Movement Disorders Related to Gluten Sensitivity: A Systematic Review
Abstract
:1. Introduction
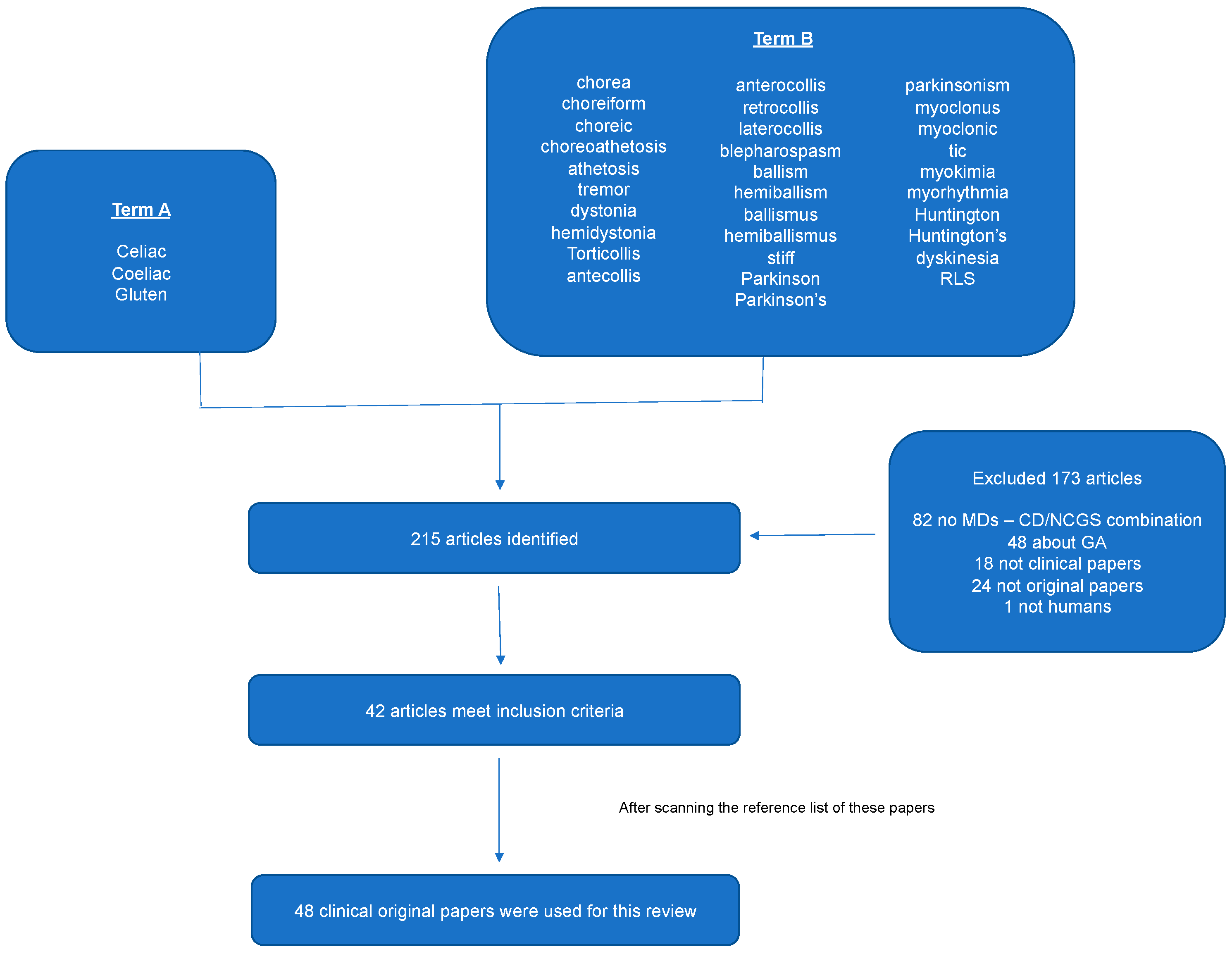
2. Materials and Methods
2.1. Literature and Search Strategy
2.2. Inclusion and Exclusion Criteria
- To be original clinical papers.
- To study human subjects.
- To involve single cases, case series, or retrospective observational studies with the combination of CD or GS and MDs.
- Reviews, book chapters, letters to editors, and editorials that are not providing new data.
- Papers referring only to GA.
3. Results
3.1. Search Results
3.2. Chorea
3.3. Restless Legs Syndrome
3.4. Myoclonus
3.5. Palatal Tremor
3.6. Dystonia
3.7. Postural Tremor
3.8. Stiff-Person Syndrome
3.9. Parkinsonism
3.10. Tics
3.11. Other Movement Disorders
3.11.1. Opsoclonus-Myoclonus
3.11.2. Propiospinal Myoclonus
3.11.3. Paroxysmal Dyskinesia
3.11.4. Myorhythmia
3.11.5. Myokymia
4. Conclusions
- GS and CD should be considered in the diagnostic workup of MDs of unknown etiology in patients of all ages and both genders, even in the absence of GI symptoms.
- Neurologic manifestations, including MDs, may precede the diagnosis of GS and CD.
- Some of the MDs may improve or resolve after dietary gluten removal, so early diagnosis should rapidly lead to the implementation of GFD.
- Once GFD is implemented, it should generally continue lifelong like in CD. In fact, in some cases, sporadic accidental gluten ingestion continues to trigger the MD.
- In contrast, other types of MDs, such as ataxia with myoclonus, appear to be linked to refractory CD and when observed, there is prompt need for repeat biopsy of the small intestine and often aggressive immunosuppression.
- The fact that the majority of the included papers refer to CD rather than the broader spectrum of GS may mean that the relationship of MDs to GS without enteropathy is under-studied.
Author Contributions
Funding
Conflicts of Interest
References
- Kang, J.Y.; Kang, A.H.Y.; Green, A.; Gwee, K.A.; Ho, K.Y. Systematic review: Worldwide variation in the frequency of coeliac disease and changes over time. Aliment. Pharmacol. Ther. 2013, 38, 226–245. [Google Scholar] [CrossRef] [PubMed]
- Daum, S.; Cellier, C.; Mulder, C.J. Refractory coeliac disease. Best Pract. Res. Clin. Gastroenterol. 2005, 19, 413–424. [Google Scholar] [CrossRef] [PubMed]
- Gobbi, G.; Ambrosetto, P.; Zaniboni, M.G.; Lambertini, A.; Ambrosioni, G.; Tassinari, C.A. Celiac disease, posterior cerebral calcifications and epilepsy. Brain Dev. 1992, 14, 23–29. [Google Scholar] [CrossRef]
- Chapman, R.W.; Laidlow, J.M.; Colin-Jones, D.; Eade, O.E.; Smith, C.L. Increased prevalence of epilepsy in coeliac disease. Br. Med. J. 1978, 2, 250–251. [Google Scholar] [CrossRef] [PubMed]
- Hadjivassiliou, M.; Grünewald, R.A.; Lawden, M.; Davies-Jones, G.A.B.; Powell, T.; Smith, C.M.L. Headache and CNS white matter abnormalities associated with gluten sensitivity. Neurology 2001, 56, 385–388. [Google Scholar] [CrossRef] [PubMed]
- Kieslich, M.; Errázuriz, G.; Posselt, H.G.; Moeller-Hartmann, W.; Zanella, F.; Boehles, H. Brain white-matter lesions in celiac disease: A prospective study of 75 diet-treated patients. Pediatrics 2001, 108, E21. [Google Scholar] [CrossRef] [PubMed]
- Hadjivassiliou, M.; Chattopadhyay, A.K.; Grünewald, R.A.; Jarratt, J.A.; Kandler, R.H.; Rao, D.G.; Sanders, D.S.; Wharton, S.B.; Davies-Jones, G.A. Myopathy associated with gluten sensitivity. Muscle Nerve 2007, 35, 443–450. [Google Scholar] [CrossRef] [PubMed]
- Ludvigsson, J.F.; Olsson, T.; Ekbom, A.; Montgomery, S.M. A population-based study of coeliac disease, neurodegenerative and neuroinflammatory diseases. Aliment. Pharmacol. Ther. 2007, 25, 1317–1327. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chin, R.L.; Sander, H.W.; Brannagan, T.H. Celiac neuropathy. Neurology 2003, 60, 1581–1585. [Google Scholar] [CrossRef] [PubMed]
- Zis, P.; Rao, D.G.; Sarrigiannis, P.G.; Aeschlimann, P.; Aeschlimann, D.P.; Sanders, D.; Grünewald, R.A.; Hadjivassiliou, M. Transglutaminase 6 antibodies in gluten neuropathy. Dig. Liver Dis. 2017, 49, 1196–1200. [Google Scholar] [CrossRef] [PubMed]
- Zis, P.; Sarrigiannis, P.G.; Rao, D.G.; Hadjivassiliou, M. Quality of life in patients with gluten neuropathy. Nutrients 2018, 10, 662. [Google Scholar] [CrossRef] [PubMed]
- Baizabal-carvallo, J.F.; Jankovic, J. Movement disorders in autoimmune diseases. Mov. Disord. 2012, 27, 935–946. [Google Scholar] [CrossRef] [PubMed]
- Zis, P.; Argiriadou, V.; Temperikidis, P.P.; Zikou, L.; Tzartos, S.J.; Tavernakis, A. Parkinson’s disease associated with myasthenia gravis and rheumatoid arthritis. Neurol. Sci. 2014, 35, 797–799. [Google Scholar] [CrossRef] [PubMed]
- Hadjivassiliou, M.; Sanders, D.D.; Aeschlimann, D.P. Gluten-related disorders: Gluten ataxia. Dig. Dis. 2015, 33, 264–268. [Google Scholar] [CrossRef] [PubMed]
- Hadjivassiliou, M.; Sanders, D.S.; Woodroofe, N.; Williamson, C.; Grünewald, R.A. Gluten ataxia. Cerebellum 2008, 7, 494–498. [Google Scholar] [CrossRef] [PubMed]
- Higgins, D.S. Chorea and its disorders. Neurol. Clin. 2001, 19, 707–722. [Google Scholar] [CrossRef]
- Shannon, K.M. Treatment of chorea. Contin. Lifelong Learn. Neurol. 2007, 13, 72–93. [Google Scholar] [CrossRef]
- Piccolo, I.; Defanti, C.A.; Soliveri, P. Cause and course in a series of patients with sporadic chorea. J. Neurol. 2003, 250, 429–435. [Google Scholar] [CrossRef] [PubMed]
- Wild, E.J.; Tabrizi, S.J. The differential diagnosis of chorea. Pract. Neurol. 2007, 7, 360–373. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Willis, A.J.; Turner, B.; Lock, R.J.; Johnston, S.L.; Unsworth, D.J.; Fry, L. Dermatitis herpetiformis and neurological dysfunction. J. Neurol. Neurosurg. Psychiatry 2002, 72, 259–261. [Google Scholar] [CrossRef] [Green Version]
- Shulman, L.; Singer, C.; Weiner, W. Phenytoin-induced focal chorea. Mov. Disord. 1996, 11, 111–114. [Google Scholar] [CrossRef] [PubMed]
- Haider, Y.; Abbot, R. Phenytoin-induced choreoathetosis. Postgr. Med. J. 1990, 66, 1089–1990. [Google Scholar] [CrossRef]
- Pereira, A.C.; Edwards, M.J.; Buttery, P.C.; Hawkes, C.H.; Quinn, N.P.; Giovannoni, G.; Hadjivassiliou, M.; Bhatia, K.P. Chorewic syndrome and coeliac disease: A hitherto unrecognised association. Mov. Disord. 2004, 19, 478–481. [Google Scholar] [CrossRef] [PubMed]
- Andrade, C.; Rocha, H.; Albuquerque, A.; Sá, M.J. Gluten chorea. Clin. Neurol. Neurosurg. 2015, 138, 8–9. [Google Scholar] [CrossRef] [PubMed]
- Walker, R.H. Further evidence for coeliac disease-associated chorea? Tremor Other Hyperkinet. Mov. 2011, 1, 1–3. [Google Scholar] [CrossRef]
- Kitiyakara, T.; Jackson, M.; Gorard, D.A. Refractory coeliac disease, small bowel lymphoma and chorea. J. R. Soc. Med. 2002, 95, 133–134. [Google Scholar] [CrossRef] [PubMed]
- Allen, R.P.; Picchietti, D.; Hening, W.A.; Trenkwalder, C.; Walters, A.S.; Montplaisi, J. The participants in the Restless Legs Syndrome Diagnosis and Epidemiology workshop at the National Institutes of Health in collaboration with members of the International Restless Legs Syndrome Study Group. Restless legs syndrome: Diagnostic criteria, special considerations, and epidemiology. A report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Med. 2003, 4, 101–109. [Google Scholar] [PubMed]
- Allen, R.P.; Picchietti, D.L.; Garcia-Borreguero, D.; Ondo, W.G.; Walters, A.S.; Winkelman, J.W.; Zucconi, M.; Ferri, R.; Trenkwalder, C. Restless legs syndrome/Willis-Ekbom disease diagnostic criteria: Updated International Restless Legs Syndrome Study Group (IRLSSG) consensus criteria-history, rationale, description and significance. Sleep Med. 2014, 15, 860–873. [Google Scholar] [CrossRef] [PubMed]
- Hening, W.; Walters, A.S.; Allen, R.P.; Montplaisir, J.; Myers, A.; Ferini-Strambi, L. Impact, diagnosis and treatment of restless legs syndrome (RLS) in a primary care population: The REST (RLS epidemiology, symptoms, and treatment) primary care study. Sleep Med. 2004, 5, 237–246. [Google Scholar] [CrossRef] [PubMed]
- Allen, R. Dopamine and iron in the pathophysiology of restless leg syndrome (RLS). Sleep Med. 2004, 5, 385–391. [Google Scholar] [CrossRef] [PubMed]
- Sun, E.R.; Chen, C.A.; Ho, G.; Earley, C.J.; Allen, R.P. Iron and the restless leg syndrome. Sleep 1998, 21, 381–387. [Google Scholar] [CrossRef]
- Allen, R.P.; Auerbach, S.; Auerbach, M.; Earley, C.J. The prevalence and impact of restless legs syndrome on patients with iron deficiency anemia. Am. J. Hematol. 2013, 88, 261–264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Manchanda, S.; Davies, C.R.; Picchietti, D. Celiac disease as a possible cause for low serum ferritin in patients with restless legs syndrome. Sleep Med. 2009, 10, 763–765. [Google Scholar] [CrossRef] [PubMed]
- Weinstock, L.B.; Walters, A.S.; Mullin, G.E.; Duntley, S.P. Celiac disease is associated with restless legs syndrome. Dig. Dis. Sci. 2010, 55, 1667–1673. [Google Scholar] [CrossRef] [PubMed]
- Moccia, M.; Pellecchia, M.T.; Erro, R.; Zingone, F.; Marelli, S.; Barone, D.G.; Ciacci, C.; Strambi, L.F.; Barone, P. Restless legs syndrome is a common feature of adult celiac disease. Mov. Disord. 2010, 25, 877–881. [Google Scholar] [CrossRef] [PubMed]
- Cikrikcioglu, M.A.; Halac, G.; Hursitoglu, M.; Erkal, H.; Cakirca, M.; Kinas, B.E.; Erek, A.; Yetmis, M.; Gundogan, E.; Tukek, T. Prevalence of gluten sensitive enteropathy antibodies in restless legs syndrome. Acta Neurol. Belg. 2011, 111, 282–286. [Google Scholar] [PubMed]
- Marsden, C.; Hallett, M.; Fahn, S. The nosology and pathophysiology of myoclonus. Mov. Disord. 1982, 2, 196–248. [Google Scholar]
- Caviness, J.N.; Alving, L.I.; Maraganore, D.M.; Black, R.A.; McDonnell, S.K.; Rocca, W.A. The incidende and prevalence of myoclonus in Olmsted County, Minnesota. Mayo Clin. Proc. 1999, 74, 565–569. [Google Scholar] [CrossRef] [PubMed]
- Marsden, C.D.; Harding, A.E.; Obeso, J.A.; Lu, C. Progressive Myoclonic Ataxia (The Ramsay Hunt Syndrome). Arch. Neurol. 1990, 47, 1121–1125. [Google Scholar] [CrossRef] [PubMed]
- Cooke, W.; Smith, W. Neurological disorders associated with coeliac disease. Brain 1966, 89, 683–722. [Google Scholar] [CrossRef] [PubMed]
- Finelli, P.F.; McEntee, W.J.; Ambler, M.; Kestenbaum, D. Adult celiac-disease presenting as cerebellar syndrome. Neurology 1980, 30, 245–249. [Google Scholar] [CrossRef] [PubMed]
- Kinney, H.C.; Burger, P.C.; Hurwitz, B.J.; Hijmans, J.C.; Grant, J.P. Degeneration of the central nervous system associated with celiac disease. J. Neurol. Sci. 1982, 53, 9–22. [Google Scholar] [CrossRef]
- Chinnery, P.F.; Reading, P.J.; Milne, D.; Gardner-Medwin, D.; Turnbull, D.M. CSF antigliadin antibodies and the Ramsay Hunt syndrome. Neurology 1997, 49, 1131–1134. [Google Scholar] [CrossRef] [PubMed]
- Hanagasi, H.A.; Gürol, E.; Sahin, H.A.; Emre, M. Atypical neurological involvement associated with celiac disease. Eur. J. Neurol. 2001, 8, 67–69. [Google Scholar] [CrossRef] [PubMed]
- Tüzün, E.; Gürses, C.; Baykan, B.; Büyükbabani, N.; Oztür, A.S.; Gökyigit, A. Lafora body-like inclusions in a case of progressive myoclonic ataxia associated with coeliac disease. Eur. Neurol. 2001, 46, 157–158. [Google Scholar] [CrossRef] [PubMed]
- Sallem, F.S.; Castro, L.M.; Jorge, C.; Marchiori, P.; Barbosa, E. Gluten Sensitivity Presenting as Myoclonic Epilepsy with Cerebellar Syndrome. Mov. Disord. 2009, 24, 2162–2163. [Google Scholar] [CrossRef] [PubMed]
- Siqueira Neto, J.I.; Costa, A.C.; Magalhaes, F.G.; Silva, G.S. Neurological manifestations of celiac disease. Arq. Neuropsiquiatr. 2004, 62, 969–972. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lu, C.S.; Thompson, P.D.; Quinn, N.P.; Parkes, J.D.; Marsden, C.D. Ramsay Hunt syndrome and coeliac disease: A new association? Mov. Disord. 1986, 1, 209–219. [Google Scholar] [CrossRef] [PubMed]
- Smith, G.D.; Saldanha, G.; Britton, T.C.; Brown, P. Neurological manifestations of coeliac disease. J. Neurol. Neurosurg. Psychiatry 1997, 63, 550–551. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tison, F.; Arne, P.; Henry, P. Myoclonus and adult coeliac disease. J. Neurol. 1989, 236, 307–308. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, K.P.; Brown, P.; Gregory, R.; Lennox, G.G.; Manji, H.; Thompson, P.D.; Ellison, D.W.; Marsden, C.D. Progressive myoclonic ataxia associated with coeliac disease: The myoclonus is of cortical origin, but the pathology is in the cerebellum. Brain 1995, 118, 1087–1093. [Google Scholar] [CrossRef] [PubMed]
- Tijssen, M.A.; Thom, M.; Ellison, D.W.; Wilkins, P.; Barnes, D.; Thompson, P.D.; Brown, P. Cortical myoclonus and cerebellar pathology. Neurology 2000, 54, 1350–1356. [Google Scholar] [CrossRef] [PubMed]
- Javed, S.; Safdar, A.; Forster, A.; Selvan, A.; Chadwick, D.; Nicholson, A.; Jacob, A. refractory coeliac disease associated with late onset epilepsy, ataxia, tremor and progressive myoclonus with giant cortical evoked potentials-A case report and review of literature. Seizure 2012, 21, 482–485. [Google Scholar] [CrossRef] [PubMed]
- Sarrigiannis, P.G.; Hoggard, N.; Aeschlimann, D.; Sanders, D.S.; Grünewald, R.A.; Unwin, Z.C.; Hadjivassiliou, M. Myoclonus ataxia and refractory coeliac disease. Cerebellum & Ataxias 2014, 1, 11. [Google Scholar] [CrossRef]
- Samuel, M.; Torun, N.; Tuite, P.J.; Sharpe, J.A.; Lang, A.E. Progressive ataxia and palatal tremor (PAPT): Clinical and MRI assessment with review of palatal tremors. Brain 2004, 127, 1252–1268. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kheder, A.; Currie, S.; Romanowski, C.; Hadjivassiliou, M. Progressive ataxia with palatal tremor due to gluten sensitivity. Mov. Disord. 2012, 27, 62–63. [Google Scholar] [CrossRef] [PubMed]
- Balint, B.; Bhatia, K.P. Dystonia: An update on phenomenology, classification, ptahogenesis and treatment. Curr. Opin. Neurol. 2014, 27, 468–476. [Google Scholar] [CrossRef] [PubMed]
- Steeves, T.D.; Day, L.; Dykeman, J.; Jette, N.; Pringsheim, T. The prevalence of primary dystonia: A systematic review and meta-analysis. Mov. Disord. 2012, 27, 1789–1796. [Google Scholar] [CrossRef] [PubMed]
- Kaji, R.; Bhatia, K.; Graybiel, A.M. Pathogenesis of dystonia: Is it of cerebellar or basal ganglia origin? J. Neurol. Neurosurg. Psychiatry 2018, 89, 488–492. [Google Scholar] [CrossRef] [PubMed]
- Fung, V.S.; Duggins, A.; Morris, J.G.; Lorentz, I.T. Progressive Myoclonic Ataxia Associated With Celiac Disease Presenting as Unilateral Cortical Tremor and Dystonia. Mov. Disord. 2000, 15, 732–734. [Google Scholar] [CrossRef]
- Bürk, K.; Fareki, M.L.; Lamprecht, G.; Roth, G.; Decker, P.; Weller, M.; Rammensee, H.G.; Oertel, W. Neurological symptoms in patients with biopsy proven celiac disease. Mov. Disord. 2009, 24, 2358–2362. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wittstock, M.; Grossmann, A.; Kunesch, E. Symptomatic vascular dystonia in Celiac disease. Mov. Disord. 2006, 21, 427–429. [Google Scholar] [CrossRef] [PubMed]
- Deuschl, G.; Bain, P.; Brin, M. Consensus statement of the movement disorder society on tremor. Mov. Disord. 1998, 13, 2–23. [Google Scholar] [CrossRef] [PubMed]
- Hermaszewski, R.A.; Rigby, S.; Dalgleish, A.G. Coeliac disease presenting with cerebellar degeneration. Postgrad. Med. J. 1991, 67, 1023–1024. [Google Scholar] [CrossRef] [PubMed]
- Luostarinen, L.; Himanen, S.L.; Luostarinen, M.; Collin, P.; Pirttilä, T. Neuromuscular and sensory disturbances in patients with well treated coeliac disease. J. Neurol. Neurosurg. Psychiatry 2003, 74, 490–494. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Habek, M.; Hojsak, I.; Barun, B.; Brinar, V.V. Downbeat nystagmus, ataxia and spastic tetraparesis due to coeliac disease. Neurol. Sci. 2011, 32, 911–914. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hernández-Lahoz, C.; Rodrigo-Sáez, L.; Vega-Villar, J.; Mauri-Capdevila, G.; Mier-Juanes, J. Familial gluten ataxia. Mov. Disord. 2014, 29, 308–310. [Google Scholar] [CrossRef] [PubMed]
- Sharma, P.; Sharma, S.; Panwar, N.; Mahto, D.; Kumar, P.; Kumar, A.; Aneja, S. Central pontine myelinolysis presenting with tremor in a child with celiac disease. J. Child Neurol. 2014, 29, 381–384. [Google Scholar] [CrossRef] [PubMed]
- Meinck, H.M.; Thompson, P.D. Stiff man syndrome and related conditions. Mov. Disord. 2002, 17, 853–866. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, E.P.; Behan, L.A.; King, T.F.J.; Hardiman, O.; Smith, D. A case of stiff-person syndrome, type 1 diabetes, celiac disease and dermatitis herpetiformis. Clin. Neurol. Neurosurg. 2009, 111, 384–386. [Google Scholar] [CrossRef] [PubMed]
- Bilic, E.; Bilic, E.; Sepec, B.I.; Vranjes, D.; Zagar, M.; Butorac, V.; Cerimagic, D. Stiff-person syndrome in a female patient with type 1 diabetes, dermatitis herpetiformis, celiac disease, microcytic anemia and copper deficiency Just a coincidence or an additional shared pathophysiological mechanism? Clin. Neurol. Neurosurg. 2009, 111, 644–645. [Google Scholar] [CrossRef] [PubMed]
- Soós, Z.; Salamon, M.; Erdei, K.; Kaszás, N.; Folyovich, A.; Szücs, A.; Barcs, G.; Arányi, Z.; Skaliczkis, J.; Vadasdi, K. LADA type diabetes, celiac disease, cerebellar ataxia and stiff person syndrome. A rare association of autoimmune disorders. Ideggyogy. Sz. 2014, 67, 205–209. [Google Scholar] [PubMed]
- Dalakas, M.C. Stiff person syndrome: Advances in pathogenesis and therapeutic interventions. Curr. Treat. Opt. Neurol. 2009, 11, 102–110. [Google Scholar] [CrossRef] [PubMed]
- Hadjivassiliou, M.; Gibson, A.; Davies-Jones, G.A.B.; Lobo, A.J.; Stephenson, T.J.; Milford-Ward, A. Does cryptic gluten sensitivity play a part in neurological illness? Lancet 1996, 347, 369–371. [Google Scholar] [CrossRef]
- Hadjivassiliou, M.; Grünewald, R.A.; Davies-Jones, G.A.B. Gluten sensitivity as a neurological illness. J. Neurol. Neurosurg. Psychiatry 2002, 72, 560–563. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hadjivassiliou, M.; Williamson, C.; Grûnewald, R.A.; Davies-Jones, G.A.B.; Sanders, D.S.; Sharrack, B.; Woodroofe, N. Glutamic acid Decarboxylase as a Target Antigen in Gluten Sensitivity: The Link to Neurological Manifestation? Available online: https://jnnp.bmj.com/content/76/1/150 (accessed on 7 August 2018).
- Hadjivassiliou, M.; Aeschlimann, D.; Grünewald, R.A.; Sanders, D.S.; Sharrack, B.; Woodroofe, N. GAD antibody-associated neurological illness and its relationship to gluten sensitivity. Acta. Neurol. Scand. 2011, 123, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Wickremaratchi, M.M.; Perera, D.; O’Loghlen, C.; Sastry, D.; Morgan, E.; Jones, A.; Edwards, P.; Robertson, N.P.; Butler, C.; Morris, H.R.; et al. Prevalence and age of onset of Parkinson’s disease in Cardiff: A community based cross sectional study and meta-analysis. J. Neurol. Neurosurg. Psychiatry 2009, 80, 805–807. [Google Scholar] [CrossRef] [PubMed]
- Jankovic, J.; Lang, A.E. Movement Disorders: Diagnosis and Assessment, 5th ed.; Butterworth-Heinemann: Philadelphia, PA, USA, 2008. [Google Scholar]
- Di Lazzaro, V.; Capone, F.; Cammarota, G.; Di Giud, D.; Ranieri, F. Dramatic improvement of parkinsonian symptoms after gluten-free diet introduction in a patient with silent celiac disease. J. Neurol. 2014, 261, 443–445. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez Aleman, G.; Florenzano, N.; Padilla, E.; Bourdieu, M.; Guerrero, G.; Calvó, M.; Alberio, G.; Strejilevich, S.; de Erausquin, G.A. A 37-year-old woman with celiac disease, recurrent psychosis, and Parkinsonism. Mov. Disord. 2006, 21, 729–731. [Google Scholar] [CrossRef] [PubMed]
- Singer, H.S. Tourette syndrome and other tic disorders. Hanb. Clin. Neurol. 2011, 100, 641–657. [Google Scholar] [CrossRef]
- Cath, D.C.; Hedderly, T.; Ludolph, A.G. European clinical guidelines for Tourette syndrome and other tic disorders. Part I: Assessment. Eur. Child Adolesc. Psychiatry 2011, 20, 155–171. [Google Scholar] [CrossRef] [PubMed]
- Knight, T.; Steeves, T.; Day, L.; Lowerison, M.; Jette, N.; Pringsheim, T. Prevalence of tic disorders: A systematic review and meta-analysis. Pediatr. Neurol. 2012, 47, 77–90. [Google Scholar] [CrossRef] [PubMed]
- Zelnik, N.; Pacht, A.; Obeid, R.; Lerner, A. Range of neurologic disorders in patients with celiac disease. Pediatrics 2004, 113, 1672–1676. [Google Scholar] [CrossRef] [PubMed]
- Jankovic, J. Diagnosis and classification of tics and Tourette syndrome. Adv. Neurol. 1992, 58, 7–14. [Google Scholar] [PubMed]
- Rodrigo, L.; Huerta, M.; Salas-Puig, J. Tourette syndrome and non-celiac gluten sensitivity. Clinical remission with a gluten-free diet: A description case. J. Sleep Disord. Ther. 2015, 4, 183. [Google Scholar] [CrossRef]
- Rodrigo, L.; Nuria, Á.; Fern, E.; Salas-puig, J.; Huerta, M.; Hern, C. Efficacy of a Gluten-Free Diet in the Gilles de la Tourette Syndrome: A Pilot Study. Nutrients 2018, 10, 573. [Google Scholar] [CrossRef] [PubMed]
- Kinsbourne, M. Myoclonic encephalopathy of infants. J. Neurol. Neurosurg. Psychiatry 1962, 25, 271–276. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leigh, R.J.; Zee, D.S. The Neurology of Eye Movements; Oxford University Press: Philadelphia, PA, USA, 1991. [Google Scholar]
- Leigh, R.J.; Averbuch-Heller, L.; Tomsak, R.L. Treatment of abnormal eye movements that impair vision. Strategies based on current concepts of physiology and pharmacology. Ann. Neurol. 1994, 36, 129–141. [Google Scholar] [CrossRef] [PubMed]
- Deconinck, N.; Scaillon, M.; Segers, V.; Groswasser, J.J.; Dan, B. Opsoclonus-Myoclonus Associated with Celiac Disease. Pediatr. Neurol. 2006, 34, 312–314. [Google Scholar] [CrossRef] [PubMed]
- Brown, P.; Thompson, P.D.; Rothwell, J.C.; Day, B.L.; Marsden, C.D. Axial myoclonus of propiospinal origin. Brain 1991, 114, 197–214. [Google Scholar] [PubMed]
- Roze, E.; Bounolleau, P.; Ducreux, D.; Cochen, V.; Leu-Semenescu, S.; Beaugendre, Y. Propiospinal myoclonus revisited: Clinical, neurophysiologic, and neuroradiologic findings. Neurology 2009, 72, 1301–1309. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Menkes, D.L.; Silvers, D.S. Propriospinal myoclonus associated with gluten sensitivity in a young woman. J. Neurol. Sci. 2012, 315, 141–142. [Google Scholar] [CrossRef] [PubMed]
- Fahn, S. The paroxysmal dyskinesias. In Movement Disorders; Oxford University Press: Oxford, UK, 1994; pp. 310–345. [Google Scholar]
- Blakeley, J.; Jankovic, J. Secondary Paroxysmal Dyskinesias. Mov. Disord. 2002, 17, 726–734. [Google Scholar] [CrossRef] [PubMed]
- Hall, D.A.; Parsons, J.; Benke, T. Paroxysmal nonkinesigenic dystonia and celiac disease. Mov. Disord. 2007, 22, 708–710. [Google Scholar] [CrossRef] [PubMed]
- Masucci, E.F.; Kurtzke, J.F.; Saini, N. Myorhythmia: A widespread movement disorder. Clinicopathological correlations. Brain 1984, 107, 53–79. [Google Scholar] [CrossRef] [PubMed]
- Dimberg, E.L.; Crowe, S.E.; Trugman, J.M.; Swerdlow, R.H.; Lopes, M.B.; Bourne, T.D.; Burns, T.M. Fatal encephalitis in a patient with refractory celiac disease presenting with myorhythmia and carpal spasm. Mov. Disord. 2007, 22, 407–411. [Google Scholar] [CrossRef] [PubMed]
- Gutmann, L.; Gutmann, L. Myokymia and neuromyotonia 2004. J. Neurol. 2004, 251, 138–142. [Google Scholar] [CrossRef] [PubMed]
- Beydoun, S.R.; Copeland, D.D.; Korula, J. Generalized Myokymia as a Unique Association with Gluten-Sensitive Enteropathy. Eur. Neurol. 2000, 44, 254–255. [Google Scholar] [CrossRef] [PubMed]
| Number of Papers Related to Each Movement Disorder (%) | |
| Chorea | 5 (11%) |
| Restless leg syndrome | 4 (8%) |
| Myoclonus | 15 (31%) |
| Palatal tremor | 3 (6%) |
| Dystonia | 3 (6%) |
| Tremor | 5 (11%) |
| Stiff Person Syndrome | 2 (5%) |
| Parkinsonism | 3 (6%) |
| Tics | 3 (6%) |
| Other less commonly reported movement disorders | |
| Opsoclonus-myoclonus | 1 (2%) |
| Propiospinal myoclonus | 1 (2%) |
| Paroxysmal dyskinesia | 1 (2%) |
| Myorhythmia | 1 (2%) |
| Myokymia | 1(2%) |
| Demographics | |
| Female to male ratio | 7:2 |
| Mean age (SD), in years | 44.6 (22.7) |
| Types of Publications | |
| Case reports | 30 |
| Case series | 8 |
| Retrospective observational studies | 9 |
| Prospective pilot study | 1 |
| Year of Publication | |
| Range | 1966–2018 |
| Number of Publications per Decade | |
| Until 1990 | 5 |
| 1991–2000 | 9 |
| 2001–2010 | 20 |
| 2011–2018 | 14 |
| Movement Disorder | Number of Cases of Patients Published until the Date | Male:Female | Mean Age of Onset (SD)/Age of Onset | Response to GFD E, S, N, L | HLA DQ2/DQ8 | CD:GS |
|---|---|---|---|---|---|---|
| Chorea | 8 | 1:7 | 57.4 (12.9) | E 5 (62.5%) S 2 (25%) L 1 (12.5%) | DQ2(+) 2 (25%) DQ2(-) 2 (25%) NA (50%) | 5:3 |
| RLS | 65 | 6:59 | NA | E 18 (28%) N 16 (25%) L 31 (47%) | NA | 65:0 |
| Myoclonus | 28 | 15:13 | 47.7 (17.3) | S 1 (3%) N 28 (97%) | NA | 28:0 |
| Palatal tremor | 3 | 1:2 | 51.3 (8.1) | E 1 (33%) N 2 (67%) | DQ2(+) 1 (33%) NA: 2 (67%) | 1:2 |
| Dystonia | 2 | 1:1 | 49.50 (2.1) | N 2 (100%) | NA | 2:0 |
| Tremor | 9 | 3:6 | 54.6 (14.9) | E 6 (67%) N 3 (33%) | DQ2(+) 6 (67%) NA: 3 (33%) | 9:0 |
| Parkinsonism | 3 | 0:3 | 54.0 (18.7) | E 1 (33%) N 2 (67%) | NA | 3:0 |
| Tics | 1 | 0:1 | 13 | E (100%) | DQ8(+) 1 (100%) | 0:1 |
| OM | 1 | 1:0 | 2 | E (100%) | NA | 1:0 |
| PSM | 1 | 0:1 | 23 | E (100%) | NA | 1:0 |
| Paroxysmal dyskinesia | 1 | 0:1 | 0.5 | E (100%) | NA | 1:0 |
| Myorhythmia | 1 | 0:1 | 68 | N (100%) | DQ2 (+) 1 (100%) | 1:0 |
| Myokymia | 1 | 0:1 | 72 | N (100%) | NA | 1:0 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vinagre-Aragón, A.; Zis, P.; Grunewald, R.A.; Hadjivassiliou, M. Movement Disorders Related to Gluten Sensitivity: A Systematic Review. Nutrients 2018, 10, 1034. https://doi.org/10.3390/nu10081034
Vinagre-Aragón A, Zis P, Grunewald RA, Hadjivassiliou M. Movement Disorders Related to Gluten Sensitivity: A Systematic Review. Nutrients. 2018; 10(8):1034. https://doi.org/10.3390/nu10081034
Chicago/Turabian StyleVinagre-Aragón, Ana, Panagiotis Zis, Richard Adam Grunewald, and Marios Hadjivassiliou. 2018. "Movement Disorders Related to Gluten Sensitivity: A Systematic Review" Nutrients 10, no. 8: 1034. https://doi.org/10.3390/nu10081034
APA StyleVinagre-Aragón, A., Zis, P., Grunewald, R. A., & Hadjivassiliou, M. (2018). Movement Disorders Related to Gluten Sensitivity: A Systematic Review. Nutrients, 10(8), 1034. https://doi.org/10.3390/nu10081034






