The Association between Early Childhood and Later Childhood Sugar-Containing Beverage Intake: A Prospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
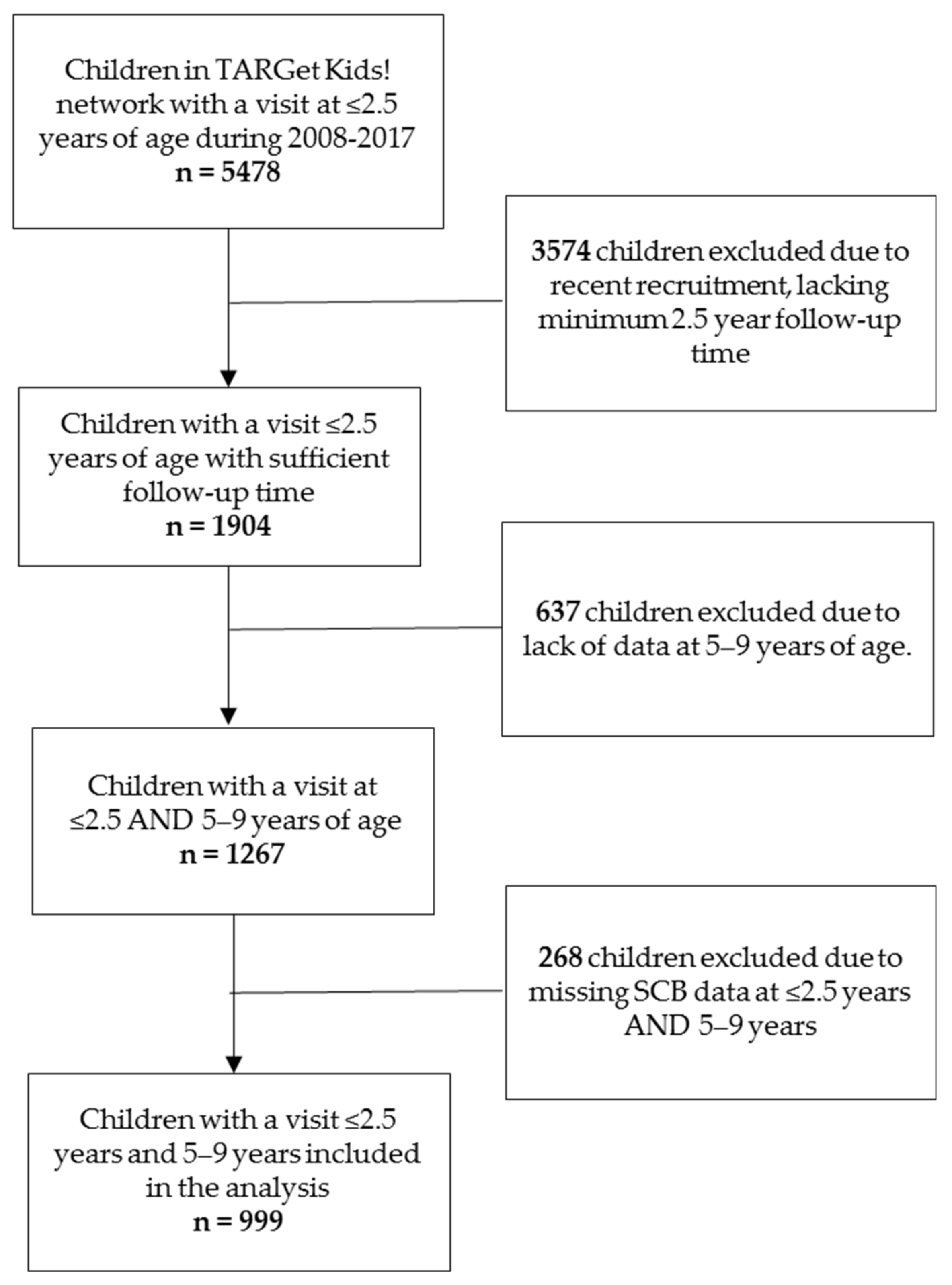
2.2. Study Population and Sample Size
2.3. Measurement of Sugar-Containing Beverage Intake
2.4. Other Variables
2.5. Statistical Analysis
3. Results
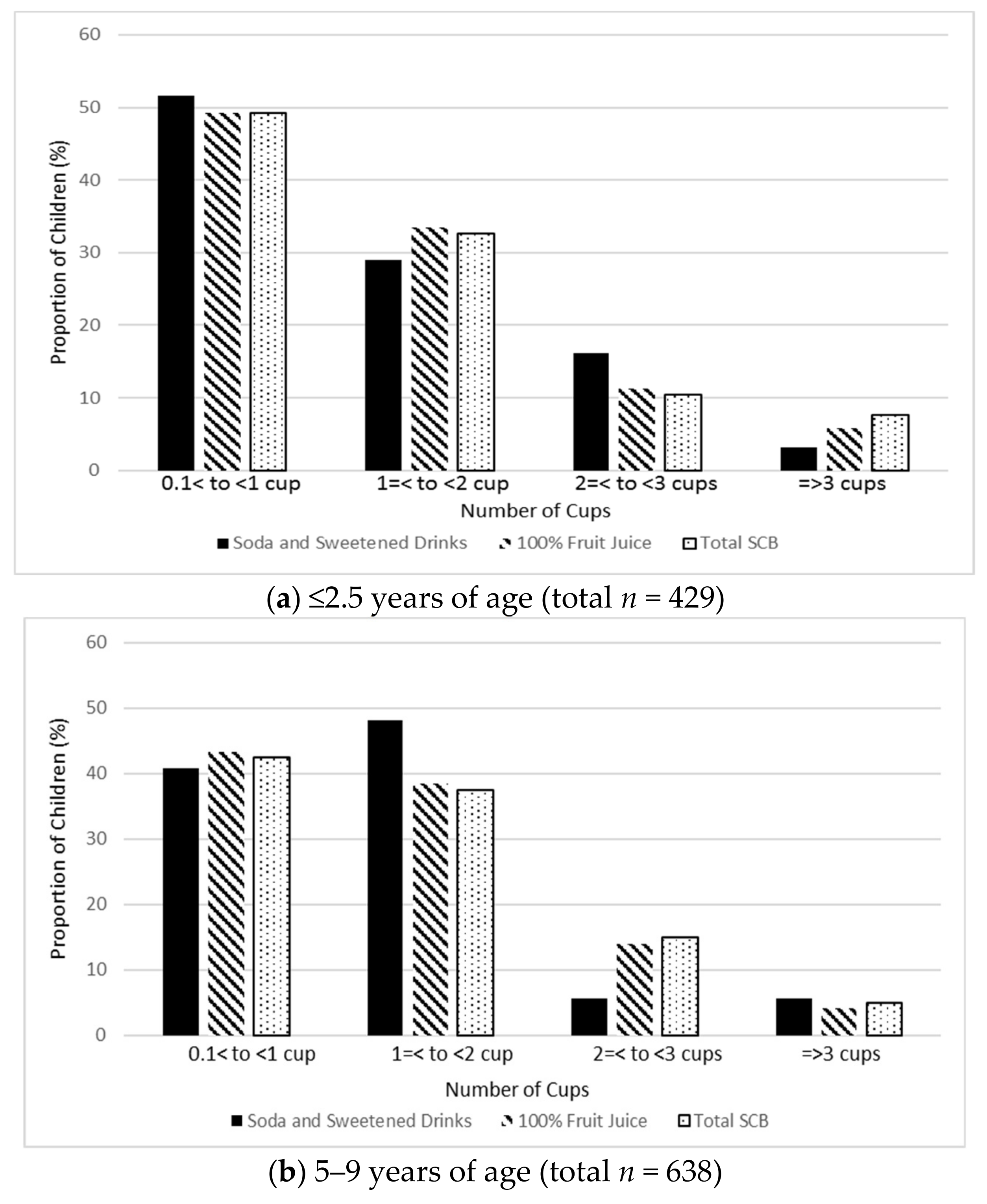
3.1. Description of SCB Consumption at ≤2.5 Years and 5–9 Years
3.2. SCB Intake at ≤2.5 Years Association with SCB Intake at 5–9 Years
3.3. Other Early Childhood Risk Factors
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Frantsve-Hawley, J.; Bader, J.D.; Welsh, J.A.; Wright, J.T. A systematic review of the association between consumption of sugar-containing beverages and excess weight gain among children under age 12. J. Public Health Dent. 2017, 77 (Suppl. S1), S43–S66. [Google Scholar] [CrossRef] [PubMed]
- Hu, F.B. Resolved: There is sufficient scientific evidence that decreasing sugar-sweetened beverage consumption will reduce the prevalence of obesity and obesity-related diseases. Obes. Rev. 2013, 14, 606–619. [Google Scholar] [CrossRef]
- Vos, M.B.; Kaar, J.L.; Welsh, J.A.; Van Horn, L.V.; Feig, D.I.; Anderson, C.A.M.; Patel, M.J.; Cruz Munos, J.; Krebs, N.F.; Xanthakos, S.A.; et al. Added Sugars and Cardiovascular Disease Risk in Children: A Scientific Statement From the American Heart Association. Circulation 2017, 135, e1017–e1034. [Google Scholar] [CrossRef] [PubMed]
- Fidler Mis, N.; Braegger, C.; Bronsky, J.; Campoy, C.; Domellöf, M.; Embleton, N.D.; Hojsak, I.; Hulst, J.; Indrio, F.; Lapillonne, A.; et al. Sugar in Infants, Children and Adolescents: A Position Paper of the European Society for Paediatric Gastroenterology, Hepatology and Nutrition Committee on Nutrition. J. Pediatr. Gastroenterol. Nutr. 2017, 65, 681–696. [Google Scholar] [CrossRef] [PubMed]
- Ambrosini, G.L.; Oddy, W.H.; Huang, R.C.; Mori, T.A.; Beilin, L.J.; Jebb, S.A. Prospective associations between sugar-sweetened beverage intakes and cardiometabolic risk factors in adolescents. Am. J. Clin. Nutr. 2013, 98, 327–334. [Google Scholar] [CrossRef]
- Kell, K.P.; Cardel, M.I.; Bohan Brown, M.M.; Fernández, J.R. Added sugars in the diet are positively associated with diastolic blood pressure and triglycerides in children. Am. J. Clin. Nutr. 2014, 100, 46–52. [Google Scholar] [CrossRef] [PubMed]
- Kosova, E.C.; Auinger, P.; Bremer, A.A. The relationships between sugar-sweetened beverage intake and cardiometabolic markers in young children. J. Acad. Nutr. Diet. 2013, 113, 219–227. [Google Scholar] [CrossRef]
- Wang, J.W.; Mark, S.; Henderson, M.; O’Loughlin, J.; Tremblay, A.; Wortman, J.; Paradis, G.; Gray-Donald, K. Adiposity and glucose intolerance exacerbate components of metabolic syndrome in children consuming sugar-sweetened beverages: QUALITY cohort study. Pediatr. Obes. 2013, 8, 284–293. [Google Scholar] [CrossRef]
- Moynihan, P.J.; Kelly, S.A. Effect on caries of restricting sugars intake: Systematic review to inform WHO guidelines. J. Dent. Res. 2014, 93, 8–18. [Google Scholar] [CrossRef]
- Scientific Advisory Committee On Nutrition. Carbohydrates and Health; The Stationary Office: London, UK, 2015; pp. 1–384. [Google Scholar]
- Malik, V.S.; Popkin, B.M.; Bray, G.A.; Després, J.P.; Willett, W.C.; Hu, F.B. Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: A meta-analysis. Diabetes Care 2010, 33, 2477–2483. [Google Scholar] [CrossRef]
- Sahoo, K.; Sahoo, B.; Choudhury, A.K.; Sofi, N.Y.; Kumar, R.; Bhadoria, A.S. Childhood obesity: Causes and consequences. J. Fam. Med. Prim. Care 2015, 4, 187–192. [Google Scholar] [CrossRef]
- Raitakari, O.T.; Juonala, M.; Kahonen, M.; Taittonen, L.; Laitinen, T.; Maki-Torkko, N.; Jarvisalo, M.J.; Uhari, M.; Jokinen, E.; Ronnemaa, T.; et al. Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood: The Cardiovascular Risk in Young Finns Study. JAMA 2003, 290, 2277–2283. [Google Scholar] [CrossRef] [PubMed]
- Nissinen, K.; Mikkilä, V.; Männistö, S.; Lahti-Koski, M.; Räsänen, L.; Viikari, J.; Raitakari, O.T. Sweets and sugar-sweetened soft drink intake in childhood in relation to adult BMI and overweight. The Cardiovascular Risk in Young Finns Study. Public Health Nutr. 2009, 12, 2018–2026. [Google Scholar] [CrossRef] [PubMed]
- Langlois, K.; Garriguet, D.; Gonzalez, A.; Sinclair, S.; Colapinto, C.K. Change in total sugars consumption among Canadian children and adults. Health Rep. 2019, 30, 10–19. [Google Scholar]
- Wang, Y.C.; Bleich, S.N.; Gortmaker, S.L. Increasing caloric contribution from sugar-sweetened beverages and 100% fruit juices among US children and adolescents, 1988-2004. Pediatrics 2008, 121, e1604–e1614. [Google Scholar] [CrossRef]
- Hamner, H.C.; Perrine, C.G.; Gupta, P.M.; Herrick, K.A.; Cogswell, M.E. Food Consumption Patterns among U.S. Children from Birth to 23 Months of Age, 2009-2014. Nutrients 2017, 9, 942. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services. 2015–2020 Dietary Guidelines for Americans. Available online: https://health.gov/dietaryguidelines/2015/guidelines/ (accessed on 10 June 2019).
- World Health Organization. Guideline: Sugar Intake for Adults and Children; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Heyman, M.B.; Abrams, S.A.; SECTION ON GASTROENTEROLOGY, HEPATOLOGY, AND NUTRITION, COMMITTEE ON NUTRITION. Fruit Juice in Infants, Children, and Adolescents: Current Recommendations. Pediatrics 2017, 139. [Google Scholar] [CrossRef]
- Health Canada. Canada’s Dietary Guidelines 2019; Health Canada: Ottawa, ON, Canada, 2019. [Google Scholar]
- Mikkilä, V.; Räsänen, L.; Raitakari, O.T.; Pietinen, P.; Viikari, J. Consistent dietary patterns identified from childhood to adulthood: The cardiovascular risk in Young Finns Study. Br. J. Nutr. 2005, 93, 923–931. [Google Scholar] [CrossRef]
- Movassagh, E.Z.; Baxter-Jones, A.D.G.; Kontulainen, S.; Whiting, S.J.; Vatanparast, H. Tracking Dietary Patterns over 20 Years from Childhood through Adolescence into Young Adulthood: The Saskatchewan Pediatric Bone Mineral Accrual Study. Nutrients 2017, 9, 990. [Google Scholar] [CrossRef]
- Kvaavik, E.; Andersen, L.F.; Klepp, K.I. The stability of soft drinks intake from adolescence to adult age and the association between long-term consumption of soft drinks and lifestyle factors and body weight. Public Health Nutr. 2005, 8, 149–157. [Google Scholar] [CrossRef]
- Bjelland, M.; Brantsæter, A.L.; Haugen, M.; Meltzer, H.M.; Nystad, W.; Andersen, L.F. Changes and tracking of fruit, vegetables and sugar-sweetened beverages intake from 18 months to 7 years in the Norwegian Mother and Child Cohort Study. BMC Public Health 2013, 13, 793. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Pan, L.; Sherry, B.; Li, R. The association of sugar-sweetened beverage intake during infancy with sugar-sweetened beverage intake at 6 years of age. Pediatrics 2014, 134, S56–S62. [Google Scholar] [CrossRef] [PubMed]
- Mazarello, P.; Hesketh, K.; O’Malley, C.; Moore, H.; Summerbell, C.; Griffin, S.; Ong, K.; Lakshman, R. Determinants of sugar-sweetened beverage consumption in young children: A systematic review. Obes. Rev. 2015, 16, 903–913. [Google Scholar] [CrossRef] [PubMed]
- Carsley, S.; Borkhoff, C.M.; Maguire, J.L.; Birken, C.S.; Khovratovich, M.; McCrindle, B.; Macarthur, C.; Parkin, P.C.; Collaboration, T.K. Cohort Profile: The Applied Research Group for Kids (TARGet Kids!). Int. J. Epidemiol. 2015, 44, 776–788. [Google Scholar] [CrossRef] [PubMed]
- Carsley, S.E.; Anderson, L.N.; Plumptre, L.; Parkin, P.C.; Maguire, J.L.; Birken, C.S. Severe Obesity, Obesity, and Cardiometabolic Risk in Children 0 to 6 Years of Age. Child. Obes. 2017, 13, 415–424. [Google Scholar] [CrossRef]
- De Onis, M. WHO Child groth standards based on length/height, weight, and age. Int. J. Paediatr. 2006, 450, 76–85. [Google Scholar]
- Skinner, J.D.; Carruth, B.R.; Bounds, W.; Ziegler, P.; Reidy, K. Do food-related experiences in the first 2 years of life predict dietary variety in school-aged children? J. Nutr. Educ. Behav. 2002, 34, 310–315. [Google Scholar] [CrossRef]
- Fiorito, L.M.; Marini, M.; Mitchell, D.C.; Smiciklas-Wright, H.; Birch, L.L. Girls’ early sweetened carbonated beverage intake predicts different patterns of beverage and nutrient intake across childhood and adolescence. J. Am. Diet. Assoc. 2010, 110, 543–550. [Google Scholar] [CrossRef]
- Teegarden, D.; Lyle, R.M.; Proulx, W.R.; Johnston, C.C.; Weaver, C.M. Previous milk consumption is associated with greater bone density in young women. Am. J. Clin. Nutr. 1999, 69, 1014–1017. [Google Scholar] [CrossRef]
- Garriguet, D. Changes in beverage consumption in Canada. Health Rep. 2019, 30, 20–30. [Google Scholar] [CrossRef]
- Lora, K.R.; Davy, B.; Hedrick, V.; Ferris, A.M.; Anderson, M.P.; Wakefield, D. Assessing Initial Validity and Reliability of a Beverage Intake Questionnaire in Hispanic Preschool-Aged Children. J. Acad. Nutr. Diet. 2016, 116, 1951–1960. [Google Scholar] [CrossRef] [PubMed]
- Lewis, K.H.; Skelton, J.A.; Hsu, F.C.; Ezouah, P.; Taveras, E.M.; Block, J.P. Implementing a novel electronic health record approach to track child sugar-sweetened beverage consumption. Prev. Med. Rep. 2018, 11, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Clemens, R.; Drewnowski, A.; Ferruzzi, M.G.; Toner, C.D.; Welland, D. Squeezing fact from fiction about 100% fruit juice. Adv. Nutr. 2015, 6, 236S–243S. [Google Scholar] [CrossRef] [PubMed]
- Government of Canada. Juice and Juice Products. Available online: http://www.inspection.gc.ca/food/requirements-and-guidance/labelling/industry/processed-fruit-or-vegetable-products/juice-and-juice-products/eng/1348153076023/1348153220895 (accessed on 19 August 2019).
- Ventura, A.K.; Mennella, J.A. Innate and learned preferences for sweet taste during childhood. Curr. Opin. Clin. Nutr. Metab. Care 2011, 14, 379–384. [Google Scholar] [CrossRef] [PubMed]
- Ventura, A.K.; Worobey, J. Early influences on the development of food preferences. Curr. Biol. 2013, 23, R401–R408. [Google Scholar] [CrossRef]
| Characteristic | n | % |
|---|---|---|
| Sex | ||
| Male | 533 | 53.4 |
| Female | 466 | 46.7 |
| Maternal Education | ||
| College/University | 917 | 91.8 |
| High school or Less | 56 | 5.6 |
| Missing | 26 | 2.6 |
| Number of Siblings | ||
| 0 | 442 | 44.2 |
| 1 | 378 | 37.8 |
| ≥2 | 107 | 10.7 |
| Missing | 72 | 7.2 |
| Family Income 1 | ||
| <$49,999 | 65 | 6.5 |
| $50,000-99,999 | 161 | 16.1 |
| $100,000-149,999 | 173 | 17.3 |
| ≥$150,000 | 555 | 55.6 |
| Missing | 45 | 4.5 |
| Child zBMI 2 | ||
| Normal and underweight (zBMI ≤ 1.0) | 790 | 79.1 |
| Risk of overweight (1 > zBMI ≤ 2.0) | 141 | 14.1 |
| Overweight and obesity (zBMI > 2) | 34 | 3.4 |
| Missing | 34 | 3.4 |
| Maternal Ethnicity | ||
| European | 729 | 73.0 |
| East, South, or South-East Asian | 135 | 13.5 |
| Other | 102 | 10.2 |
| Missing | 33 | 3.3 |
| Mean | SD | |
| Age (months) | 18.1 | 4.8 |
| Parent BMI (kg/m2) 3 | 24.6 | 4.6 |
| Typical Weekday Free Play (minutes) | 58.7 | 56.5 |
| Child zBMI | 0.09 | 1.07 |
| Breastfeeding duration (months) | 11.3 | 5.7 |
| Sugar-Containing Beverages | ≤2.5 years of age N (%) | 5–9 years of age N (%) |
|---|---|---|
| 100% Fruit Juice 1 | ||
| 0 cups/day | 564 (57.1) | 368 (37.1) |
| ≥0.5 cups/day | 424 (42.9) | 623 (62.9) |
| Soda and Sweetened Drinks 2 | ||
| 0 cups/day | 934 (96.8) | 829 (93.9) |
| ≥0.5 cups/day | 31 (3.2) | 54 (6.1) |
| Total SCB consumption | ||
| 0 cups/day | 570 (57.1) | 361 (36.1) |
| ≥0.5 cups/day | 429 (42.9) | 638 (63.9) |
| Minimally Adjusted Model Total SCB Intake at 5–9 Years of Age | Fully Adjusted Model Total SCB Intake at 5–9 Years of Age | Minimally Adjusted Model Soda and Sweetened Drink at 5–9 Years of Age | Fully Adjusted Model Soda and Sweetened drink at 5–9 Years of Age | Minimally Adjusted Model Fruit Juice Intake at 5–9 Years of Age | Fully Adjusted Model Fruit Juice Intake at 5–9 Years of Age | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR 1 | 95% CI | OR 2 | 95% CI | OR 1 | 95% CI | OR 2 | 95% CI | OR 1 | 95% CI | OR2 | 95% CI | |
| Total SCB at ≤2.5 years | ||||||||||||
| 0 cups/day | 1.00 | 1.00 | ||||||||||
| ≥0.5 cups/day | 4.33 | 3.18, 5.91 | 4.03 | 2.92, 5.55 | ||||||||
| Soda & sweetened drinks at ≤2.5 years | ||||||||||||
| 0 cups/day | 1.00 | 1.00 | ||||||||||
| ≥0.5 cups/day | 23.48 | 9.55, 57.76 | 16.91 | 3.68, 77.69 | ||||||||
| Fruit Juice at age ≤2.5 years | ||||||||||||
| 0 cups/day | 1.00 | 1.00 | ||||||||||
| ≥0.5 cups/day | 3.85 | 2.83, 5.23 | 3.61 | 2.63, 4.95 | ||||||||
| Age (months) | 1.02 | 0.99, 1.05 | 0.98 | 0.95, 1.01 | 0.99 | 0.94, 1.06 | 0.98 | 0.87, 1.09 | 0.98 | 0.95, 1.00 | 0.98 | 0.95, 1.01 |
| Sex | ||||||||||||
| Male | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Female | 1.33 | 1.01, 1.75 | 0.77 | 0.58, 1.02 | 0.67 | 0.36, 1.23 | 0.43 | 0.65, 8.21 | 0.78 | 0.59, 1.02 | 0.80 | 0.60, 1.05 |
| Education (mother) | ||||||||||||
| College/University | 1.00 | 1.00 | 1.00 | |||||||||
| Highschool or less | 1.90 | 0.89, 4.05 | 2.31 | 0.69, 4.92 | 1.26 | 0.63, 2.52 | ||||||
| Sibling | 1.20, 11.47 0.54, 11.89 | |||||||||||
| 0 | 1.00 | 1.00 | 1.00 | |||||||||
| 1 | 1.10 | 0.80, 1.50 | 3.72 | 1.15 | 0.85, 1.56 | |||||||
| 2+ | 1.14 | 0.71, 1.82 | 2.55 | 1.08 | 0.67, 1.75 | |||||||
| Ethnicity (mother) | 2.47, 22.11 0.43, 2.90 | |||||||||||
| European | 1.00 | 1.00 | 1.00 | |||||||||
| East, South or South-East Asian | 1.34 | 0.86, 2.08 | 7.39 | 1.37 | 0.88, 2.12 | |||||||
| Other | 0.93 | 0.58, 1.50 | 1.12 | 0.85 | 0.53, 1.35 | |||||||
| Household income | 0.79, 3.39 0.89, 1.80 0.82, 1.80 | 2.86, 50.09 0.38, 4.79 0.41, 5.20 | 0.82, 3.40 0.90, 2.00 0.82, 1.76 | |||||||||
| <49,999 | 1.64 | 11.96 | 1.67 | |||||||||
| 50,000–99,999 | 1.33 | 1.16 | 1.34 | |||||||||
| 100,000–149,999 | 1.22 | 1.46 | 1.19 | |||||||||
| ≥150,000 | 1.00 | 1.00 | 1.00 | |||||||||
| Child zBMI (per 1-unit increase) | 1.04 | 0.91, 1.19 | 0.79 | 0.49, 1.27 | 1.04 | 0.91, 1.20 | ||||||
| Breastfeeding duration (per 2 months increase) | 0.94 | 0.89, 0.99 | 0.89 | 0.82, 0.97 | 0.95 | 0.91, 1.01 | ||||||
| Parental BMI 3 (per 5-unit increase) | 1.12 | 0.93, 1.34 | 1.09 | 1.01, 1.18 | 1.12 | 0.94, 1.33 | ||||||
| Typical weekday free play (per 30 min increase) | 1.04 | 0.96, 1.28 | 1.00 | 1.00, 1.01 | 1.03 | 0.95, 1.13 | ||||||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ziesmann, A.; Kiflen, R.; De Rubeis, V.; Smith, B.T.; Maguire, J.L.; Birken, C.S.; Anderson, L.N., on behalf of the TARGet Kids Collaboration. The Association between Early Childhood and Later Childhood Sugar-Containing Beverage Intake: A Prospective Cohort Study. Nutrients 2019, 11, 2338. https://doi.org/10.3390/nu11102338
Ziesmann A, Kiflen R, De Rubeis V, Smith BT, Maguire JL, Birken CS, Anderson LN on behalf of the TARGet Kids Collaboration. The Association between Early Childhood and Later Childhood Sugar-Containing Beverage Intake: A Prospective Cohort Study. Nutrients. 2019; 11(10):2338. https://doi.org/10.3390/nu11102338
Chicago/Turabian StyleZiesmann, Andrea, Ruhi Kiflen, Vanessa De Rubeis, Brendan T. Smith, Jonathon L. Maguire, Catherine S. Birken, and Laura N. Anderson on behalf of the TARGet Kids Collaboration. 2019. "The Association between Early Childhood and Later Childhood Sugar-Containing Beverage Intake: A Prospective Cohort Study" Nutrients 11, no. 10: 2338. https://doi.org/10.3390/nu11102338
APA StyleZiesmann, A., Kiflen, R., De Rubeis, V., Smith, B. T., Maguire, J. L., Birken, C. S., & Anderson, L. N., on behalf of the TARGet Kids Collaboration. (2019). The Association between Early Childhood and Later Childhood Sugar-Containing Beverage Intake: A Prospective Cohort Study. Nutrients, 11(10), 2338. https://doi.org/10.3390/nu11102338




