1. Introduction
Dietary sodium reduction is an important goal for the improvement of public health, as reduced sodium intake has been shown to decrease hypertension risk [
1]. Hypertension is a valid surrogate endpoint reflective of risks for a myriad of cardiovascular diseases, a leading source of mortality in U.S. adults [
2]. Many multifaceted policy and education initiatives aimed at reducing sodium intakes have been ongoing for decades. It has been estimated that a 40% reduction in the U.S. population’s intake of sodium over 10 years may save at least 280,000 lives [
3] and drastically reduce the number of disability-adjusted life years (DALYs). Despite ongoing public health education and policy initiatives, the preponderance of the U.S. population exceeds current recommendations for sodium intake [
4]. Among hypertensive adults, 86% exceed 2300 mg dietary sodium/day [
5].
Trends in sodium intakes have not changed over the past 10 years (five U.S. National Health and Nutrition Examination Survey (NHANES) cycles) [
6]. Those with the lowest household education, non-Hispanic black race/Hispanic origin, and lowest income have seen the largest increase in sodium intakes derived from snack foods from 1977–1978 to 2011–2014 [
7]. Sodium is primarily consumed as sodium chloride (NaCl) and the majority of intake is derived from sodium added during food processing for the purposes of providing flavor or food safety properties. NaCl may also be used as a processing aide. More than 70% of sodium intake in the United States comes from commercially processed and restaurant foods and no single category comprises >7% of total intake [
8]. With the exception of milk, which naturally contains sodium, the top ten food categories contributing sodium to the diet of U.S. school-aged children are composed of foods in which sodium is added during processing or preparation [
9]. Yeast breads contribute the most sodium to the U.S. diet (for individuals aged ≥2 years) [
8].
Sodium reduction poses technical challenges given its role in the palatability and safety of food (e.g., preventing bacterial growth and spoilage) [
10]. When salt is reduced, palatability and consumer acceptance of a product generally tends to decrease. In 2016, the U.S. Food and Drug Administration (FDA) published draft guidance on voluntary sodium reduction goals for public comment with an aim to reduce U.S. daily intake from 3400 mg to 3000 mg within 2 years (short-term goal) and to 2300 mg within 10 years (long-term goal) [
11]. This gradual process set reduction targets for >150 food categories.
Currently, no perfectly viable alternative for replacing sodium exists in the contemporary food marketplace, although several innovations do exist among various product categories. For example, glutamate, a nonessential amino acid, has been used to enhance the taste and palatability of food. Indeed, the 2010 Institute of Medicine (now the Institute of Medicine) report,
Strategies to Reduce Sodium Intake in the United States, emphasizes that achieving lower intakes of excessive sodium should be a critical focus for all Americans and it is possible to use monosodium glutamate (MSG), the most common glutamate salt and flavor enhancer, to lower the overall sodium level in certain foods while maintaining palatability [
10]. MSG contains about 12% sodium, which is less than one-third of that contained in table salt (39%) [
12]. There is an appropriate amount of MSG that can be used to replace salt while maintaining consumer acceptance in food [
12]. Excess MSG does not promote umami taste, and to the contrary, may negatively impact the taste profile of food, most notably at levels >1% [
13]. Although MSG is the most widely used flavor enhancer in food, other effective glutamate salts, such as calcium di-glutamate, exist but do not provide as pronounced of an effect. A considerable number of studies have demonstrated that various forms of glutamate can help reduce the amount of sodium in specific foods, including soups, prepared dishes, processed meat, and dairy products, by enhancing palatability [
14,
15,
16,
17,
18,
19,
20,
21]. However, much less is known about how glutamate substitution would affect sodium intakes at the population level across a range of different foods. Therefore, the purpose of this study was to first estimate contemporary sodium intakes of the U.S. population, and then to model MSG substitution in select products—with substantial supportive literature to ensure feasibility—to estimate potential population-level reductions in sodium intakes.
3. Results
3.1. Current Mean Sodium Intakes, Percentages above the CDRR, and Percentages above the UL
Overall, sodium intakes among the general U.S. population are higher than federal recommendations. On the basis of NHANES 2013–2016 data, Americans (aged >1 year) consume approximately 3361 mg sodium/day on average (
Table 3). Mean daily sodium intake from foods and beverages among the U.S. population was 2906 mg/day for children (aged 1–18 years) and 3499 mg/day for adults (aged ≥19 years).
Regardless of age, men had higher sodium intakes than women. Specifically, among adults (≥19 years), men typically consumed approximately 4067 mg sodium/day, whereas women only consumed approximately 2956 mg sodium/day. Similar themes were apparent among children (1–18 years); boys had higher mean sodium intakes than girls (3268 versus 2673 mg/day, respectively). Therefore, women of all ages were less likely to exceed the CDRR and UL compared to men.
Across age subgroups, sodium intake was highest among men and women aged 19–30 years (4431 versus 3138 mg/day, respectively) and varied across the life course. For men, sodium intake increased with age in the adolescent years (1–18 years), plateaued among early adulthood (19–30 years), and then decreased through the remainder of adulthood (≥31 years). However, slightly different patterns were observed among women. Whereas sodium intakes among young girls increased with age until 9–13 years, a slight decrease in intake was observed between the ages of 14–18 years, followed by an increase in intake from 19–30 years, and lastly, a final decrease in intake for the remainder of adulthood (≥31 years). Older adults (≥71 years) had the lowest sodium intakes of all adult participants among both men and women. Thus, younger adults were more likely to exceed the CDRR and UL for sodium compared to their older adult (≥71 years) counterparts. Among children, boys and girls in the 4–8-year and 9–13-year life stages had the highest prevalence of exceeding the CDRR and UL.
Estimated mean sodium intake and the percent-wise contributions for selected food categories to total sodium intake in the diets of U.S adults (≥19 years) and children (1–18 years) are presented in
Table 4 and
Table 5. On a population level, no individual food group contributes large amounts of sodium to the diet; sodium intakes appear to be widespread throughout the food supply. However, the savory food groups represented in
Table 4 and
Table 5 provide much larger proportions of sodium to the diets of those who consumed these products (i.e., “consumers”). For example, meat-based frozen meals provide 0.3% of the sodium present in the diets of all U.S adults, but as much as one-third (32%) among consumers. Among children, the top three contributors to total sodium intakes are crackers and salty snacks, cured meats, and select cheeses (
Table 5). Although intakes of these select food categories remain high overall, intakes among consumers of these categories are significantly higher than the general population of U.S. children (
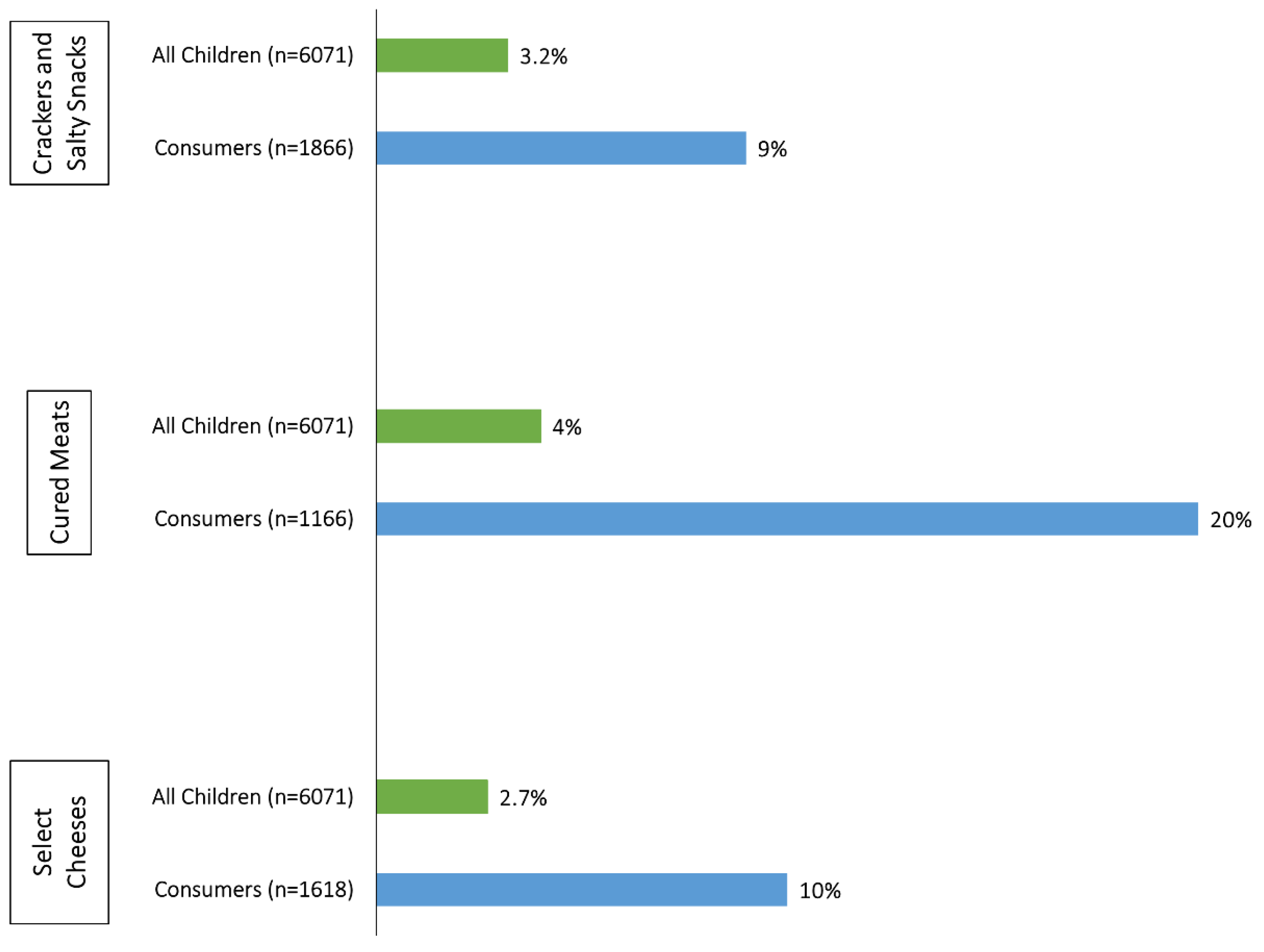
Figure 1). For cured meats in particular, children who consume these products receive 20% of their usual sodium intake from this source, whereas cured meats account for only 4% of total sodium intakes among the general population of U.S. children.
3.2. Models of the Effects of Gutamates on Mean Usual Sodium Intakes, Percentages above the CDRR, and Percentages above the UL
Universal incorporation of glutamates into the select savory food groups (presented in
Table 2) would result in a 3% (162 mg/day) reduction in overall sodium intakes in the U.S. population (aged ≥ 1 year) and a 7–8 percentage point reduction among consumers of one or more food categories in which sodium chloride could be substituted for by glutamates. Among U.S. children specifically, glutamates have the potential to reduce the proportion of the population exceeding the UL for sodium by 5 percentage points (
Table 3) and to reduce consumer intakes by 211–263 mg/day among boys and girls. Likewise, glutamates could reduce the sodium intakes of consumers by 321 and 236 mg/day in adult men and women, respectively (
Table 6 and
Table 7).
4. Discussion
Dietary factors are among the top contributors to chronic disease risk and DALYs in the United States. High intake of sodium is one risk factor that has been identified as a contributor to this burden [
33]. According to our analysis, current estimates of mean usual sodium intake remain high across all age and sex subgroups of the U.S. population, and they continue to exceed authoritative recommendations, consistent with previous reports [
4,
6]. Contrary to prior reports [
6], age-related differences in estimated usual intakes did not appear to be more pronounced in men than women (
Table 3). Our analyses provide unique data on the diets of consumers of select food categories. Although reducing the amount of sodium among certain food groups may show modest effects on intakes across the population, it may have a large effect on individuals who consume these types of products. For example, about 18.7% of U.S. adults consume cured meats on any given day; reducing sodium intake of cured meat products by 40% would have a large impact on those consumers, since cured meats account for 21% of their total sodium intake from the diet.
Figure 1 illustrates substantial effects of incorporating glutamates into crackers and salty snacks, cured meats, and select cheeses on U.S. children (1–18 years). Given current sources of sodium in the diets of young children, glutamate’s use in these select categories may have the greatest impact on sodium intakes in this age group. Meat-based frozen meals, vegetable and meat-based soups, and cured meats contain the highest amounts of sodium; however, grain products were previously shown to be the largest contributor of sodium intakes to the U.S. diet because they are more ubiquitously consumed [
6]. Consumer sentiment around MSG has deterred many consumer-packaged food companies from utilizing it to reduce sodium intake in products [
34].
Several other strategies have been applied to reduce the population’s sodium intake. Gradual reduction through a cumulative series of small decreases over 6 weeks was shown to be effective in reducing the sodium content of white bread by about 25% without altering palatability. However, reduction would need to be applied to all breads on the market to go unnoticed by consumers [
35]. Potassium chloride (KCl), calcium chloride (CaCl
2), and magnesium sulfate (MgSO
4) have been used as substitutes for table salt; however, their bitter taste has limited their use and uptake by consumers [
36]. Citric acid in tomato soup [
37] and lactic acid in bread [
38] have the potential to enhance saltiness and be useful in reducing sodium intake. SODA-LO, a new but more costly sodium-reduction ingredient that can reduce sodium in certain applications through its technology that turns standard salt crystals into free-flowing, hollow salt microspheres, has been shown to deliver taste and function by maximizing surface area in products such as potato chips and baked goods [
6].
Current intake above public health recommendations is not solely a United States-centric issue, but a global pandemic demonstrated by high intakes of sodium in other countries [
39]. Assuming the accuracy of NHANES and other international databases, ongoing public health education initiatives show no signs of success in decreasing intakes. Frequent use of nutrition labels appears to be associated with lower consumption of sodium and high-sodium foods; however, while surveys suggest that consumers may wish to reduce their sodium intake, it is likely not a priority in what most consumers choose to eat [
40]. In fact, evidence indicates that many consumers avoid products labeled as “low sodium” [
40]. Reducing intakes through food science and technological advances seems appropriate, in order to make the most impactful reductions in the consumption of sodium at the population level.
Our study has some strengths and limitations to consider. First, the strengths of our analysis are that the models applied to examine usual intakes adjusted for the effects of within-person variation measurement error, and that NHANES is a large nationally representative sample that allows for the estimation of usual intakes of sodium at the population level. However, the limitations of our study should also be noted. This modeling study used conservative assumptions of sodium reduction by substituting glutamates for sodium chloride in several What We Eat in America food categories. We chose these conservative reduction values, presented in
Table 2, upon consultation with food scientists, with the hopes of accounting for what is already contained in the food supply so as not to overestimate the total effect of glutamates. Restaurant foods supply a large portion of sodium to the U.S. diet [
40]; however, we chose to not model inclusion of glutamates into restaurant foods, since many of these flavor enhancers are already in widespread use in restaurants. Therefore, the effect of glutamates could be greater than what is presented in our study. NHANES also has several limitations, including the reliance on self-reported dietary intake data and assumptions of USDA reference database accuracy for estimating sodium intakes across the population. Self-reported dietary data are prone to systematic errors, such as energy underreporting. Additionally, we cannot completely rule out the potential for self-selection bias; that is, people who participate in nutrition- and health-related research tend to differ by sociodemographic factors and may have been more interested in participating in NHANES [
41]. Finally, in order to fully maximize the effectiveness of sodium reduction, the acceptability of MSG among consumers must be taken into consideration [
42,
43].