Optimal Adherence to a Mediterranean Diet May Not Overcome the Deleterious Effects of Low Physical Fitness on Cardiovascular Disease Risk in Adolescents: A Cross-Sectional Pooled Analysis
Abstract
1. Introduction
2. Methods
2.1. Study Design, Sampling Procedures, and Participants
2.2. Adherence to the Mediterranean Diet
2.3. Cardiorespiratory Fitness
2.4. Muscular Fitness
2.5. Data Management
2.6. Cardiometabolic Variables
2.7. Pubertal Stage
2.8. Statistical Analysis
3. Results
3.1. Study Participants
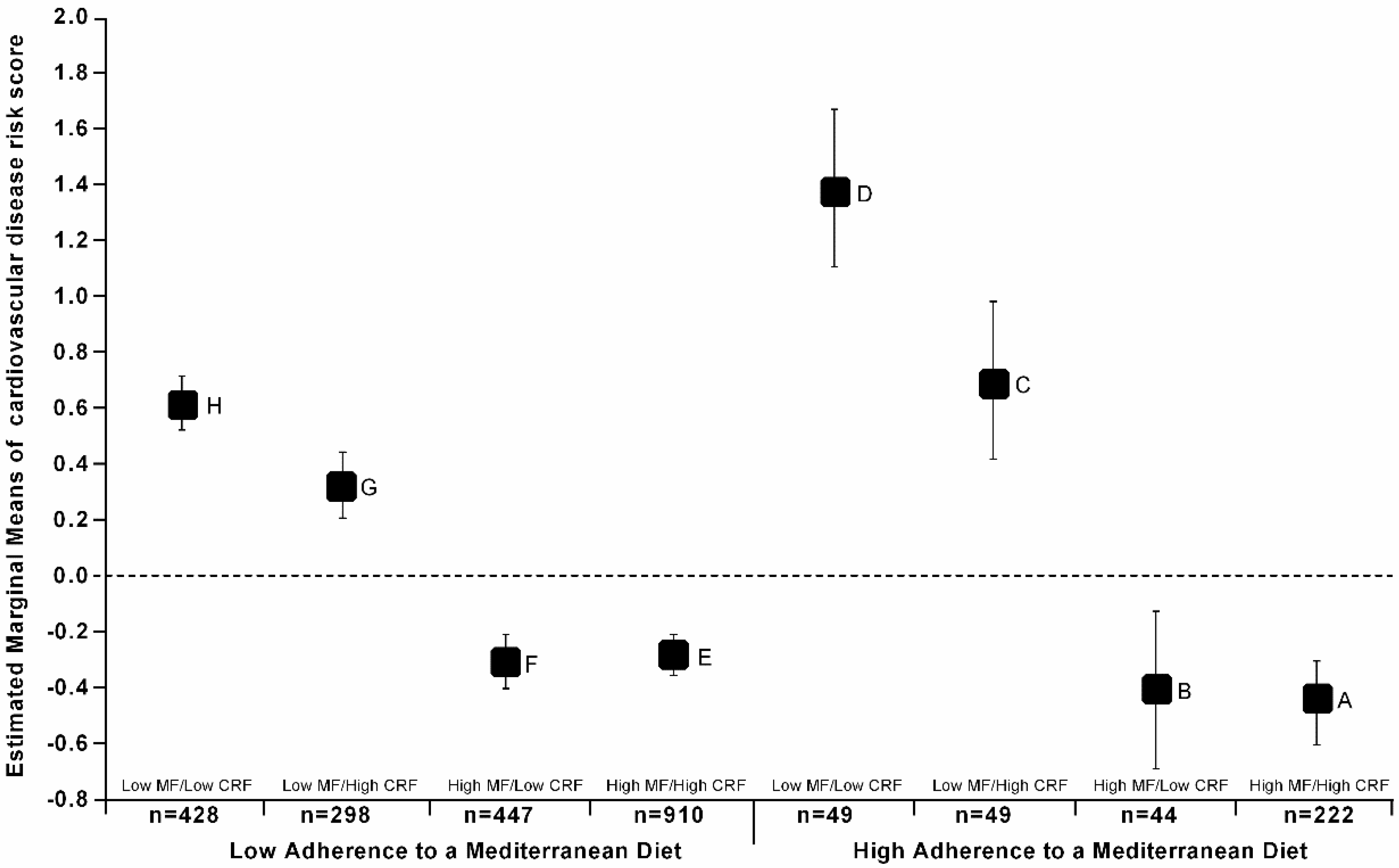
3.2. Relationship between Cardiovascular Risk Scores across Combined Groups of Adherence to a MeDiet, Cardiorespiratory Fitness, and Muscular Fitness
3.3. Association between High Cardiovascular Risk by Adherence to a MeDiet, Cardiorespiratory Fitness, and Muscular Fitness Categories
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| BMI | Body mass index |
| CRF | Cardiorespiratory fitness |
| CVD | Cardiovascular disease |
| HDL | High-density lipoprotein cholesterol |
| MedDiet | Adherence to Mediterranean Diet |
| MF | Muscular Fitness |
| TC | Total cholesterol |
| VO2max | Maximum oxygen consumption |
| WC | Waist circumference |
References
- Balagopal, P.B.; De Ferranti, S.D.; Cook, S.; Daniels, S.R.; Gidding, S.S.; Hayman, L.L.; McCrindle, B.W.; Mietus-Snyder, M.L.; Steinberger, J.; American Heart Association Committee on Atherosclerosis Hypertension and Obesity in Youth of the Council on Cardiovascular Disease in the Young; et al. Nontraditional risk factors and biomarkers for cardiovascular disease: Mechanistic, research, and clinical considerations for youth: A scientific statement from the American Heart Association. Circulation 2011, 123, 2749–2769. [Google Scholar] [CrossRef] [PubMed]
- Friend, A.; Craig, L.; Turner, S. The Prevalence of Metabolic Syndrome in Children: A Systematic Review of the Literature. Metab. Syndr. Relat. Disord. 2013, 11, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Alberti, S.G.; Zimmet, P. The IDF Consensus Definition of the Metabolic Syndrome in Children and Adolescents; International Diabetes Federation: Brussels, Belgium, 2007; p. 24. [Google Scholar]
- Andersen, L.B.; Lauersen, J.B.; Brønd, J.C.; Anderssen, S.A.; Sardinha, L.B.; Steene-Johannessen, J.; McMurray, R.G.; Barros, M.V.G.; Kriemler, S.; Møller, N.C.; et al. A New Approach to Define and Diagnose Cardiometabolic Disorder in Children. J. Diabetes Res. 2015, 2015, 539835. [Google Scholar] [CrossRef] [PubMed]
- WHO. 2008–2013 Action Plan for the Global Strategy for the Prevention and Control of Noncommunicable Diseases; Geneva World Heal Organ: Geneva, Switzerland, 2008. [Google Scholar]
- Okubo, H.; Crozier, S.R.; Harvey, N.C.; Godfrey, K.M.; Inskip, H.M.; Cooper, C.; Robinson, S.M. Diet quality across early childhood and adiposity at 6 years: The Southampton Women’s Survey. Int. J. Obes. 2015, 39, 1456–1462. [Google Scholar] [CrossRef] [PubMed]
- Storey, K.E.; Hanning, R.M.; Lambraki, I.A.; Driezen, P.; Fraser, S.N.; McCargar, L.J. Determinants of Diet quality among Canadian adolescents. Can. J. Diet. Pract. Res. 2009, 70, 58–65. [Google Scholar] [CrossRef] [PubMed]
- WHO. Diet, Nutrition and the Prevention of Chronic Diseases; World Health Organ Tech Rep Ser 2003, 916, i–viii-1-149-Backcover; WHO: Geneva, Switzerland, 2003. [Google Scholar]
- Kohl, H.W.; Craig, C.L.; Lambert, E.V.; Inoue, S.; Alkandari, J.R.; Leetongin, G.; Kahlmeier, S. The pandemic of physical inactivity : Global action for public health. Lancet 2012, 380, 294–305. [Google Scholar] [CrossRef]
- Cooper, A.R.; Goodman, A.; Page, A.S.; Sherar, L.B.; Esliger, D.W.; van Sluijs, E.M.; Andersen, L.B.; Anderssen, S.; Cardon, G.; Davey, R.; et al. Objectively measured physical activity and sedentary time in youth: The International children’s accelerometry database (ICAD). Int. J. Behav. Nutr. Phys. Act. 2015, 12, 113. [Google Scholar] [CrossRef] [PubMed]
- Neill, S.O.; Driscoll, L.O.; O’Neill, S.; O’Driscoll, L. Metabolic syndrome: A closer look at the growing epidemic and its associated pathologies. Obes. Rev. 2015, 16, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Kodama, S.; Saito, K.; Tanaka, S.; Maki, M.; Yachi, Y.; Asumi, M.; Sugawara, A.; Totsuka, K.; Shimano, H.; Ohashi, Y.; et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women. J. Am. Med. Assoc. 2009, 301, 2024–2035. [Google Scholar] [CrossRef] [PubMed]
- García-Hermoso, A.; Cavero-Redondo, I.; Ramírez-Vélez, R.; Ruiz, J.; Ortega, F.B.; Lee, D.-C.; Martínez-Vizcaíno, V. Muscular strength as a predictor of all-cause mortality in apparently healthy population: A systematic review and meta-analysis of data from approximately 2 million men and women. Arch. Phys. Med. Rehabil. 2018. [Google Scholar] [CrossRef] [PubMed]
- Hogstrom, G.; Nordstrom, A.; Nordstrom, P. High aerobic fitness in late adolescence is associated with a reduced risk of myocardial infarction later in life: A nationwide cohort study in men. Eur. Heart J. 2014, 35, 3133–3140. [Google Scholar] [CrossRef] [PubMed]
- Agostinis-Sobrinho, C.; Ruiz, J.R.; Moreira, C.; Abreu, S.; Lopes, L.; Oliveira-Santos, J.; Mota, J.; Santos, R. Cardiorespiratory Fitness and Blood Pressure: A Longitudinal Analysis. J. Pediatr. 2018, 192, 130–135. [Google Scholar] [CrossRef] [PubMed]
- Agostinis-Sobrinho, C.C.A.; Ruiz, J.R.J.; Moreira, C.; Abreu, S.; Luís, L.; Oliveira-Santos, J.; Mota, J.; Santos, R. Cardiorespiratory fitness and inflammatory profile on cardiometabolic risk in adolescents from the LabMed Physical Activity Study. Eur. J. Appl. Physiol. 2017, 117, 2271–2279. [Google Scholar] [CrossRef] [PubMed]
- Agostinis-Sobrinho, C.A.; Ramirez-Velez, R.; Garcia-Hermoso, A.; Moreira, C.; Lopes, L.; Oliveira-Santos, J.; Abreu, S.; Mota, J.; Santos, R. Low-grade inflammation and muscular fitness on insulin resistance in adolescents: Results from LabMed Physical Activity Study. Pediatr. Diabetes 2017, 19, 429–435. [Google Scholar] [CrossRef] [PubMed]
- Fraser, B.J.; Blizzard, L.; Schmidt, M.D.; Juonala, M.; Dwyer, T.; Venn, A.J.; Magnussen, C.G. Childhood cardiorespiratory fitness, muscular fitness and adult measures of glucose homeostasis. J. Sci. Med. Sport 2018. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, J.R.; Cavero-Redondo, I.; Ortega, F.B.; Welk, G.J.; Andersen, L.B.; Martinez-Vizcaino, V. Cardiorespiratory fitness cut points to avoid cardiovascular disease risk in children and adolescents; what level of fitness should raise a red flag? A systematic review and meta-analysis. Br. J. Sports Med. 2016, 50, 1451–1458. [Google Scholar] [CrossRef] [PubMed]
- Agostinis-Sobrinho, C.; Brand, C.; Moreira, C.; Lopes, L.; Oliveira-Santos, J.; Silva, P.; Reis Gaya, A.; Gaya, A.; Mota, J.; Santos, R.; et al. Muscular fitness, Southern European Atlantic Diet and inflammation in adolescents. Azorean Physical Activity and Health Study II. Eur. J. Sport Sci. 2018, 18, 104–111. [Google Scholar] [CrossRef] [PubMed]
- Grøntved, A.; Ried-Larsen, M.; Ekelund, U.; Froberg, K.; Brage, S.; Andersen, L.B. Independent and combined association of muscle strength and cardiorespiratory fitness in youth with insulin resistance and β-cell function in young adulthood: The european youth heart study. Diabetes Care 2013, 36, 2575–2581. [Google Scholar] [CrossRef] [PubMed]
- Morikawa, S.Y.; Fujihara, K.; Hatta, M.; Osawa, T.; Ishizawa, M.; Yamamoto, M.; Furukawa, K.; Ishiguro, H.; Matsunaga, S.; Ogawa, Y.; et al. Relationships among cardiorespiratory fitness, muscular fitness, and cardiometabolic risk factors in Japanese adolescents: Niigata screening for and preventing the development of non-communicable disease study-Agano (NICE EVIDENCE Study-Agano) 2. Pediatr. Diabetes 2017, 19, 593–602. [Google Scholar] [CrossRef] [PubMed]
- Sofi, F.; Cesari, F.; Abbate, R.; Gensini, G.F.; Casini, A. Adherence to Mediterranean diet and health status: Meta-analysis. BMJ 2008, 337, a1344. [Google Scholar] [CrossRef] [PubMed]
- Arouca, A.; Michels, N.; Moreno, L.A.; González-Gil, E.M.; Marcos, A.; Gómez, S.; Díaz, L.E.; Widhalm, K.; Molnár, D.; Manios, Y.; et al. Associations between a Mediterranean diet pattern and inflammatory biomarkers in European adolescents. Eur. J. Nutr. 2017. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Vélez, R.; Morales, O.; Peña-Ibagon, J.C.; Palacios-López, A.; Prieto-Benavides, D.H.; Vivas, A.; Correa-Bautista, J.E.; Lobelo, F.; Alonso-Martínez, A.M.; Izquierdo, M. Normative Reference Values for Handgrip Strength in Colombian Schoolchildren. J. Strength Cond. Res. 2017, 31, 217–226. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Vélez, R.; Rodrigues-Bezerra, D.; Correa-Bautista, J.E.; Izquierdo, M.; Lobelo, F. Reliability of health-related physical fitness tests among Colombian children and adolescents: The Fuprecol study. PLoS ONE 2015, 10, e0140875. [Google Scholar] [CrossRef] [PubMed]
- Agostinis-Sobrinho, C.; Santos, R.; Moreira, C.; Abreu, S.; Lopes, L.; Oliveira-Santos, J.; Rosário, R.; Póvoas, S.; Mota, J. Association between serum adiponectin levels and muscular fitness in Portuguese adolescents: LabMed Physical Activity Study. Nutr. Metab. Cardiovasc. Dis. 2016, 6, 517–524. [Google Scholar] [CrossRef] [PubMed]
- Agostinis-Sobrinho, C.A.; Moreira, C.; Abreu, S.; Lopes, L.; Sardinha, L.B.; Oliveira-Santos, J.; Oliveira, A.; Mota, J.; Santos, R. Muscular fitness and metabolic and inflammatory biomarkers in adolescents: Results from LabMed Physical Activity Study. Scand. J. Med. Sci. Sports 2016, 27, 1873–1880. [Google Scholar] [CrossRef] [PubMed]
- Serra-Majem, L.; Ribas, L.; Ngo, J.; Ortega, R.M.; García, A.; Pérez-Rodrigo, C.; Aranceta, J. Food, youth and the Mediterranean diet in Spain. Development of KIDMED, Mediterranean Diet Quality Index in children and adolescents. Public Health Nutr. 2004, 7, 931–935. [Google Scholar] [CrossRef] [PubMed]
- Leger, L.A.; Mercier, D.; Gadoury, C.; Lambert, J. The multistage 20 m shuttle run test for aerobic fitness. J. Sport Sci. 1988, 6, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, J.R.; Castro-Piñero, J.; España-Romero, V.; Artero, E.G.; Ortega, F.B.; Cuenca, M.M.; Jimenez-Pavón, D.; Chillón, P.; Girela-Rejón, M.J.; Mora, J.; et al. Field-based fitness assessment in young people: The ALPHA health-related fitness test battery for children and adolescents. Br. J. Sports Med. 2011, 45, 518–524. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Vélez, R.; García-Hermoso, A.; Agostinis-Sobrinho, C.; Mota, J.; Santos, R.; Correa-Bautista, J.E.J.E.; Peña-Guzmán, C.A.; Domínguez-Sánchez, M.A.; Schmidt-RioValle, J.; González-Jiménez, E. Pubertal stage, body mass index, and cardiometabolic risk in children and adolescents in Bogotá, Colombia: The cross-sectional fuprecol study. Nutrients 2017, 9, 644. [Google Scholar] [CrossRef] [PubMed]
- Tanner, J.M.; Whitehouse, R.H. Clinical longitudinal standards for height, weight, height velocity, weight velocity, and stages of puberty. Arch. Dis. Child. 1976, 51, 170–179. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.J.; Eather, N.; Morgan, P.J.; Plotnikoff, R.C.; Faigenbaum, A.D.; Lubans, D.R. The health benefits of muscular fitness for children and adolescents: A systematic review and meta-analysis. Sports Med. 2014, 44, 1209–1223. [Google Scholar] [CrossRef] [PubMed]
- Ortega, F.B.; Silventoinen, K.; Tynelius, P.; Rasmussen, F. Muscular strength in male adolescents and premature death: Cohort study of one million participants. BMJ 2012, 345, e7279. [Google Scholar] [CrossRef] [PubMed]
- Ortega, F.B.; Ruiz, J.R.; Castillo, M.J.; Sjöström, M. Physical fitness in childhood and adolescence: A powerful marker of health. Int. J. Obes. (Lond.) 2008, 32, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Moreira, C.; Santos, R.; Moreira, P.; Lobelo, F.; Ruiz, J.R.; Vale, S.; Santos, P.C.; Abreu, S.; Mota, J. Cardiorespiratory fitness is negatively associated with metabolic risk factors independently of the adherence to a healthydietary pattern. Nutr. Metab. Cardiovasc. Dis. 2013, 23, 670–676. [Google Scholar] [CrossRef] [PubMed]
- Magriplis, E.; Farajian, P.; Pounis, G.D.; Risvas, G.; Panagiotakos, D.B.; Zampelas, A. High sodium intake of children through “hidden” food sources and its association with the Mediterranean diet: The GRECO study. J. Hypertens. 2011, 29, 1069–1076. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Hermoso, A.; Agostinis-Sobrinho, C.; Mota, J.; Santos, R.M.; Correa-Bautista, J.E.; Ramírez-Vélez, R. Adiposity as a Full Mediator of the Influence of Cardiorespiratory Fitness and Inflammation in Schoolchildren: The FUPRECOL Study. Nutr. Metab. Cardiovasc. Dis. 2017, 27, 525–533. [Google Scholar] [CrossRef] [PubMed]
- García-Hermoso, A.; Carrillo, H.A.; González-Ruóz, K.; Vivas, A.; Triana-Reina, H.R.; Martoínez-Torres, J.; Prieto-Benavidez, D.H.; Correa-Bautista, J.E.; Ramos-Sepúlveda, J.A.; Villa-González, E.; et al. Fatness mediates the influence of muscular fitness on metabolic syndrome in Colombian collegiate students. PLoS ONE 2017, 12, e0173932. [Google Scholar] [CrossRef] [PubMed]
- Cohen, D.D.; Gómez-Arbeláez, D.; Camacho, P.A.; Pinzon, S.; Hormiga, C.; Trejos-Suarez, J.; Duperly, J.; Lopez-Jaramillo, P. Low muscle strength is associated with metabolic risk factors in Colombian children: The ACFIES study. PLoS ONE 2014, 9, e93150. [Google Scholar] [CrossRef] [PubMed]
- Artero, E.G.; Ruiz, J.R.; Ortega, F.B.; España-Romero, V.; Vicente-Rodríguez, G.; Molnar, D.; Gottrand, F.; González-Gross, M.; Breidenassel, C.; Moreno, L.A.; et al. Muscular and cardiorespiratory fitness are independently associated with metabolic risk in adolescents: The HELENA study. Pediatr. Diabetes 2011, 12, 704–712. [Google Scholar] [CrossRef] [PubMed]
- Steene-Johannessen, J.; Anderssen, S.A.; Kolle, E.; Andersen, L.B. Low muscle fitness is associated with metabolic risk in youth. Med. Sci. Sport Exerc. 2009, 41, 1361–1367. [Google Scholar] [CrossRef] [PubMed]
- Volaklis, K.A.; Halle, M.; Meisinger, C. Muscular strength as a strong predictor of mortality: A narrative review. Eur. J. Intern. Med. 2015, 26, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Ottevaere, C.; Huybrechts, I.; Benser, J.; De Bourdeaudhuij, I.; Cuenca-Garcia, M.; Dallongeville, J.; Zaccaria, M.; Gottrand, F.; Kersting, M.; Rey-López, J.P. Clustering patterns of physical activity, sedentary and dietary behavior among European adolescents: The HELENA study. BMC Public Health 2011, 11, 328. [Google Scholar] [CrossRef] [PubMed]
- Jago, R.; Ness, A.R.; Emmett, P.; Mattocks, C.; Jones, L.; Riddoch, C.J. Obesogenic diet and physical activity: Independent or associated behaviours in adolescents? Public Health Nutr. 2010, 13, 673–681. [Google Scholar] [CrossRef] [PubMed]
- Della Corte, C.; Mosca, A.; Vania, A.; Alterio, A.; Iasevoli, S.; Nobili, V. Good Adherence to Mediterranean Diet reduces the risk to develop NASH and diabetes in pediatric patients with obesity: The results of an Italian Study. Nutrition 2017, 39–40, 8–14. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Low MeDiet (n = 2115) | High MeDiet (n = 362) | Low MF (n = 828) | High MF (n = 1649) | Low CRF (n = 982) | High CRF (n = 1495) |
|---|---|---|---|---|---|---|
| Age (year) | 14.2 (1.5) | 14.1 (1.6) | 14.2 (1.5) | 14.2 (1.5) | 14.6 (1.5) | 14.1 (1.5) |
| BMI (kg m2) | 20.3 (3.0) | 21.0 (3.7) | 21.7 (3.7) b | 19.9 (3.1) | 21.2 (3.5) c | 20.0 (2.7) |
| Waist circumference (cm) | 66.8 (7.6) a | 70.8 (10.1) | 69.8 (9.6) b | 66.2 (7.1) | 68.7 (9.2) c | 66.5 (7.5) |
| Pubertal status A: ≤III/IV/V (%) | 48.0/44.7/8.3 | 44.7/48.8/10.5 | 51.0/41.2/7.8 | 46.7/44.1/9.2 | 48.1/42.1/9.8 | 48.2/43.8/8.1 |
| Pubertal status B: ≤III/IV/V (%) | 48.6/43.4/8.0 | 40.6/43.1/16.3 | 51.3/41.7.7 | 46.4/43.0/10.5 | 49.2/42.0/8.8 | 47.4/43.0/9.7 |
| HDL-Cholesterol (mg/dL) | 47.1 (12.1) a | 52.0 (12.2) | 45.6 (11.2) b | 49.0 (12.6) | 46.4 (11.9) c | 48,8 (12.5) |
| Triglycerides (mg/dL) | 87.9 (42.1) a | 76.6 (37.7) | 93.7 (47.6) b | 82.5 (37.9) | 88.7 (42.8) c | 84.6 (40.9) |
| Glucose (mg/dL) | 83.0 (15.1) a | 86.4 (12.3) | 82.7 (15.0) | 83.4 (14.9) | 83.0 (15.6) | 83.3 (14.5) |
| Systolic Blood Pressure (mm Hg) | 113.1 (13.1) | 116.5 (13.8) | 114.1 (13.4) | 113.3 (13.1) | 113.5 (13.4) | 113.7 (13.7) |
| CRF—VO2max (mL/kg/min) | 39.3 (5.7) a | 42.1 (6.4) | 37.3 (5.1) b | 40.9 (5.9) | - | - |
| Muscular Fitness Score | −0.8 (1.5) a | 0.4 (1.7) | - | - | −0.6 (1.4) c | 0.4 (1.5) |
| Parameter | High Cardiovascular Risk | |||
|---|---|---|---|---|
| OR Unadjusted (95% CI) | p-Value | OR Adjusted (95% CI) * | p-Value | |
| High-MeDiet HighMF/HighCRF | 1.0 | - | 1.0 | - |
| High-MeDiet HighMF/LowCRF | 2.0 (0.8–4.9) | 0.109 | 1.8 (0.7–4.0) | 0.165 |
| High-MeDiet LowMF/HighCRF | 2.5 (1.1–5.6) | 0.023 | 3.1 (1.4–7.0) | 0.006 |
| High-MeDiet LowMF/LowCRF | 6.5 (3.1–13.3) | <0.001 | 7.1 (3.4–15.1) | <0.001 |
| Low-MeDiet HighMF/HighCRF | 0.9 (0.6–1.5) | 0.897 | 1.3 (0.7–2.1) | 0.346 |
| Low-MeDiet HighMF/LowCRF | 1.1 (0.6–1.9) | 0.611 | 1.6 (0.8–2.7) | 0.112 |
| Low-MeDiet LowMF/HighCRF | 1.5 (0.9–2.6) | 0.113 | 2.5 (1.5–4.4) | 0.002 |
| Low-MeDiet LowMF/LowCRF | 2.5 (1.5–4.1) | <0.001 | 3.7 (2.2–6.3) | <0.001 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Agostinis-Sobrinho, C.; Santos, R.; Rosário, R.; Moreira, C.; Lopes, L.; Mota, J.; Martinkenas, A.; García-Hermoso, A.; Correa-Bautista, J.E.; Ramírez-Vélez, R. Optimal Adherence to a Mediterranean Diet May Not Overcome the Deleterious Effects of Low Physical Fitness on Cardiovascular Disease Risk in Adolescents: A Cross-Sectional Pooled Analysis. Nutrients 2018, 10, 815. https://doi.org/10.3390/nu10070815
Agostinis-Sobrinho C, Santos R, Rosário R, Moreira C, Lopes L, Mota J, Martinkenas A, García-Hermoso A, Correa-Bautista JE, Ramírez-Vélez R. Optimal Adherence to a Mediterranean Diet May Not Overcome the Deleterious Effects of Low Physical Fitness on Cardiovascular Disease Risk in Adolescents: A Cross-Sectional Pooled Analysis. Nutrients. 2018; 10(7):815. https://doi.org/10.3390/nu10070815
Chicago/Turabian StyleAgostinis-Sobrinho, César, Rute Santos, Rafaela Rosário, Carla Moreira, Luís Lopes, Jorge Mota, Arvydas Martinkenas, Antonio García-Hermoso, Jorge Enrique Correa-Bautista, and Robinson Ramírez-Vélez. 2018. "Optimal Adherence to a Mediterranean Diet May Not Overcome the Deleterious Effects of Low Physical Fitness on Cardiovascular Disease Risk in Adolescents: A Cross-Sectional Pooled Analysis" Nutrients 10, no. 7: 815. https://doi.org/10.3390/nu10070815
APA StyleAgostinis-Sobrinho, C., Santos, R., Rosário, R., Moreira, C., Lopes, L., Mota, J., Martinkenas, A., García-Hermoso, A., Correa-Bautista, J. E., & Ramírez-Vélez, R. (2018). Optimal Adherence to a Mediterranean Diet May Not Overcome the Deleterious Effects of Low Physical Fitness on Cardiovascular Disease Risk in Adolescents: A Cross-Sectional Pooled Analysis. Nutrients, 10(7), 815. https://doi.org/10.3390/nu10070815







