Dietary Acid Load and Mental Health Outcomes in Children and Adolescents: Results from the GINIplus and LISA Birth Cohort Studies
Abstract
1. Introduction
2. Materials and Methods
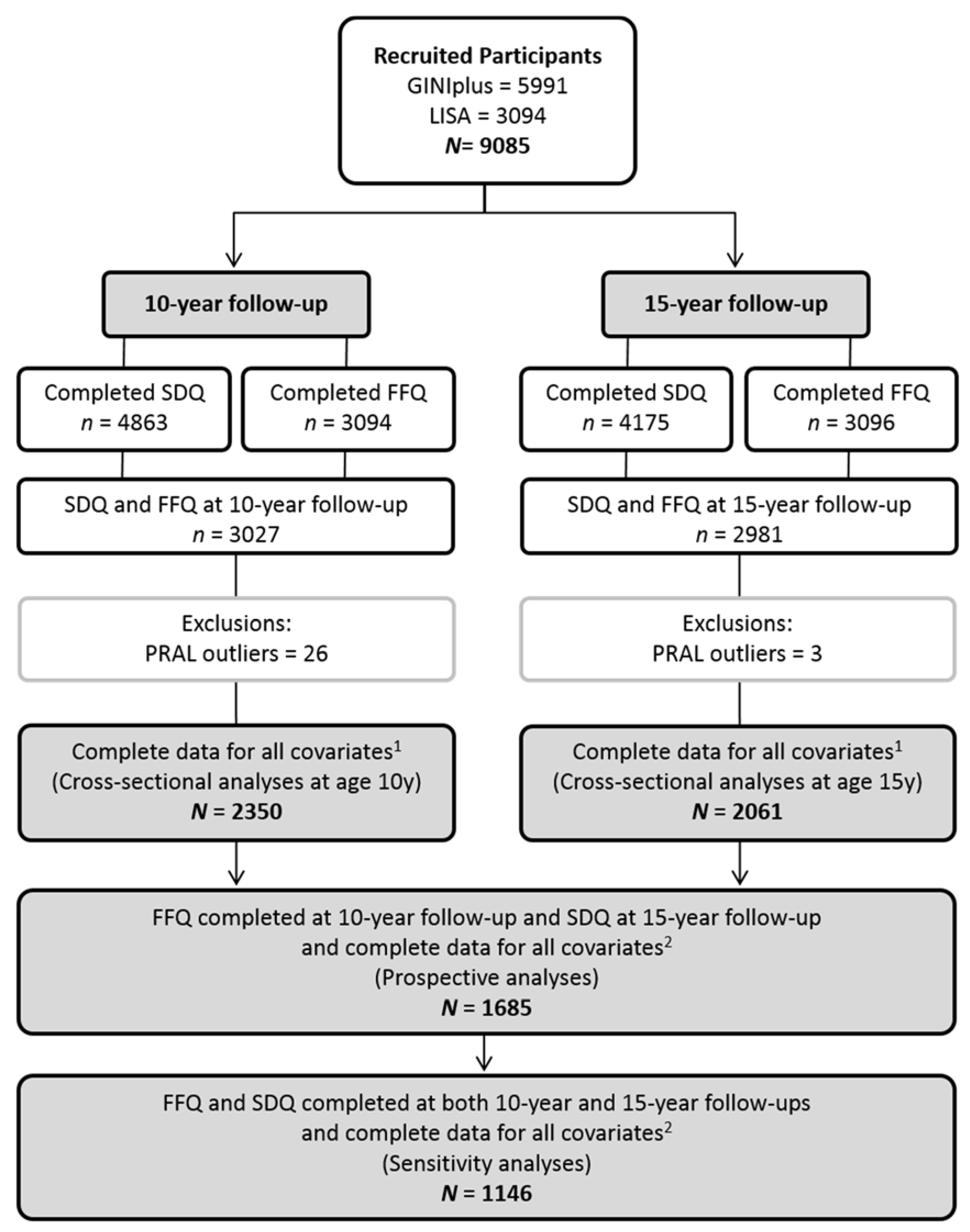
2.1. Study Population
2.2. Dietary Assessment and Estimation of Diet-Induced Acid Load
2.3. Measurement of Mental Health Outcomes
2.4. Covariates
2.5. Statistical Analysis
3. Results
3.1. Study Population
3.2. Association between PRAL and SDQ—Main Analyses
3.3. Sensitivity Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Kessler, R.C.; Aguilar-Gaxiola, S.; Alonso, J.; Chatterji, S.; Lee, S.; Ormel, J.; Ustun, T.B.; Wang, P.S. The global burden of mental disorders: An update from the WHO world mental health (WMH) surveys. Epidemiol. Psichiatr. Soc. 2009, 18, 23–33. [Google Scholar] [CrossRef] [PubMed]
- Ravens-Sieberer, U.; Wille, N.; Erhart, M.; Bettge, S.; Wittchen, H.U.; Rothenberger, A.; Herpertz-Dahlmann, B.; Resch, F.; Holling, H.; Bullinger, M.; et al. Prevalence of mental health problems among children and adolescents in Germany: Results of the BELLA study within the National Health Interview and Examination Survey. Eur. Child Adolesc. Psychiatry 2008, 17 (Suppl. 1), 22–33. [Google Scholar] [CrossRef] [PubMed]
- Sarris, J.; Murphy, J.; Mischoulon, D.; Papakostas, G.I.; Fava, M.; Berk, M.; Ng, C.H. Adjunctive nutraceuticals for depression: A systematic review and meta-analyses. Am. J. Psychiatry 2016, 173, 575–587. [Google Scholar] [CrossRef] [PubMed]
- Lange, K.W.; Hauser, J.; Lange, K.M.; Makulska-Gertruda, E.; Nakamura, Y.; Reissmann, A.; Sakaue, Y.; Takano, T.; Takeuchi, Y. The role of nutritional supplements in the treatment of ADHD: What the evidence says. Curr. Psychiatry Rep. 2017, 19, 8. [Google Scholar] [CrossRef] [PubMed]
- Molendijk, M.; Molero, P.; Sanchez-Pedreno, F.O.; Van der Does, W.; Martinez-Gonzalez, M.A. Diet quality and depression risk: A systematic review and dose-response meta-analysis of prospective studies. J. Affect. Disord. 2018, 226, 346–354. [Google Scholar] [CrossRef] [PubMed]
- Schmitz, G.; Ecker, J. The opposing effects of n-3 and n-6 fatty acids. Prog. Lipid Res. 2008, 47, 147–155. [Google Scholar] [CrossRef] [PubMed]
- O’Neil, A.; Quirk, S.E.; Housden, S.; Brennan, S.L.; Williams, L.J.; Pasco, J.A.; Berk, M.; Jacka, F.N. Relationship between diet and mental health in children and adolescents: A systematic review. Am. J. Public Health 2014, 104, e31–e42. [Google Scholar] [CrossRef] [PubMed]
- Deriemaeker, P.; Aerenhouts, D.; Hebbelinck, M.; Clarys, P. Nutrient based estimation of acid-base balance in vegetarians and non-vegetarians. Plant Foods Hum. Nutr. 2010, 65, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Ausman, L.M.; Oliver, L.M.; Goldin, B.R.; Woods, M.N.; Gorbach, S.L.; Dwyer, J.T. Estimated net acid excretion inversely correlates with urine pH in vegans, lacto-ovo vegetarians, and omnivores. J. Ren. Nutr. 2008, 18, 456–465. [Google Scholar] [CrossRef] [PubMed]
- Ball, D.; Maughan, R.J. Blood and urine acid-base status of premenopausal omnivorous and vegetarian women. Br. J. Nutr. 1997, 78, 683–693. [Google Scholar] [CrossRef] [PubMed]
- Remer, T.; Manz, F. Potential renal acid load of foods and its influence on urine pH. J. Am. Diet. Assoc. 1995, 95, 791–797. [Google Scholar] [CrossRef]
- Remer, T. Influence of nutrition on acid-base balance—Metabolic aspects. Eur. J. Nutr. 2001, 40, 214–220. [Google Scholar] [CrossRef] [PubMed]
- Bullo, M.; Amigo-Correig, P.; Marquez-Sandoval, F.; Babio, N.; Martinez-Gonzalez, M.A.; Estruch, R.; Basora, J.; Sola, R.; Salas-Salvado, J. Mediterranean diet and high dietary acid load associated with mixed nuts: Effect on bone metabolism in elderly subjects. J. Am. Geriatr. Soc. 2009, 57, 1789–1798. [Google Scholar] [CrossRef] [PubMed]
- Alexy, U.; Remer, T.; Manz, F.; Neu, C.M.; Schoenau, E. Long-term protein intake and dietary potential renal acid load are associated with bone modeling and remodeling at the proximal radius in healthy children. Am. J. Clin. Nutr. 2005, 82, 1107–1114. [Google Scholar] [CrossRef] [PubMed]
- Han, E.; Kim, G.; Hong, N.; Lee, Y.H.; Kim, D.W.; Shin, H.J.; Lee, B.W.; Kang, E.S.; Lee, I.K.; Cha, B.S. Association between dietary acid load and the risk of cardiovascular disease: Nationwide surveys (KNHANES 2008–2011). Cardiovasc. Diabetol. 2016, 15, 122. [Google Scholar] [CrossRef] [PubMed]
- Esche, J.; Shi, L.; Sanchez-Guijo, A.; Hartmann, M.F.; Wudy, S.A.; Remer, T. Higher diet-dependent renal acid load associates with higher glucocorticoid secretion and potentially bioactive free glucocorticoids in healthy children. Kidney Int. 2016, 90, 325–333. [Google Scholar] [CrossRef] [PubMed]
- Buehlmeier, J.; Remer, T.; Frings-Meuthen, P.; Maser-Gluth, C.; Heer, M. Glucocorticoid activity and metabolism with NaCl-induced low-grade metabolic acidosis and oral alkalization: Results of two randomized controlled trials. Endocrine 2016, 52, 139–147. [Google Scholar] [CrossRef] [PubMed]
- Weiner, I.D. Untangling the complex relationship between dietary acid load and glucocorticoid metabolism. Kidney Int. 2016, 90, 247–249. [Google Scholar] [CrossRef] [PubMed]
- Hamm, L.L.; Ambuhl, P.M.; Alpern, R.J. Role of glucocorticoids in acidosis. Am. J. Kidney Dis. 1999, 34, 960–965. [Google Scholar] [CrossRef]
- Buehlmeier, J.; Frings-Meuthen, P.; Remer, T.; Maser-Gluth, C.; Stehle, P.; Biolo, G.; Heer, M. Alkaline salts to counteract bone resorption and protein wasting induced by high salt intake: Results of a randomized controlled trial. J. Clin. Endocrinol. Metab. 2012, 97, 4789–4797. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Shi, L.; Sanchez-Guijo, A.; Hartmann, M.F.; Schonau, E.; Esche, J.; Wudy, S.A.; Remer, T. Higher glucocorticoid secretion in the physiological range is associated with lower bone strength at the proximal radius in healthy children: Importance of protein intake adjustment. J. Bone Miner. Res. 2015, 30, 240–248. [Google Scholar] [CrossRef] [PubMed]
- Prodam, F.; Ricotti, R.; Agarla, V.; Parlamento, S.; Genoni, G.; Balossini, C.; Walker, G.E.; Aimaretti, G.; Bona, G.; Bellone, S. High-end normal adrenocorticotropic hormone and cortisol levels are associated with specific cardiovascular risk factors in pediatric obesity: A cross-sectional study. BMC Med. 2013, 11, 44. [Google Scholar] [CrossRef] [PubMed]
- Mora, F.; Segovia, G.; Del Arco, A.; de Blas, M.; Garrido, P. Stress, neurotransmitters, corticosterone and body-brain integration. Brain Res. 2012, 1476, 71–85. [Google Scholar] [CrossRef] [PubMed]
- Dedovic, K.; Duchesne, A.; Andrews, J.; Engert, V.; Pruessner, J.C. The brain and the stress axis: The neural correlates of cortisol regulation in response to stress. Neuroimage 2009, 47, 864–871. [Google Scholar] [CrossRef] [PubMed]
- Crespo, I.; Santos, A.; Gomez-Anson, B.; Lopez-Mourelo, O.; Pires, P.; Vives-Gilabert, Y.; Webb, S.M.; Resmini, E. Brain metabolite abnormalities in ventromedial prefrontal cortex are related to duration of hypercortisolism and anxiety in patients with cushing’s syndrome. Endocrine 2016, 53, 848–856. [Google Scholar] [CrossRef] [PubMed]
- Berg, A.; Kramer, U.; Link, E.; Bollrath, C.; Heinrich, J.; Brockow, I.; Koletzko, S.; Grubl, A.; Filipiak-Pittroff, B.; Wichmann, H.E.; et al. Impact of early feeding on childhood eczema: Development after nutritional intervention compared with the natural course—The giniplus study up to the age of 6 years. Clin. Exp. Allergy 2010, 40, 627–636. [Google Scholar] [CrossRef] [PubMed]
- Heinrich, J.; Bolte, G.; Holscher, B.; Douwes, J.; Lehmann, I.; Fahlbusch, B.; Bischof, W.; Weiss, M.; Borte, M.; Wichmann, H.E.; et al. Allergens and endotoxin on mothers’ mattresses and total immunoglobulin e in cord blood of neonates. Eur. Respir. J. 2002, 20, 617–623. [Google Scholar] [CrossRef] [PubMed]
- Stiegler, P.; Sausenthaler, S.; Buyken, A.E.; Rzehak, P.; Czech, D.; Linseisen, J.; Kroke, A.; Gedrich, K.; Robertson, C.; Heinrich, J. A new FFQ designed to measure the intake of fatty acids and antioxidants in children. Public Health Nutr. 2010, 13, 38–46. [Google Scholar] [CrossRef] [PubMed]
- Sausenthaler, S.; Standl, M.; Buyken, A.; Rzehak, P.; Koletzko, S.; Bauer, C.P.; Schaaf, B.; von Berg, A.; Berdel, D.; Borte, M.; et al. Regional and socio-economic differences in food, nutrient and supplement intake in school-age children in germany: Results from the giniplus and the lisaplus studies. Public Health Nutr. 2011, 14, 1724–1735. [Google Scholar] [CrossRef] [PubMed]
- Harris, C.; Flexeder, C.; Thiering, E.; Buyken, A.; Berdel, D.; Koletzko, S.; Bauer, C.P.; Bruske, I.; Koletzko, B.; Standl, M.; et al. Changes in dietary intake during puberty and their determinants: Results from the giniplus birth cohort study. BMC Public Health 2015, 15, 841. [Google Scholar] [CrossRef] [PubMed]
- Bohlscheid-Thomas, S.; Hoting, I.; Boeing, H.; Wahrendorf, J. Reproducibility and relative validity of food group intake in a food frequency questionnaire developed for the German part of the epic project. European prospective investigation into cancer and nutrition. Int. J. Epidemiol. 1997, 26 (Suppl. 1), S59–S70. [Google Scholar] [CrossRef] [PubMed]
- Willett, W. Nutritional Epidemiology; Oxford University Press: New York, USA, 1998. [Google Scholar]
- Remer, T.; Dimitriou, T.; Manz, F. Dietary potential renal acid load and renal net acid excretion in healthy, free-living children and adolescents. Am. J. Clin. Nutr. 2003, 77, 1255–1260. [Google Scholar] [CrossRef] [PubMed]
- Goodman, R. The strengths and difficulties questionnaire: A research note. J. Child Psychol. Psychiatry 1997, 38, 581–586. [Google Scholar] [CrossRef] [PubMed]
- Woerner, W.; Becker, A.; Friedrich, C.; Klasen, H.; Goodman, R.; Rothenberger, A. Normal values and evaluation of the german parents’ version of strengths and difficulties questionnaire (SDQ): Results of a representative field study. Z. Kinder Jugendpsychiatr. Psychother. 2002, 30, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Woerner, W.; Becker, A.; Rothenberger, A. Normative data and scale properties of the German parent SDQ. Eur. Child Adolesc. Psychiatry 2004, 13 (Suppl. 2), II3–II10. [Google Scholar] [CrossRef] [PubMed]
- Lindeboom, M.; van Doorslaer, E. Cut-point shift and index shift in self-reported health. J. Health Econ. 2004, 23, 1083–1099. [Google Scholar] [CrossRef] [PubMed]
- Derogatis, L. BSI 18 Brief Symptom Inventory 18: Administration, Scoring, and Procedures Manual; NCS Pearson, Inc.: Minneapolis, MN, USA, 2000. [Google Scholar]
- Libuda, L.; Antel, J.; Hebebrand, J.; Focker, M. Nutrition and mental diseases: Focus depressive disorders. Nervenarzt 2017, 88, 87–101. [Google Scholar] [CrossRef] [PubMed]
- Lohbeck, A.; Schultheiss, J.; Petermann, F.; Petermann, U. The German self-report version of the strengths and difficulties questionnaire (SDQ-Deu-S): Psychometric properties, factor structure, and critical values. Diagnostica 2015, 61, 222–235. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2016. [Google Scholar]
- Davson, H.; Segal, M.B. The effects of some inhibitors and accelerators of sodium transport on the turnover of 22 Na in the cerebrospinal fluid and the brain. J. Physiol. 1970, 209, 131–153. [Google Scholar] [CrossRef] [PubMed]
- Ang, R.C.; Hoop, B.; Kazemi, H. Brain glutamate metabolism during metabolic alkalosis and acidosis. J. Appl. Physiol. 1992, 73, 2552–2558. [Google Scholar] [CrossRef] [PubMed]
- Jhee, J.H.; Lee, E.; Cha, M.U.; Lee, M.; Kim, H.; Park, S.; Yun, H.R.; Jung, S.Y.; Kee, Y.K.; Yoon, C.Y.; et al. Prevalence of depression and suicidal ideation increases proportionally with renal function decline, beginning from early stages of chronic kidney disease. Medicine 2017, 96, e8476. [Google Scholar] [CrossRef] [PubMed]
- Afsar, B.; Elsurer, R. Association between serum bicarbonate and pH with depression, cognition and sleep quality in hemodialysis patients. Ren. Fail. 2015, 37, 957–960. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Maurer, M.; Riesen, W.; Muser, J.; Hulter, H.N.; Krapf, R. Neutralization of western diet inhibits bone resorption independently of K intake and reduces cortisol secretion in humans. Am. J. Physiol. Ren. Physiol. 2003, 284, F32–F40. [Google Scholar] [CrossRef] [PubMed]
- Alexy, U.; Kersting, M.; Remer, T. Potential renal acid load in the diet of children and adolescents: Impact of food groups, age and time trends. Public Health Nutr. 2008, 11, 300–306. [Google Scholar] [CrossRef] [PubMed]
- Oddy, W.H.; Robinson, M.; Ambrosini, G.L.; O’Sullivan, T.A.; de Klerk, N.H.; Beilin, L.J.; Silburn, S.R.; Zubrick, S.R.; Stanley, F.J. The association between dietary patterns and mental health in early adolescence. Prev. Med. 2009, 49, 39–44. [Google Scholar] [CrossRef] [PubMed]
- McMartin, S.E.; Jacka, F.N.; Colman, I. The association between fruit and vegetable consumption and mental health disorders: Evidence from five waves of a national survey of Canadians. Prev. Med. 2013, 56, 225–230. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.F.; Gorski, M.T.; Gruber, S.A.; Kurdziel, L.B.; Rimm, E.B. The effect of healthy dietary consumption on executive cognitive functioning in children and adolescents: A systematic review. Br. J. Nutr. 2016, 116, 989–1000. [Google Scholar] [CrossRef] [PubMed]
- Hooper, L.; Kroon, P.A.; Rimm, E.B.; Cohn, J.S.; Harvey, I.; Le Cornu, K.A.; Ryder, J.J.; Hall, W.L.; Cassidy, A. Flavonoids, flavonoid-rich foods, and cardiovascular risk: A meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 2008, 88, 38–50. [Google Scholar] [CrossRef] [PubMed]
- Shrime, M.G.; Bauer, S.R.; McDonald, A.C.; Chowdhury, N.H.; Coltart, C.E.; Ding, E.L. Flavonoid-rich cocoa consumption affects multiple cardiovascular risk factors in a meta-analysis of short-term studies. J. Nutr. 2011, 141, 1982–1988. [Google Scholar] [CrossRef] [PubMed]
- Bell, L.; Lamport, D.J.; Butler, L.T.; Williams, C.M. A review of the cognitive effects observed in humans following acute supplementation with flavonoids, and their associated mechanisms of action. Nutrients 2015, 7, 10290–10306. [Google Scholar] [CrossRef] [PubMed]
- Van der Ende, J.; Verhulst, F.C.; Tiemeier, H. Agreement of informants on emotional and behavioral problems from childhood to adulthood. Psychol. Assess. 2012, 24, 293–300. [Google Scholar] [CrossRef] [PubMed]
- Holling, H.; Schlack, R.; Petermann, F.; Ravens-Sieberer, U.; Mauz, E.; Ki, G.G.S.S.G. Psychopathological problems and psychosocial impairment in children and adolescents aged 3–17 years in the German population: Prevalence and time trends at two measurement points (2003–2006 and 2009–2012): Results of the kiggs study: First follow-up (kiggs wave 1). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2014, 57, 807–819. [Google Scholar] [PubMed]
- Leykin, Y.; Roberts, C.S.; DeRubeis, R.J. Decision-making and depressive symptomatology. Cogn. Ther. Res. 2011, 35, 333–341. [Google Scholar] [CrossRef] [PubMed]
| 10-Year Follow-Up | 15-Year Follow-Up | |||||||
|---|---|---|---|---|---|---|---|---|
| Total (N = 2350) | Females (N = 1137) | Males (N = 1213) | p-Value a | Total (N = 2061) | Females (N = 1101) | Males (N = 960) | p-Value a | |
| Total difficulties (borderline) | 149 (6.34) | 54 (4.75) | 95 (7.83) | <0.001 | 99 (4.8) | 60 (5.45) | 39 (4.06) | 0.110 |
| (abnormal) | 174 (7.4) | 63 (5.54) | 111 (9.15) | 20 (0.97) | 14 (1.27) | 6 (0.62) | ||
| Emotional problems (borderline) | 174 (7.4) | 86 (7.56) | 88 (7.25) | 0.910 | 63 (3.06) | 49 (4.45) | 14 (1.46) | <0.001 |
| (abnormal) | 223 (9.49) | 110 (9.67) | 113 (9.32) | 71 (3.44) | 64 (5.81) | 7 (0.73) | ||
| Conduct problems (borderline) | 164 (6.98) | 56 (4.93) | 108 (8.9) | <0.001 | 78 (3.78) | 37 (3.36) | 41 (4.27) | 0.006 |
| (abnormal) | 99 (4.21) | 36 (3.17) | 63 (5.19) | 56 (2.72) | 19 (1.73) | 37 (3.85) | ||
| Hyperactivity (borderline) | 114 (4.85) | 44 (3.87) | 70 (5.77) | <0.001 | 134 (6.5) | 68 (6.18) | 66 (6.88) | 0.024 |
| (abnormal) | 185 (7.87) | 45 (3.96) | 140 (11.54) | 109 (5.29) | 45 (4.09) | 64 (6.67) | ||
| Peer problems (borderline) | 94 (4) | 39 (3.43) | 55 (4.53) | 0.045 | 177 (8.59) | 89 (8.08) | 88 (9.17) | 0.650 |
| (abnormal) | 108 (4.6) | 42 (3.69) | 66 (5.44) | 37 (1.8) | 19 (1.73) | 18 (1.88) | ||
| Prosocial (borderline) | 109 (4.64) | 32 (2.81) | 77 (6.35) | <0.001 | 120 (5.82) | 36 (3.27) | 84 (8.75) | <0.001 |
| (abnormal) | 68 (2.89) | 18 (1.58) | 50 (4.12) | 43 (2.09) | 18 (1.63) | 25 (2.6) | ||
| PRAL (mEg/d) b | 6.63 (−0.36; 14.56) | 4.96 (−1.47; 12.33) | 8.43 (0.88; 16.12) | <0.001 | 9.39 (0.95; 18.72) | 6.39 (−1.35; 13.88) | 13.6 (5; 23.9) | <0.001 |
| BMI (kg/m2) c | 16.6 (15.5; 18.4) | 16.6 (15.5; 18.3) | 16.6 (15.6; 18.4) | 0.406 | 20 (18.6; 21.9) | 20.1 (18.6; 21.8) | 19.9 (18.4; 21.9) | 0.114 |
| Total energy intake (kcal/day) d | 1909 (1578; 2283) | 1768 (1467; 2107) | 2067 (1692; 2447) | <0.001 | 1979 (1538; 2511) | 1712 (1362.; 2148) | 2324 (1870; 2791) | <0.001 |
| Moderate–vigorous PA (low) | 544 (23.15) | 322 (28.32) | 222 (18.3) | <0.001 | 473 (22.95) | 308 (27.97) | 165 (17.19) | <0.001 |
| (medium) | 1262 (53.7) | 607 (53.39) | 655 (54.0) | 1120 (54.34) | 604 (54.86) | 516 (53.75) | ||
| (high) | 544 (23.15) | 208 (18.29) | 336 (27.7) | 468 (22.71) | 189 (17.17) | 279 (29.06) | ||
| Screen time (high) | 258 (10.98) | 101 (8.88) | 157 (12.94) | 0.002 | 1099 (53.32) | 509 (46.23) | 590 (61.46) | <0.001 |
| Puberty signs (yes) | 674 (28.68) | 536 (47.14) | 138 (11.38) | <0.001 | - | - | - | |
| Pubertal stage (pre–mid) | - | - | - | 431 (20.91) | 46 (4.18) | 385 (40.1) | <0.001 | |
| (late) | - | - | - | 1440 (69.87) | 873 (79.29) | 567 (59.06) | ||
| (post) | - | - | - | 190 (9.22) | 182 (16.53) | 8 (0.83) | ||
| Parental education (high) | 1628 (69.28) | 816 (71.77) | 812 (66.94) | 0.013 | 1477 (71.66) | 798 (72.48) | 679 (70.73) | 0.410 |
| Study (arm) (GINI (observation)) | 853 (36.3) | 434 (38.17) | 419 (34.54) | 0.084 | 756 (36.68) | 419 (38.06) | 337 (35.1) | 0.017 |
| (GINI (intervention)) | 628 (26.72) | 307 (27) | 321 (26.46) | 528 (25.62) | 298 (27.07) | 230 (23.96) | ||
| (LISA) | 869 (36.98) | 396 (34.83) | 473 (38.99) | 777 (37.7) | 384 (34.88) | 393 (40.94) | ||
| Region (Munich) | 1211 (51.53) | 586 (51.54) | 625 (51.53) | 0.870 | 1129 (54.78) | 583 (52.95) | 546 (56.88) | 0.061 |
| (Leipzig) | 185 (7.87) | 86 (7.56) | 99 (8.16) | 169 (8.2) | 82 (7.45) | 87 (9.06) | ||
| (Bad Honnef) | 111 (4.72) | 51 (4.49) | 60 (4.95) | 93 (4.51) | 52 (4.72) | 41 (4.27) | ||
| (Wesel) | 843 (35.87) | 414 (36.41) | 429 (35.37) | 670 (32.51) | 384 (34.88) | 286 (29.79) | ||
| Cross-Sectional b (10-Year Follow-Up; N = 2350) | Cross-Sectional b (15-Year Follow-Up; N = 2061) | Prospective c (10- to 15-Year Follow-Up; N = 1685) | ||||
|---|---|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| (A) Borderline/abnormal vs. normal | ||||||
| Total difficulties | 1.12 (0.96; 1.31) | 0.139 | 1.02 (0.81; 1.28) | 0.880 | 0.93 (0.72; 1.20) | 0.566 |
| Emotional problems | 1.33 (1.15; 1.54) | <0.001 | 1.03 (0.81; 1.32) | 0.805 | 1.02 (0.77; 1.34) | 0.900 |
| Conduct problems | 0.98 (0.83; 1.15) | 0.799 | 1.12 (0.91; 1.39) | 0.277 | 0.92 (0.72; 1.18) | 0.529 |
| Hyperactivity | 1.22 (1.04; 1.43) | 0.014 | 1.09 (0.93; 1.28) | 0.288 | 1.12 (0.93; 1.35) | 0.223 |
| Peer problems | 1.13 (0.94; 1.37) | 0.205 | 1.02 (0.85; 1.22) | 0.851 | 1.12 (0.93; 1.35) | 0.224 |
| Prosocial | 1.13 (0.92; 1.38) | 0.257 | 1.02 (0.83; 1.25) | 0.860 | 0.87 (0.68; 1.10) | 0.248 |
| (B) Abnormal vs. normal/borderline | ||||||
| Total difficulties | 1.25 (1.02; 1.53) | 0.031 | 1.12 (0.67; 1.88) | 0.672 | 1.04 (0.50; 2.15) | 0.921 |
| Emotional problems | 1.26 (1.05; 1.52) | 0.013 | 0.83 (0.59; 1.17) | 0.289 | 0.88 (0.62; 1.25) | 0.485 |
| Conduct problems | 1.00 (0.77; 1.28) | 0.969 | 1.07 (0.78; 1.46) | 0.683 | 0.98 (0.66; 1.45) | 0.908 |
| Hyperactivity | 1.32 (1.09; 1.61) | 0.005 | 0.98 (0.78; 1.23) | 0.885 | 1.24 (0.95; 1.61) | 0.111 |
| Peer problems | 1.09 (0.84; 1.40) | 0.523 | 0.88 (0.57; 1.36) | 0.562 | 1.20 (0.79; 1.84) | 0.394 |
| Prosocial | 1.08 (0.77; 1.50) | 0.658 | 0.97 (0.65; 1.43) | 0.870 | 0.88 (0.57; 1.36) | 0.571 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bühlmeier, J.; Harris, C.; Koletzko, S.; Lehmann, I.; Bauer, C.-P.; Schikowski, T.; Von Berg, A.; Berdel, D.; Heinrich, J.; Hebebrand, J.; et al. Dietary Acid Load and Mental Health Outcomes in Children and Adolescents: Results from the GINIplus and LISA Birth Cohort Studies. Nutrients 2018, 10, 582. https://doi.org/10.3390/nu10050582
Bühlmeier J, Harris C, Koletzko S, Lehmann I, Bauer C-P, Schikowski T, Von Berg A, Berdel D, Heinrich J, Hebebrand J, et al. Dietary Acid Load and Mental Health Outcomes in Children and Adolescents: Results from the GINIplus and LISA Birth Cohort Studies. Nutrients. 2018; 10(5):582. https://doi.org/10.3390/nu10050582
Chicago/Turabian StyleBühlmeier, Judith, Carla Harris, Sibylle Koletzko, Irina Lehmann, Carl-Peter Bauer, Tamara Schikowski, Andrea Von Berg, Dietrich Berdel, Joachim Heinrich, Johannes Hebebrand, and et al. 2018. "Dietary Acid Load and Mental Health Outcomes in Children and Adolescents: Results from the GINIplus and LISA Birth Cohort Studies" Nutrients 10, no. 5: 582. https://doi.org/10.3390/nu10050582
APA StyleBühlmeier, J., Harris, C., Koletzko, S., Lehmann, I., Bauer, C.-P., Schikowski, T., Von Berg, A., Berdel, D., Heinrich, J., Hebebrand, J., Föcker, M., Standl, M., & Libuda, L. (2018). Dietary Acid Load and Mental Health Outcomes in Children and Adolescents: Results from the GINIplus and LISA Birth Cohort Studies. Nutrients, 10(5), 582. https://doi.org/10.3390/nu10050582






