Lactase Persistence, Milk Intake, and Adult Acne: A Mendelian Randomization Study of 20,416 Danish Adults
Abstract
:1. Introduction
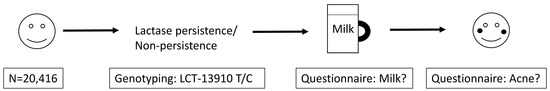
2. Materials and Methods
2.1. Participants
2.2. Milk Intake
2.3. Acne Diagnosis
2.4. Genotyping
2.5. Statistical Analyses
2.6. Meta-Analysis of Acne in Adults
3. Results
3.1. Baseline Characteristics
3.2. Milk Intake and Acne
3.3. Lactase Genotype and Milk Intake
3.4. Lactase Genotype and Acne
3.5. Meta-Analysis of Milk Intake and Adult Acne
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- White, G.M. Recent findings in the epidemiologic evidence, classification, and subtypes of acne vulgaris. J. Am. Acad. Dermatol. 1998, 39, S34–S37. [Google Scholar] [CrossRef]
- Bhate, K.; Williams, H.C. Epidemiology of acne vulgaris. Br. J. Dermatol. 2013, 168, 474–485. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gollnick, H.; Cunliffe, W.; Berson, D.; Dreno, B.; Finlay, A.; Leyden, J.J.; Shalita, A.R.; Thiboutot, D. Management of acne: A report from a Global Alliance to Improve Outcomes in Acne. J. Am. Acad. Dermatol. 2003, 49, S1–S37. [Google Scholar] [CrossRef] [PubMed]
- Ghodsi, S.Z.; Orawa, H.; Zouboulis, C.C. Prevalence, severity, and severity risk factors of acne in high school pupils: A community-based study. J. Invest. Dermatol. 2009, 129, 2136–2141. [Google Scholar] [CrossRef] [PubMed]
- Perkins, A.C.; Maglione, J.; Hillebrand, G.G.; Miyamoto, K.; Kimball, A.B. Acne vulgaris in women: Prevalence across the life span. J. Womens Health 2012, 21, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Williams, H.C.; Dellavalle, R.P.; Garner, S. Acne vulgaris. Lancet 2012, 379, 361–372. [Google Scholar] [CrossRef]
- Tuchayi, S.M.; Makrantonaki, E.; Ganceviciene, R.; Dessinioti, C.; Feldman, S.R.; Zouboulis, C.C. Acne vulgaris. Nat. Rev. Dis. Primers 2015, 1, 15029. [Google Scholar] [CrossRef] [PubMed]
- Capitanio, B.; Sinagra, J.L.; Bordignon, V.; Fei, P.C.; Picardo, M.; Zouboulis, C.C. Underestimated clinical features of postadolescent acne. J. Am. Acad. Dermatol. 2010, 63, 782–788. [Google Scholar] [CrossRef] [PubMed]
- Lichtenberger, R.; Simpson, M.A.; Smith, C.; Barker, J.; Navarini, A.A. Genetic architecture of acne vulgaris. J. Eur. Acad. Dermatol. Venereol. 2017, 31, 1978–1990. [Google Scholar] [CrossRef] [PubMed]
- Zouboulis, C.C.; Jourdan, E.; Picardo, M. Acne is an inflammatory disease and alterations of sebum composition initiate acne lesions. J. Eur. Acad. Dermatol. Venereol. 2014, 28, 527–532. [Google Scholar] [CrossRef] [PubMed]
- Adebamowo, C.A.; Spiegelman, D.; Danby, F.W.; Frazier, A.L.; Willett, W.C.; Holmes, M.D. High school dietary dairy intake and teenage acne. J. Am. Acad. Dermatol. 2005, 52, 207–214. [Google Scholar] [CrossRef] [PubMed]
- Adebamowo, C.A.; Spiegelman, D.; Berkey, C.S.; Danby, F.W.; Rockett, H.H.; Colditz, G.A.; Walter, C.W.; Michelle, D.H. Milk consumption and acne in adolescent girls. Dermatol. Online J. 2006, 12, 1. [Google Scholar] [PubMed]
- Adebamowo, C.A.; Spiegelman, D.; Berkey, C.S.; Danby, F.W.; Rockett, H.H.; Colditz, G.A.; Willett, W.C.; Holmes, M.D. Milk consumption and acne in teenaged boys. J. Am. Acad. Dermatol. 2008, 58, 787–793. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grossi, E.; Cazzaniga, S.; Crotti, S.; Naldi, L.; Di Landro, A.; Ingordo, V.; Cusano, F.; Atzori, L.; Tripodi Cutrì, F.; Musumeci, M.L.; et al. The constellation of dietary factors in adolescent acne: A semantic connectivity map approach. J. Eur. Acad. Dermatol. Venereol. 2016, 30, 96–100. [Google Scholar] [CrossRef] [PubMed]
- Karadag, A.S.; Balta, I.; Saricaoglu, H.; Kilic, S.; Kelekci, K.H.; Yildirim, M.; Arica, D.A.; Öztürk, S.; Karaman, G.; Çerman, A.A.; et al. The effect of personal, familial, and environmental characteristics on acne vulgaris: A prospective, multicenter, case controlled study from Turkey. G. Ital. Dermatol. Venereol. 2017. [Google Scholar] [CrossRef]
- Wolkenstein, P.; Machovcova, A.; Szepietowski, J.C.; Tennstedt, D.; Veraldi, S.; Delarue, A. Acne prevalence and associations with lifestyle: A cross-sectional online survey of adolescents/young adults in 7 European countries. J. Eur. Acad. Dermatol. Venereol. 2017. [Google Scholar] [CrossRef] [PubMed]
- Enattah, N.S.; Sahi, T.; Savilahti, E.; Terwilliger, J.D.; Peltonen, L.; Järvelä, I. Identification of a variant associated with adult-type hypolactasia. Nat. Genet. 2002, 30, 233–247. [Google Scholar] [CrossRef] [PubMed]
- Smith, G.D.; Ebrahim, S. Mendelian randomization: Prospects, potentials, and limitations. Int. J. Epidemiol. 2004, 33, 30–42. [Google Scholar] [CrossRef] [PubMed]
- Bergholdt, H.K.M.; Bathum, L.; Kvetny, J.; Rasmussen, D.B.; Moldow, B.; Hoeg, T.; Jemec, G.B.E.; Berner-Nielsen, H.; Nordestgaard, B.G.; Ellervik, C. Study design, participation and characteristics of the Danish General Suburban Population Study. Dan. Med. J. 2013, 60, A4693. [Google Scholar] [PubMed]
- Dalgard, F.; Svensson, A.; Holm, J.O.; Sundby, J. Self-reported skin complaints: validation of a questionnaire for population surveys. Br. J. Dermatol. 2003, 149, 794–810. [Google Scholar] [CrossRef] [PubMed]
- Bergholdt, H.K.M.; Nordestgaard, B.G.; Varbo, A.; Ellervik, C. Milk intake is not associated with ischaemic heart disease in observational or Mendelian randomization analyses in 98 529 Danish adults. Int. J. Epidemiol. 2015, 44, 587–603. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jemec, G.B.; Linneberg, A.; Nielsen, N.H.; Frolund, L.; Madsen, F.; Jorgensen, T. Have oral contraceptives reduced the prevalence of acne? A population-based study of acne vulgaris, tobacco smoking and oral contraceptives. Dermatology. 2002, 204, 179–184. [Google Scholar] [CrossRef] [PubMed]
- Alan, S.; Cenesizoglu, E. Effects of hyperandrogenism and high body mass index on acne severity in women. Saudi Med. J. 2014, 35, 886–889. [Google Scholar] [PubMed]
- Dreno, B.; Thiboutot, D.; Layton, A.M.; Berson, D.; Perez, M.; Kang, S. Large-scale international study enhances understanding of an emerging acne population: Adult females. J. Eur. Acad. Dermatol. Venereol. 2015, 29, 1096–1106. [Google Scholar] [CrossRef] [PubMed]
- Di Landro, A.; Cazzaniga, S.; Cusano, F.; Bonci, A.; Carla, C.; Musumeci, M.L.; Patrizi, A.; Bettoli, V.; Pezzarossa, E.; Caproni, M.; et al. Adult female acne and associated risk factors: Results of a multicenter case-control study in Italy. J. Am. Acad. Dermatol. 2016, 75, 1134–1141. [Google Scholar] [CrossRef] [PubMed]
- Wolkenstein, P.; Misery, L.; Amici, J.M.; Maghia, R.; Branchoux, S.; Cazeau, C.; Voisard, J.-J.; Taïeb, C. Smoking and dietary factors associated with moderate-to-severe acne in French adolescents and young adults: results of a survey using a representative sample. Dermatology 2015, 230, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Di Landro, A.; Cazzaniga, S.; Parazzini, F.; Ingordo, V.; Cusano, F.; Atzori, L.; Cutrì, F.T.; Musumeci, M.L.; Zinetti, C.; Pezzarossa, E.; et al. Family history, body mass index, selected dietary factors, menstrual history, and risk of moderate to severe acne in adolescents and young adults. J. Am. Acad. Dermatol. 2012, 67, 1129–1135. [Google Scholar] [CrossRef] [PubMed]
- Ulvestad, M.; Bjertness, E.; Dalgard, F.; Halvorsen, J.A. Acne and dairy products in adolescence: Results from a Norwegian longitudinal study. J. Eur. Acad. Dermatol. Venereol. 2017, 31, 530–545. [Google Scholar] [CrossRef] [PubMed]
- Juhl, C.R.; Berholdt, H.K.M.; Miller, I.M.; Jemec, G.B.; Kanters, J.K.; Ellervik, C. Dietary intake and acne vulgaris: a systematic review and meta-analysis of 78,529 children, adolescents, and young adults. Nutrients 2018, in press. [Google Scholar]
- Mirdamadi, Y.; Thielitz, A.; Wiede, A.; Goihl, A.; Papakonstantinou, E.; Hartig, R.; Zouboulis, C.C.; Reinhold, D.; Simeoni, L.; Bommhardt, U.; et al. Insulin and insulin-like growth factor-1 can modulate the phosphoinositide-3-kinase/Akt/FoxO1 pathway in SZ95 sebocytes in vitro. Mol. Cell Endocrinol. 2015, 415, 32–44. [Google Scholar] [CrossRef] [PubMed]
- Jansen, T.; Janssen, O.E.; Plewig, G. [Acne tarda. Acne in adults]. Hautarzt 2013, 64, 241–251. [Google Scholar] [CrossRef] [PubMed]
- Massa, A.F.; Burmeister, L.; Bass, D.; Zouboulis, C.C. Acne Fulminans: Treatment Experience from 26 Patients. Dermatology 2017, 233, 136–150. [Google Scholar] [CrossRef] [PubMed]
- Pascoe, V.L.; Kimball, A.B. Seasonal variation of acne and psoriasis: A 3-year study using the Physician Global Assessment severity scale. J. Am. Acad. Dermatol. 2015, 73, 523–535. [Google Scholar] [CrossRef] [PubMed]
- Itan, Y.; Jones, B.L.; Ingram, C.J.; Swallow, D.M.; Thomas, M.G. A worldwide correlation of lactase persistence phenotype and genotypes. BMC Evol. Biol. 2010, 10, 36. [Google Scholar] [CrossRef] [PubMed]
| All n = 20,416 100% | Acne n = 303 1.5% | Control n = 20,113 98.5% | p-Value * | Age 20–39 n = 2742 13.4% | Age > 40 n = 17,674 86.6% | p-Value * | LCT-13910 Genotype | p-Value ** | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| CC n = 1246 6.1% | TC n = 7377 36.1% | TT n = 11,793 57.8% | |||||||||
| Acne, n (%) | 303 (1.5) | - | - | - | 141 (5.1) | 162 (0.9) | <0.0001 | 20 (1.6) | 119 (1.6) | 164 (1.4) | 0.4523 |
| Age, mean (SD), years | 56.3 (13.6) | 44.2 (13.2) | 56.5 (13.5) | <0.0001 | 35.0 (4.0) | 59.7 (11.3) | <0.0001 | 55.7 (13.2) | 56.4 (13.6) | 56.4 (13.6) | 0.1892 |
| Age: 20–39, n (%) | 2742 (13.4) | 141 (46.5) | 2601 (12.9) | <0.0001 | - | - | - | 166 (6.1) | 955 (34.8) | 1621 (59.1) | 0.2851 |
| Age: > 40, n (%) | 17674 (86.6) | 162 (53.5) | 17512 (87.1) | <0.0001 | - | - | - | 1080 (6.1) | 6422 (36.3) | 10172 (57.6) | |
| Men, n (%) | 9294 (45.5) | 125 (41.3) | 9169 (44.9) | 0.1327 | 1193 (43.5) | 8101 (45.8) | 0.0228 | 540 (43.3) | 3332 (45.2) | 5422 (46.0) | 0.1522 |
| Body Mass Index, mean (SD), kg/m2 | 26.7 (4.7) | 26.9 (5.6) | 26.7 (4.7) | 0.4549 | 25.9 (4.9) | 26.9 (4.6) | <0.0001 | 26.5 (4.7) | 26.6 (4.6) | 26.8 (4.7) | 0.0290 |
| Current Smoker, n (%) | 3632 (17.8) | 75 (24.8) | 3557 (17.7) | 0.0014 | 490 (17.9) | 3142 (17.8) | 0.9060 | 233 (18.7) | 1318 (17.9) | 2081 (17.7) | 0.6371 |
| Milk Intake, mean (SD), glasses/week | 8.1 (9.1) | 10.2 (14.3) | 8.1 (9.0) | <0.0001 | 11.0 (9.9) | 7.7 (8.9) | <0.0001 | 6.1 (7.1) | 8.2 (9.1) | 8.3 (9.4) | <0.0001 |
| Milk Intake (glasses/week) | Female | Male | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n Total | n Acne | Unadjusted | Adjusted * | n Total | n Acne | Unadjusted | Adjusted * | |||||
| OR [95% CI] | p | OR [95% CI] | p | OR [95% CI] | p | OR [95% CI] | p | |||||
| 0 | 172 | 11 | 1.00 | - | 1.00 | - | 122 | 8 | 1.00 | - | 1.00 | - |
| 1–3 | 274 | 19 | 1.09 [0.51:2.35] | 0.82 | 0.98 [0.45:2.13] | 0.96 | 147 | 4 | 0.40 [0.12:1.36] | 0.14 | 0.43 [0.13:1.47] | 0.18 |
| 4–7 | 375 | 25 | 1.05 [0.50:2.18] | 0.91 | 0.98 [0.47:2.06] | 0.96 | 186 | 11 | 0.90 [0.35:2.29] | 0.82 | 0.93 [0.36:2.41] | 0.89 |
| 8–14 | 397 | 25 | 0.98 [0.47:2.05] | 0.96 | 0.90 [0.43:1.90] | 0.79 | 322 | 7 | 0.32 [0.11:0.89] | 0.03 | 0.36 [0.13:1.02] | 0.06 |
| >14 | 331 | 20 | 0.94 [0.44:2.01] | 0.88 | 0.85 [0.39:1.83] | 0.67 | 416 | 11 | 0.39 [0.15:0.98] | 0.05 | 0.40 [0.16:1.02] | 0.05 |
| Any | 1377 | 89 | 1.01 [0.53:1.93] | 0.97 | 0.93 [0.48:1.78] | 0.82 | 1071 | 33 | 0.45 [0.20:1.00] | 0.05 | 0.49 [0.22:1.08] | 0.08 |
| Low-fat ** | 1348 | 85 | 0.83 [0.47:1.48] | 0.53 | 0.84 [0.47:1.52] | 0.57 | 1031 | 31 | 0.47 [0.23:0.98] | 0.04 | 0.49 [0.23:1.03] | 0.06 |
| High-fat *** | 58 | 7 | 2.06 [0.91:4.67] | 0.08 | 1.42 [0.55:3.69] | 0.47 | 82 | 5 | 1.94 [0.74:5.08] | 0.18 | 2.01 [0.75:5.38] | 0.17 |
| Milk Intake (glasses/week) | Female | Male | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n Total | n Acne | Unadjusted | Adjusted * | n Total | n Acne | Unadjusted | Adjusted * | |||||
| OR [95% CI] | p | OR [95% CI] | p | OR [95% CI] | p | OR [95% CI] | p | |||||
| 0 | 2802 | 17 | 1.00 | - | 1.00 | - | 2099 | 20 | 1.00 | - | 1.00 | - |
| 1–3 | 1564 | 16 | 1.69 [0.85:3.36] | 0.13 | 1.30 [0.65:2.59] | 0.46 | 1099 | 10 | 0.95 [0.45:2.05] | 0.90 | 0.91 [0.42:1.96] | 0.80 |
| 4–7 | 2129 | 22 | 1.71 [0.91:3.23] | 0.10 | 1.40 [0.74:2.65] | 0.31 | 1592 | 13 | 0.86 [0.42:1.73] | 0.66 | 0.82 [0.40:1.68] | 0.59 |
| 8–14 | 1816 | 11 | 1.00 [0.47:2.14] | 1.00 | 0.76 [0.35:1.63] | 0.48 | 1682 | 23 | 1.44 [0.79:2.63] | 0.23 | 1.31 [0.71:2.43] | 0.39 |
| >14 | 1262 | 12 | 1.57 [0.75:3.30] | 0.23 | 1.13 [0.53:2.40] | 0.75 | 1629 | 18 | 1.16 [0.61:2.20] | 0.65 | 0.99 [0.51:1.91] | 0.97 |
| Any | 6771 | 61 | 1.49 [0.87:2.55] | 0.15 | 1.15 [0.66:1.99] | 0.62 | 6002 | 64 | 1.12 [0.68:1.86] | 0.66 | 1.02 [0.61:1.72] | 0.94 |
| Low-fat ** | 6324 | 58 | 1.49 [0.90:2.49] | 0.12 | 1.14 [0.68:1.91] | 0.63 | 5268 | 57 | 1.14 [0.72:1.80] | 0.59 | 0.98 [0.61:1.58] | 0.94 |
| High-fat *** | 590 | 4 | 0.82 [0.30:2.26] | 0.70 | 0.97 [0.35:2.68] | 0.95 | 901 | 10 | 1.08 [0.56:2.10] | 0.82 | 1.25 [0.64:2.46] | 0.51 |
| LCT-13910 Genotype | Lactase | n | % | Median | IQR | Kruskal-Wallis Test | |
|---|---|---|---|---|---|---|---|
| Age Group 20–39 Years | |||||||
| CC | Non-persistent | 166 | 6 | 7 | [2:14] | Chi-Square | 14.73 |
| TC | Persistent | 955 | 35 | 10 | [3:16] | DF | 2 |
| TT | Persistent | 1621 | 59 | 10 | [4:16] | P | 6.32 × 10−4 |
| Age Group ≥ 40 Years | |||||||
| CC | Non-persistent | 1080 | 6 | 3 | [0:14] | Chi-Square | 52.83 |
| TC | Persistent | 6422 | 36 | 6 | [0:14] | DF | 2 |
| TT | Persistent | 10,172 | 58 | 5 | [0:10] | P | 3.38 × 10−12 |
| Median Milk Intake [IQR] | |||||
|---|---|---|---|---|---|
| LCT-13910 C/T Genotype | Glasses/Week | n Total | n Acne | OR [95% CI] | p-Value |
| Age Group 20–39 Years | |||||
| CC | 7 [2:14] | 166 | 10 | 1 | - |
| TC | 10 [3:16] | 955 | 50 | 0.86 [0.43:1.74] | 0.68 |
| TT | 10 [4:16] | 1621 | 81 | 0.82 [0.42:1.62] | 0.57 |
| TC/TT | 10 [3:16] | 2576 | 131 | 0.84 [0.43:1.62] | 0.60 |
| LCT gene (additive model) × milk (no/yes) interaction test LCT gene (dominant model) × milk (no/yes) interaction test | 0.36 | ||||
| 0.15 | |||||
| Age Group ≥ 40 Years | |||||
| CC | 3 [0:10] | 1080 | 10 | 1 | - |
| TC | 6 [0:14] | 6422 | 69 | 1.16 [0.60:2.26] | 0.67 |
| TT | 5 [0:14] | 10,172 | 83 | 0.88 [0.46:1.70] | 0.70 |
| TC/TT | 5 [0:14] | 16,594 | 152 | 0.99 [0.52:1.88] | 0.97 |
| LCT gene (additive model) × milk (no/yes) interaction test LCT gene (dominant model) × milk (no/yes) interaction test | 0.32 | ||||
| 0.37 | |||||
| Dairy | Author | Year | OR | Low 95% CI | Upper 95% CI | p-Value |
|---|---|---|---|---|---|---|
| Any intake | Di Landro [25] | 2016 | 0.88 | 0.61 | 1.28 | 0.52 |
| Any intake | Juhl | Current | 1.27 | 0.84 | 1.92 | 0.26 |
| Fixed effects pooled odds ratio | 1.04 | 0.79 | 1.37 | 0.78 | ||
| Random effects pooled odds ratio | 1.05 | 0.74 | 1.49 | 0.80 | ||
| Whole milk | Di Landro [25] | 2016 | 0.84 | 0.49 | 1.44 | 0.53 |
| Whole milk | Juhl | Current | 1.43 | 0.76 | 2.70 | 0.27 |
| Fixed effects pooled odds ratio | 1.05 | 0.70 | 1.58 | 0.82 | ||
| Random effects pooled odds ratio | 1.07 | 0.64 | 1.79 | 0.81 | ||
| Low-fat milk | Di Landro [25] | 2016 | 0.90 | 0.61 | 1.32 | 0.59 |
| Low-fat milk | Juhl | Current | 1.15 | 0.79 | 1.68 | 0.47 |
| Fixed effects pooled odds ratio | 1.02 | 0.78 | 1.34 | 0.89 | ||
| Random effects pooled odds ratio | 1.02 | 0.78 | 1.34 | 0.89 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Juhl, C.R.; Bergholdt, H.K.M.; Miller, I.M.; Jemec, G.B.E.; Kanters, J.K.; Ellervik, C. Lactase Persistence, Milk Intake, and Adult Acne: A Mendelian Randomization Study of 20,416 Danish Adults. Nutrients 2018, 10, 1041. https://doi.org/10.3390/nu10081041
Juhl CR, Bergholdt HKM, Miller IM, Jemec GBE, Kanters JK, Ellervik C. Lactase Persistence, Milk Intake, and Adult Acne: A Mendelian Randomization Study of 20,416 Danish Adults. Nutrients. 2018; 10(8):1041. https://doi.org/10.3390/nu10081041
Chicago/Turabian StyleJuhl, Christian R., Helle K. M. Bergholdt, Iben M. Miller, Gregor B. E. Jemec, Jørgen K. Kanters, and Christina Ellervik. 2018. "Lactase Persistence, Milk Intake, and Adult Acne: A Mendelian Randomization Study of 20,416 Danish Adults" Nutrients 10, no. 8: 1041. https://doi.org/10.3390/nu10081041
APA StyleJuhl, C. R., Bergholdt, H. K. M., Miller, I. M., Jemec, G. B. E., Kanters, J. K., & Ellervik, C. (2018). Lactase Persistence, Milk Intake, and Adult Acne: A Mendelian Randomization Study of 20,416 Danish Adults. Nutrients, 10(8), 1041. https://doi.org/10.3390/nu10081041