Associations of Maternal Vitamin D Deficiency with Pregnancy and Neonatal Complications in Developing Countries: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Criteria
2.2. Search Strategy
2.3. Data Extraction
2.4. Quality Assessment
3. Results
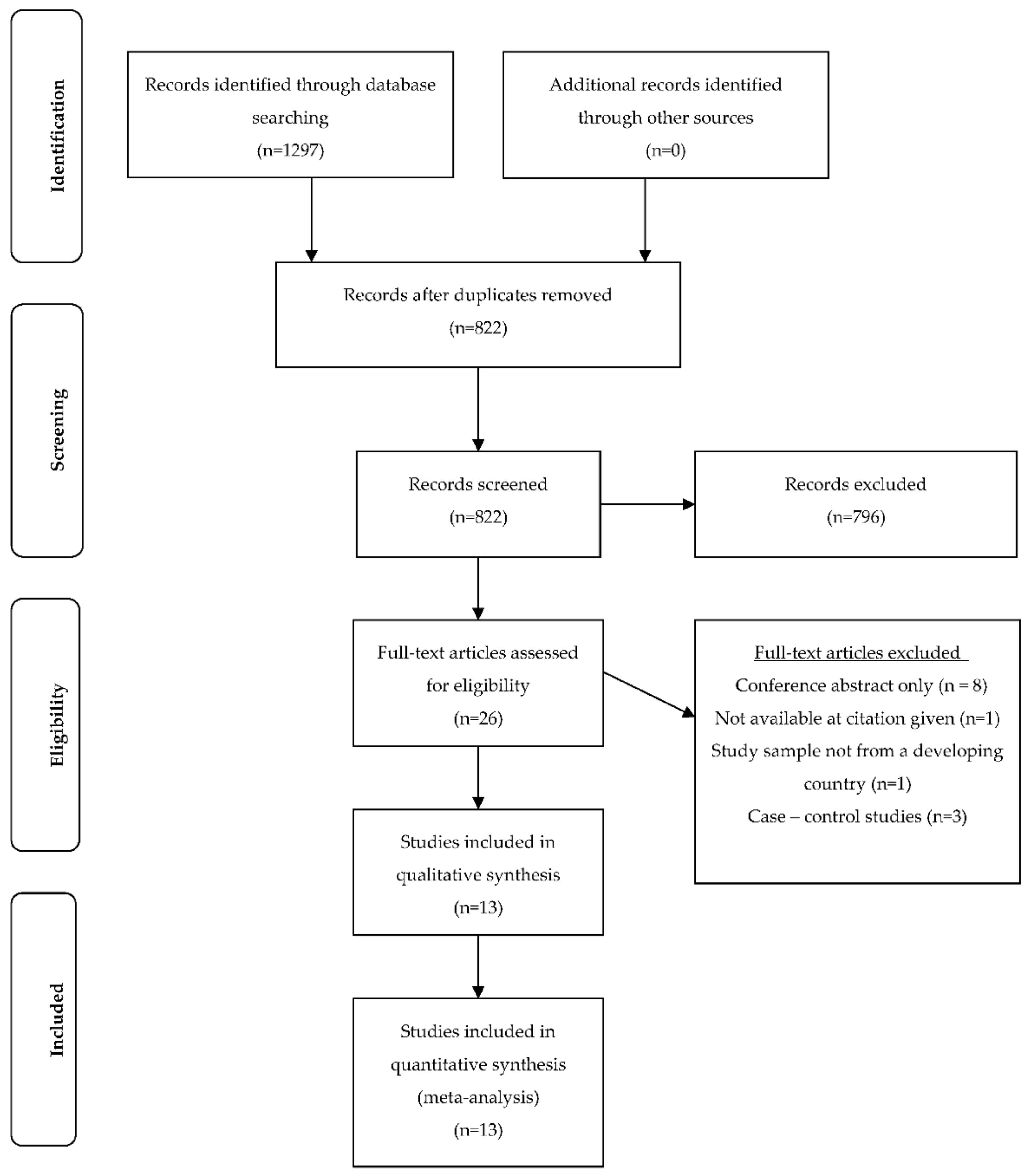
3.1. Study Selection
3.2. Setting and Participants
3.3. Vitamin D Assessment
3.4. Vitamin D Deficiency, Criteria and Prevalence
3.5. Maternal and Neonatal Outcomes
3.6. Biological and Lifestyle Risk Factors
3.7. Study Quality
4. Discussion
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Holick, M.F.; Binkley, N.C.; Bischoff-Ferrari, H.A.; Gordon, C.M.; Hanley, D.A.; Heaney, R.P.; Murad, M.H.; Weaver, C.M. Evaluation, treatment, and prevention of vitamin D deficiency: An endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 2011, 96, 1911–1930. [Google Scholar] [CrossRef] [PubMed]
- Nair, R.; Maseeh, A. Vitamin D: The “sunshine” vitamin. J. Pharmacol. Pharmacother. 2012, 3, 118–126. [Google Scholar] [PubMed]
- Kiely, M.E. Invited commentray: Further evidence that prevention of maternal vitamin D deficiency may benefit the health of the next generation. Br. J. Nutr. Diet. 2016, 116, 573–575. [Google Scholar]
- Munns, C.F.; Shaw, N.; Kiely, M.; Specker, B.L.; Thacher, T.D.; Ozono, K.; Michigami, T.; Tiosano, D.; Mughal, M.Z.; Mäkitie, O.; et al. Global consensus recommendations on prevention and management of nutritional rickets. Hormone Res. Paediatr. 2016, 85, 83–106. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Vitamin D. Vitamin and Mineral Requirements in Human Nutrition: Report of a Joint FAO/WHO Expert Consultation, 2nd ed.; WHO: Geneva, Switzerland, 2003; Chapter 3. [Google Scholar]
- Toko, E.N.; Sumba, O.P.; Daud, I.I.; Ogolla, S.; Majiwa, M.; Krisher, J.T.; Ouma, C.; Dent, A.E.; Rochford, R.; Mehta, S. Maternal vitamin D status and adverse birth outcomes in children from rural western Kenya. Nutrients 2016, 8, 794. [Google Scholar] [CrossRef] [PubMed]
- Nimitphong, H.; Holick, M.F. Vitamin D status and sun exposure in southeast Asia. Derm. Endocrinol. 2013, 5, 34–37. [Google Scholar] [CrossRef] [PubMed]
- Mehta, S.; Spiegelman, D.; Aboud, S.; Giovannucci, E.L.; Msamanga, G.I.; Hertzmark, E.; Mugusi, F.M.; Hunter, D.J.; Fawzi, W.W.; Mehta, S.; et al. Lipid-soluble vitamins A, D, and E in HIV-infected pregnant women in Tanzania. Eur. J. Clin. Nutr. 2010, 64, 808–817. [Google Scholar] [CrossRef] [PubMed]
- Halicioglu, O.; Aksit, S.; Koc, F.; Akman, S.A.; Albudak, E.; Yaprak, I.; Coker, I.; Colak, A.; Ozturk, C.; Gulec, E.S. Vitamin D deficiency in pregnant women and their neonates in spring time in western Turkey. Paediatr. Perinat. Epidemiol. 2012, 26, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.M.; Smith, J.R.; Philipp, B.L.; Chen, T.C.; Mathieu, J.; Holick, M.F. Vitamin D deficiency in a healthy group of mothers and newborn infants. Clin. Pediatr. 2007, 46, 42–44. [Google Scholar] [CrossRef] [PubMed]
- Mutlu, N.; Esra, H.; Begum, A.; Fatma, D.; Arzu, Y.; Yalcin, H.; Fatih, K.; Selahattin, K. Relation of maternal vitamin D status with gestational diabetes mellitus and perinatal outcome. Afr. Health Sci. 2015, 15, 523–531. [Google Scholar] [CrossRef] [PubMed]
- Tao, M.; Shao, H.; Gu, J.; Zhen, Z. Vitamin D status of pregnant women in Shanghai, China. J. Matern. Fetal Neonatal Med. 2012, 25, 237–239. [Google Scholar] [CrossRef] [PubMed]
- Palacios, C.; De-Regil, L.M.; Lombardo, L.K.; Peña-Rosas, J.P. Vitamin D supplementation during pregnancy: Updated meta-analysis on maternal outcomes. J. Steroid Biochem. Mol. Biol. 2016, 164, 148–155. [Google Scholar] [CrossRef] [PubMed]
- Verstuyf, A.; Carmeliet, G.; Bouillon, R.; Mathieu, C. Vitamin D: A pleiotropic hormone. Kidney Int. 2010, 78, 140–145. [Google Scholar] [CrossRef] [PubMed]
- Jones, G.; Strugnell, S.A.; DeLuca, H.F. Current understanding of the molecular actions of vitamin D. Physiol. Rev. 1998, 78, 1193–1231. [Google Scholar] [CrossRef] [PubMed]
- Wei, S.Q.; Qi, H.P.; Luo, Z.C.; Fraser, W.D. Maternal vitamin D status and adverse pregnancy outcomes: A systematic review and meta-analysis. J. Matern. Fetal Neonatal Med. 2013, 26, 889–899. [Google Scholar] [CrossRef] [PubMed]
- Lapillonne, A. Vitamin D deficiency during pregnancy may impair maternal and fetal outcomes. Med. Hypotheses 2010, 74, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Josefson, J.L.; Reisetter, A.; Scholtens, D.M.; Price, H.E.; Metzger, B.E.; Langman, C.B.; Group HSCR. Maternal BMI associations with maternal and cord blood vitamin D levels in a North American subset of hyperglycemia and adverse pregnancy outcome (HAPO) study participants. PLoS ONE 2016, 11. [Google Scholar] [CrossRef] [PubMed]
- Robinson, M.; Whitehouse, A.J.O.; Newnham, J.P.; Gorman, S.; Jacoby, P.; Holt, B.J.; Serralha, M.; Tearne, J.E.; Holt, P.G.; Hart, P.H.; et al. Low maternal serum vitamin D during pregnancy and the risk for postpartum depression symptoms. Arch. Women’s Ment. Health 2014, 17, 213–219. [Google Scholar] [CrossRef] [PubMed]
- Prentice, A.; Jarjou, L.M.A.; Goldberg, G.R.; Bennett, J.; Cole, T.J.; Schoenmakers, I. Maternal plasma 25-hydroxyvitamin D concentration and birthweight, growth and bone mineral accretion of Gambian infants. Acta Paediatr. 2009, 98, 1360–1362. [Google Scholar] [CrossRef] [PubMed]
- Eggemoen, Å.R.; Falk, R.S.; Knutsen, K.V.; Lagerløv, P.; Sletner, L.; Birkeland, K.I.; Jenum, A.K. Vitamin D deficiency and supplementation in pregnancy in a multiethnic population-based cohort. BMC Pregnancy Child. 2016, 16. [Google Scholar] [CrossRef] [PubMed]
- Lips, P.; van Schoor, N.M.; de Jongh, R.T. Diet, sun, and lifestyle as determinants of vitamin D status. Ann. N. Y. Acad. Sci. 2014, 1317, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Torheim, L.E.; Ferguson, E.L.; Penrose, K.; Arimond, M. Women in resource-poor settings are at risk of inadequate intakes of multiple micronutrients. J. Nutr. 2010, 140, 2051S–2058S. [Google Scholar] [CrossRef] [PubMed]
- Ajmani, S.N.; Paul, M.; Chauhan, P.; Ajmani, A.K.; Yadav, N. Prevalence of vitamin D deficiency in burka-clad pregnant women in a 450-bedded maternity hospital of Delhi. J. Obs. Gynecol. India 2016, 66, 67–71. [Google Scholar] [CrossRef] [PubMed]
- Pirdehghan, A.; Vakili, M.; Dehghan, R.; Zare, F. High prevalence of vitamin D deficiency and adverse pregnancy outcomes in Yazd, a central province of Iran. J. Reprod. Infertil. 2016, 17, 34–38. [Google Scholar] [PubMed]
- Song, S.; Si, S.; Liu, J.; Chen, X.; Zhou, L.; Jia, G.; Liu, G.; Niu, Y.; Wu, J.; Zhang, W. Vitamin D status in Chinese pregnant women and their newborns in Beijing and their relationships to birth size. Public Health Nutr. 2013, 16, 687–692. [Google Scholar] [CrossRef] [PubMed]
- Gbadegesin, A.; Sobande, A.; Adedeji, O.; Disu, E.; Korede, O.; Dosunmu, A.; Shakunle, A. Maternal serum vitamin D levels and pregnancy outcomes: From Lagos, Nigeria. J. Obs. Gynaecol. 2017, 37, 25–28. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Cohort and case control studies. In Special Programme of Research, Development and Research Training in Human Reproduction; WHO: Geneva, Switzerland, 2017. [Google Scholar]
- Lewallen, S.; Courtright, P. Epidemiology in practice: Case-control studies. Commun. Eye Health 1998, 11, 57–58. [Google Scholar]
- Fatusi, A.O. Young people’s sexual and reproductive health interventions in developing countries: Making the investments count. J. Adolesc. Health 2016, 59, S1–S3. [Google Scholar] [CrossRef] [PubMed]
- Department of Foreign Affairs and Trade (DFAT). List of Developing countries as declared by the Minister for Foreign Affairs; DFAT: Canberra, Australia, 2015.
- Van der Pligt, P.; Willcox, J.; Hesketh, K.D.; Ball, K.; Wilkinson, S.; Crawford, D.; Campbell, K. Systematic review of lifestyle interventions to limit postpartum weight retention: Implications for future opportunities to prevent maternal overweight and obesity following childbirth. Obes. Rev. 2013, 14, 792–805. [Google Scholar] [CrossRef] [PubMed]
- Thomas, H. Quality assessment tool for quantitative studies. In Effective Public Health Practice Project; McMaster University: Toronto, ON, Canada, 2003. [Google Scholar]
- Farrant, H.J.W.; Krishnaveni, G.V.; Hill, J.C.; Boucher, B.J.; Fisher, D.J.; Noonan, K.; Osmond, C.; Veena, S.R.; Fall, C.H.D. Vitamin D insufficiency is common in Indian mothers but is not associated with gestational diabetes or variation in newborn size. Eur. J. Clin. Nutr. 2009, 63, 646–652. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-H.; Fu, L.; Hao, J.-H.; Yu, Z.; Zhu, P.; Wang, H.; Xu, Y.-Y.; Zhang, C.; Tao, F.-B.; Xu, D.-X. Maternal vitamin D deficiency during pregnancy elevates the risks of small for gestational age and low birth weight infants in Chinese population. J. Clin. Endocrinol. Metab. 2015, 100, 1912–1919. [Google Scholar] [CrossRef] [PubMed]
- Xin, Z.; Jianping, X.; Rui, F.; Renqiang, Y.; Daozhen, C.; Jun, Z. Maternal vitamin D status in the late second trimester and the risk of severe preeclampsia in southeastern China. Nutrients 2017, 9, 138. [Google Scholar] [CrossRef]
- Ates, S.; Sevket, O.; Ozcan, P.; Ozkal, F.; Kaya, M.O.; Dane, B. Vitamin D status in the first-trimester: Effects of vitamin D deficiency on pregnancy outcomes. Afr. Health Sci. 2016, 16, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Aydogmus, S.; Kelekci, S.; Aydogmus, H.; Eriş, S.; Desdicioğlu, R.; Yilmaz, B.; Sağlam, G. High prevalence of vitamin D deficiency among pregnant women in a Turkish population and impact on perinatal outcomes. J. Matern. Fetal Neonatal Med. 2015, 28, 1828–1832. [Google Scholar] [CrossRef] [PubMed]
- Hossain, N.; Kanani, F.H.; Ramzan, S.; Kausar, R.; Ayaz, S.; Khanani, R.; Pal, L. Obstetric and neonatal outcomes of maternal vitamin d supplementation: Results of an open-label, randomized controlled trial of antenatal vitamin d supplementation in pakistani women. J. Clin. Endocrinol. Metab. 2014, 99, 2448–2455. [Google Scholar] [CrossRef] [PubMed]
- Maghbooli, Z.; Hossein-Nezhad, A.; Karimi, F.; Shafaei, A.-R.; Larijani, B. Correlation between vitamin D3 deficiency and insulin resistance in pregnancy. Diabetes Metab. Res. Rev. 2008, 24, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Gur, E.B.; Gokduman, A.; Turan, G.A.; Tatar, S.; Hepyilmaz, I.; Zengin, E.B.; Eskicioglu, F.; Guclu, S. Mid-pregnancy vitamin D levels and postpartum depression. Eur. J. Obs. Gynecol. Reprod. Biol. 2014, 179, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Hossain, N.; Khanani, R.; Hussain-Kanani, F.; Tahira, S.; Shaheen, A.; Pal, L. High prevalence of vitamin D deficiency in Pakistani mothers and their newborns. Int. J. Gynecol. Obs. 2011, 112, 229–233. [Google Scholar] [CrossRef] [PubMed]
- Saraf, R.; Morton, S.M.B.; Camargo, C.A.; Grant, C.C. Global summary of maternal and newborn vitamin D status—A systematic review. Matern. Child Nutr. 2016, 12, 647–668. [Google Scholar] [CrossRef] [PubMed]
- Black, R.E.; Levin, C.; Walker, N.; Chou, D.; Liu, L.; Temmerman, M. Reproductive, maternal, newborn, and child health: Key messages from Disease Control Priorities 3rd Edition. Lancet 2016, 388, 2811–2824. [Google Scholar] [CrossRef]
- Aghajafari, F.; Nagulesapillai, T.; Ronksley, P.E.; Tough, S.C.; O’Beirne, M.; Rabi, D.M. Association between maternal serum 25-hydroxyvitamin D level and pregnancy and neonatal outcomes: Systematic review and meta-analysis of observational studies. Br. Med. J. 2013, 346. [Google Scholar] [CrossRef] [PubMed]
- Umesawa, M.; Kobashi, G. Epidemiology of hypertensive disorders in pregnancy: Prevalence, risk factors, predictors and prognosis. Hypertens. Res. 2016, 40, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Kassebaum, N.J.; Bertozzi-Villa, A.; Coggeshall, M.S.; Shackelford, K.A.; Steiner, C.; Heuton, K.R.; Gonzalez-Medina, D.; Barber, R.; Huynh, C.; Dicker, D.; et al. Global, regional, and national levels and causes of maternal mortality during 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 980–1004. [Google Scholar] [CrossRef]
- World Health Organisation. Vitamin D supplementation during pregnancy for the prevention of pre-eclampsia. In e-Library of Evidence for Nutrition Actions (eLENA); WHO: Geneva, Switzerland, 2016. [Google Scholar]
- The United Nations. Sustainable Development Goals Report; The United Nations: New York, NY, USA, 2017. [Google Scholar]
- The United Nations. Sustainable Development Goals: 17 Golas to Transform Our World; The United Nations: New York, NY, USA, 2015. [Google Scholar]
- Global nutrition report: Tracking progress, strengthening accountability, reducing malnutrition faster. In Nourishing the SDGs; Development Initiatives: Bristol, UK, 2017.
- World Health Organisation. Exclusive Breastfeeding for Six Motnhs Best for Babies Everywhere; WHO: Geneva, Switzerland, 2011. [Google Scholar]
- Takeuchi, A.; Okano, T.; Tsugawa, N.; Tasaka, Y.; Kobayashi, T.; Kodama, S.; Matsuo, T. Effects of ergocalciferol supplementation on the concentration of vitamin D and its metabolites in human milk. J. Nutr. 1989, 119, 1639–1646. [Google Scholar] [CrossRef] [PubMed]
- Saadi, H.F.; Dawodu, A.; Afandi, B.O.; Zayed, R.; Benedict, S.; Nagelkerke, N. Efficacy of daily and monthly high-dose calciferol in vitamin D–deficient nulliparous and lactating women. Am. J. Clin. Nutr. 2007, 85, 1565–1571. [Google Scholar] [CrossRef] [PubMed]
- Nozza, J.M.; Rodda, C.P. Vitamin D deficiency in mothers of infants with rickets. Med. J. Aust. 2001, 175, 253–255. [Google Scholar] [PubMed]
- Elder, C.J.; Bishop, N.J. Rickets. Lancet 2014, 383, 1665–1676. [Google Scholar] [CrossRef]
- Baker, R.D.; Greer, F.R. Diagnosis and prevention of iron deficiency and iron-deficiency anemia in infants and young children (0–3 years of age). Pediatrics 2010, 126, 1040–1050. [Google Scholar] [CrossRef] [PubMed]
- Taren, D.; Lutter, C.K. The role of breastfeeding protection, promotion and support in a developing world. In Nutrition and Health in a Developing World; de Pee, S., Taren, D., Bloem, M.W., Eds.; Springer International Publishing: Cham, Switzerland, 2017. [Google Scholar]
- Davies-Tuck, M.; Yim, C.; Knight, M.; Hodges, R.; Doery, J.C.; Wallace, E. Vitamin D testing in pregnancy: Does one size fit all? Aust. N. Z. J. Obstet. Gynaecol. 2015, 55, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Christesen, H.T.; Elvander, C.; Lamont, R.F.; Jorgensen, J.S. The impact of vitamin D in pregnancy on extraskeletal health in children: A systematic review. Acta Obstet. Gynecol. Scand. 2012, 91, 1368–1380. [Google Scholar] [CrossRef] [PubMed]
- Karras, S.N.; Anagnostis, P.; Paschou, S.A.; Kandaraki, E.; Goulis, D.G. Vitamin D status during pregnancy: Time for a more unified approach beyond borders? Eur. J. Clin. Nutr. 2015, 69, 874–877. [Google Scholar] [CrossRef] [PubMed]
- Arneson, W.L.; Arneson, D.L. Current methods for routine clinical laboratory testing of Vitamin D levels. Lab. Med. 2013, 44, e38–e42. [Google Scholar] [CrossRef]
- Sempos, C.T.; Vesper, H.W.; Phinney, K. Vitamin D Standardization Program (VDSP). Available online: https://ods.od.nih.gov/Research/vdsp.aspx (accessed on 17 May 2018).
- World Health Organisation. Vitamin D supplementation during pregnancy: Guidance summary. In e-Library of Evidence for Nutrition Actions (eLENA); WHO: Geneva, Switzerland, 2017. [Google Scholar]
- Pérez-López, F.R.; Pasupuleti, V.; Mezones-Holguin, E.; Benites-Zapata, V.A.; Thota, P.; Deshpande, A.; Hernandez, A.V. Effect of vitamin D supplementation during pregnancy on maternal and neonatal outcomes: A systematic review and meta-analysis of randomized controlled trials. Fertil. Steril. 2015, 103, 1278–1288. [Google Scholar] [CrossRef] [PubMed]
- Veselka, B.; van der Merwe, A.E.; Hoogland, M.L.P.; Waters-Rist, A.L. Gender-related vitamin D deficiency in a Dutch 19th century farming community. Int. J. Paleopathol. 2017. [Google Scholar] [CrossRef]
| Study | Design | Recruitment | Sample | Serum Vitamin D Measurement | Criteria for Vitamin D Deficiency and Reported Prevalence | Outcomes | Risk Factors |
|---|---|---|---|---|---|---|---|
| Ajmani et al., 2016 India [24] | Prospective cohort | Approached/screened: not reported Enrolled: not reported Complete data: n = 200 burka-clad women Setting: antenatal clinic and inpatients in antenatal ward at Kasturba Hospital, Delhi Season: all (year-long) | Age: mean 24.8 years Demographics: 64.5% multigravida, 44% dark complexion, 36% low SES, 64% illiterate, 2.5% graduate level educated Trimester: not reported Exclusion criteria: non-burka clad, age <18 years or >40 years, history of liver/renal disease, osteoporosis or rheumatoid arthritis, antitubercular or antiepileptic treatment in last 6 months, taking vitamin D supplements | ELISA | Criteria *: Deficiency < 50 nmol/L Inadequacy 50–75 nmol/L Adequate > 75 nmol/L Prevalence of deficiency: Deficient n = 75 (37.5%) Inadequate n = 78 (39%) Adequate n = 47 (23.5%) | Maternal: 7.5% women diagnosed with pre-eclampsia, significant correlation between VDD and pre-eclampsia (p = 0.001) Neonatal: 9.5% LBW babies, significant correlation between VDD and LBW (p = 0.0001) No correlation: VDD and GDM, LSCS, bony abnormality, Apgar score, premature birth or NICU admission | Dark skin complexion, limited outdoor activity, low dairy intake, low fish intake (p < 0.05) |
| Ates et al., 2016 Turkey [37] | Prospective cohort | Approached/screened: n = 286 Enrolled: n = 266 (93%) Complete data: n = 229 (86%) Setting: first antenatal appointment at outpatient clinic of Obstetrics and Gynecology, Bezmialem Vakif University, Istanbul Season: 48.9% summer (May–October), 51.1% winter (November–April) | Age: mean 29.5 years Demographics: 64.5% primigravida, mean BMI 25.3 kg/m2, 61.3% covered dress, 63.1% multivitamin use, 6.6% smoking, 46.9% ≥ 9 years education Trimester: first Exclusion criteria: thyroid, parathyroid or adrenal disease, hepatic or renal failure, metabolic bone disease, medication affecting vitamin D metabolism, multiple pregnancy, taking vitamin D supplements | LC-MS/MS | Criteria *: Severe deficiency < 25 nmol/L Mod deficiency 25–47.5 nmol/L Mild deficiency 50–72.5 nmol/L Adequate > 75 nmol/L Prevalence of deficiency: Severe n = 105 (45.9%) Mod n = 83 (36.2%) Mild n = 31 (13.5%) Adequate n = 10 (4.4%) | Maternal: 53.8% women with severe VDD had vaginal delivery, compared with 32.7% as primary caesarean section (p = 0.018) No correlation: VDD and GDM, pre-eclampsia, gestational hypertension, preterm birth, SGA, intrauterine fetal death, congenital malformation, birth weight or Apgar score | Covered dress, non-multivitamin use, winter (p < 0.05) |
| Aydogmus et al., 2014 Turkey [38] | Prospective cohort | Approached/screened: n = 180 Enrolled: n = 152 (84%) Complete data: n = 148 (97%) Setting: inpatients at Izmir Katip Celebi University Ataturk Training and Research Hospital, Izmir Season: not reported | Age: mean 24.4 years Demographics: not reported Trimester: third Exclusion criteria: taking vitamin D supplements, multiparity, disease affecting vitamin D and calcium metabolism, medications for chronic disease | ELISA | Criteria *: Deficient < 37.5 nmol/L Insufficient 37.5–72.5 nmol/L Sufficient > 75 nmol/L (grouped for analysis Deficient < 37.5 nmol/L; Other ≥ 37.5 nmol/L) Prevalence of deficiency: Deficient: n = 66 (44.6%) Other n = 82 (55.4%) | Maternal: 39.9% women with VDD had poor pregnancy outcomes compared with 23.2% of women without VDD (p = 0.001), VDD increased risk of perinatal complications (OR 4.30; 95% CI 1.85–9.99) Neonatal: 16.7% SGA neonates born to mothers with VDD compared with 4.9% neonates born to mothers without VDD (p = 0.007), VDD increased risk of SGA (OR 4.5; 95% CI 1.41–15.78); mean birthweight significantly lower for neonates born to mothers with VDD (3187.6 ± 495.5 g) compared with those born to mothers without VDD (3268.1 ± 477.1 g) (p = 0.02) No correlation: VDD and mode of delivery, post maturity, GDM, maternal anemia, hypertension, pre-eclampsia, cholestasis, oligohydraminos, fetal distress, still birth, preterm labor, PPROM, Apgar scores, prolonged hospitalization, mortality, NICU admission or macrosomia | No significant associations |
| Chen et al., 2015 China [35] | Prospective cohort | Approached/screened: n = 4358 (sub-sample of a population-based cohort study n = 16,766) Enrolled: n = 3658 (84%) Complete data: 3658 (100%) Setting: women recruited to the larger China-Anhui Birth Cohort study from six major cities of Anhui province Season: all (year-long), 36.7% spring, 22.5% summer, 20.6% autumn, 20.2% winter | Age: mean 27.5 years Demographics: 96.0% nulliparous, 45.2% low income, 75.3% healthy BMI, 16.5% multivitamin use Trimester: all, 35.1% first, 62.0% second, 2.9% third Exclusion criteria: multiple pregnancy, abortion | RIA | Criteria *: Deficient < 50 nmol/L Insufficient 50–74.75 nmol/L Sufficient ≥ 75 nmol/L Prevalence of deficiency: Deficiency n = 1405 (38.4%) Insufficiency n = 1289 (35.2%) Sufficient n = 964 (26.4%) | Maternal: not assessed Neonatal: 16.01% SGA neonates born to mothers with VDD compared with 5.59% born to mothers with vitamin D insufficiency and 2.80% with sufficient vitamin D (p < 0.001); compared to sufficiency, maternal VDD increased risk of SGA (RR 6.47; 95% CI 4.30–9.75) and insufficiency (RR 2.01; 95% CI 1.28–3.16) (p < 0.001); 4.98% LBW neonates born to mothers with VDD compared with 1.32% born to mothers with vitamin D insufficiency and 0.41% with sufficient vitamin D (p < 0.001); VDD increased risk of LBW (RR 12.31; 95% CI 4.47–33.89) (p < 0.001). Adjusted for: Pre-pregnancy maternal BMI, maternal age, season and gestational week | Not assessed |
| Farrant et al., 2009 India [34] | Prospective cohort | Approached/screened: n = 1539 Enrolled: n = 830 (54%) Complete data: n = 674 (81%) Setting: women attending antenatal clinic at Holdsworth Memorial Hospital, Mysore Season: all (year-long) | Age: mean 23.7 years Demographics: mean BMI 23.4 kg/m2, women supplemented at recruitment (n = 156) with vitamin D as part of routine management, no information available at 30 weeks Trimester: third Exclusion criteria: not reported | RIA | Criteria: Hypovitaminosis < 50 nmol/L Adequate > 50 nmol/L Prevalence of deficiency: Hypovitaminosis n = 372 (67%) Adequate: n = 187 (33%) | No correlation: VDD and GDM, birthweight, impaired fetal growth | Autumn/winter (p < 0.05) |
| Gbadegesin et al., 2016 Nigeria [27] | Prospective cohort | Approached/screened: not reported Enrolled: n = 461 Complete data: n = 461 (100%) Setting: maternity unit of the Lagos State University Teaching Hospital, Ikeja and women of mixed ethnicity, social class and religion Season: all (year-long) | Age: mean 31.3 years Demographics: mean parity 1.16 Trimester: all Exclusion criteria: multiple pregnancy, previous medical condition (hypertension, renal disease, diabetes), taking vitamin D supplements, elevated BP | HPLC | Criteria *: Deficiency < 50 nmol/L Insufficiency 52.5–75 nmol/L Adequate > 75 nmol/L Prevalence of deficiency: Deficiency n = 134 (29.0%) Insufficiency n = 48 (10.4%) Adequate n = 279 (60.6%) | No correlation: VDD and preeclampsia, SROM, anemia, GDM, preterm delivery, mode of delivery, Apgar score or stillbirth | No significant associations |
| Gur et al., 2014 Turkey [41] | Prospective cohort | Approached/screened: n = 687 Enrolled: n = 208 (30%) Complete data: n = 189 at 1/52 (91%); n = 184 at 6/52 (88%); n = 179 at 6/12 (86%) Setting: women attending routine antenatal reviews at Sifa University Bornova Health Research and Application Hospital, Izmir Season: summer/autumn | Age: mean 28.5 years Demographics: mean BMI 26.5 kg/m2, 7.6% women supplemented with vitamin D ≥ 3 days per week and 84.6% supplemented daily, all women Caucasian and native Turkish speaking Trimester: second Exclusion criteria: unmarried, unplanned pregnancy, BMI < 20 or >30 kg/m2, smoker, diagnosed psychiatric illness, pre-diagnosed medical condition, parity > 3, education level < 8 years, multiple birth, employed, annual income < US $450, fetal death, complex delivery, newborn with anomaly, postpartum bleeding or hysterectomy | ELISA | Criteria *: Severe deficiency < 25 nmol/L Mild deficiency 25 nmol/L–50 nmol/L Normal ≥ 50 nmol/L Prevalence of deficiency: Severe: n = 23 (11%) Mild n = 84 (40.3%) Normal n = 101 (48.5%) | Maternal: 21.1%, 23.2% and 23.7% women had PPD at week 1, 6 and 6 months respectively; significant negative correlation (r = −0.2, −0.2, −0.3) between vitamin D levels and Edinburgh Postnatal Depression Scale (EPDS) score at each of the three time points; mean vitamin D level was significantly different between women with and without PPD at each of the three time points (p = 0.003, p = 0.004 and p < 0.001 respectively) Neonatal: not assessed | Not assessed |
| Hossain et al., 2010 Pakistan [39] | Cross-sectional | Approached: not reported (all women admitted to the labor suite for delivery during the study period were deemed eligible) RR: not reported Complete data: n = 75 Setting: delivery at Dow University of Health Sciences and Civil Hospital, Karachi Season: spring | Age: mean 26.0 years Demographics: mean BMI 27 kg/m2, mean parity 2.2, 26% covering arms, hands heads, 76% covering face Trimester: third Exclusion criteria: not reported | CI | Criteria *: Severe deficiency < 25 nmol/L Mod deficiency 27.5–50 nmol/L Mild deficiency 52.5–60 nmol/L Adequate > 60 nmol/L Prevalence of deficiency: Severe: n = 34 (45%) Mod: n = 20 (27%) Mild: n = 13 (17%) Adequate: n = 8 (11%) | Maternal: compared with women in the highest tertile for vitamin D, women in the lowest tertile and mid-tertile were more likely to meet criteria for pre-eclampsia and gestational pre-hypertension (OR 2.28; 95% CI 0.35–23.28) and (OR 19.27; 95% CI 1.96–188.92 respectively); vitamin D levels were inversely correlated with maternal mean arterial pressure (r = 0.029) (p = 0.020) Neonatal: not assessed in relation to maternal vitamin D Adjusted for maternal age, level of exercise, maternal weight, birthweight and gestational age | Not assessed |
| Maghbooli et al., 2008 Iran [40] | Cross-sectional | Approached/screened: not reported Enrolled: n = 741 Complete data: n = 579 Setting: referral to five university hospital clinics of the Tehran University of Medical Sciences during the first half of pregnancy Season: not reported | Age: mean 27.4 years Demographics: mean BMI 26.4 kg/m2 Trimester: second Exclusion criteria: prenatal diabetes | RIA | Criteria: Severe deficiency < 12.5 nmol/L Mild deficiency 12.5–24.9 nmol/L Mod deficiency 25–34.9 nmol/L Sufficiency > 34.9 nmol/L Prevalence of deficiency: Severe n = 201 (27.1%) Mild n = 118 (15.9%) Mod n = 344 (46.4%) Sufficient n = 78 (10.5%) | Maternal: 52% women diagnosed with GDM, mean vitamin D significantly lower in women with GDM (16.49 ± 10.44 nmol/L) compared with non-GDM women (22.97 ± 18.25 nmol/L) (p = 0.009), prevalence of severe VDD was significantly higher in women with GDM (44.2%) compared with non-GDM women (23.5%) (p = 0.011) Neonatal: not assessed | Not assessed |
| Pirdehghan et al., 2016 Iran [25] | Cross-sectional | Approached/screened: not reported Enrolled: not reported Complete data: n = 200 Setting: admission to hospital delivery room for natural delivery, caesarean section or abortion at Shahid Sadoughi hospital Season: autumn/spring | Age: mean 26.7 years Demographics: all women nulliparous, 48.7% diploma/university educated, 97.5% housewives, 38.5% women taking multivitamins containing vitamin D during pregnancy, Trimester: not reported Exclusion criteria: pre-existing medical conditions (renal or bone disorders), medication influencing calcium or vitamin D metabolism. multiparity | ELISA | Criteria *: Severe deficiency < 25 nmol/L Moderate deficiency 25–50 nmol/L Mild deficiency 52.5–75 nmol/L Adequate 75–125 nmol/L Upper normal/toxic > 125 nmol/L Prevalence of deficiency: (figures reported in text) Severe 12.5% Deficiency 60% | Maternal: mean vitamin D significantly higher in natural or elective caesarean section women compared with abortion and emergency caesarean section women (p = 0.040); VDD associated with risk of abortion 3.1 (1.39–6.8) which was higher in severe deficiency women compared with VDD women (p = 0.045), mean vitamin D significantly lower in women with oligohydramnios or polyhydramnios complication (13.9 + 9.5 and 20.6 + 10.8 respectively) (p = 0.045) No correlation: VDD and preeclampsia, PROM, GDM, birth weight, birth length, head circumference or Apgar score | No significant associations |
| Song et al., 2012 China [26] | Cross-sectional | Approached/screened: not reported Enrolled: not reported Complete data: 70 Setting: delivery at 306 Hospital of PLA in Beijing from surrounding communities of the Beijing urban area Season: spring | Age: 29.9 (±0.3) years Demographics: Mean weight: 73.9 kg, pregravid range 0–3 Trimester: third Exclusion criteria: multiparity, taking calcium and/or vitamin D supplements, pre-existing medical conditions (hypertension, renal disease, pre-gestational diabetes) | ELISA | Criteria: Severe deficiency < 25 nmol/L Mild deficiency 25– < 50 nmol/L Insufficiency 50– < 75 nmol/L (21–29 ng/mL) Sufficiency ≥ 75 nmol/L (grouped for analysis Deficient < 25 nmol/L and other ≥ 25 nmol/L Prevalence of deficiency: Severe n = 38 (54.5%) Mild n = 25 (35.7%) Insufficient n = 7 (10.0%) Sufficient n = 0 (0%) | Maternal: not assessed Neonatal: significant correlation between maternal vitamin D and newborn length (r = 0.247) (p = 0.039); compared with women who had vitamin D ≥ 25 nmol/L, birth weight (3633.1 g) and length (51.0 cm) of newborns were significantly lower in women with vitamin D < 25 nmol/L (3386 g and 50.2 cm respectively) (p = 0.015, p = 0.037) No correlation: VDD or head circumference | Not assessed |
| Toko et al., 2016 Kenya [6] | Longitudinal | Approached/screened: n = 99 RR: not reported Complete data: n = 63 (baseline data used) (64%) Setting: women residing within a 10 km radius of Chulaimbo Sub-district hospital in Kisumu County Season: dry season | Age: mean 22.5 years Demographics: mean BMI 22.9 kg/m2 Trimester: second and third Exclusion criteria: more than 26 weeks gestation, HIV infected, residing >10 km from the hospital | ELISA | Criteria: Deficiency < 50 nmol/L Insufficiency 50–75 nmol/L Sufficiency > 75 nmol/L (grouped for analysis low < 50 nmol/L and adequate ≥ 50 nmol/L) Prevalence of deficiency: Deficient n = 13 (20.6%) Insufficient n = 32 (50.8%) Sufficient n = 19 (28.6%) | Maternal: not assessed Neonatal: newborns more likely to have stunted growth at birth when born to mothers with deficient vitamin D (RR 4.4 (CI 1.0–18.6) (p = 0.04) and more likely to be born preterm (<37 weeks) (RR 5.4 (CI 1.1, 25.3) (p = 0.03) Adjusted for: maternal age, gestational age at delivery and maternal BMI No correlation: VDD and wasting or BMI z-score | Not assessed |
| Xin et al., 2017 China [36] | Prospective cohort | Approached/screened: not reported Enrolled: n = 13,806 Complete data: n = 11,151 (81%) Setting: routine visit to antenatal care clinic and delivery at the Wuxi Maternity and Child Health Hospital Season: 28.4% winter, 18.5% spring, 22.7% autumn, 30.4% summer | Age: mean 27.3 years Demographics: 88.9% nulliparous, 9.2% BMI ≥ 25 kg/m2, 96% GA at delivery ≥ 37 weeks Trimester: second and third Exclusion criteria: taking calcium and/or vitamin D supplements, pre-existing medical conditions (hypertension, renal disease, pre-gestational diabetes), fetal anomalies | CI | Criteria: Deficiency < 50 nmol/L Sufficiency > 50 nmol/L Prevalence of deficiency: Deficient n = 8799 (78.9%) Sufficient n = 2352 (20.8%) | Maternal: 1.2% pre-eclampsia, significant difference in incidence of severe pre-eclampsia in pregnant women with VDD (<50 nmol/L) (n = 123; 1.4%) compared with sufficiency (≥50 nmol/L) (n = 16; 0.6%) (p = 0.002), women with VDD were more at risk of developing severe pre-eclampsia compared with women who were vitamin D sufficient (OR: 3.16; 95% CI: 1.77–5.65) (p = 0.000) Adjusted for: pre-pregnancy BMI, maternal age, parity and season of blood sampling Neonatal: not assessed | Age ≥ 35 years, pre-pregnancy BMI ≥ 25 kg/m2, nulliparity (p < 0.05) |
| Maternal Outcomes | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | PE | GDM | Anemia | GHTN | OHD | Mode of Delivery * | Cholestasis | PPO | PH | MMAP | PPD | PC | PROM/SROM |
| Ajmani et al. (2016) India [24] | + | - | - | ||||||||||
| Ates et al. (2016) Turkey [37] | - | - | - | + | |||||||||
| Aydogmus et al. (2014) Turkey [38] | - | - | - | - | - | - | - | + | - | + | - | ||
| Chen et al. (2015) China [35] | |||||||||||||
| Farrant et al. (2009) India [34] | - | ||||||||||||
| Gbadegesin et al. (2016) Nigeria [27] | - | - | - | - | - | ||||||||
| Gur et al. (2014) Turkey [41] | + | ||||||||||||
| Hossain et al. (2010) Pakistan [39] | + | + | + | ||||||||||
| Maghbooli et al. (2008) Iran [40] | + | ||||||||||||
| Pirdehghan et al. (2016) Iran [25] | - | - | + | - | |||||||||
| Song et al. (2012) China [26] | |||||||||||||
| Toko et al. (2016) Kenya [6] | |||||||||||||
| Xin et al. (2017) China [36] | + | ||||||||||||
| Neonatal Outcomes | |||||||||||||
| Study | Macro. | Stunted Growth * | Preterm Birth | W z-Score | Still Birth/IFD | NICU Admit | Apgar Score | Post MB | HC | CM * | Birth Weight * | Birth Length | SGA |
| Ajmani et al. (2016) India [24] | - | - | - | - | + | ||||||||
| Ates et al. (2016) Turkey [37] | - | - | - | - | - | - | |||||||
| Aydogmus et al. (2014) Turkey [38] | - | - | - | - | - | - | + | + | |||||
| Chen et al. (2015) China [35] | + | + | |||||||||||
| Farrant et al. (2009) India [34] | - | - | |||||||||||
| Gbadegesin et al. (2016) Nigeria [27] | - | - | - | ||||||||||
| Gur et al. (2014) Turkey [41] | |||||||||||||
| Hossain et al. (2010) Pakistan [39] | |||||||||||||
| Maghbooli et al. (2008) Iran [40] | |||||||||||||
| Pirdehghan et al. (2016) Iran [25] | - | - | - | - | |||||||||
| Song et al. (2012) China [26] | - | + | + | ||||||||||
| Toko et al. (2016) Kenya [6] | + | + | - | ||||||||||
| Xin et al. (2017) China [36] | |||||||||||||
| Study | Selection Bias | Study Design | Cofounders | Blinding | Data Collection Method | Withdrawals and Dropouts | Global Rating |
|---|---|---|---|---|---|---|---|
| Ajmani et al. (2016) India [24] | 3 | 3 | 3 | 3 | 1 | 3 | Weak |
| Ates et al. (2016) Turkey [37] | 1 | 3 | 3 | 3 | 1 | 1 | Weak |
| Aydogmus et al. (2015) Turkey [38] | 2 | 3 | 3 | 3 | 1 | 1 | Weak |
| Chen et al. (2015) China [35] | 1 | 3 | 1 | 3 | 1 | 1 | Weak |
| Farrant et al. (2009) India [34] | 2 | 3 | 3 | 3 | 1 | 2 | Weak |
| Gbadegesin et al. (2016) Nigeria [27] | 3 | 3 | 3 | 3 | 1 | 3 | Weak |
| Gur et al. (2014) Turkey [41] | 3 | 3 | 3 | 2 | 1 | 1 | Weak |
| Hossain et al. (2010) Pakistan [39] | 3 | 3 | 3 | 3 | 1 | 3 | Weak |
| Maghbooli et al. (2008) Iran [40] | 2 | 3 | 3 | 3 | 1 | 3 | Weak |
| Pirdehghan et al. (2016) Iran [25] | 3 | 3 | 3 | 2 | 1 | 3 | Weak |
| Song et al. (2012) China [26] | 3 | 3 | 3 | 3 | 1 | 3 | Weak |
| Toko et al. (2016) Kenya [6] | 3 | 3 | 1 | 3 | 1 | 3 | Weak |
| Xin et al. (2017) China [36] | 2 | 3 | 1 | 3 | 1 | 1 | Weak |
| Quality Rating | |||
|---|---|---|---|
| Quality Component | Strong (n) | Moderate (n) | Weak (n) |
| Selection bias | 2/13 | 4/13 | 7/13 |
| Study design | 0/13 | 0/13 | 13/13 |
| Confounders | 3/13 | 0/13 | 10/13 |
| Blinding | 0/13 | 2/13 | 11/13 |
| Data collection methods | 13/13 | 0/13 | 0/13 |
| Withdrawal and dropout | 5/13 | 1/13 | 7/13 |
| Global rating | 0/13 | 0/13 | 13/13 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Van der Pligt, P.; Willcox, J.; Szymlek-Gay, E.A.; Murray, E.; Worsley, A.; Daly, R.M. Associations of Maternal Vitamin D Deficiency with Pregnancy and Neonatal Complications in Developing Countries: A Systematic Review. Nutrients 2018, 10, 640. https://doi.org/10.3390/nu10050640
Van der Pligt P, Willcox J, Szymlek-Gay EA, Murray E, Worsley A, Daly RM. Associations of Maternal Vitamin D Deficiency with Pregnancy and Neonatal Complications in Developing Countries: A Systematic Review. Nutrients. 2018; 10(5):640. https://doi.org/10.3390/nu10050640
Chicago/Turabian StyleVan der Pligt, Paige, Jane Willcox, Ewa A. Szymlek-Gay, Emily Murray, Anthony Worsley, and Robin M. Daly. 2018. "Associations of Maternal Vitamin D Deficiency with Pregnancy and Neonatal Complications in Developing Countries: A Systematic Review" Nutrients 10, no. 5: 640. https://doi.org/10.3390/nu10050640
APA StyleVan der Pligt, P., Willcox, J., Szymlek-Gay, E. A., Murray, E., Worsley, A., & Daly, R. M. (2018). Associations of Maternal Vitamin D Deficiency with Pregnancy and Neonatal Complications in Developing Countries: A Systematic Review. Nutrients, 10(5), 640. https://doi.org/10.3390/nu10050640






