Interactions between Vitamin D Status, Calcium Intake and Parathyroid Hormone Concentrations in Healthy White-Skinned Pregnant Women at Northern Latitude
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Biochemical Analysis
2.2.1. Serum 25(OH)D
2.2.2. Serum PTH
2.2.3. Serum Calcium
2.3. Statistical Analysis
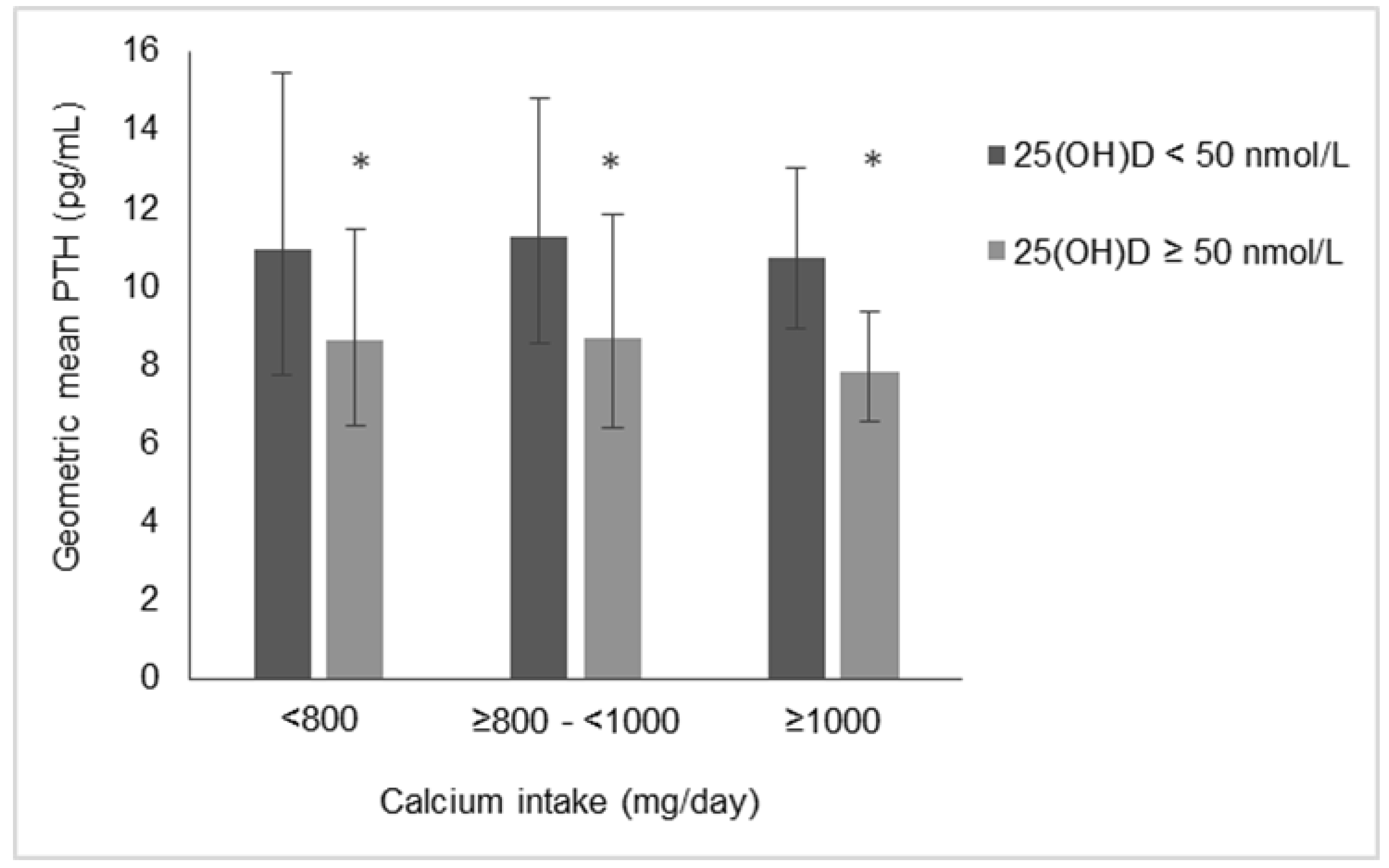
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Haider, B.A.; Bhutta, Z.A. Multiple-micronutrient supplementation for women during pregnancy. Cochrane Database Syst. Rev. 2017, 4, CD004905. [Google Scholar] [CrossRef] [PubMed]
- Saraf, R.; Morton, S.M.; Camargo, C.A., Jr.; Grant, C.C. Global summary of maternal and newborn vitamin D status—A systematic review. Matern. Child Nutr. 2016, 12, 647–668. [Google Scholar] [CrossRef] [PubMed]
- Vinkhuyzen, A.A.E.; Eyles, D.W.; Burne, T.H.; Blanken, L.M.E.; Kruithof, C.J.; Verhulst, F.; Jaddoe, V.W.; Tiemeier, H.; McGrath, J.J. Prevalence and predictors of vitamin D deficiency based on maternal mid-gestation and neonatal cord bloods: The generation R study. J. Steroid Biochem. Mol. Biol. 2016, 164, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Bärebring, L.; Schoenmakers, I.; Glantz, A.; Hulthén, L.; Jagner, A.; Ellis, J.; Bärebring, M.; Bullarbo, M.; Augustin, H. Vitamin D status during pregnancy in a multi-ethnic population-representative Swedish cohort. Nutrients 2016, 8, 655. [Google Scholar] [CrossRef] [PubMed]
- Kiely, M.E.; Zhang, J.Y.; Kinsella, M.; Khashan, A.S.; Kenny, L.C. Vitamin D status is associated with uteroplacental dysfunction indicated by pre-eclampsia and small-for-gestational-age birth in a large prospective pregnancy cohort in Ireland with low vitamin D status. Am. J. Clin. Nutr. 2016, 104, 354–361. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kiely, M.; O’Donovan, S.M.; Kenny, L.C.; Hourihane, J.O.; Irvine, A.D.; Murray, D.M. Vitamin D metabolite concentrations in umbilical cord blood serum and associations with clinical characteristics in a large prospective mother-infant cohort in Ireland. J. Steroid Biochem. Mol. Biol. 2017, 167, 162–168. [Google Scholar] [CrossRef] [PubMed]
- Haggarty, P.; Campbell, D.M.; Knox, S.; Horgan, G.W.; Hoad, G.; Boulton, E.; McNeill, G.; Wallace, A.M. Vitamin D in pregnancy at high latitude in Scotland. Br. J. Nutr. 2013, 109, 898–905. [Google Scholar] [CrossRef] [PubMed]
- Roth, D.E.; Leung, M.; Mesfin, E.; Qamar, H.; Watterworth, J.; Papp, E. Vitamin D supplementation during pregnancy: State of the evidence from a systematic review of randomised trials. BMJ 2017, 359, j5237. [Google Scholar] [CrossRef] [PubMed]
- De-Regil, L.M.; Palacios, C.; Lombardo, L.K.; Peña-Rosas, J.P. Vitamin D supplementation for women during pregnancy. Cochrane Database Syst. Rev. 2016, 1, CD008873. [Google Scholar]
- Aghajafari, F.; Nagulesapillai, T.; Ronksley, P.E.; Tough, S.C.; O’Beirne, M.; Rabi, D.M. Association between maternal serum 25-hydroxyvitamin D level and pregnancy and neonatal outcomes: Systematic review and meta-analysis of observational studies. BMJ 2013, 346, f1169. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D; Ross, A.C., Taylor, C.L., Yaktine, A.L., Valle, H.B.D.V., Eds.; National Academies Press: Washington, DC, USA, 2011; pp. 35–345. [Google Scholar]
- Nordic Council of Ministers. Nordic Nutrition Recommendations 2012, 5th ed.; Narayana Press: Copenhagen, Denmark, 2014. [Google Scholar]
- European Food Safety Authority. Scientific opinion on dietary reference values for vitamin D. EFSA J. 2016, 14, 4547. [Google Scholar]
- O’Callaghan, K.M.; Hennessy, Á.; Hull, G.L.; Healy, K.; Ritz, C.; Kenny, L.C.; Cashman, K.D.; Kiely, M.E. Estimation of the maternal vitamin D intake that maintains circulating 25-hydroxyvitamin D in late gestation at a concentration sufficient to keep umbilical cord sera ≥25–30 nmol/L: A dose-response, double-blind, randomized placebo-controlled trial in pregnant women at northern latitude. Am. J. Clin. Nutr. 2018, 108, 77–91. [Google Scholar] [PubMed]
- March, K.M.; Chen, N.N.; Karakochuk, C.D.; Shand, A.W.; Innis, S.M.; von Dadelszen, P.; Barr, S.I.; Lyon, M.R.; Whiting, S.J.; Weiler, H.A.; et al. Maternal vitamin D3 supplementation at 50 μg/d protects against low serum 25-hydroxyvitamin D in infants at 8 wk of age: A randomized controlled trial of 3 doses of vitamin D beginning in gestation and continued in lactation. Am. J. Clin. Nutr. 2015, 102, 402–410. [Google Scholar] [CrossRef] [PubMed]
- Prentice, A. Mining the depths: Metabolic insights into mineral nutrition. Proc. Nutr. Soc. 2007, 66, 512–521. [Google Scholar] [CrossRef] [PubMed]
- Redmond, J.; Jarjou, L.M.; Zhou, B.; Prentice, A.; Schoenmakers, I. Ethnic differences in calcium, phosphate and bone metabolism. Proc. Nutr. Soc. 2014, 73, 340–351. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hofmeyr, G.J.; Lawrie, T.A.; Atallah, A.N.; Duley, L.; Torloni, M.R. Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems. Cochrane Database Syst. Rev. 2014, 6, CD001059. [Google Scholar] [CrossRef] [PubMed]
- Brannon, P.M.; Picciano, M.F. Vitamin D in pregnancy and lactation in humans. Annu. Rev. Nutr. 2011, 31, 89–115. [Google Scholar] [CrossRef] [PubMed]
- Møller, U.K.; Streym, S.; Mosekilde, L.; Heickendorff, L.; Flyvbjerg, A.; Frystyk, J.; Jensen, L.T.; Rejnmark, L. Changes in calcitropic hormones, bone markers and insulin-like growth factor I (IGF-I) during pregnancy and postpartum: A controlled cohort study. Osteoporos Int. 2013, 24, 1307–1320. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, S.A.; McNeil, R.; Hollis, B.W.; Davis, D.J.; Winkler, J.; Cook, C.; Warner, G.; Bivens, B.; McShane, P.; Wagner, C.L. Profound vitamin D deficiency in a diverse group of women during pregnancy living in a sun-rich environment at latitude 32 °N. Int. J. Endocrinol. 2010, 917428. [Google Scholar] [CrossRef] [PubMed]
- Prentice, A. Vitamin D deficiency: A global perspective. Nutr. Rev. 2008, 66, S153–S164. [Google Scholar] [CrossRef] [PubMed]
- Lips, P. Vitamin D deficiency and secondary hyperparathyroidism in the elderly: Consequences for bone loss and fractures and therapeutic implications. Endocr. Rev. 2001, 22, 477–501. [Google Scholar] [CrossRef] [PubMed]
- Hemmingway, A.; Kenny, L.C.; Malvisi, L.; Kiely, M.E. Exploring the concept of functional vitamin D deficiency in pregnancy: impact of the interaction between 25-hydroxyvitamin D and parathyroid hormone on perinatal outcomes. Am. J. Clin. Nutr 2018, in press. [Google Scholar]
- Scholl, T.O.; Chen, X.; Stein, T.P. Vitamin D, secondary hyperparathyroidism, and preeclampsia. Am. J. Clin. Nutr. 2013, 98, 787–793. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cashman, K.D.; Hill, T.R.; Lucey, A.J.; Taylor, N.; Seamans, K.M.; Muldowney, S.; Fitzgerald, A.P.; Flynn, A.; Barnes, M.S.; Horigan, G.; et al. Estimation of the dietary requirement for vitamin D in healthy adults. Am. J. Clin. Nutr. 2008, 88, 1535–1542. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cashman, K.D.; Wallace, J.M.; Horigan, G.; Hill, T.R.; Barnes, M.S.; Lucey, A.J.; Bonham, M.P.; Taylor, N.; Duffy, E.M.; Seamans, K.; et al. Estimation of the dietary requirement for vitamin D in free-living adults ≥64 y of age. Am. J. Clin. Nutr. 2009, 89, 1366–1374. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mortensen, C.; Damsgaard, C.T.; Hauger, H.; Ritz, C.; Lanham-New, S.A.; Smith, T.J.; Hennessy, Á.; Dowling, K.; Cashman, K.D.; Kiely, M.; et al. Estimation of the dietary requirement for vitamin D in white children aged 4–8 y: A randomized, controlled, dose-response trial. Am. J. Clin. Nutr. 2016, 104, 1310–1317. [Google Scholar] [CrossRef] [PubMed]
- Smith, T.J.; Tripkovic, L.; Damsgaard, C.T.; Molgaard, C.; Ritz, C.; Wilson-Barnes, S.L.; Dowling, K.G.; Hennessy, Á.; Cashman, K.D.; Kiely, M.; et al. Estimation of the dietary requirement for vitamin D in adolescents aged 14–18 y: A dose-response, double-blind, randomized placebo-controlled trial. Am. J. Clin. Nutr. 2016, 104, 1301–1309. [Google Scholar] [CrossRef] [PubMed]
- Kiely, M.; Collins, A.; Lucey, A.J.; Andersen, R.; Cashman, K.D.; Hennessy, Á. Development, validation and implementation of a quantitative food frequency questionnaire to assess habitual vitamin D intake. J. Hum. Nutr. Diet. 2016, 29, 495–504. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goltzman, D. Approach to Hypercalcemia; de Groot, L.J., Chrousos, G., Dungan, K., Eds.; Endotext: South Dartmouth, MA, USA, 2016. [Google Scholar]
- Holick, M.F.; Binkley, N.C.; Bischoff-Ferrari, H.A.; Gordon, C.M.; Hanley, D.A.; Heaney, R.P.; Murad, M.H.; Weaver, C.M.; Endocrine Society. Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 2011, 96, 1911–1930. [Google Scholar] [CrossRef] [PubMed]
- Black, L.J.; Walton, J.; Flynn, A.; Cashman, K.D.; Kiely, M. Small increments in vitamin D intake by Irish adults over a decade show that strategic initiatives to fortify the food supply are needed. J. Nutr. 2015, 145, 969–976. [Google Scholar] [CrossRef] [PubMed]
- Irish University Nutrition Alliance. National Adult Nutrition Survey: Summary Report, 2011. National Food Consumption Surveys in Ireland. 2011. Available online: https://www.iuna.net/surveyreports (accessed on 1 June 2018).
- Joy, E.J.; Ander, E.L.; Young, S.D.; Black, C.R.; Watts, M.J.; Chilimba, A.D.; Chilima, B.; Siyame, E.W.; Kalimbira, A.A.; Hurst, R.; et al. Dietary mineral supplies in Africa. Physiol. Plant 2014, 151, 208–229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kumssa, D.B.; Joy, E.J.; Ander, E.L.; Watts, M.J.; Young, S.D.; Walker, S.; Broadley, M.R. Dietary calcium and zinc deficiency risks are decreasing but remain prevalent. Sci. Rep. 2015, 5, 10974. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kiely, M.; Hemmingway, A.; O’Callaghan, K.M. Vitamin D in pregnancy: current perspectives and future directions. Ther. Adv. Musculoskelet. Dis. 2017, 9, 145–154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jorde, R.; Sundsfjord, J.; Haug, E.; Bonaa, K.H. Relation between low calcium intake, parathyroid hormone, and blood pressure. Hypertension 2000, 35, 1154–1159. [Google Scholar] [CrossRef] [PubMed]
- Steingrimsdottir, L.; Gunnarsson, O.; Indridason, O.S.; Franzson, L.; Sigurdsson, G. Relationship between serum parathyroid hormone levels, vitamin D sufficiency, and calcium intake. JAMA 2005, 294, 2336–2341. [Google Scholar] [CrossRef] [PubMed]
- Joo, N.S.; Dawson-Hughes, B.; Kim, Y.S.; Oh, K.; Yeum, K.J. Impact of calcium and vitamin D insufficiencies on serum parathyroid hormone and bone mineral density: Analysis of the fourth and fifth Korea national health and nutrition examination survey. J. Bone Miner. Res. 2013, 28, 764–770. [Google Scholar] [CrossRef] [PubMed]
- Cashman, K.D.; Hayes, A.; O’Donovan, S.M.; Zhang, J.Y.; Kinsella, M.; Galvin, K.; Kiely, M.; Seamans, K.M. Dietary calcium does not interact with vitamin D3 in terms of determining the response and catabolism of serum 25-hydroxyvitamin D during winter in older adults. Am. J. Clin. Nutr. 2014, 99, 1414–1423. [Google Scholar] [CrossRef] [PubMed]
- Young, B.E.; McNanley, T.J.; Cooper, E.M.; McIntyre, A.W.; Witter, F.; Harris, Z.L.; O’Brien, K.O. Maternal vitamin D status and calcium intake interact to affect fetal skeletal growth in utero in pregnant adolescents. Am. J. Clin. Nutr. 2012, 95, 1103–1112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pettifor, J.M. Calcium and vitamin D metabolism in children in developing countries. Ann. Nutr. Metab. 2014, 64 (Suppl. 2), 15–22. [Google Scholar] [CrossRef] [PubMed]
- Jarjou, L.M.A.; Prentice, A.; Sawo, Y.; Laskey, M.A.; Bennett, J.; Goldberg, G.R.; Cole, T.J. Randomized, placebo-controlled, calcium supplementation study in pregnant Gambian women: Effects on breast-milk calcium concentrations and infant birth weight, growth, and bone mineral accretion in the first year of life. Am. J. Clin. Nutr. 2006, 83, 657–666. [Google Scholar] [CrossRef] [PubMed]
- Jarjou, L.M.; Laskey, M.A.; Sawo, Y.; Goldberg, G.R.; Cole, T.J.; Prentice, A. Effect of calcium supplementation in pregnancy on maternal bone outcomes in women with a low calcium intake. Am. J. Clin. Nutr. 2010, 92, 450–457. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scholl, T.O.; Chen, X.; Stein, T.P. Maternal calcium metabolic stress and fetal growth. Am. J. Clin. Nutr. 2014, 99, 918–925. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Calvo, M.S.; Uribarri, J. Public health impact of dietary phosphorus excess on bone and cardiovascular health in the general population. Am. J. Clin. Nutr. 2013, 98, 6–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Castiglioni, S.; Cazzaniga, A.; Albisetti, W.; Maier, J.A. Magnesium and osteoporosis: Current state of knowledge and future research directions. Nutrients 2013, 5, 3022–3033. [Google Scholar] [CrossRef] [PubMed]
- Ahmadieh, H.; Arabi, A. Vitamins and bone health: Beyond calcium and vitamin D. Nutr. Rev. 2011, 69, 584–598. [Google Scholar] [CrossRef] [PubMed]
- Gröber, U.; Reichrath, J.; Holick, M.F.; Kisters, K. Vitamin K: An old vitamin in a new perspective. Dermatoendocrinol. 2014, 6, e968490. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez, O.M.; Farwell, W.R.; Kermah, D.; Taylor, E.N. Racial differences in the relationship between vitamin D, bone mineral density, and parathyroid hormone in the National Health and Nutrition Examination Survey. Osteoporos. Int. 2011, 22, 1745–1753. [Google Scholar] [CrossRef] [PubMed]
- Aloia, J.F.; Chen, D.G.; Chen, H. The 25(OH)D/PTH threshold in black women. J. Clin. Endocrinol. Metab. 2010, 95, 5069–5073. [Google Scholar] [CrossRef] [PubMed]
- O’Callaghan, K.M.; Kiely, M.E. Ethnic disparities in the dietary requirement for vitamin D during pregnancy: Considerations for nutrition policy and research. Proc. Nutr. Soc. 2018, 77, 164–173. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Value |
|---|---|
| Age (years) | 33.4 ± 3.8 |
| BMI (kg/m2) | 25.8 ± 4.3 |
| Nulliparous | 32.4 (46) |
| University Education | 70.4 (100) |
| Winter season at baseline visit 1 | 77.5 (110) |
| Gestational Age at visit (weeks) | 14.3 ± 1.8 |
| Vitamin D supplement user | 68.3 (97) |
| Calcium supplement user | 23.2 (33) |
| Vitamin D intake (μg/day) 2 | 10.7 ± 5.2 |
| Calcium intake (mg/day) 2 | 1182 ± 488 |
| Serum 25(OH)D (nmol/L) | 54.9 ± 22.6 |
| Serum PTH (pg/mL) | 9.2 (8.4, 10.2) |
| Serum calcium (mmol/L) 3 | 2.2 ± 0.1 |
| 25(OH)D | Serum Calcium 1 | Vitamin D Intake 2 | Calcium Intake 2 | ||
|---|---|---|---|---|---|
| PTH | r | −0.311 | 0.057 | −0.132 | −0.087 |
| (p-value) | (<0.001) | (0.499) | (0.118) | (0.306) | |
| 25(OH)D | r | −0.092 | 0.372 | 0.064 | |
| (p-value) | (0.276) | (<0.001) | (0.448) | ||
| Serum calcium 1 | r | 0.058 | 0.064 | ||
| (p-value) | (0.493) | (0.450) | |||
| Vitamin D intake 2 | r | 0.194 | |||
| (p-value) | (0.021) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hemmingway, A.; O’Callaghan, K.M.; Hennessy, Á.; Hull, G.L.J.; Cashman, K.D.; Kiely, M.E. Interactions between Vitamin D Status, Calcium Intake and Parathyroid Hormone Concentrations in Healthy White-Skinned Pregnant Women at Northern Latitude. Nutrients 2018, 10, 916. https://doi.org/10.3390/nu10070916
Hemmingway A, O’Callaghan KM, Hennessy Á, Hull GLJ, Cashman KD, Kiely ME. Interactions between Vitamin D Status, Calcium Intake and Parathyroid Hormone Concentrations in Healthy White-Skinned Pregnant Women at Northern Latitude. Nutrients. 2018; 10(7):916. https://doi.org/10.3390/nu10070916
Chicago/Turabian StyleHemmingway, Andrea, Karen M. O’Callaghan, Áine Hennessy, George L. J. Hull, Kevin D. Cashman, and Mairead E. Kiely. 2018. "Interactions between Vitamin D Status, Calcium Intake and Parathyroid Hormone Concentrations in Healthy White-Skinned Pregnant Women at Northern Latitude" Nutrients 10, no. 7: 916. https://doi.org/10.3390/nu10070916





