Timing of Breakfast, Lunch, and Dinner. Effects on Obesity and Metabolic Risk
Abstract
1. Introduction
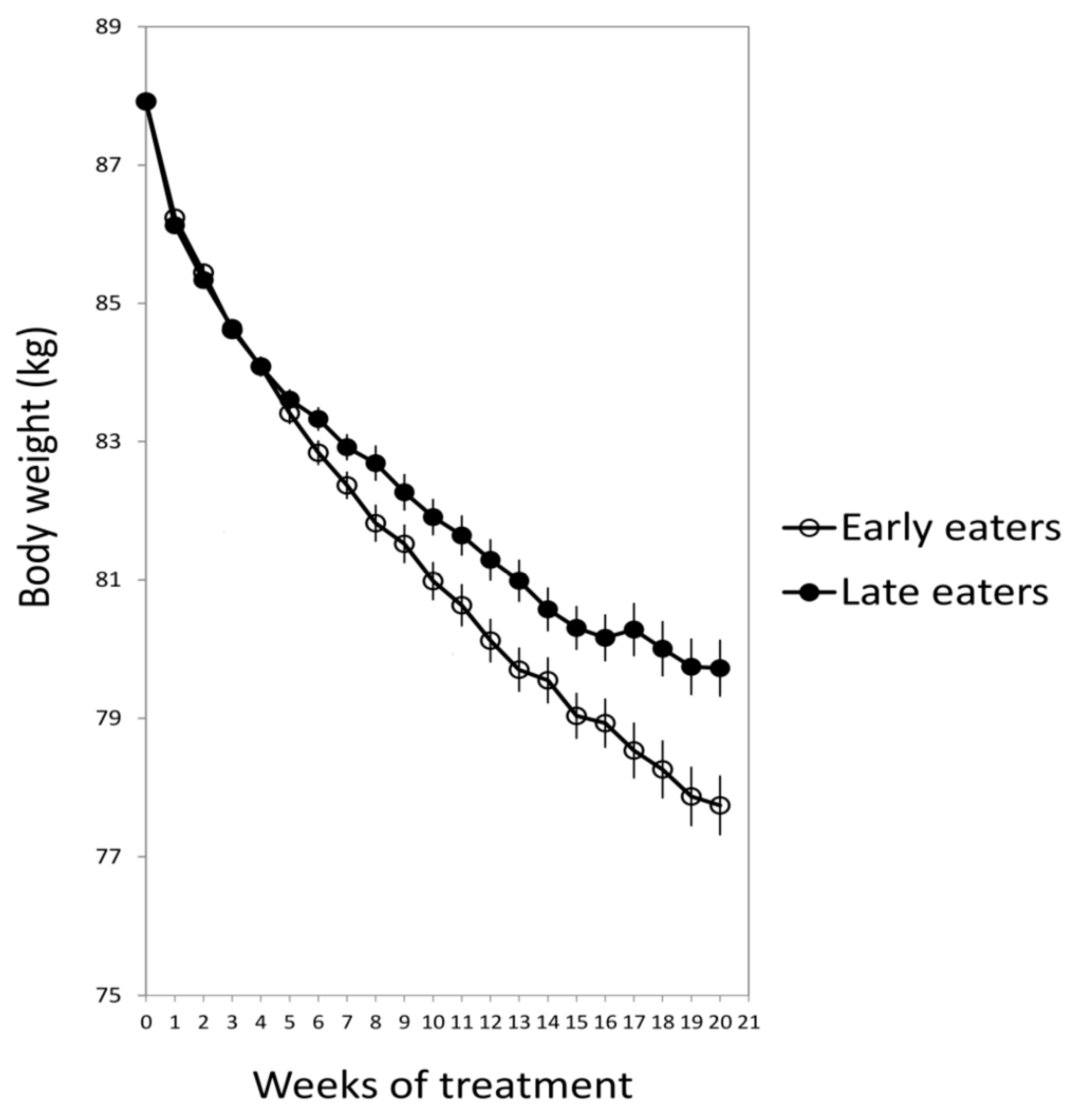
2. Lunch Timing Affects Weight Loss Effectiveness
3. How Does the Timing of Food Intake Affect Metabolism?
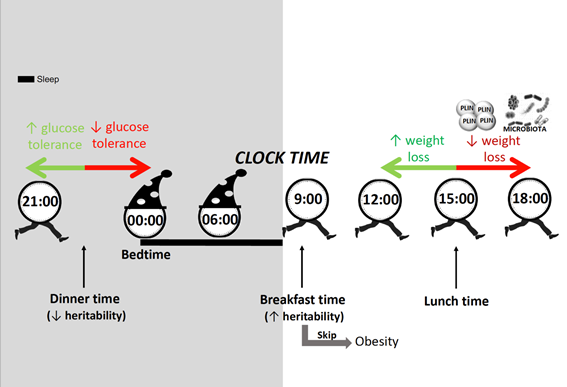
4. Timing of Food Intake Does Affect Everyone or it Depends on Genetics?
5. Late Dinner
5.1. Melatonin and Late Eating
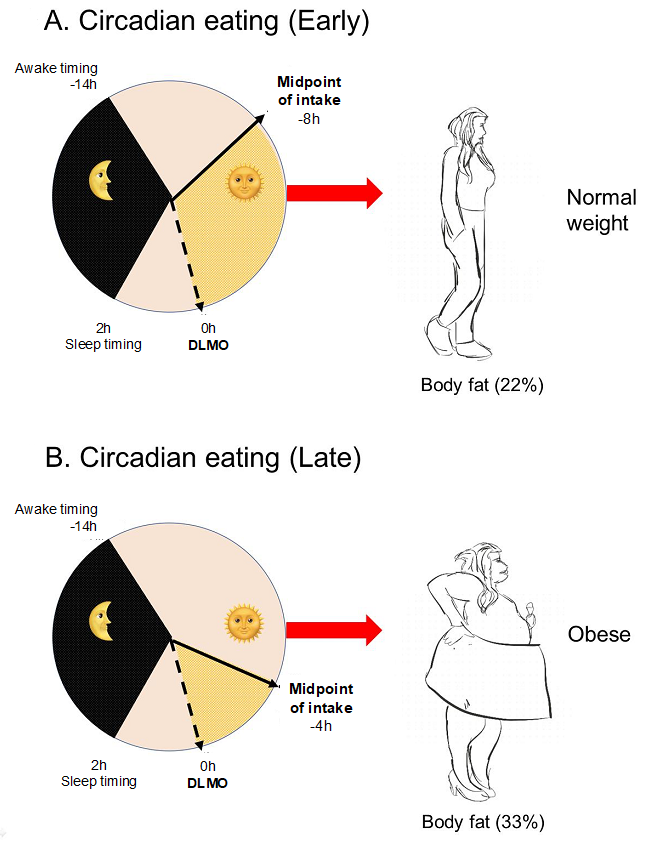
5.2. “Circadian” Timing of Food Intake Versus “Clock” Timing
6. Breakfast
Contradictory Results in Breakfast Skipping and Weight Loss
7. Summary
Author Contributions
Funding
Conflicts of Interest
References
- Marquez-Ibanez, B.; Armendariz-Anguiano, A.L.; Bacardi-Gascon, M.; Jimenez-Cruz, A. Review of controled clinical trials of behavioral treatment for obesity. Nutr. Hosp. 2008, 23, 1–5. [Google Scholar] [PubMed]
- Council on Scientific Affairs. Treatment of obesity in adults. JAMA 1988, 260, 2547–2551. [Google Scholar] [CrossRef]
- Kassirer, J.P.; Angell, M. Losing weight—An ill-fated New Year’s resolution. N. Engl. J. Med. 1998, 338, 52–54. [Google Scholar] [CrossRef] [PubMed]
- Kramer, F.M.; Jeffery, R.W.; Forster, J.L.; Snell, M.K. Long-term follow-up of behavioral treatment for obesity: Patterns of weight regain among men and women. Int. J. Obes. 1989, 13, 123–136. [Google Scholar] [PubMed]
- Bandin, C.; Martinez-Nicolas, A.; Ordovas, J.M.; Madrid, J.A.; Garaulet, M. Circadian rhythmicity as a predictor of weight-loss effectiveness. Int. J. Obes. 2014, 38, 1083. [Google Scholar] [CrossRef] [PubMed]
- Corbalan, M.D.; Morales, E.M.; Canteras, M.; Espallardo, A.; Hernandez, T.; Garaulet, M. Effectiveness of cognitive-behavioral therapy based on the Mediterranean diet for the treatment of obesity. Nutrition 2009, 25, 861–869. [Google Scholar] [CrossRef]
- Dansinger, M.L.; Gleason, J.A.; Griffith, J.L.; Selker, H.P.; Schaefer, E.J. Comparison of the Atkins, Ornish, Weight Watchers, and Zone diets for weight loss and heart disease risk reduction: A randomized trial. JAMA 2005, 293, 43–53. [Google Scholar] [CrossRef]
- Anderson, J.W.; Konz, E.C.; Frederich, R.C.; Wood, C.L. Long-term weight-loss maintenance: A meta-analysis of US studies. Am. J. Clin. Nutr. 2001, 74, 579–584. [Google Scholar] [CrossRef]
- Garaulet, M.; Gomez-Abellan, P. Timing of food intake and obesity: A novel association. Physiol. Behav. 2014, 134, 44–50. [Google Scholar] [CrossRef]
- Jakubowicz, D.; Barnea, M.; Wainstein, J.; Froy, O. High Caloric intake at breakfast vs. dinner differentially influences weight loss of overweight and obese women. Obesity 2013, 21, 2504–2512. [Google Scholar] [CrossRef]
- Bandin, C.; Scheer, F.A.; Luque, A.J.; Avila-Gandia, V.; Zamora, S.; Madrid, J.A.; Gomez-Abellan, P.; Garaulet, M. Meal timing affects glucose tolerance, substrate oxidation and circadian-related variables: A randomized, crossover trial. Int. J. Obes. 2015, 39, 828–833. [Google Scholar] [CrossRef] [PubMed]
- Garaulet, M.; Corbalan, M.D.; Madrid, J.A.; Morales, E.; Baraza, J.C.; Lee, Y.C.; Ordovas, J.M. CLOCK gene is implicated in weight reduction in obese patients participating in a dietary programme based on the Mediterranean diet. Int. J. Obes. 2010, 34, 516–523. [Google Scholar] [CrossRef] [PubMed]
- Garaulet, M.; Esteban Tardido, A.; Lee, Y.C.; Smith, C.E.; Parnell, L.D.; Ordovas, J.M. SIRT1 and CLOCK 3111T>C combined genotype is associated with evening preference and weight loss resistance in a behavioral therapy treatment for obesity. Int. J. Obes. 2012, 36, 1436. [Google Scholar] [CrossRef] [PubMed]
- Garaulet, M.; Corbalan-Tutau, M.D.; Madrid, J.A.; Baraza, J.C.; Parnell, L.D.; Lee, Y.C.; Ordovas, J.M. PERIOD2 variants are associated with abdominal obesity, psycho-behavioral factors, and attrition in the dietary treatment of obesity. J. Am. Diet. Assoc. 2010, 110, 917–921. [Google Scholar] [CrossRef] [PubMed]
- Garaulet, M.; Gomez-Abellan, P.; Alburquerque-Bejar, J.J.; Lee, Y.C.; Ordovas, J.M.; Scheer, F.A. Timing of food intake predicts weight loss effectiveness. Int. J. Obes. 2013, 37, 604–611. [Google Scholar] [CrossRef]
- Turek, F.W.; Joshu, C.; Kohsaka, A.; Lin, E.; Ivanova, G.; McDearmon, E.; Laposky, A.; Losee-Olson, S.; Easton, A.; Jensen, D.R.; et al. Obesity and metabolic syndrome in circadian Clock mutant mice. Science 2005, 308, 1043–1045. [Google Scholar] [CrossRef]
- Randler, C. Differences between smokers and nonsmokers in morningness-eveningness. Soc. Behav. Personal. 2008, 36, 673–680. [Google Scholar] [CrossRef]
- Collado, M.C.; Engen, P.A.; Bandin, C.; Cabrera-Rubio, R.; Voigt, R.M.; Green, S.J.; Naqib, A.; Keshavarzian, A.; Scheer, F.; Garaulet, M. Timing of food intake impacts daily rhythms of human salivary microbiota: A randomized, crossover study. FASEB J. 2018, 32, 2060–2072. [Google Scholar] [CrossRef]
- Garaulet, M.; Vera, B.; Bonnet-Rubio, G.; Gomez-Abellan, P.; Lee, Y.C.; Ordovas, J.M. Lunch eating predicts weight-loss effectiveness in carriers of the common allele at PERILIPIN1: The ONTIME (Obesity, Nutrigenetics, Timing, Mediterranean) study. Am. J. Clin. Nutr. 2016, 104, 1160–1166. [Google Scholar] [CrossRef]
- Xiao, Q.; Garaulet, M.; Scheer, F. Meal timing and obesity: Interactions with macronutrient intake and chronotype. Int. J. Obes. 2019, 43, 1701–1711. [Google Scholar] [CrossRef]
- Yoshida, J.; Eguchi, E.; Nagaoka, K.; Ito, T.; Ogino, K. Association of night eating habits with metabolic syndrome and its components: A longitudinal study. BMC Public Health 2018, 18, 1366. [Google Scholar] [CrossRef] [PubMed]
- Kutsuma, A.; Nakajima, K.; Suwa, K. Potential Association between Breakfast Skipping and Concomitant Late-Night-Dinner Eating with Metabolic Syndrome and Proteinuria in the Japanese Population. Scientifica (Cairo) 2014, 2014, 253581. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.J.; Chuang, S.Y.; Chang, H.Y.; Pan, W.H. Energy intake at different times of the day: Its association with elevated total and LDL cholesterol levels. Nutr. Metab. Cardiovasc. Dis. 2019, 29, 390–397. [Google Scholar] [CrossRef] [PubMed]
- Nakajima, K.; Suwa, K. Association of hyperglycemia in a general Japanese population with late-night-dinner eating alone, but not breakfast skipping alone. J. Diabetes Metab. Disord. 2015, 14, 16. [Google Scholar] [CrossRef] [PubMed]
- Morgan, L.M.; Shi, J.W.; Hampton, S.M.; Frost, G. Effect of meal timing and glycaemic index on glucose control and insulin secretion in healthy volunteers. Br. J. Nutr. 2012, 108, 1286–1291. [Google Scholar] [CrossRef]
- Morris, C.J.; Yang, J.N.; Garcia, J.I.; Myers, S.; Bozzi, I.; Wang, W.; Buxton, O.M.; Shea, S.A.; Scheer, F.A. Endogenous circadian system and circadian misalignment impact glucose tolerance via separate mechanisms in humans. Proc. Natl. Acad. Sci. USA 2015, 112, E2225–E2234. [Google Scholar] [CrossRef]
- Lopez-Minguez, J.; Saxena, R.; Bandin, C.; Scheer, F.A.; Garaulet, M. Late dinner impairs glucose tolerance in MTNR1B risk allele carriers: A randomized, cross-over study. Clin. Nutr. 2018, 37, 1133–1140. [Google Scholar] [CrossRef]
- Uzhova, I.; Fuster, V.; Fernandez-Ortiz, A.; Ordovas, J.M.; Sanz, J.; Fernandez-Friera, L.; Lopez-Melgar, B.; Mendiguren, J.M.; Ibanez, B.; Bueno, H.; et al. The Importance of Breakfast in Atherosclerosis Disease: Insights from the PESA Study. J. Am. Coll. Cardiol. 2017, 70, 1833–1842. [Google Scholar] [CrossRef]
- Smith, K.J.; Gall, S.L.; McNaughton, S.A.; Blizzard, L.; Dwyer, T.; Venn, A.J. Skipping breakfast: Longitudinal associations with cardiometabolic risk factors in the Childhood Determinants of Adult Health Study. Am. J. Clin. Nutr. 2010, 92, 1316–1325. [Google Scholar] [CrossRef]
- Timlin, M.T.; Pereira, M.A. Breakfast frequency and quality in the etiology of adult obesity and chronic diseases. Nutr. Rev. 2007, 65, 268–281. [Google Scholar] [CrossRef]
- Gill, S.; Panda, S. A Smartphone App Reveals Erratic Diurnal Eating Patterns in Humans that Can Be Modulated for Health Benefits. Cell Metab. 2015, 22, 789–798. [Google Scholar] [CrossRef] [PubMed]
- De Castro, J.M. The time of day of food intake influences overall intake in humans. J. Nutr. 2004, 134, 104–111. [Google Scholar] [CrossRef] [PubMed]
- Archer, E. The childhood obesity epidemic as a result of nongenetic evolution: The maternal resources hypothesis. Mayo Clin. Proc. 2015, 90, 77–92. [Google Scholar] [CrossRef] [PubMed]
- Mekary, R.A.; Giovannucci, E.; Willett, W.C.; van Dam, R.M.; Hu, F.B. Eating patterns and type 2 diabetes risk in men: Breakfast omission, eating frequency, and snacking. Am. J. Clin. Nutr. 2012, 95, 1182–1189. [Google Scholar] [CrossRef]
- Sievert, K.; Hussain, S.M.; Page, M.J.; Wang, Y.; Hughes, H.J.; Malek, M.; Cicuttini, F.M. Effect of breakfast on weight and energy intake: Systematic review and meta-analysis of randomised controlled trials. BMJ 2019, 364, 142. [Google Scholar] [CrossRef]
- Lopez-Minguez, J.; Dashti, H.S.; Madrid-Valero, J.J.; Madrid, J.A.; Saxena, R.; Scheer, F.; Ordonana, J.R.; Garaulet, M. Heritability of the timing of food intake. Clin. Nutr. 2019, 38, 767–773. [Google Scholar] [CrossRef]
- Kant, A.K.; Graubard, B.I. Within-person comparison of eating behaviors, time of eating, and dietary intake on days with and without breakfast: NHANES 2005–2010. Am. J. Clin. Nutr. 2015, 102, 661–670. [Google Scholar] [CrossRef]
- Ruiz-Lozano, T.; Vidal, J.; de Hollanda, A.; Scheer, F.A.; Garaulet, M.; Izquierdo-Pulido, M. Timing of food intake is associated with weight loss evolution in severe obese patients after bariatric surgery. Clin. Nutr. 2016, 35, 1308–1314. [Google Scholar] [CrossRef]
- Archer, E.; Pavela, G.; McDonald, S.; Lavie, C.J.; Hill, J.O. Cell-Specific “Competition for Calories” Drives Asymmetric Nutrient-Energy Partitioning, Obesity, and Metabolic Diseases in Human and Non-human Animals. Front. Physiol. 2018, 9, 1053. [Google Scholar] [CrossRef]
- Corbalan-Tutau, M.D.; Madrid, J.A.; Ordovas, J.M.; Smith, C.E.; Nicolas, F.; Garaulet, M. Differences in daily rhythms of wrist temperature between obese and normal-weight women: Associations with metabolic syndrome features. Chronobiol. Int. 2011, 28, 425–433. [Google Scholar] [CrossRef]
- Gevers, D.; Kugathasan, S.; Denson, L.A.; Vazquez-Baeza, Y.; Van Treuren, W.; Ren, B.; Schwager, E.; Knights, D.; Song, S.J.; Yassour, M.; et al. The treatment-naive microbiome in new-onset Crohn’s disease. Cell Host Microbe 2014, 15, 382–392. [Google Scholar] [CrossRef] [PubMed]
- Harley, I.T.; Karp, C.L. Obesity and the gut microbiome: Striving for causality. Mol. Metab. 2012, 1, 21–31. [Google Scholar] [CrossRef] [PubMed]
- Berg, C.; Lappas, G.; Wolk, A.; Strandhagen, E.; Toren, K.; Rosengren, A.; Thelle, D.; Lissner, L. Eating patterns and portion size associated with obesity in a Swedish population. Appetite 2009, 52, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Mattson, M.P.; Allison, D.B.; Fontana, L.; Harvie, M.; Longo, V.D.; Malaisse, W.J.; Mosley, M.; Notterpek, L.; Ravussin, E.; Scheer, F.A.; et al. Meal frequency and timing in health and disease. Proc. Natl. Acad. Sci. USA 2014, 111, 16647–16653. [Google Scholar] [CrossRef] [PubMed]
- Scheer, F.A.; Hilton, M.F.; Mantzoros, C.S.; Shea, S.A. Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc. Natl. Acad. Sci. USA 2009, 106, 4453–4458. [Google Scholar] [CrossRef] [PubMed]
- Rubio-Sastre, P.; Scheer, F.A.; Gomez-Abellan, P.; Madrid, J.A.; Garaulet, M. Acute melatonin administration in humans impairs glucose tolerance in both the morning and evening. Sleep 2014, 37, 1715–1719. [Google Scholar] [CrossRef]
- Gabel, V.; Reichert, C.F.; Maire, M.; Schmidt, C.; Schlangen, L.J.; Kolodyazhniy, V.; Garbazza, C.; Cajochen, C.; Viola, A.U. Differential impact in young and older individuals of blue-enriched white light on circadian physiology and alertness during sustained wakefulness. Sci. Rep. 2017, 7, 7620. [Google Scholar] [CrossRef]
- Kim, J.Y.; Coletta, D.K.; Mandarino, L.J.; Shaibi, G.Q. Glucose response curve and type 2 diabetes risk in Latino adolescents. Diabetes Care 2012, 35, 1925–1930. [Google Scholar] [CrossRef]
- Tuomi, T.; Nagorny, C.L.F.; Singh, P.; Bennet, H.; Yu, Q.; Alenkvist, I.; Isomaa, B.; Ostman, B.; Soderstrom, J.; Pesonen, A.K.; et al. Increased Melatonin Signaling Is a Risk Factor for Type 2 Diabetes. Cell Metab. 2016, 23, 1067–1077. [Google Scholar] [CrossRef]
- DIAbetes Genetics Replication; Meta-Analysis Consortium; Asian Genetic Epidemiology Network Type 2 Diabetes Consortium; South Asian Type 2 Diabetes Consortium; Mexican American Type 2 Diabetes Consortium; Type 2 Diabetes Genetic Exploration by Nex-Generation Sequencing in Muylti-Ethnic Samples Consortium; Mahajan, A.; Go, M.J.; Zhang, W.; Below, J.E.; et al. Genome-wide trans-ancestry meta-analysis provides insight into the genetic architecture of type 2 diabetes susceptibility. Nat. Genet. 2014, 46, 234–244. [Google Scholar] [CrossRef]
- Jonsson, A.; Ladenvall, C.; Ahluwalia, T.S.; Kravic, J.; Krus, U.; Taneera, J.; Isomaa, B.; Tuomi, T.; Renstrom, E.; Groop, L.; et al. Effects of common genetic variants associated with type 2 diabetes and glycemic traits on alpha- and beta-cell function and insulin action in humans. Diabetes 2013, 62, 2978–2983. [Google Scholar] [CrossRef] [PubMed]
- Keijzer, H.; Smits, M.G.; Duffy, J.F.; Curfs, L.M. Why the dim light melatonin onset (DLMO) should be measured before treatment of patients with circadian rhythm sleep disorders. Sleep Med. Rev. 2014, 18, 333–339. [Google Scholar] [CrossRef] [PubMed]
- McHill, A.W.; Phillips, A.J.; Czeisler, C.A.; Keating, L.; Yee, K.; Barger, L.K.; Garaulet, M.; Scheer, F.A.; Klerman, E.B. Later circadian timing of food intake is associated with increased body fat. Am. J. Clin. Nutr. 2017, 106, 1213–1219. [Google Scholar] [CrossRef] [PubMed]
- Vera, B.; Dashti, H.S.; Gomez-Abellan, P.; Hernandez-Martinez, A.M.; Esteban, A.; Scheer, F.; Saxena, R.; Garaulet, M. Modifiable lifestyle behaviors, but not a genetic risk score, associate with metabolic syndrome in evening chronotypes. Sci. Rep. 2018, 8, 945. [Google Scholar] [CrossRef]
- Pan, A.; Schernhammer, E.S.; Sun, Q.; Hu, F.B. Rotating night shift work and risk of type 2 diabetes: Two prospective cohort studies in women. PLoS Med. 2011, 8, e1001141. [Google Scholar] [CrossRef]
- Cain, S.W.; Filtness, A.J.; Phillips, C.L.; Anderson, C. Enhanced preference for high-fat foods following a simulated night shift. Scand. J. Work Environ. Health 2015, 41, 288–293. [Google Scholar] [CrossRef]
- Bonnell, E.K.; Huggins, C.E.; Huggins, C.T.; McCaffrey, T.A.; Palermo, C.; Bonham, M.P. Influences on Dietary Choices during Day versus Night Shift in Shift Workers: A Mixed Methods Study. Nutrients 2017, 9, 193. [Google Scholar] [CrossRef]
- Qian, J.; Morris, C.J.; Caputo, R.; Garaulet, M.; Scheer, F. Ghrelin is impacted by the endogenous circadian system and by circadian misalignment in humans. Int. J. Obes. 2019, 43, 1644–1649. [Google Scholar] [CrossRef]
- Ruxton, C.H.; Kirk, T.R. Breakfast: A review of associations with measures of dietary intake, physiology and biochemistry. Br. J. Nutr. 1997, 78, 199–213. [Google Scholar] [CrossRef]
- Song, W.O.; Chun, O.K.; Obayashi, S.; Cho, S.; Chung, C.E. Is consumption of breakfast associated with body mass index in US adults? J. Am. Diet. Assoc. 2005, 105, 1373–1382. [Google Scholar] [CrossRef]
- Timlin, M.T.; Pereira, M.A.; Story, M.; Neumark-Sztainer, D. Breakfast eating and weight change in a 5-year prospective analysis of adolescents: Project EAT (Eating Among Teens). Pediatrics 2008, 121, e638–e645. [Google Scholar] [CrossRef] [PubMed]
- Van der Heijden, A.A.; Hu, F.B.; Rimm, E.B.; van Dam, R.M. A prospective study of breakfast consumption and weight gain among U.S. men. Obesity 2007, 15, 2463–2469. [Google Scholar] [CrossRef] [PubMed]
- Reutrakul, S.; Hood, M.M.; Crowley, S.J.; Morgan, M.K.; Teodori, M.; Knutson, K.L. The relationship between breakfast skipping, chronotype, and glycemic control in type 2 diabetes. Chronobiol. Int. 2014, 31, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Mekary, R.A.; Giovannucci, E.; Cahill, L.; Willett, W.C.; van Dam, R.M.; Hu, F.B. Eating patterns and type 2 diabetes risk in older women: Breakfast consumption and eating frequency. Am. J. Clin. Nutr. 2013, 98, 436–443. [Google Scholar] [CrossRef]
- Jakubowicz, D.; Froy, O.; Wainstein, J.; Boaz, M. Meal timing and composition influence ghrelin levels, appetite scores and weight loss maintenance in overweight and obese adults. Steroids 2012, 77, 323–331. [Google Scholar] [CrossRef] [PubMed]
- Dashti, H.S.; Merino, J.; Lane, J.M.; Song, Y.; Smith, C.E.; Tanaka, T.; McKeown, N.M.; Tucker, C.; Sun, D.; Bartz, T.M.; et al. Genome-wide association study of breakfast skipping links clock regulation with food timing. Am. J. Clin. Nutr. 2019, 110, 473–484. [Google Scholar] [CrossRef]
- Lewontin, R.C. The analysis of variance and the analysis of causes. 1974. Int. J. Epidemiol. 2006, 35, 520–525. [Google Scholar] [CrossRef]
- Lewontin, R.C. Biological determinism. Tanner Lect. Human Values 1983, 4, 147–183. [Google Scholar]
- Lewontin, R.C.; Rose, S.P.R.; Kamin, L.J. Not in Our Genes: Biology, Ideology, and Human Nature; Pantheon Books: New York, NY, USA, 1984. [Google Scholar]
- Maestripieri, D.; Mateo, J.M. Maternal Effects in Mammals; University of Chicago Press: Chicago, IL, USA, 2009. [Google Scholar]
- Waddington, C.H. Canalization of development and the inheritance of acquired characters. Nature 1942, 150, 563. [Google Scholar] [CrossRef]
- Archer, E.; Lavie, C.J.; Hill, J.O. The Contributions of ‘Diet’, ‘Genes’, and Physical Activity to the Etiology of Obesity: Contrary Evidence and Consilience. Prog. Cardiovasc. Dis. 2018, 61, 89–102. [Google Scholar] [CrossRef]
- Lane, J.M.; Vlasac, I.; Anderson, S.G.; Kyle, S.D.; Dixon, W.G.; Bechtold, D.A.; Gill, S.; Little, M.A.; Luik, A.; Loudon, A.; et al. Genome-wide association analysis identifies novel loci for chronotype in 100, 420 individuals from the UK Biobank. Nat. Commun. 2016, 7, 10889. [Google Scholar] [CrossRef] [PubMed]
- Archer, E.; Marlow, M.L.; Lavie, C.J. Controversy and debate: Memory-Based Methods Paper 1: The fatal flaws of food frequency questionnaires and other memory-based dietary assessment methods. J. Clin. Epidemiol. 2018, 104, 113–124. [Google Scholar] [CrossRef] [PubMed]
| Reference | Study Type | Population | Age (Years) | Sex | Meal Timing | Metabolic Effect | Main Results | Reference |
|---|---|---|---|---|---|---|---|---|
| Garaulet M et al., 2013 | Observational study | 420 obese subjects | 42 ± 11 | 50% Women | Lunch timing (early eaters (lunch before 3 p.m.), late eaters (lunch after 3 p.m.)) | Weight loss effectiveness | 1. Late eaters lost less weight and displayed a slower weight loss rate than early eaters | [15] |
| 2. Late eaters were more evening types, had less energetic breakfasts and skipped breakfast more frequently than early eaters | ||||||||
| Ruiz-Lozano T et al., 2016 | Observational prospective study | 270 subjects | 52 ± 11 | 78% Women | Lunch timing (early eaters (lunch before 3 p.m.), late lunch eaters (lunch after 3 p.m.)) | Weight loss evolution after bariatric surgery | 1. The percentage of late eaters was significantly higher in the primarily poor weight-loss-responders (~70%) than in both secondarily poor weight-loss-responders (~42%) and good weight-loss-responders (~37%) | [17] |
| 2. Primarily poor weight-loss-responders had lunch later as compared to good and secondarily poor weight-loss-responders | ||||||||
| Bandín C et al., 2015 | Randomized, crossover trial | 32 subjects | 24 ± 4 | Women | Lunch timing (early eaters (lunch at 1 p.m.), late eaters (lunch at 4:30 p.m.)) | Energy-expenditure, glucose-tolerance and circadian-related variables | 1. Eating late is associated with decreased resting-energy-expenditure, decreased fasting carbohydrate oxidation, decreased glucose-tolerance, blunted daily profile in free cortisol concentrations, and decreased the thermal effect of food on wrist temperature | [11] |
| Collado M.C et al., 2018 | Randomized, crossover trial | 10 subjects | 25 ± 6 | Women | Lunch timing (early eaters (lunch at 2 p.m.), late eaters (lunch at 4 p.m.)) | Daily rhythms of human salivary microbiota | 1. Eating the main meal late inverts the daily rhythm of salivary microbiota diversity which may have a deleterious effect on the metabolism of the host | [18] |
| Garaulet M et al., 2016 | Observational study | 1287 subjects | 39 ± 12 | 82% Women | Lunch timing (12 p.m. until 4:30 p.m.) | Weight-loss effectiveness | 1. Variability at the PLIN1 locus is associated with variability in weight loss | [19] |
| 2. Eating late is related to lower weight-loss effectiveness among carriers of the AA genotype at the PLIN1 14995AT variant | ||||||||
| Xiao Q et al., 2019 | Observational study | 872 subjects | ≥18 | 53% Women | 24-h dietary recalls (during one year every two months) | Interaction with macronutrient intake and chronotype | 1. Higher dietary consumption after waking up and lower consumption close to bedtime associate with lower BMI, but the relationship differs by chronotype 2. A higher percentage of carbohydrates and protein close to bedtime was associated with higher odds of being overweight or obese, particularly in people with a later chronotype | [20] |
| Yoshida J et al., 2018 | Longitudinal study | 8153 subjects | 47 ± 8 | 60% Men | Night eating (“dinner before bed” (within two hours before bedtime) and “snacks after dinner” (snacks after dinner) | Night eating habits and metabolic syndrome | 1. In women, there was an association between eating habits at night and metabolic syndrome | [21] |
| 2. Night eating habits were associated with dyslipidemia in men and women | ||||||||
| Kutsuma A et al., 2014 | Observational study (Cross-sectional) | 60,800 subjects | 41 ± 12 | 67% Men | Breakfast (skipping) and late-night eating (within two hours of bedtime) | Breakfast skipping, late-night-dinner eating, and metabolic syndrome | 1. Skipping breakfast alone and late-night-dinner alone were not associated with metabolic syndrome | [22] |
| 2. Habitual breakfast skipping concomitant with late-night eating may represent poorer eating behavior than skipping breakfast alone and associated with metabolic syndrome | ||||||||
| Chen HJ et al., 2019 | Observational study (Cross-sectional) | 1283 subjects | ≥19 | 56% Men | Energy intake at different times (morning (5–9 a.m.), noon (11:30 a.m.–1:30 p.m.), evening (5:30–8:30 p.m.)) | Total and LDL cholesterol levels | 1. Transferring 100 kcal of energy or fat intake at night to the morning or noon decreased LDL cholesterol 2. Elevated total and LDL cholesterol were positively associated with nighttime energy and fat intake | [23] |
| Nakajima K et al., 2015 | Observational study (Cross-sectional) | 61,364 subjects | 46 ± 10 | 66% Men | Breakfast (skipping) and late-night eating (within two hours of bedtime) | Night eating, skipping breakfast and hyperglycemia | 1. Hyperglycemia in the general Japanese population associated with late-night dinner eating alone, but not with breakfast skipping alone | [24] |
| Morgan L M et al., 2012 | Randomized crossover study | 6 subjects | 30 ± 4 | 67% Women | Energy intake at different times (low glycemic index and high glycemic index, morning and night, at breakfast (9:30 a.m.), lunch (1:30 p.m.), dinner (8:30 p.m.)) | Meal timing and glycemic index on glucose and insulin secretion | 1. Lower insulin sensitivity in high energy consumed in the evening | [25] |
| 2. Both meal timing and glycemic index affected glucose tolerance and insulin secretion | ||||||||
| Jakubowicz et al., 2013 | Randomized, open-label, parallel-arm study | 93 subjects | 46 ± 7 | Women | Energy intake at different times (breakfast (8 a.m.), lunch (1 p.m.), dinner (7 p.m.)) | High caloric intake at breakfast vs. dinner influences weight loss | 1. High-calorie breakfast with reduced intake at dinner is beneficial | [10] |
| Rubio-Sastre P et al., 2014 | Placebo-controlled, single-blind design study | 21 subjects | 24 ± 6 | Women | Morning (9 a.m.) and night melatonin supplementation (9 p.m.) | Melatonin administration impairs glucose tolerance | 1. Acute melatonin supplementation (5 mg) impaired glucose tolerance in both, morning and evening time | [26] |
| Lopez-Minguez J et al., 2017 | Randomized, crossover trial | 40 subjects | 42 ± 10 | Women | Dinner timing (early dinner (8 p.m.), late dinner (11 p.m.)) | Late dinner and glucose tolerance | 1. The concurrence of meal timing (late dinner) with elevated endogenous melatonin concentrations impaired glucose tolerance | [27] |
| 2. The effect was stronger in MTNR1B risk-carriers (GG) than in non-carriers (CC) | ||||||||
| Smith KJ et al., 2010 | Longitudinal study | 2184 subjects | 7 to 15 26 to 36 | 53% Women | Skipping breakfast | Cardiometabolic risk factors | 1. Those who skipped breakfast in both childhood and adulthood had higher waist circumference and higher fasting insulin, total cholesterol, and LDL cholesterol concentrations than did those who ate breakfast | [28] |
| 2. Skipping breakfast over a long period may have detrimental effects on cardiometabolic health | ||||||||
| Reutrakul S et al., 2014 | Observational study | 194 subjects | 54 ± 13 | 71% Women | Skipping breakfast | Chronotype and glycemic control in type 2 diabetes | 1. Breakfast skipping is associated with a later chronotype | [29] |
| 2. Later chronotype and breakfast skipping both contribute to poorer glycemic control, as indicated by higher glycosylated hemoglobin (HbA1C) levels | ||||||||
| Jakubowicz et al., 2012 | Randomized crossover study | 193 subjects | 47 ± 7 | 60% Women | Energy intake timing (low carbohydrate diet, low carbohydrate breakfast, and high carbohydrate enriched breakfast diet) | Weight loss, ghrelin levels, and appetite scores | 1. A high carbohydrate and high protein breakfast may prevent weight regain by reducing diet-induced compensatory changes in hunger, cravings and ghrelin suppression | [30] |
| de Castro JM et al., 2004 | Observational study | 886 subjects | 36 ± 14 | 57% Women | Energy intake at different times (6–9:59 a.m., 10 a.m.–1:59 p.m., 2–5:59 p.m., 6–9:59 p.m., 10:00 p.m.–1:59 a.m.) | Food intake influences overall intake | 1. Energy intake in the morning is particularly satiating and can reduce the total amount ingested for the day | [31] |
| 2. Energy intake in the late-night lacks satiating value and can result in greater overall daily intake | ||||||||
| Kant AK et al., 2015 | Observational study | 13,298 subjects | ≥20 | 52% Men | Skipping breakfast (energy intake at different times) | Eating behaviors, time of eating, and dietary intake | 1. Lunch meal provided more energy on the no-breakfast day than on the breakfast day | [32] |
| Lopez-Minguez J et al., 2019 | Observational study | 106 subjects | 52 ± 6 | Women | Timing of food intake | Heritability of the timing of food intake | 1. Genetic factors contributed to a higher degree to the timing of breakfast (56%) than the timing of lunch (38%) or dinner (0%) | [33] |
| Mekary RA et al., 2013 | Observational study | 1560 subjects | 66 ± 7 | Women | Skipping breakfast (energy intake at different times) | Eating patterns and type 2 diabetes risk | 1. Irregular breakfast consumption was associated with a higher type 2 diabetes risk | [34] |
| Dashti HS et al., 2019 | Observational study | 193,860 subjects | ≥19 | 55% Women | Skipping breakfast | Genetic variants of skipping breakfast | 1. Proxy-phenotype Genome-Wide Association Study (GWAS) identified six genetic variants for breakfast skipping, linking clock regulation with food timing | [35] |
| 2. Skipping breakfast was causal of obesity | ||||||||
| Lane JM et al., 2016 | Observational study | 100,420 subjects | 40–69 years | 55% Women | Chronotype | Genetic variants of chronotype | 1. The study reports the discovery of 12 genetic loci associated with chronotype | [36] |
| Sievert K et al., 2019 | Systematic review and meta-analysis | 12 studies | ≥18 | 70% Women | Regular breakfast consumption | Weight change and energy intake | 1. The addition of breakfast might not be a good strategy for weight loss | [37] |
| 2. Caution is needed when recommending breakfast for weight loss in adults, as it could have the opposite effect |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lopez-Minguez, J.; Gómez-Abellán, P.; Garaulet, M. Timing of Breakfast, Lunch, and Dinner. Effects on Obesity and Metabolic Risk. Nutrients 2019, 11, 2624. https://doi.org/10.3390/nu11112624
Lopez-Minguez J, Gómez-Abellán P, Garaulet M. Timing of Breakfast, Lunch, and Dinner. Effects on Obesity and Metabolic Risk. Nutrients. 2019; 11(11):2624. https://doi.org/10.3390/nu11112624
Chicago/Turabian StyleLopez-Minguez, Jesus, Purificación Gómez-Abellán, and Marta Garaulet. 2019. "Timing of Breakfast, Lunch, and Dinner. Effects on Obesity and Metabolic Risk" Nutrients 11, no. 11: 2624. https://doi.org/10.3390/nu11112624
APA StyleLopez-Minguez, J., Gómez-Abellán, P., & Garaulet, M. (2019). Timing of Breakfast, Lunch, and Dinner. Effects on Obesity and Metabolic Risk. Nutrients, 11(11), 2624. https://doi.org/10.3390/nu11112624





