Dermatitis Herpetiformis: A Common Extraintestinal Manifestation of Coeliac Disease
Abstract
:1. Introduction
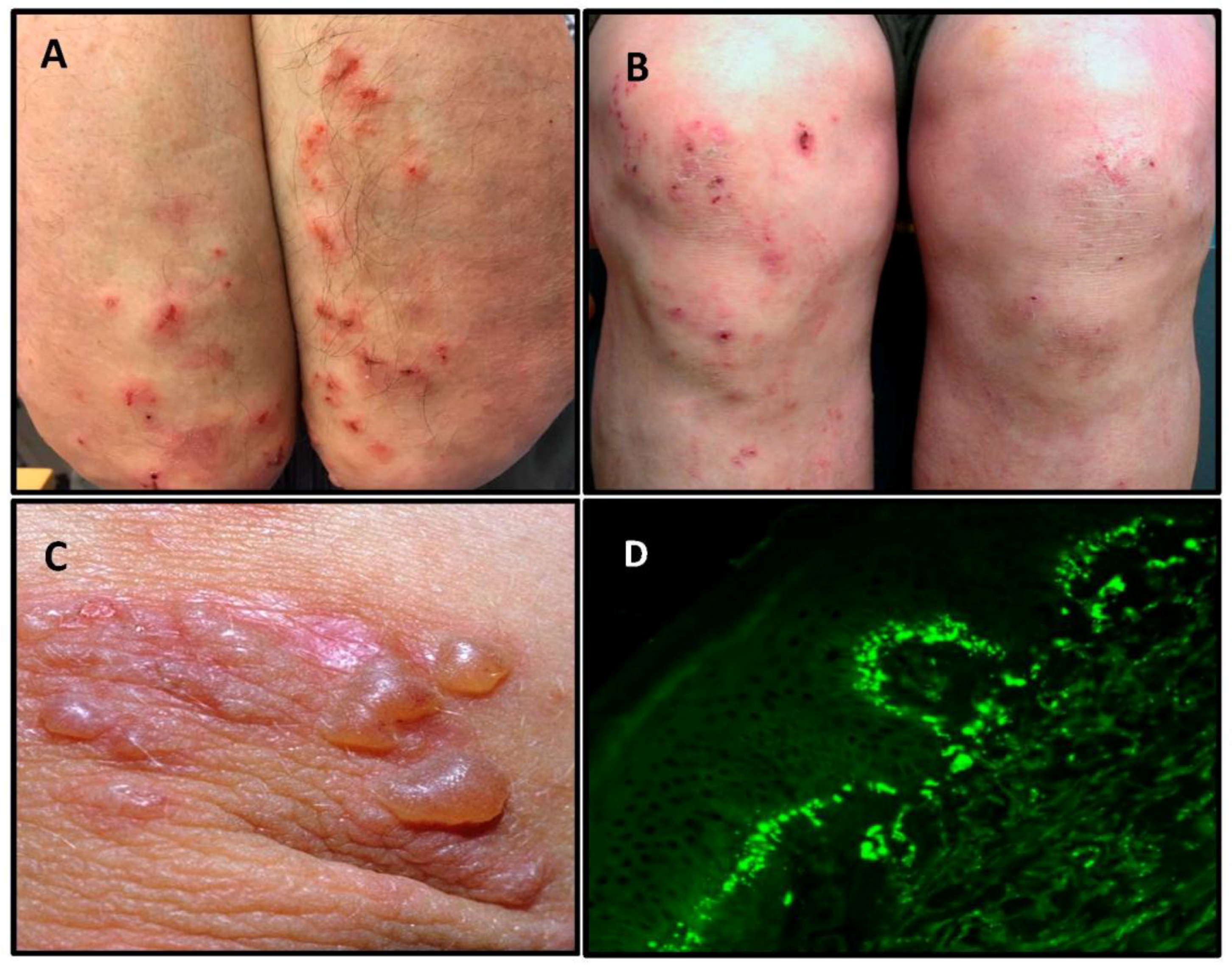
2. Clinical Presentation and Diagnosis of Dermatitis Herpetiformis
3. Gender and Age at Onset
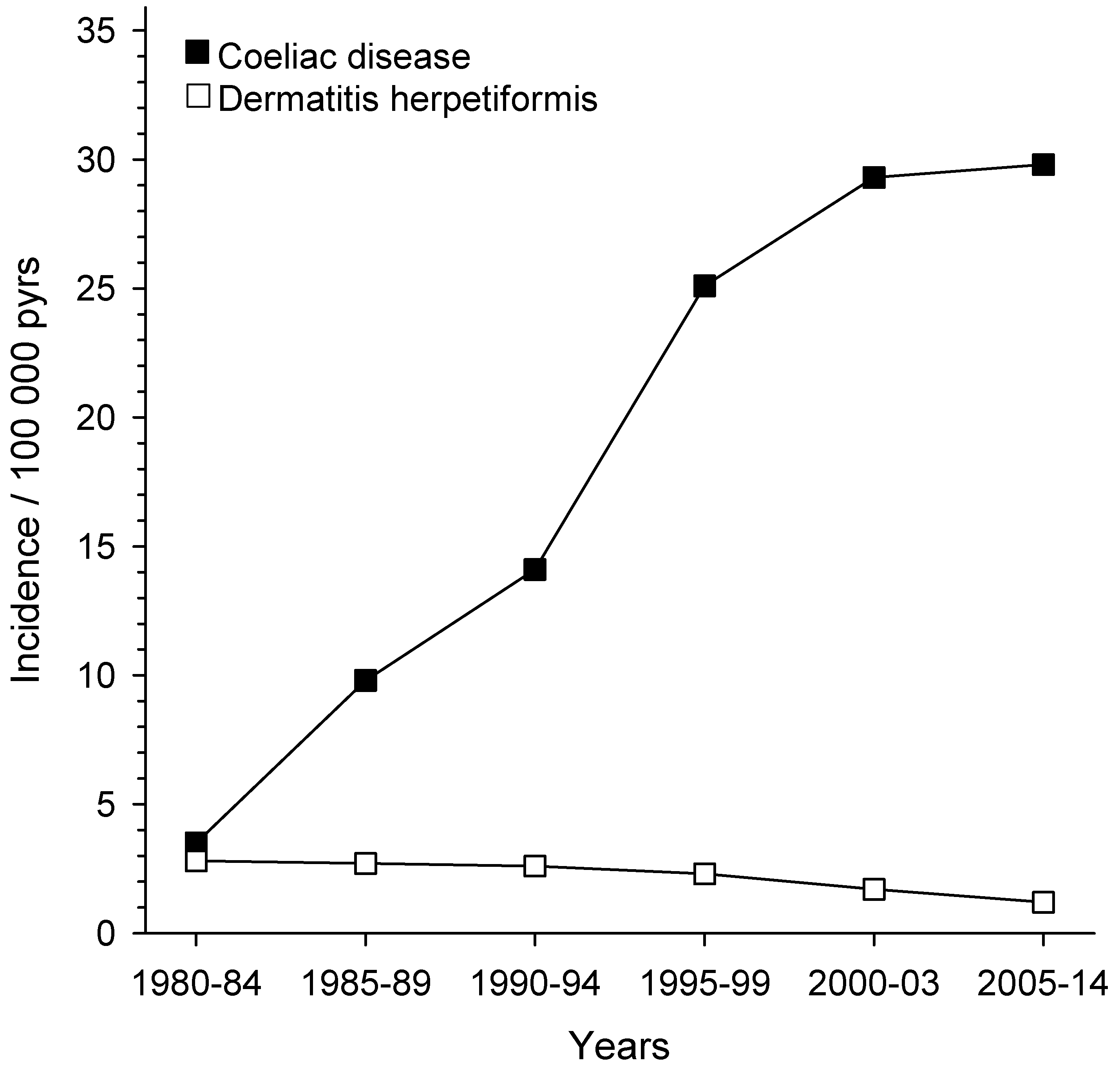
4. Prevalence and Incidence
5. Pathogenesis of Dermatitis Herpetiformis: From Gut to Skin
6. Long-Term Prognosis on a Gluten-Free Diet Treatment
7. Concluding Remarks
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Duhring, L.A. Landmark article, Aug 30, 1884: Dermatitis herpetiformis. By Louis A. Duhring. JAMA 1983, 250, 212–216. [Google Scholar] [CrossRef] [PubMed]
- Losowsky, M.S. A history of coeliac disease. Dig. Dis. 2008, 26, 112–120. [Google Scholar] [CrossRef] [PubMed]
- Bolotin, D.; Petronic-Rosic, V. Dermatitis herpetiformis. Part I. Epidemiology, pathogenesis, and clinical presentation. J. Am. Acad. Dermatol. 2011, 64, 1017–1024. [Google Scholar] [CrossRef] [PubMed]
- Van der Meer, J.B. Granular deposits of immunoglobulins in the skin of patients with dermatitis herpetiformis. An immunofluorescent study. Br. J. Dermatol. 1969, 81, 493–503. [Google Scholar] [CrossRef] [PubMed]
- Marks, J.; Shuster, S.; Watson, A.J. Small-bowel changes in dermatitis herpetiformis. Lancet 1966, 2, 1280–1282. [Google Scholar] [CrossRef]
- Savilahti, E.; Reunala, T.; Mäki, M. Increase of lymphocytes bearing the gamma/delta T cell receptor in the jejunum of patients with dermatitis herpetiformis. Gut 1992, 33, 206–211. [Google Scholar] [CrossRef] [PubMed]
- Fry, L.; Seah, P.P.; Riches, D.J.; Riches, D.J.; Hoffbrand, A.V. Clearance of skin lesions in dermatitis herpetiformis after gluten withdrawal. Lancet 1973, 1, 288–291. [Google Scholar] [CrossRef]
- Reunala, T.; Blomqvist, K.; Tarpila, S.; Halme, H.; Kangas, K. Gluten-free diet in dermatitis herpetiformis. I. Clinical response of skin lesions in 81 patients. Br. J. Dermatol. 1977, 97, 473–480. [Google Scholar] [CrossRef] [PubMed]
- Leonard, J.; Haffenden, G.; Tucker, W.; Unsworth, J.; Swain, F.; McMinn, R.; Holborow, J.; Fry, L. Gluten challenge in dermatitis herpetiformis. N. Engl. J. Med. 1983, 308, 816–819. [Google Scholar] [CrossRef] [PubMed]
- Garioch, J.J.; Lewis, H.M.; Sargent, S.A.; Leonard, J.N.; Fry, L. 25 years’ experience of a gluten-free diet in the treatment of dermatitis herpetiformis. Br. J. Dermatol. 1994, 131, 541–545. [Google Scholar] [CrossRef] [PubMed]
- Balas, A.; Vicario, J.L.; Zambrano, A.; Acuna, D.; Garcıa-Novo, D. Absolute linkage of celiac disease and dermatitis herpetiformis to HLA-DQ. Tissue Antigens 1997, 50, 52–56. [Google Scholar] [CrossRef] [PubMed]
- Hervonen, K.; Hakanen, M.; Kaukinen, K.; Collin, P.; Reunala, T. First-degree relatives are frequently affected in coeliac disease and dermatitis herpetiformis. Scand. J. Gastroenterol. 2002, 37, 51–55. [Google Scholar] [CrossRef] [PubMed]
- Hervonen, K.; Karell, K.; Holopainen, P.; Collin, P.; Partanen, J.; Reunala, T. Concordance of dermatitis herpetiformis and celiac disease in monozygous twins. J. Investig. Dermatol. 2000, 115, 990–993. [Google Scholar] [CrossRef] [PubMed]
- Mansikka, E.; Salmi, T.; Kaukinen, K.; Collin, P.; Huhtala, H.; Reunala, T.; Hervonen, K. Diagnostic delay in dermatitis herpetiformis in a high-prevalence area. Acta Derm. Venereol. 2018, 98, 195–199. [Google Scholar] [CrossRef] [PubMed]
- Chanal, J.; Ingen-Housz-Oro, S.; Ortonne, N.; Duong, T.A.; Thomas, M.; Valeyrie-Allanore, L.; Lebrun-Vignes, B.; André, C.; Roujeau, J.C.; Chosidow, O.; et al. Linear IgA bullous dermatosis: Comparison between the drug-induced and spontaneous forms. Br. J. Dermatol. 2013, 169, 1041–1048. [Google Scholar] [CrossRef] [PubMed]
- Caproni, M.; Antiga, E.; Melani, L.; Fabbri, P. Guidelines for the diagnosis and treatment of dermatitis herpetiformis. J. Eur. Acad. Dermatol. Venereol. 2009, 23, 633–638. [Google Scholar] [CrossRef] [PubMed]
- Zone, J.J.; Meyer, L.J.; Petersen, M.J. Deposition of granular IgA relative to clinical lesions in dermatitis herpetiformis. Arch. Dermatol. 1996, 132, 912–918. [Google Scholar] [CrossRef] [PubMed]
- Salmi, T.T.; Hervonen, K.; Kautiainen, H.; Collin, P.; Reunala, T. Prevalence and incidence of dermatitis herpetiformis: A 40-year prospective study from Finland. Br. J. Dermatol. 2011, 165, 354–359. [Google Scholar] [CrossRef] [PubMed]
- West, J.; Fleming, K.M.; Tata, L.J.; Card, T.R.; Crooks, C.J. Incidence and prevalence of celiac disease and dermatitis herpetiformis in the UK over two decades: Population-based study. Am. J. Gastroenterol. 2014, 109, 757–768. [Google Scholar] [CrossRef] [PubMed]
- Green, P.H.; Cellier, C. Celiac disease. N. Engl. J. Med. 2007, 357, 1731–1743. [Google Scholar] [CrossRef] [PubMed]
- Vilppula, A.; Kaukinen, K.; Luostarinen, L.; Krekelä, I.; Patrikainen, H.; Valve, R.; Mäki, M.; Collin, P. Increasing prevalence and high incidence of celiac disease in elderly people: A population-based study. BMC. Gastroenterol. 2009, 9, 49. [Google Scholar] [CrossRef] [PubMed]
- Fasano, A.; Berti, I.; Gerarduzzi, T.; Not, T.; Colletti, R.B.; Drago, S.; Elitsur, Y.; Green, P.H.; Guandalini, S.; Hill, I.D.; et al. Prevalence of celiac disease in at-risk and not-at-risk groups in the United States: A large multicenter study. Arch. Intern. Med. 2003, 163, 286–292. [Google Scholar] [CrossRef] [PubMed]
- Tack, G.J.; Verbeek, W.H.; Schreurs, M.W.; Mulder, C.J. The spectrum of celiac disease: Epidemiology, clinical aspects and treatment. Nat. Rev. Gastroenterol. Hepatol. 2010, 7, 204–213. [Google Scholar] [CrossRef] [PubMed]
- Alonso-Llamazares, J.; Gibson, L.E.; Rogers, R.S., 3rd. Clinical, pathologic, and immunopathologic features of dermatitis herpetiformis: Review of the Mayo Clinic experience. Int. J. Dermatol. 2007, 46, 910–919. [Google Scholar] [CrossRef] [PubMed]
- Hervonen, K.; Salmi, T.T.; Kurppa, K.; Kaukinen, K.; Collin, P.; Reunala, T. Dermatitis herpetiformis in children: A long-term follow-up study. Br. J. Dermatol. 2014, 171, 1242–1243. [Google Scholar] [CrossRef] [PubMed]
- Antiga, E.; Verdelli, A.; Calabri, A.; Fabbri, P.; Caproni, M. Clinical and immunopathological features of 159 patients with dermatitis herpetiformis: An Italian experience. G. Ital. Dermatol. Venereol. 2013, 148, 163–169. [Google Scholar] [PubMed]
- Dahlbom, I.; Korponay-Szabó, I.R.; Kovács, J.B.; Szalai, Z.; Mäki, M.; Hansson, T. Prediction of clinical and mucosal severity of coeliac disease and dermatitis herpetiformis by quantification of IgA/IgG serum antibodies to tissue transglutaminase. J. Pediatr. Gastroenterol. Nutr. 2010, 50, 140–146. [Google Scholar] [CrossRef] [PubMed]
- Collin, P.; Huhtala, H.; Virta, L.; Kekkonen, L.; Reunala, T. Diagnosis of celiac disease in clinical practice: Physician’s alertness to the condition essential. J. Clin. Gastroenterol. 2007, 41, 152–156. [Google Scholar] [CrossRef] [PubMed]
- Rampertab, S.D.; Pooran, N.; Brar, P.; Singh, P.; Green, P.H. Trends in the presentation of celiac disease. Am. J. Med. 2006, 119, 355.e9–355.e14. [Google Scholar] [CrossRef] [PubMed]
- Dominguez Castro, P.; Harkin, G.; Hussey, M.; Christopher, B.; Kiat, C.; Liong Chin, J.; Trimble, V.; McNamara, D.; MacMathuna, P.; Egan, B.; et al. Changes in presentation of celiac disease in Ireland from the 1960s to 2015. Clin. Gastroenterol. Hepatol. 2017, 15, 864–871. [Google Scholar] [CrossRef] [PubMed]
- Carlsson, A.; Agardh, D.; Borulf, S.; Grodzinsky, E.; Axelsson, I.; Ivarsson, S.A. Prevalence of celiac disease: Before and after a national change in feeding recommendations. Scand. J. Gastroenterol. 2006, 41, 553–558. [Google Scholar] [CrossRef] [PubMed]
- Finnish National Nutrition Council. Action Programme for Implementing National Nutrition Recommendations; Edita Prima: Helsinki, Finland, 2003. (In Finnish) [Google Scholar]
- Mansikka, E.; Hervonen, K.; Salmi, T.T.; Kautiainen, H.; Kaukinen, K.; Collin, P.; Reunala, T. The decreasing prevalence of severe villousa atrophy in Dermatitis herpetiformis: A 45-year experience in 393 patients. J. Clin. Gastroenterol. 2017, 51, 235–239. [Google Scholar] [PubMed]
- Brar, P.; Kwon, G.Y.; Egbuna, I.I.; Holleran, S.; Ramakrishnan, R.; Bhagat, G.; Green, P.H. Lack of correlation of degree of villous atrophy with severity of clinical presentation of coeliac disease. Dig. Liver Dis. 2007, 39, 26–29. [Google Scholar] [CrossRef] [PubMed]
- Green, P.H.R.; Stavropoulos, S.N.; Panagi, S.G.; Goldstein, S.L.; Mcmahon, D.J.; Absan, H.; Neugut, A.I. Characteristics of adult celiac disease in the USA: Results of a national survey. Am. J. Gastroenterol. 2001, 96, 126–131. [Google Scholar] [CrossRef] [PubMed]
- Koskinen, O.; Collin, P.; Korponay-Szabo, I.; Salmi, T.; Iltanen, S.; Haimila, K.; Partanen, J.; Mäki, M.; Kaukinen, K. Gluten-dependent small bowel mucosal transglutaminase 2-specific IgA deposits in overt and mild enteropathy coeliac disease. J. Pediatr. Gastroenterol. Nutr. 2008, 47, 436–442. [Google Scholar] [CrossRef] [PubMed]
- Salmi, T.T.; Hervonen, K.; Laurila, K.; Collin, P.; Mäki, M.; Koskinen, O.; Huhtala, H.; Kaukinen, K.; Reunala, T. Small bowel transglutaminase 2-specific IgA deposits in dermatitis herpetiformis. Acta Derm. Venereol. 2014, 94, 393–397. [Google Scholar] [CrossRef] [PubMed]
- Virta, L.; Kaukinen, K.; Collin, P. Incidence and prevalence of diagnosed coeliac disease in Finland: Results of effective case finding in adults. Scand. J. Gastroenterol. 2009, 44, 933–938. [Google Scholar] [CrossRef] [PubMed]
- Hervonen, K.; Alakoski, A.; Salmi, T.T.; Helakorpi, S.; Kautiainen, H.; Kaukinen, K.; Pukkala, E.; Collin, P.; Reunala, T. Reduced mortality in dermatitis herpetiformis: A population-based study of 476 patients. Br. J. Dermatol. 2012, 167, 1331–1337. [Google Scholar] [CrossRef] [PubMed]
- Lewis, N.R.; Logan, R.F.; Hubbard, R.B.; West, J. No increase in risk of fracture, malignancy or mortality in dermatitis herpetiformis: A cohort study. Aliment. Pharmacol. Ther. 2008, 27, 1140–1147. [Google Scholar] [CrossRef] [PubMed]
- Tio, M.; Cox, M.R.; Eslick, G.D. Meta-analysis: Coeliac disease and the risk of all-cause mortality, any malignancy and lymphoid malignancy. Aliment. Pharmacol. Ther. 2012, 35, 540–551. [Google Scholar] [CrossRef] [PubMed]
- Leffler, D.A.; Green, P.H.; Fasano, A. Extraintestinal manifestations of coeliac disease. Nat. Rev. Gastroenterol. Hepatol. 2015, 12, 561–571. [Google Scholar] [CrossRef] [PubMed]
- Virta, L.J.; Saarinen, M.M.; Kolho, K.L. Declining trend in the incidence of biopsy-verified coeliac disease in the adult population of Finland, 2005–2014. Aliment. Pharmacol. Ther. 2017, 46, 1085–1093. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.Y.; Kang, A.H.; Green, A.; Gwee, K.A.; Ho, K.Y. Systematic review: Worldwide variation in the frequency of coeliac disease and changes over time. Aliment. Pharmacol. Ther. 2013, 38, 226–245. [Google Scholar] [CrossRef] [PubMed]
- Lohi, S.; Mustalahti, K.; Kaukinen, K.; Laurila, K.; Collin, P.; Rissanen, H.; Lohi, O.; Bravi, E.; Gasparin, M.; Reunanen, A.; et al. Increasing prevalence of coeliac disease over time. Aliment. Pharmacol. Ther. 2007, 26, 1217–1225. [Google Scholar] [CrossRef] [PubMed]
- Salmi, T.T.; Hervonen, K.; Kurppa, K.; Collin, P.; Kaukinen, K.; Reunala, T. Coeliac disease evolving into dermatitis herpetiformis in patients adhering to normal or gluten-free diet. Scand. J. Gastroenterol. 2015, 50, 387–392. [Google Scholar] [CrossRef] [PubMed]
- Aine, L.; Mäki, M.; Reunala, T. Coeliac-type dental enamel defects in patients with dermatitis herpetiformis. Acta Derm. Venereol. 1992, 72, 25–27. [Google Scholar] [PubMed]
- Sárdy, M.; Kárpáti, S.; Merkl, B.; Paulsson, M.; Smyth, N. Epidermal transglutaminase (TGase 3) is the autoantigen of dermatitis herpetiformis. J. Exp. Med. 2002, 195, 747–757. [Google Scholar] [CrossRef] [PubMed]
- Dieterich, W.; Ehnis, T.; Bauer, M.; Donner, P.; Volta, U.; Riecken, E.O.; Schuppan, D. Identification of tissue transglutaminase as the autoantigen of celiac disease. Nat. Med. 1997, 3, 797–801. [Google Scholar] [CrossRef] [PubMed]
- Korponay-Szabó, I.R.; Halttunen, T.; Szalai, Z.; Laurila, K.; Király, R.; Kovács, J.B.; Király, R.; Kovács, J.B.; Fésüs, L.; Mäki, M. In vivo targeting of intestinal and extraintestinal transglutaminase 2 by coeliac autoantibodies. Gut 2004, 53, 641–648. [Google Scholar] [CrossRef] [PubMed]
- Kárpáti, S.; Sárdy, M.; Németh, K.; Mayer, B.; Smyth, N.; Paulsson, M.; Traupe, H. Transglutaminases in autoimmune and inherited skin diseases: The phenomena of epitope spreading and functional compensation. Exp. Dermatol. 2018, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Hietikko, M.; Hervonen, K.; Ilus, T.; Salmi, T.; Huhtala, H.; Laurila, K.; Rauhavirta, T.; Reunala, T.; Kaukinen, K.; Lindfors, K. Ex vivo culture of duodenal biopsies from patients with Dermatitis herpetiformis indicates that transglutaminase 3 antibody production occurs in the gut. Acta Derm. Venereol. 2018, 98, 366–372. [Google Scholar] [CrossRef] [PubMed]
- Reunala, T.; Salmi, T.T.; Hervonen, K.; Laurila, K.; Kautiainen, H.; Collin, P.; Kaukinen, K. IgA anti-epidermal transglutaminase antibodies in dermatitis herpetiformis: A significant but not complete response to a gluten-free diet treatment. Br. J. Dermatol. 2015, 172, 1139–1141. [Google Scholar] [CrossRef] [PubMed]
- Hietikko, M.; Hervonen, K.; Salmi, T.; Ilus, T.; Zone, J.J.; Kaukinen, K.; Reunala, T.; Lindfors, K. Disappearance of epidermal transglutaminase and IgA deposits from the papillary dermis of dermatitis herpetiformis patients after a long-term gluten-free diet. Br. J. Dermatol. 2018, 178, e198–e201. [Google Scholar] [CrossRef] [PubMed]
- Taylor, T.B.; Schmidt, L.A.; Meyer, L.J.; Zone, J.J. Transglutaminase 3 present in the IgA aggregates in dermatitis herpetiformis skin is enzymatically active and binds soluble fibrinogen. J. Investig. Dermatol. 2015, 135, 623–625. [Google Scholar] [CrossRef] [PubMed]
- Grainge, M.J.; West, J.; Solaymani-Dodaran, M.; Card, T.R.; Logan, R.F. The long-term risk of malignancy following a diagnosis of coeliac disease or dermatitis herpetiformis: A cohort study. Aliment. Pharmacol. Ther. 2012, 35, 730–739. [Google Scholar] [CrossRef] [PubMed]
- Lewis, H.M.; Reunala, T.L.; Garioch, J.J.; Leonard, J.N.; Fry, J.S.; Collin, P.; Evans, D.; Fry, L. Protective effect of gluten-free diet against development of lymphoma in dermatitis herpetiformis. Br. J. Dermatol. 1996, 135, 363–367. [Google Scholar] [CrossRef] [PubMed]
- Abdul Sultan, A.; Crooks, C.J.; Card, T.; Tata, L.J.; Fleming, K.M.; West, J. Causes of death in people with coeliac disease in England compared with the general population: A competing risk analysis. Gut 2015, 64, 1220–1226. [Google Scholar] [CrossRef] [PubMed]
- Corrao, G.; Corazza, G.R.; Bagnardi, V.; Brusco, G.; Ciacci, C.; Cottone, M.; Sategna Guidetti, C.; Usai, P.; Cesari, P.; Pelli, M.A.; et al. Mortality in patients with coeliac disease and their relatives: A cohort study. Lancet 2001, 358, 356–361. [Google Scholar] [CrossRef]
- Paarlahti, P.; Kurppa, K.; Ukkola, A.; Collin, P.; Huhtala, H.; Mäki, M.; Kaukinen, K. Predictors of persistent symptoms and reduced quality of life in treated coeliac disease patients: A large cross-sectional study. BMC Gastroenterol. 2013, 13, 75. [Google Scholar] [CrossRef] [PubMed]
- Burger, J.P.W.; de Brouwer, B.; IntHout, J.; Wahab, P.J.; Tummers, M.; Drenth, J.P.H. Systematic review with meta-analysis: Dietary adherence influences normalization of health-related quality of life in coeliac disease. Clin. Nutr. 2017, 36, 399–406. [Google Scholar] [CrossRef] [PubMed]
- Pasternack, C.; Kaukinen, K.; Kurppa, K.; Mäki, M.; Collin, P.; Reunala, T.; Huhtala, H.; Salmi, T. Quality of life and gastrointestinal symptoms in long-term treated Dermatitis herpetiformis patients: A cross-sectional study in Finland. Am. J. Clin. Dermatol. 2015, 16, 545–552. [Google Scholar] [CrossRef] [PubMed]
| Dermatitis Herpetiformis | Coeliac Disease | |
|---|---|---|
| Gender | Slightly more males | Females predominate |
| Age at onset | Mainly adults | Children and adults |
| IgA-TG3 deposits in the skin | 100% | 0% |
| Small bowel villous atrophy | 75% | 100% * |
| IgA-TG2 deposits in the small bowel mucosa [36,37] | 80% | up to 100% ** |
| Prevalence in Finland and United Kingdom [18,19,38] | 75 and 30 per 100,000 | 660 and 240 per 100,000 |
| Incidence | Decreasing | Increasing |
| Response to a gluten-free diet [7,8,20] | Slow; months, in the beginning most patients need dapsone to control the rash | Rapid; days or weeks until gastro-intestinal symptoms end whereas small bowel villous atrophy may persist for many years |
| Long-term prognosis on a gluten-free diet [39,40,41] | Excellent | All-cause and lymphoma mortality may be increased |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reunala, T.; Salmi, T.T.; Hervonen, K.; Kaukinen, K.; Collin, P. Dermatitis Herpetiformis: A Common Extraintestinal Manifestation of Coeliac Disease. Nutrients 2018, 10, 602. https://doi.org/10.3390/nu10050602
Reunala T, Salmi TT, Hervonen K, Kaukinen K, Collin P. Dermatitis Herpetiformis: A Common Extraintestinal Manifestation of Coeliac Disease. Nutrients. 2018; 10(5):602. https://doi.org/10.3390/nu10050602
Chicago/Turabian StyleReunala, Timo, Teea T. Salmi, Kaisa Hervonen, Katri Kaukinen, and Pekka Collin. 2018. "Dermatitis Herpetiformis: A Common Extraintestinal Manifestation of Coeliac Disease" Nutrients 10, no. 5: 602. https://doi.org/10.3390/nu10050602
APA StyleReunala, T., Salmi, T. T., Hervonen, K., Kaukinen, K., & Collin, P. (2018). Dermatitis Herpetiformis: A Common Extraintestinal Manifestation of Coeliac Disease. Nutrients, 10(5), 602. https://doi.org/10.3390/nu10050602




