Intake of Processed Meat and Association with Sociodemographic and Lifestyle Factors in a Representative Sample of the Swiss Population
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Ethical Approval
2.3. Dietary Assessment
2.4. Sociodemographic, Lifestyle, and Anthropometric Variables
2.5. Categorization of Processed Meats
2.6. Data Handling and Statistical Analysis
2.7. Weighting of Data
2.8. Reporting Data
3. Results
3.1. Characteristics of the Study Population
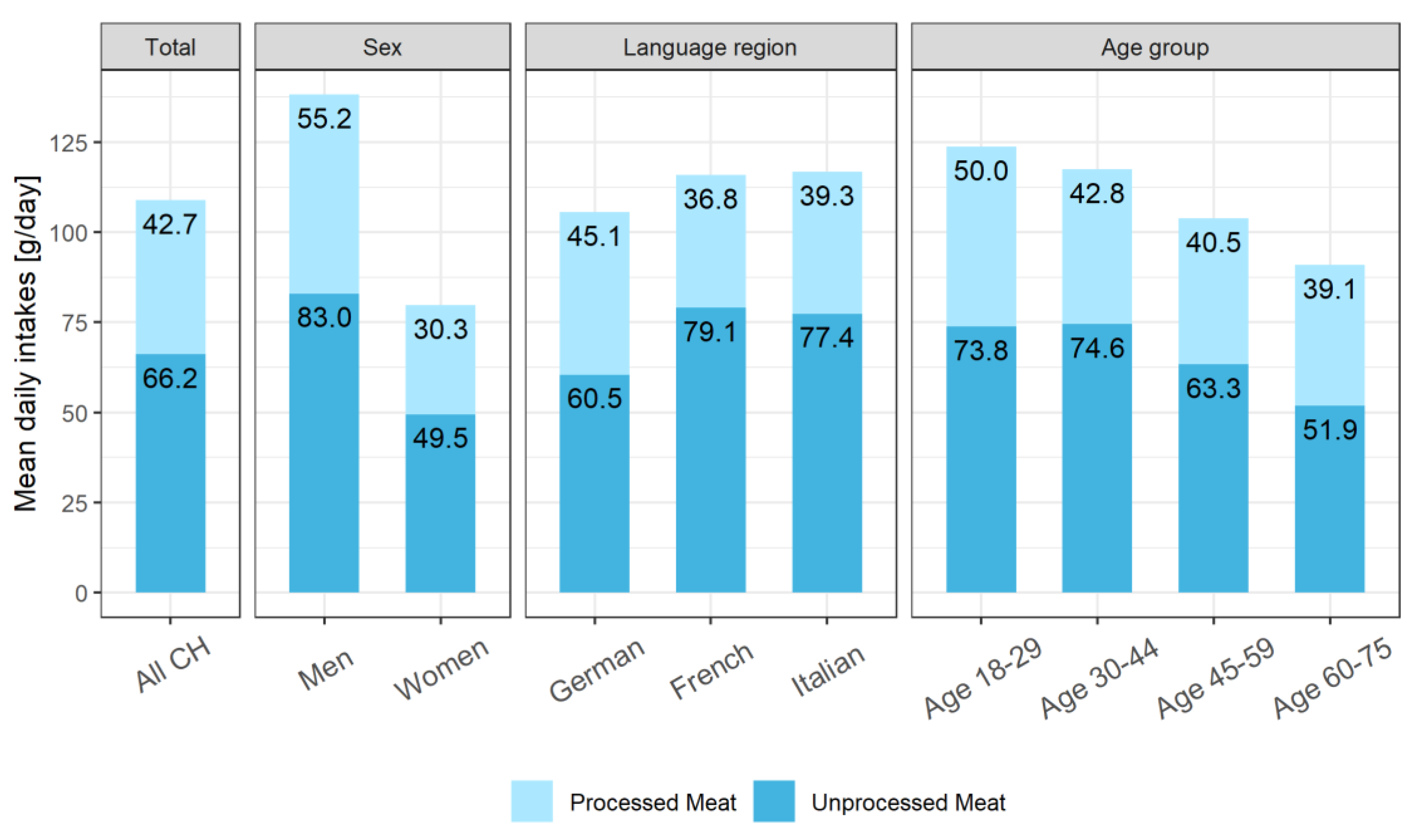
3.2. Intake of Total Meat, Processed and Unprocessed
3.3. Intake of Different Types of Processed Meat
3.4. Processed Meats Containing Nitrate and Nitrite
3.5. Sociodemographic and Lifestyle Factors Associated with Processed Meat Intake
4. Discussion
4.1. Summary of Main Findings
4.2. Processed Meat Consumption in Switzerland and in Europe
4.3. Nutritional Recommendations for Meat and Processed Meat Consumption
4.4. Different Types of Processed Meat
4.5. Processed Meat Consumption and Sociodemographic and Lifestyle Factors
4.6. Processed Meat Consumption and Colorectal Cancer Risk
4.7. Strengths and Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Micha, R.; Michas, G.; Mozaffarian, D. Unprocessed red and processed meats and risk of coronary artery disease and type 2 diabetes—An updated review of the evidence. Curr. Atheroscler. Rep. 2012, 14, 515–524. [Google Scholar] [CrossRef]
- Rohrmann, S.; Linseisen, J. Processed meat: The real villain? Proc. Nutr. Soc. 2016, 75, 233–241. [Google Scholar] [CrossRef]
- Bouvard, V.; Loomis, D.; Guyton, K.Z.; Grosse, Y.; El Ghissassi, F.; Benbrahim-Tallaa, L.; Guha, N.; Mattock, H.; Straif, K.; International Agency for Research on Cancer Monograph Working Group. Carcinogenicity of consumption of red and processed meat. Lancet Oncol. 2015, 16, 1599–1600. [Google Scholar] [CrossRef] [Green Version]
- Clonan, A.; Roberts, K.E.; Holdsworth, M. Socioeconomic and demographic drivers of red and processed meat consumption: Implications for health and environmental sustainability. Proc. Nutr. Soc. 2016, 75, 367–373. [Google Scholar] [CrossRef] [PubMed]
- Willett, W.; Rockstrom, J.; Loken, B.; Springmann, M.; Lang, T.; Vermeulen, S.; Garnett, T.; Tilman, D.; DeClerck, F.; Wood, A.; et al. Food in the Anthropocene: The EAT–Lancet Commission on healthy diets from sustainable food systems. Lancet 2019, 393, 447–492. [Google Scholar] [CrossRef]
- Maddock, R. Meat and Meat Products. In Handbook of Meat and Meat Processing, 2nd ed.; Hui, Y.H., Ed.; CRC Press: London, UK, 2012; pp. 598–603. [Google Scholar]
- Schweizer Fleisch–Fachverbandes (SFF). Qualitätsleitsätze für Fleisch und Fleischprodukte, Version 3. Available online: https://m.sff.ch/de-wAssets/docs/fleischinfos/deklaration/qualitaetsleitsaetze/1_Qualitaetsleitsaetze-def_V3_D.pdf (accessed on 19 June 2018).
- Linseisen, J.; Rohrmann, S.; Norat, T.; Gonzalez, C.A.; Iraeta, M.D.; Gomez, P.M.; Chirlaque, M.-D.; Pozo, B.G.; Ardanaz, E.; Mattisson, I.; et al. Dietary intake of different types and characteristics of processed meat which might be associated with cancer risk—Results from the 24-hour diet recalls in the European Prospective Investigation into Cancer and Nutrition (EPIC). Public Health Nutr. 2006, 9, 449–464. [Google Scholar] [CrossRef] [PubMed]
- Micha, R.; Wallace, S.K.; Mozaffarian, D. Red and Processed Meat Consumption and Risk of Incident Coronary Heart Disease, Stroke, and Diabetes Mellitus. Circulation 2010, 121, 2271–2283. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jimenez-Colmenero, F.; Carballo, J.; Cofrades, S. Healthier meat and meat products: Their role as functional foods. Meat Sci. 2001, 59, 5–13. [Google Scholar] [CrossRef]
- Micha, R.; Michas, G.; Lajous, M.; Mozaffarian, D. Processing of meats and cardiovascular risk: Time to focus on preservatives. BMC Med. 2013, 11, 136. [Google Scholar] [CrossRef]
- Krebsliga Schweiz: Krebs in der Schweiz: Wichtige Zahlen. Bern. Dezember 2018. Available online: https://www.krebsliga.ch/ueber-krebs/zahlen-fakten/-dl-/fileadmin/downloads/sheets/zahlen-krebs-in-der-schweiz.pdf (accessed on 18 October 2019).
- Federal Statistical Office, Sections Health Services (SHS); Bern, Switzerland. 2016. Available online: https://www.bfs.admin.ch/bfs/en/home/statistics/health/state-health/mortality-causes-death/specific.html (accessed on 17 October 2019).
- Heuer, T.; Krems, C.; Moon, K.; Brombach, C.; Hoffmann, I. Food consumption of adults in Germany: Results of the German National Nutrition Survey II based on diet history interviews. Br. J. Nutr. 2015, 113, 1603–1614. [Google Scholar] [CrossRef]
- Guenther, P.M.; Jensen, H.H.; Batres-Marquez, S.P.; Chen, C.-F. Sociodemographic, Knowledge, and Attitudinal Factors Related to Meat Consumption in the United States. J. Am. Diet. Assoc. 2005, 105, 1266–1274. [Google Scholar] [CrossRef] [PubMed]
- Eichholzer, M.; Bisig, B. Daily consumption of (red) meat or meat products in Switzerland: Results of the 1992/93 Swiss Health Survey. Eur. J. Clin. Nutr. 2000, 54, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Linseisen, J.; Kesse, E.; Slimani, N.; Bueno-De-Mesquita, H.B.; Ocke, M.C.; Skeie, G.; Kumle, M.; Dorronsoro Iraeta, M.; Morote Gomez, P.; Janzon, L.; et al. Meat consumption in the European Prospective Investigation into Cancer and Nutrition (EPIC) cohorts: Results from 24-hour dietary recalls. Public Health Nutr. 2002, 5, 1243–1258. [Google Scholar] [CrossRef] [PubMed]
- Federal Department of Home Affaires (FDHA). Swiss Health Survey 2012 Overview. Available online: https://www.bfs.admin.ch/bfs/en/home/statistics/catalogues–databases/publications.assetdetail.349060.html (accessed on 10 June 2019).
- Chatelan, A.; Beer-Borst, S.; Randriamiharisoa, A.; Pasquier, J.; Blanco, J.M.; Siegenthaler, S.; Paccaud, F.; Slimani, N.; Nicolas, G.; Camenzind-Frey, E.; et al. Major Differences in Diet across Three Linguistic Regions of Switzerland: Results from the First National Nutrition Survey menuCH. Nutrients 2017, 9, 1163. [Google Scholar] [CrossRef]
- Krieger, J.-P.; Pestoni, G.; Cabaset, S.; Brombach, C.; Sych, J.; Schader, C.; Faeh, D.; Rohrmann, S. Dietary Patterns and Their Sociodemographic and Lifestyle Determinants in Switzerland: Results from the National Nutrition Survey menuCH. Nutrients 2018, 11, 62. [Google Scholar] [CrossRef]
- Chatelan, A.; Marques-Vidal, P.; Bucher, S.; Siegenthaler, S.; Metzger, N.; Zuberbuhler, C.; Camenzind-Frey, E.; Reggli, A.; Bochud, M.; Beer-Borst, S. Lessons Learnt About Conducting a Multilingual Nutrition Survey in Switzerland: Results from menuCH Pilot Survey. Int. J. Vitam. Nutr. Res. 2018, 87, 25–36. [Google Scholar] [CrossRef]
- Institut Universitaire de Médecine Sociale et Préventive (IUMSP)—CHUV/UNIL; Swiss Federal Food Safety and Veterinary Office (FSVO). Switzerland—National Nutrition Survey menuCH 2014–2015. Available online: https://menuch.iumsp.ch/index.php/catalog/4 (accessed on 20 March 2018).
- Crispim, S.; Nicolas, G.; Casagrande, C.; Knaze, V.; Illner, A.; Huybrechts, I.; Slimani, N. Quality assurance of the international computerised 24 h dietary recall method (EPIC–Soft). Br. J. Nutr. 2014, 111, 506–515. [Google Scholar] [CrossRef]
- Camenzind-Frey, E.; Zuberbuehler, C. menuCH—Schweizerisches Fotobuch/Livre Photo Suisse/Manuale Fotografico Svizzero; Federal Office of Public Health (FOPH) and Federal Food Safety and Veterinary Office (FSVO): Bern, Switzerland, 2014. [Google Scholar]
- Hagstromer, M.; Oja, P.; Sjostrom, M. The International Physical Activity Questionnaire (IPAQ): A study of concurrent and construct validity. Public Health Nutr. 2006, 9, 755–762. [Google Scholar] [CrossRef]
- Craig, C.; Marshall, A.; Sjostrom, M. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- IPAQ Research Committee. Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ); Karolinska Institute: Stockholm, Sweden, 2005. [Google Scholar]
- World Health Organisation (WHO). MONICA Manual, Part. III, Section 1: Population Survey Data Component; 4.6 Height, Weight, Waist and Hip Measurement; WHO Press: Geneva, Switzerland, 1997. [Google Scholar]
- Eidgenossisches Departement des Innern EDI. Verordnung des EDI Über Die in Lebensmitteln Zulässigen Zusatzstoffe (Zusatzstoffverordnung, ZuV.); Bd. SR 817.022.31; Eidgenössisches Departement des Innern EDI: Bern, Switzerland, 2014. [Google Scholar]
- Shapiro, S.S.; Wilk, M.B. An analysis of variance test for normality (complete samples). Biometrika 1965, 52, 591–611. [Google Scholar] [CrossRef]
- Bopp, M.; Braun, J.; Gutzwiller, F.; Faeh, D.; For the Swiss National Cohort Study Group. Health Risk or Resource? Gradual and Independent Association between Self–Rated Health and Mortality Persists Over 30 Years. PLoS ONE 2012, 7, e30795. [Google Scholar] [CrossRef] [PubMed]
- Buuren, S.; Groothuis-Oudshoorn, K. Mice: Multivariate Imputation by Chained Equations in R. J. Stat. Softw. 2001, 45, 1–67. [Google Scholar] [CrossRef]
- Pasquier, J.; Chatelan, A.; Bochud, M. Weighting Strategy; Institute of Social and Preventive Medicine: Lausanne, Switzerland, 2017. [Google Scholar]
- Lachat, C.; Hawwash, D.; Ocke, M.C.; Berg, C.; Forsum, E.; Hornell, A.; Larsson, C.; Sonestedt, E.; Wirfalt, E.; Akesson, A.; et al. Strengthening the Reporting of Observational Studies in Epidemiology—Nutritional Epidemiology (STROBE–nut): An Extension of the STROBE Statement. PLoS Med. 2016, 13, e1002036. [Google Scholar] [CrossRef] [PubMed]
- Proviande. Jährlicher Konsum 2018. Available online: https://www.proviande.ch/de/dienstleistungen-statistik/statistik/publikationen.html (accessed on 27 August 2019).
- Obrist, L. Nahrungsmittelbilanz (NMB08), Vergleich der Nahrungsmittelbilanz (NMB08) und der Ernährungsbilanz (EB80) als Datengrundlage für den Schweizerischen Ernährungsbericht (SEB); Schweizer Bauernverband Agristat: Brugg, Switzerland, 2016. [Google Scholar]
- Mertens, E.; Kuijsten, A.; Dofkova, M.; Mistura, L.; D’Addezio, L.; Turrini, A.; Dubuisson, C.; Favret, S.; Havard, S.; Trolle, E.; et al. Geographic and socioeconomic diversity of food and nutrient intakes: A comparison of four European countries. Eur. J. Nutr. 2018, 58, 1475–1493. [Google Scholar] [CrossRef] [PubMed]
- Mejean, C.; Si Hassen, W.; Lecossais, C.; Alles, B.; Peneau, S.; Hercberg, S.; Castetbon, K. Socio-economic indicators are independently associated with intake of animal foods in French adults. Public Health Nutr. 2016, 19, 3146–3157. [Google Scholar] [CrossRef] [Green Version]
- Irish Universities Nutrition Alliance. National Adult Nutrition Survey, 2008–2010. Available online: https://www.iuna.net/surveyreports (accessed on 18 May 2019).
- Swiss Nutrition Society (SGE). Swiss Food Pyramid. Available online: http://www.sge-ssn.ch/ich-und-du/essen-und-trinken/ausgewogen/schweizer-lebensmittelpyramide/ (accessed on 24 January 2019).
- Schneid Schuh, D.; Campos Pellanda, L.; Guessous, I.; Marques-Vidal, P. Trends and determinants of change in compliance to dietary guidelines in a Swiss community–dwelling sample. Prev. Med. 2018, 111, 198–203. [Google Scholar] [CrossRef]
- French Agency for Food; Environmental and Occupational Health & Safety (ANSES). ANSES Updates Its Food Consumption Guidelines for the French Population. Available online: https://www.anses.fr/en/content/anses-updates-its-food-consumption-guidelines-french-population (accessed on 16 August 2019).
- LaNutrition. La Pyramide Alimentaire de Lanutrition.fr. Available online: https://www.lanutrition.fr/bien-dans-son-assiette/bien-manger/les-recommandations-de-lanutrition.fr/la-pyramide-alimentaire-de-lanutritionfr (accessed on 8 April 2018).
- Unità di Ricerca di Scienza dell’Alimentazione e Nutrizione Umana, D.d.M.S. Piramide Alimentare Italiana. Available online: http://www.piramideitaliana.it/ (accessed on 10 February 2019).
- World Cancer Research Fund International (WCRF); American Institute for Cancer Research (AICR). Recommendations and Public Health and Policy Implications; WCRF International: London, UK, 2018. [Google Scholar]
- Swiss Confederation-Federal Food Safety and Veterinary Office (FSVO). Eating Well and Staying Healthy, Swiss Nutrition Policy 2017-24. 2017. Available online: https://www.blv.admin.ch/blv/en/home/das-blv/strategien/schweizer-ernaehrungsstrategie.html (accessed on 14 March 2019).
- Mozaffarian, D. Dietary and Policy Priorities for Cardiovascular Disease, Diabetes, and Obesity: A Comprehensive Review. Circulation 2016, 133, 187–225. [Google Scholar] [CrossRef]
- Sacks, F.M.; Lichtenstein, A.H.; Wu, J.H.Y.; Appel, L.J.; Creager, M.A.; Kris-Etherton, P.M.; Miller, M.; Rimm, E.B.; Rudel, L.L.; Robinson, J.G.; et al. Dietary Fats and Cardiovascular Disease: A Presidential Advisory from the American Heart Association. Circulation 2017, 136, e1–e23. [Google Scholar] [CrossRef]
- Vergnaud, A.-C.; Norat, T.; Romaguera, D.; Mouw, T.; May, A.M.; Travier, N.; Luan, J.A.; Wareham, N.; Slimani, N.; Rinaldi, S.; et al. Meat consumption and prospective weight change in participants of the EPIC–PANACEA study. Am. J. Clin. Nutr. 2010, 92, 398–407. [Google Scholar] [CrossRef]
- Oostindjer, M.; Alexander, J.; Amdam, G.V.; Andersen, G.; Bryan, N.S.; Chen, D.; Corpet, D.E.; De Smet, S.; Dragsted, L.O.; Haug, A.; et al. The role of red and processed meat in colorectal cancer development: A perspective. Meat Sci. 2014, 97, 583–596. [Google Scholar] [CrossRef]
- Sui, Z.; Raubenheimer, D.; Rangan, A. Consumption patterns of meat, poultry, and fish after disaggregation of mixed dishes: Secondary analysis of the Australian National Nutrition and Physical Activity Survey 2011–2012. BMC Nutr. 2017, 3, 52. [Google Scholar] [CrossRef]
- Lenighan, Y.M.; Nugent, A.P.; Li, K.F.; Brennan, L.; Walton, J.; Flynn, A.; Roche, H.M.; McNulty, B.A. Processed red meat contribution to dietary patterns and the associated cardio–metabolic outcomes. Br. J. Nutr. 2017, 118, 222–228. [Google Scholar] [CrossRef] [PubMed]
- Etemadi, A.; Sinha, R.; Ward, M.H.; Graubard, B.I.; Inoue-Choi, M.; Dawsey, S.M.; Abnet, C.C. Mortality from different causes associated with meat, heme iron, nitrates, and nitrites in the NIH–AARP Diet and Health Study: Population based cohort study. BMJ 2017, 357, j1957. [Google Scholar] [CrossRef] [PubMed]
- Pestoni, G.; Krieger, J.-P.; Sych, J.M.; Faeh, D.; Rohrmann, S. Cultural Differences in Diet and Determinants of Diet Quality in Switzerland: Results from the National Nutrition Survey menuCH. Nutrients 2019, 11, 126. [Google Scholar] [CrossRef] [PubMed]
- Fiolet, T.; Srour, B.; Sellem, L.; Kesse-Guyot, E.; Alles, B.; Mejean, C.; Deschasaux, M.; Fassier, P.; Latino-Martel, P.; Beslay, M.; et al. Consumption of ultra–processed foods and cancer risk: Results from NutriNet–Sante prospective cohort. BMJ 2018, 360, k322. [Google Scholar] [CrossRef]
- Habermeyer, M.; Roth, A.; Guth, S.; Diel, P.; Engel, K.-H.; Epe, B.; Fürst, P.; Heinz, V.; Humpf, H.-U.; Joost, H.-G.; et al. Nitrate and nitrite in the diet: How to assess their benefit and risk for human health. Mol. Nutr. Food Res. 2015, 59, 106–128. [Google Scholar] [CrossRef]
- Nunez De Gonzalez, M.T.; Osburn, W.N.; Hardin, M.D.; Longnecker, M.; Garg, H.K.; Bryan, N.S.; Keeton, J.T. Survey of Residual Nitrite and Nitrate in Conventional and Organic/Natural/Uncured/Indirectly Cured Meats Available at Retail in the United States. J. Agric. Food Chem. 2012, 60, 3981–3990. [Google Scholar] [CrossRef]
- Inoue-Choi, M.; Virk-Baker, M.K.; Aschebrook-Kilfoy, B.; Cross, A.J.; Subar, A.F.; Thompson, F.E.; Sinha, R.; Ward, M.H. Development and calibration of a dietary nitrate and nitrite database in the NIH-AARP Diet and Health Study. Public Health Nutr. 2016, 19, 1934–1943. [Google Scholar] [CrossRef]
- Schmid, A. Einfluss von Nitrat und Nitrit aus Fleischerzeugnissen auf die Gesundheit des Menschen. Ernährungsumschau 2006, 53, 490–495. [Google Scholar]
- Grasso, S.; Brunton, N.P.; Lyng, J.G.; Lalor, F.; Monahan, F.J. Healthy processed meat products—Regulatory, reformulation and consumer challenges. Trends Food Sci. Technol. 2014, 39, 4–17. [Google Scholar] [CrossRef]
- Daniel, C.R.; Cross, A.J.; Koebnick, C.; Sinha, R. Trends in meat consumption in the USA. Public Health Nutr. 2011, 14, 575–583. [Google Scholar] [CrossRef] [PubMed]
- Diallo, A.; Deschasaux, M.; Latino-Martel, P.; Hercberg, S.; Galan, P.; Fassier, P.; Alles, B.; Gueraud, F.; Pierre, F.H.; Touvier, M. Red and processed meat intake and cancer risk: Results from the prospective NutriNet–Sante cohort study. Int. J. Cancer 2018, 142, 230–237. [Google Scholar] [CrossRef] [PubMed]
- Rouhani, M.H.; Salehi-Abargouei, A.; Surkan, P.J.; Azadbakht, L. Is there a relationship between red or processed meat intake and obesity? A systematic review and meta–analysis of observational studies. Obes. Rev. 2014, 15, 740–748. [Google Scholar] [CrossRef] [PubMed]
- Grosso, G.; Micek, A.; Godos, J.; Pajak, A.; Sciacca, S.; Galvano, F.; Boffetta, P. Health risk factors associated with meat, fruit and vegetable consumption in cohort studies: A comprehensive meta–analysis. PLoS ONE 2017, 12, e0183787. [Google Scholar] [CrossRef]
- Schmid, A.; Gille, D.; Piccinali, P.; Bütikofer, U.; Chollet, M.; Altintzoglou, T.; Honkanen, P.; Walther, B.; Stoffers, H. Factors predicting meat and meat products consumption among middle–aged and elderly people: Evidence from a consumer survey in Switzerland. Food Nutr. Res. 2017, 61, 1308111. [Google Scholar] [CrossRef]
- International Agency for Research on Cancer (IARC). Absence of Excess Body Fatness; The International Agency for Research on Cancer: Lyon, France, 2018. [Google Scholar]
- Bopp, M.; Braun, J.; Faeh, D.; For the Swiss National Cohort Study Group. Variation in Mortality Patterns Among the General Population, Study Participants, and Different Types of Nonparticipants: Evidence from 25 Years of Follow-up. Am. J. Epidemiol. 2014, 180, 1028–1035. [Google Scholar] [CrossRef]
- Vargas, A.J.; Thompson, P.A. Diet and Nutrient Factors in Colorectal Cancer Risk. Nutr. Clin. Pract. 2012, 27, 613–623. [Google Scholar] [CrossRef]
- Lai, R.; Bian, Z.; Lin, H.; Ren, J.; Zhou, H.; Guo, H. The association between dietary protein intake and colorectal cancer risk: A meta–analysis. World J. Surg. Oncol. 2017, 15, 169. [Google Scholar] [CrossRef]
- Cascella, M.; Bimonte, S.; Barbieri, A.; Del Vecchio, V.; Caliendo, D.; Schiavone, V.; Fusco, R.; Granata, V.; Arra, C.; Cuomo, A. Dissecting the mechanisms and molecules underlying the potential carcinogenicity of red and processed meat in colorectal cancer (CRC): An overview on the current state of knowledge. Infect. Agents Cancer 2018, 13, 3. [Google Scholar] [CrossRef]
- Cotterchio, M.; Boucher, B.A.; Manno, M.; Gallinger, S.; Okey, A.B.; Harper, P.A. Red meat intake, doneness, polymorphisms in genes that encode carcinogen–metabolizing enzymes, and colorectal cancer risk. Cancer Epidemiol. Biomark. Prev. 2008, 17, 3098–3107. [Google Scholar] [CrossRef]
- Wang, J.; Joshi, A.D.; Corral, R.; Siegmund, K.D.; Marchand, L.L.; Martinez, M.E.; Haile, R.W.; Ahnen, D.J.; Sandler, R.S.; Lance, P.; et al. Carcinogen metabolism genes, red meat and poultry intake, and colorectal cancer risk. Int. J. Cancer 2012, 130, 1898–1907. [Google Scholar] [CrossRef] [PubMed]
- Figueiredo, J.C.; Hsu, L.; Hutter, C.M.; Lin, Y.; Campbell, P.T.; Baron, J.A.; Berndt, S.I.; Jiao, S.; Casey, G.; Fortini, B.; et al. Genome-Wide Diet-Gene Interaction Analyses for Risk of Colorectal Cancer. PLoS Genet. 2014, 10, e1004228. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.; Coelho, D.; Blachier, F. Review of the association between meat consumption and risk of colorectal cancer. Nutr. Res. 2013, 33, 983–994. [Google Scholar] [CrossRef] [PubMed]
- World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR). Continuous Update Project Report: Diet., Nutrition, Physical Activity and Colorectal Cancer; WCRF International: London, UK, 2017. [Google Scholar]
- National Institute for Cancer Epidemiology and Registration (NICER). Cancer Incidence in Switzerland. Available online: http://www.nicer.org/NicerReportFiles2017/EN/report/atlas.html?&geog=1 (accessed on 8 November 2018).
- European Food Safety Authority. General principles for the collection of national food consumption data in the view of a pan–European dietary survey. EFSA J. 2019, 7, 1435. [Google Scholar]
| Total Population | PM Consumers | ||
|---|---|---|---|
| Crude | Weighted 1 | Weighted 1 | |
| Number of participants | 2057 | 4,627,878 | 3,331,232 |
| Sex | |||
| Men | 45.4% | 49.8% | 54.9% |
| Women | 54.6% | 50.2% | 45.1% |
| Language region 2 | |||
| German | 65.2% | 69.2% | 71.0% |
| French | 24.4% | 25.2% | 23.5% |
| Italian | 10.4% | 5.6% | 5.5% |
| Age group 3 | |||
| 18–29 years | 19.4% | 18.8% | 18.0% |
| 30–44 years | 25.9 % | 29.9% | 31.0% |
| 45–59 years | 30.4% | 29.8% | 30.1% |
| 60–75 years | 24.3% | 21.6% | 20.9% |
| BMI category 4 | |||
| Underweight (BMI < 18.5 kg/m2) | 2.4% | 2.4% | 2.0% |
| Normal (18.5 ≤ BMI < 25.0 kg/m2) | 54.3% | 54.1% | 53.0% |
| Overweight (25.0 ≤ BMI < 30.0 kg/m2) | 30.5% | 30.6% | 31.5% |
| Obese (BMI ≥ 30.0 kg/m2) | 12.8% | 12.9% | 13.6% |
| Nationality | |||
| Swiss | 72.5% | 61.4% | 62.7% |
| Swiss binational | 14.4% | 13.8% | 23.6% |
| Non-Swiss | 13.0% | 24.8% | 13.7% |
| Education | |||
| Primary | 4.3% | 4.7% | 4.4% |
| Secondary | 47.1% | 42.6% | 43.0% |
| Tertiary | 48.5% | 52.6% | 52.4% |
| Household status | |||
| Living alone | 16.0% | 18.1% | 16.4% |
| Adult living with parents | 7.7% | 7.1% | 7.3% |
| One-parent family with children | 4.5% | 4.4% | 4.1% |
| Couple without children | 33.5% | 31.7% | 31.4% |
| Couple with children | 33.0% | 32.8% | 34.7% |
| Others | 5.3% | 5.7% | 5.9% |
| Income CHF/month | |||
| <6000 | 16.8% | 17.7% | 16.3% |
| 6000–13,000 | 40.9% | 39.8% | 40.8% |
| >13,000 | 13.9% | 14.9% | 16.0% |
| Imputed 5 | 28.4% | 27.6% | 26.9% |
| Physical activity | |||
| Low | 14.7% | 12.9% | 17.0% |
| Moderate | 22.1% | 22.7% | 21.2% |
| High | 40.2% | 40.3% | 40.6% |
| Imputed 5 | 23.0% | 24.2% | 21.2% |
| Smoking status | |||
| Never | 44.5% | 42.9% | 40.8% |
| Former | 33.5% | 33.6% | 34.4% |
| Current | 22.0% | 23.3% | 24.5% |
| Health status | |||
| Very bad to medium | 13.2% | 12.7% | 13.0% |
| Good to very good | 86.6% | 87.1% | 86.7% |
| Currently on a diet | |||
| No | 94.3% | 94.4% | 95.1% |
| Yes | 5.5% | 5.4% | 4.6% |
| Ham | Bacon | Sausages | Other Processed Meat | Total Processed Meat | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (g/day) | SEM | Mean (g/1000 kcal) | Mean (g/day) | SEM | Mean (g/1000 kcal) | Mean (g/day) | SEM | Mean (g/1000 kcal) | Mean (g/day) | SEM | Mean (g/1000 kcal) | Mean (g/day) | SEM | Mean (g/1000 kcal) | |
| All CH | 10.3 | 0.4 | 4.6 | 2.0 | 0.2 | 0.8 | 18.1 | 0.7 | 7.8 | 12.3 | 0.7 | 5.4 | 42.7 | 1.2 | 18.7 |
| Language region | |||||||||||||||
| German | 10.4 | 0.6 | 4.5 | 2.0 | 0.2 | 0.8 | 19.4 | 0.9 | 8.3 | 13.3 | 0.9 | 5.7 | 45.1 | 1.5 | 19.4 |
| French | 8.7 | 0.7 | 4.2 | 2.1 | 0.3 | 0.9 | 16.4 | 1.6 | 7.1 | 9.6 | 1.2 | 4.3 | 36.8 | 2.2 | 16.4 |
| Italian | 16.2 | 1.7 | 8.8 | 1.7 | 0.4 | 0.8 | 10.3 | 1.6 | 4.7 | 11.2 | 2.0 | 5.8 | 39.3 | 3.2 | 20.1 |
| Sex | |||||||||||||||
| Men | 13.0 | 0.7 | 5.3 | 2.5 | 0.3 | 0.9 | 23.4 | 1.2 | 9.3 | 16.2 | 1.3 | 6.5 | 55.2 | 2.0 | 21.9 |
| Women | 7.5 | 0.5 | 4.0 | 1.6 | 0.2 | 0.8 | 12.9 | 0.8 | 6.4 | 8.3 | 0.7 | 4.3 | 30.3 | 1.2 | 15.4 |
| Age group | |||||||||||||||
| 18–29 years | 11.4 | 1.2 | 4.5 | 1.6 | 0.3 | 0.6 | 18.4 | 1.8 | 7.3 | 18.6 | 2.0 | 8.0 | 50.0 | 3.0 | 20.4 |
| 30–44 years | 9.6 | 0.8 | 4.3 | 2.2 | 0.3 | 0.8 | 20.1 | 1.6 | 8.4 | 10.9 | 1.3 | 4.7 | 42.8 | 2.3 | 18.3 |
| 45–59 years | 10.8 | 0.8 | 5.1 | 2.1 | 0.3 | 0.9 | 17.6 | 1.3 | 7.6 | 9.9 | 1.1 | 4.2 | 40.5 | 2.0 | 17.7 |
| 60–75 years | 9.3 | 0.9 | 4.6 | 2.0 | 0.4 | 1.0 | 16.0 | 1.3 | 7.7 | 11.8 | 1.3 | 5.6 | 39.1 | 2.3 | 18.9 |
| Nitrate/Nitrite | Without Nitrate/Nitrite | |||
|---|---|---|---|---|
| Mean (g/day) | SEM | Mean (g/day) | SEM | |
| All CH | 27.4 | 0.9 | 9.8 | 0.6 |
| Language region | ||||
| German | 28.9 | 1.1 | 10.6 | 0.9 |
| French | 23.4 | 1.7 | 7.5 | 1.0 |
| Italian | 26.6 | 2.5 | 10.6 | 1.8 |
| Processed Meat (g/1000 kcal) | ||
|---|---|---|
| Adjusted Coefficients 1 | 95% CI | |
| Sex | ||
| Men | 0 | ref. |
| Women | −4.7 | [−6.7; −2.7] |
| Language region 2 | ||
| German | 0 | ref. |
| French | −2.9 | [−5.2; −0.7] |
| Italian | 0.2 | [−4.0; 4.4] |
| Age group 3 | ||
| 18–29 years | 1.1 | [−2.2; 4.4] |
| 30–44 years | 0 | ref. |
| 45–59 years | −1.8 | [−4.3; 0.7] |
| 60–75 years | −1.3 | [−4.4; 1.8] |
| BMI category 4 | ||
| Underweight (BMI < 18.5 kg/m2) | 1.2 | [−5.2; 7.6] |
| Normal (18.5 ≤ BMI < 25 kg/m2) | 0 | ref. |
| Overweight (25 ≤ BMI < 30 kg/m2) | 3.9 | [1.6; 6.1] |
| Obese (BMI ≥ 30 kg/m2) | 5.5 | [2.4; 8.7] |
| Nationality | ||
| Swiss | 0 | ref. |
| Swiss binational | 1.1 | [−1.7; 3.9] |
| Non-Swiss | −1.0 | [−3.4; 1.4] |
| Education degree | ||
| Primary | 1.9 | [−2.8; 6.6] |
| Secondary | 0 | ref. |
| Tertiary | −2.9 | [−5.0; −0.8] |
| Household status | ||
| Living alone | −0.4 | [−3.5; 2.7] |
| Adult living with parents | 3.4 | [−1.2; 7.9] |
| One-parent family with children | −2.0 | [−7.0; 3.0] |
| Couple without children | 0 | ref. |
| Couple with children | 0.5 | [−2.0; 3.1] |
| Others | 1.7 | [−2.9; 6.2] |
| Income (CHF/month) | ||
| <6000 | 0.5 | [−2.7; 3.7] |
| 6000–13,000 | 0 | ref. |
| >13,000 | 0.0 | [−2.9; 2.9] |
| Physical activity level | ||
| Low | 0 | ref. |
| Moderate | −2.3 | [−5.5; 1.0] |
| High | −2.5 | [−5.4; 0.3] |
| Smoking status | ||
| Never | 0 | ref. |
| Former | 1.8 | [−0.4; 4.0] |
| Current | 3.1 | [0.6; 5.6] |
| Health status | ||
| Very bad to medium | 0.82 | [−2.2; 3.9] |
| Good to very good | 0 | ref. |
| Currently on a diet | ||
| Yes | −7.5 | [−11.7; −3.4] |
| No | 0 | ref. |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sych, J.; Kaelin, I.; Gerlach, F.; Wróbel, A.; Le, T.; FitzGerald, R.; Pestoni, G.; Faeh, D.; Krieger, J.-P.; Rohrmann, S. Intake of Processed Meat and Association with Sociodemographic and Lifestyle Factors in a Representative Sample of the Swiss Population. Nutrients 2019, 11, 2556. https://doi.org/10.3390/nu11112556
Sych J, Kaelin I, Gerlach F, Wróbel A, Le T, FitzGerald R, Pestoni G, Faeh D, Krieger J-P, Rohrmann S. Intake of Processed Meat and Association with Sociodemographic and Lifestyle Factors in a Representative Sample of the Swiss Population. Nutrients. 2019; 11(11):2556. https://doi.org/10.3390/nu11112556
Chicago/Turabian StyleSych, Janice, Ivo Kaelin, Fabienne Gerlach, Anna Wróbel, Thu Le, Rex FitzGerald, Giulia Pestoni, David Faeh, Jean-Philippe Krieger, and Sabine Rohrmann. 2019. "Intake of Processed Meat and Association with Sociodemographic and Lifestyle Factors in a Representative Sample of the Swiss Population" Nutrients 11, no. 11: 2556. https://doi.org/10.3390/nu11112556





