 69 | 2.5 | |
| Other | 24 | 3.5 | 161 | 5.9 | |
| Household Food Security | |||||
| Food secure | 505 | 74.5 | 2179 | 79.5 | 0.05 |
| Food insecure without hunger | 158 | 23.3 | 441 | 16.1 | |
| Food insecure with hunger | 15 | 2.2 | 120 | 4.4 | |
| Wealth Index | |||||
| Least | 140 | 20.7 | 582 | 21.5 | 0.96 |
| Second | 173 | 25.5 | 637 | 23.6 | |
| Middle | 104 | 15.3 | 420 | 15.5 | |
| Fourth | 141 | 20.8 | 605 | 22.4 | |
| Highest | 120 | 17.7 | 459 | 17.0 | |
| Intake | Age Group | Paper-Based Data Collection | Tablet-Based Data Collection | p-Value 2 | ||
|---|---|---|---|---|---|---|
| Median | (IQR) | Median | (IQR) | |||
| Energy (Kcal) | 6–8 months | 174.3 | 103.5–290.1 | 177.9 | 112–295.2 | 0.416 |
| 9–11 months | 297.7 | 185.4–444.4 | 336.0 | 207–490.7 | 0.135 | |
| 12–18 months | 481.4 | 315.6–702.4 | 555.4 | 371.1–783.3 | 0.004 | |
| Protein (g) | 6–8 months | 4.1 | 2.4–7.0 | 4.9 | 2.6–7.9 | 0.09 |
| 9–11 months | 9.0 | 4.7–13.1 | 10.2 | 5.8–15.6 | 0.146 | |
| 12–18 months | 15.2 | 9.7–23.9 | 17.0 | 10.4–24.9 | 0.185 | |
| Calcium (mg) | 6–8 months | 113.2 | 39.5–194.7 | 71.8 | 29.3–152.4 | 0.009 |
| 9–11 months | 92.7 | 42.8–217.5 | 76.6 | 39.3–132 | 0.046 | |
| 12–18 months | 141.9 | 75.8–262.5 | 124.9 | 75–241.4 | 0.409 | |
| Iron (mg) | 6–8 months | 2.1 | 1.0–3.7 | 1.6 | 1.0–3.0 | 0.23 |
| 9–11 months | 2.3 | 1.1–4.4 | 2.3 | 1.4–3.8 | 0.583 | |
| 12–18 months | 3.3 | 1.8–5.2 | 3.4 | 2.0–5.5 | 0.652 | |
| Zinc (mg) | 6–8 months | 0.9 | 0.4–1.7 | 0.9 | 0.5–1.8 | 0.524 |
| 9–11 months | 1.4 | 0.7–2.5 | 1.7 | 0.9–2.9 | 0.073 | |
| 12–18 months | 2.3 | 1.5–3.5 | 2.5 | 1.4–3.9 | 0.392 | |
| Vitamin A (retinol) | 6–8 months | 78.8 | 4.4–142.9 | 42.4 | 2.5–115.5 | 0.037 |
| 9–11 months | 39.6 | 3.4–139.8 | 25.3 | 3.9–114.8 | 0.328 | |
| 12–18 months | 96.3 | 6.9–236.1 | 77.2 | 11.2–177.9 | 0.278 | |
| Thiamine (mg) | 6–8 months | 0.1 | 0.1–0.2 | 0.1 | 0.1–0.2 | 0.736 |
| 9–11 months | 0.1 | 0.1–0.3 | 0.2 | 0.1–0.3 | 0.293 | |
| 12–18 months | 0.3 | 0.2–0.5 | 0.3 | 0.2–0.5 | 0.051 | |
| Riboflavin (mg) | 6–8 months | 0.1 | 0.1–0.3 | 0.1 | 0.1–0.2 | 0.881 |
| 9–11 months | 0.2 | 0.1–0.3 | 0.2 | 0.1–0.4 | 0.229 | |
| 12–18 months | 0.3 | 0.2–0.6 | 0.3 | 0.2–0.6 | 0.468 | |
| Niacin (mg) | 6–8 months | 1.4 | 0.9–2.5 | 1.4 | 0.8–2.2 | 0.601 |
| 9–11 months | 2.1 | 1.1–3.3 | 2.3 | 1.3–3.5 | 0.169 | |
| 12–18 months | 3.0 | 1.8–4.8 | 3.5 | 2.1–5.8 | 0.037 | |
| Vitamin B6 (mg) | 6–8 months | 0.2 | 0.1–0.4 | 0.2 | 0.1–0.4 | 0.744 |
| 9–11 months | 0.3 | 0.2–0.4 | 0.3 | 0.2–0.5 | 0.024 | |
| 12–18 months | 0.4 | 0.3–0.6 | 0.5 | 0.3–0.7 | 0.005 | |
| Vitamin B12 (mg) | 6–8 months | 0 | 0–0.2 | 0.1 | 0–0.5 | <0.001 |
| 9–11 months | 0.2 | 0–0.7 | 0.5 | 0.1–1.0 | 0.002 | |
| 12–18 months | 0.6 | 0.2–1.2 | 0.6 | 0.3–1.3 | 0.271 | |
| Folate (DFE) | 6–8 months | 11.1 | 3.2–28.9 | 18.4 | 6.1–37.8 | 0.001 |
| 9–11 months | 27.7 | 14.4–51.4 | 30.5 | 16.6–57.9 | 0.158 | |
| 12–18 months | 47 | 27.8–76.2 | 52.6 | 31.1–82.6 | 0.033 | |
| Vitamin C (mg) | 6–8 months | 12.0 | 5.0–22.0 | 9.0 | 3.4–19.6 | 0.15 |
| 9–11 months | 8.3 | 2.3–24.1 | 7.5 | 1.8–16.4 | 0.299 | |
| 12–18 months | 8.6 | 2.8–22.8 | 11.3 | 4.1–30.2 | 0.012 | |
| Age Group | Acceptable Energy Intake Reported by Paper-Based Data Collection | Acceptable Energy Intake Reported by Tablet-Based Data Collection | p-Value 2 | ||
|---|---|---|---|---|---|
| % | N | % | N | ||
| 6–8 month | 40.9 | 36 | 60.8 | 31 | 0.018 |
| 9–11 month | 56.9 | 62 | 72.4 | 42 | 0.035 |
| 12–18 month | 54.3 | 75 | 80.7 | 71 | <0.001 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Htet, M.K.; Fahmida, U.; Do, T.T.; Dibley, M.J.; Ferguson, E. The Use of Tablet-Based Multiple-Pass 24-Hour Dietary Recall Application (MP24Diet) to Collect Dietary Intake of Children under Two Years Old in the Prospective Cohort Study in Indonesia. Nutrients 2019, 11, 2889. https://doi.org/10.3390/nu11122889
Htet MK, Fahmida U, Do TT, Dibley MJ, Ferguson E. The Use of Tablet-Based Multiple-Pass 24-Hour Dietary Recall Application (MP24Diet) to Collect Dietary Intake of Children under Two Years Old in the Prospective Cohort Study in Indonesia. Nutrients. 2019; 11(12):2889. https://doi.org/10.3390/nu11122889
Chicago/Turabian StyleHtet, Min Kyaw, Umi Fahmida, Tran Thanh Do, Michael J. Dibley, and Elaine Ferguson. 2019. "The Use of Tablet-Based Multiple-Pass 24-Hour Dietary Recall Application (MP24Diet) to Collect Dietary Intake of Children under Two Years Old in the Prospective Cohort Study in Indonesia" Nutrients 11, no. 12: 2889. https://doi.org/10.3390/nu11122889
APA StyleHtet, M. K., Fahmida, U., Do, T. T., Dibley, M. J., & Ferguson, E. (2019). The Use of Tablet-Based Multiple-Pass 24-Hour Dietary Recall Application (MP24Diet) to Collect Dietary Intake of Children under Two Years Old in the Prospective Cohort Study in Indonesia. Nutrients, 11(12), 2889. https://doi.org/10.3390/nu11122889





