Evidence for Dietary Fibre Modification in the Recovery and Prevention of Reoccurrence of Acute, Uncomplicated Diverticulitis: A Systematic Literature Review
Abstract
1. Introduction
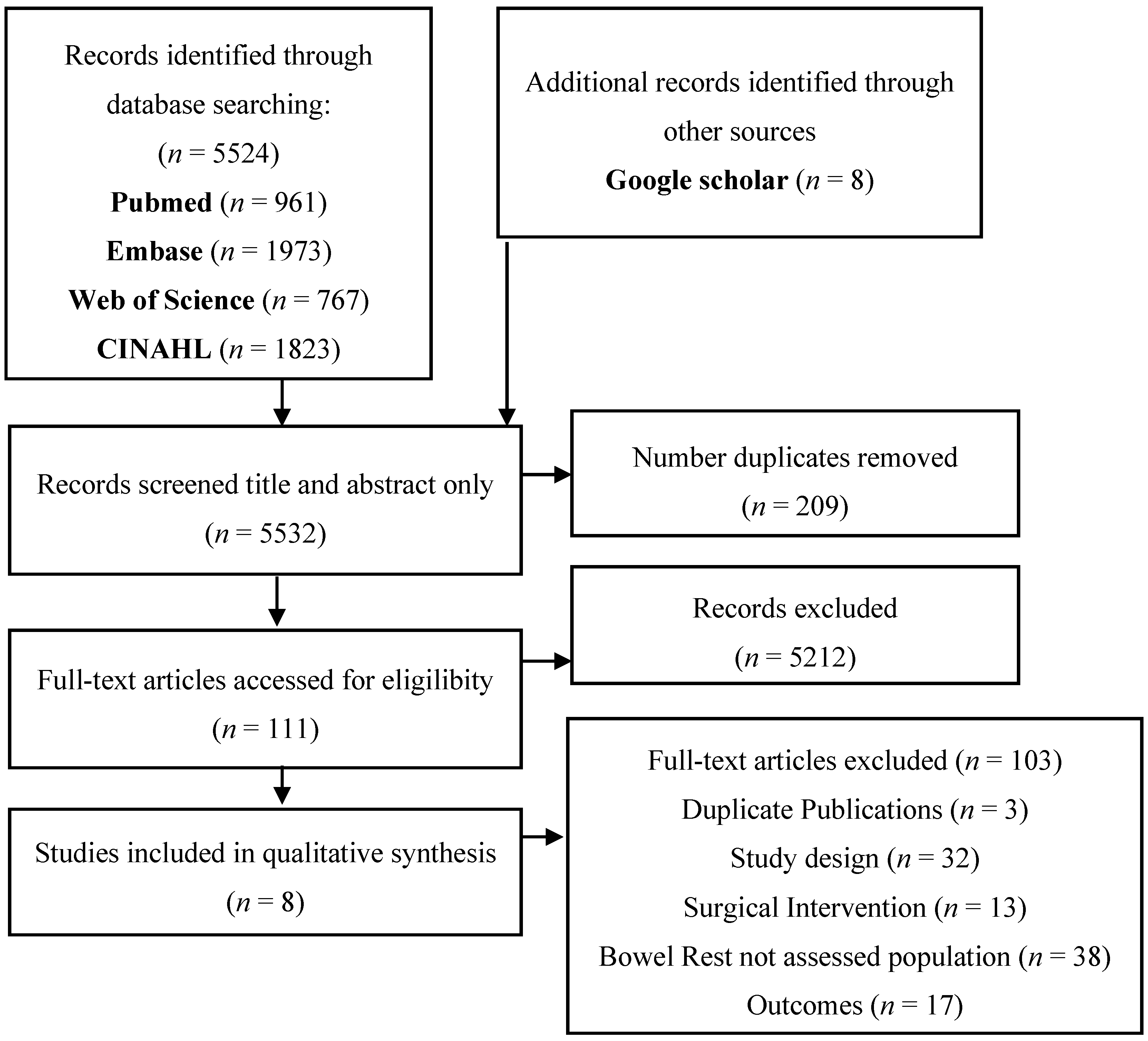
2. Materials and Methods
2.1. Study Search and Selection
2.2. Outcome Measures
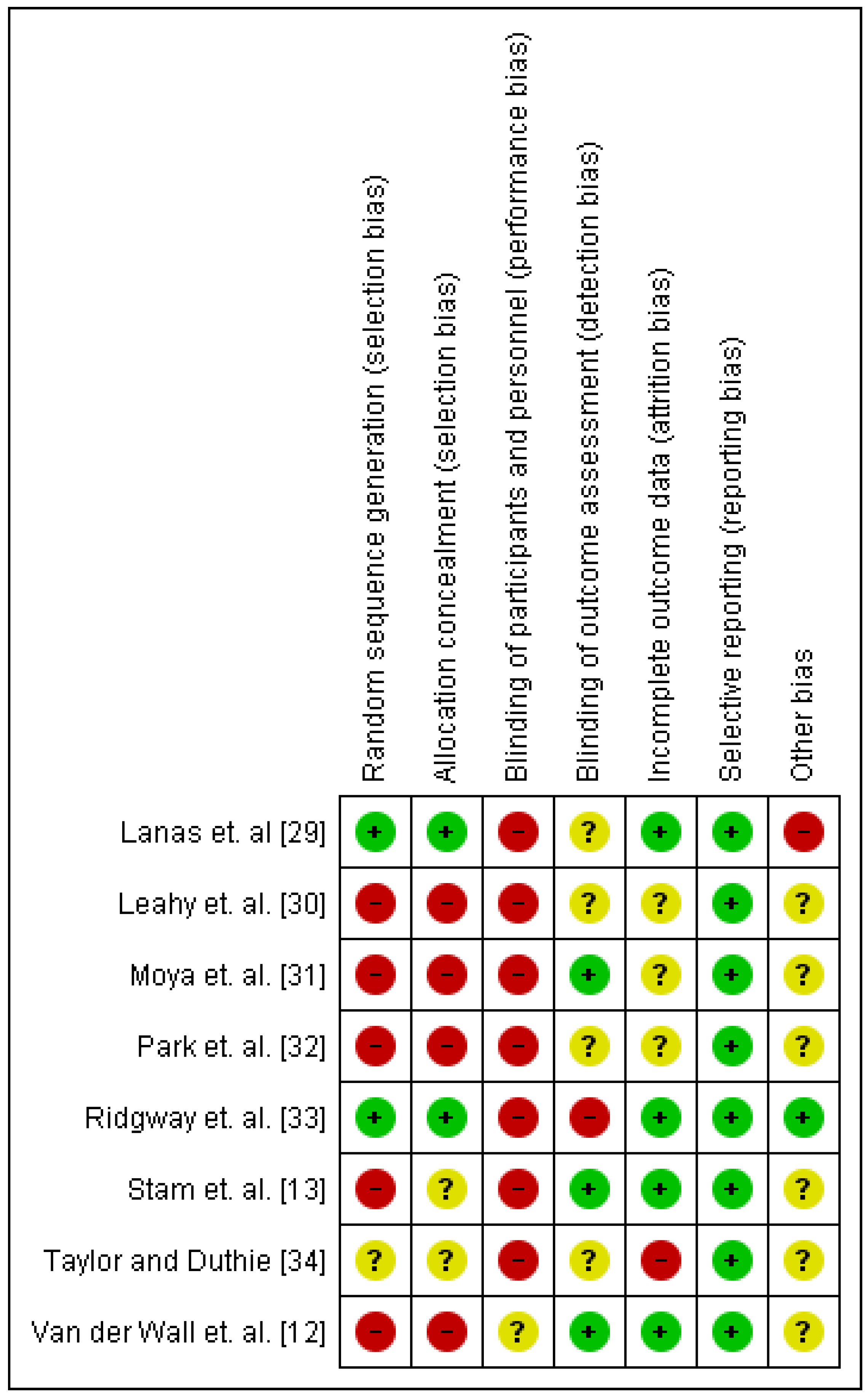
2.3. Study Strength and Quality of the Evidence
2.4. Meta-Analysis
3. Results
3.1. Liberalised versus Restricted Diets, with or without Antibiotics, for the Management of Acute, Uncomplicated Diverticulitis in the Inpatient and Outpatient Setting
3.2. Dietary Fibre Modifications with or without Probiotic Supplementation, for the Management of Uncomplicated Diverticulitis after the Acute Episode Has Resolved
4. Discussion
4.1. Summary of Judgements and Recommendations for Liberalised versus Restricted Diets for the Inpatient Dietary Management of Acute, Uncomplicated Diverticulitis
4.1.1. Recommendation for the Population
4.1.2. Strength of the Recommendation
4.1.3. Overall Justification
4.1.4. Detailed Justification:
4.2. Summary of Judgements and Recommendations for a High Dietary Fibre Diet versus Low Dietary Fibre or Standard Diets for the Dietary Management of Uncomplicated Diverticulitis after the Acute Episode Has Resolved
4.2.1. Recommendation for the Population
4.2.2. Strength of the Recommendation
4.2.3. Overall Justification
4.2.4. Detailed Justification
4.3. Research Priorities
4.4. Limitations
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Peery, A.F.; Barrett, P.R.; Park, D.; Rogers, A.J.; Galanko, J.A.; Martin, C.F.; Sandler, R.S. A high-fiber diet does not protect against asymptomatic diverticulosis. Gastroenterology 2012, 142, 266.e1–272.e1. [Google Scholar] [CrossRef] [PubMed]
- Strate, L.L. Diverticulosis and dietary fiber: Rethinking the relationship. Gastroenterology 2012, 142, 205–207. [Google Scholar] [CrossRef] [PubMed]
- Böhm, S.K. Risk Factors for Diverticulosis, Diverticulitis, Diverticular Perforation, and Bleeding: A Plea for More Subtle History Taking. Visc. Med. 2015, 31, 84–94. [Google Scholar] [CrossRef] [PubMed]
- Vather, R.; Broad, J.B.; Jaung, R.; Robertson, J.; Bissett, I.P. Demographics and trends in the acute presentation of diverticular disease: A national study. ANZ J. Surg. 2015, 85, 744–748. [Google Scholar] [CrossRef] [PubMed]
- Aune, D.; Sen, A.; Leitzmann, M.F.; Norat, T.; Tonstad, S.; Vatten, L.J. Body mass index and physical activity and the risk of diverticular disease: A systematic review and meta-analysis of prospective studies. Eur. J. Nutr. 2017, 56, 2423–2438. [Google Scholar] [CrossRef] [PubMed]
- Peery, A.F.; Dellon, E.S.; Lund, J.; Crockett, S.D.; McGowan, C.E.; Bulsiewicz, W.J.; Gangarosa, L.M.; Thiny, M.T.; Stizenberg, K.; Morgan, D.R.; et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology 2012, 143, 1179.e3–1187.e3. [Google Scholar] [CrossRef] [PubMed]
- Sandler, R.S.; Everhart, J.E.; Donowitz, M.; Adams, E.; Cronin, K.; Goodman, C.; Gemmen, E.; Shah, S.; Avdic, A.; Rubin, R. The burden of selected digestive diseases in the United States. Gastroenterology 2002, 122, 1500–1511. [Google Scholar] [CrossRef] [PubMed]
- Everhart, J.E.; Ruhl, C.E. Burden of digestive diseases in the United States part I: Overall and upper gastrointestinal diseases. Gastroenterology 2009, 136, 376–386. [Google Scholar] [CrossRef] [PubMed]
- Kozak, L.J.; DeFrances, C.J.; Hall, M.J. National hospital discharge survey: 2004 annual summary with detailed diagnosis and procedure data. Vital Health Stat. 13 2006, 162, 1–209. [Google Scholar]
- De Korte, N.; Klarenbeek, B.R.; Kuyvenhoven, J.P.; Roumen, R.M.; Cuesta, M.A.; Stockmann, H.B. Management of diverticulitis: Results of a survey among gastroenterologists and surgeons. Colorectal. Dis. 2011, 13, e411–e417. [Google Scholar] [CrossRef] [PubMed]
- Rafferty, J.; Shellito, P.; Hyman, N.H.; Buie, W.D.; Standards Committee of American Society of Colon and Rectal Surgeons. Practice parameters for sigmoid diverticulitis. Dis. Colon Rectum 2006, 49, 939–944. [Google Scholar] [CrossRef] [PubMed]
- Van de Wall, B.J.; Draaisma, W.A.; van Iersel, J.J.; van der Kaaij, R.; Consten, E.C.; Broeders, I.A. Dietary restrictions for acute diverticulitis: Evidence-based or expert opinion? Int. J. Colorectal Dis. 2013, 28, 1287–1293. [Google Scholar] [CrossRef] [PubMed]
- Stam, M.A.; Draaisma, W.A.; van de Wall, B.J.; Bolkenstein, H.E.; Consten, E.C.; Broeders, I.A. An unrestricted diet for uncomplicated diverticulitis is safe: Results of the prospective diverticulitis diet study. Colorectal Dis. 2016, 19, 372–377. [Google Scholar] [CrossRef] [PubMed]
- Marshall, S. Why is the skeleton still in the hospital closet? A look at the complex aetiology of malnutrition and its implications for the nutrition care team. J. Nutr. Health Aging. 2018, 22, 26–29. [Google Scholar]
- Sands, D.R.; Wexner, S.D. Nasogastric tubes and dietary advancement after laparoscopic and open colorectal surgery. Nutrition 1999, 15, 347–350. [Google Scholar] [CrossRef]
- Mattei, P.; Rombeau, J.L. Review of the pathophysiology and management of postoperative ileus. World J. Surg. 2006, 30, 1382–1391. [Google Scholar] [CrossRef] [PubMed]
- Feingold, D.; Steele, S.R.; Lee, S.; Kaiser, A.; Boushey, R.; Buie, W.D.; Rafferty, J.F. Practice parameters for the treatment of sigmoid diverticulitis. Dis. Colon Rectum 2014, 57, 284–294. [Google Scholar] [CrossRef] [PubMed]
- Queensland Health Nutrition Education Materials Online (NEMO). Available online: https://www.health.qld.gov.au/nutrition (accessed on 1 Mar 2017).
- Commane, D.M.; Arasaradnam, R.P.; Mills, S.; Mathers, J.C.; Bradburn, M. Diet, ageing and genetic factors in the pathogenesis of diverticular disease. World J. Gastroenterol. 2009, 15, 2479–2488. [Google Scholar] [CrossRef] [PubMed]
- Tursi, A. New physiopathological and therapeutic approaches to diverticular disease of the colon. Expert Opin. Pharmacother. 2007, 8, 299–307. [Google Scholar] [CrossRef] [PubMed]
- Tursi, A.; Papagrigoriadis, S. Review article: The current and evolving treatment of colonic diverticular disease. Aliment. Pharmacol. Ther. 2009, 30, 532–546. [Google Scholar] [CrossRef] [PubMed]
- Tursi, A.; Brandimarte, G.; Giorgetti, G.M.; Elisei, W.; Aiello, F. Balsalazide and/or high-potency probiotic mixture (VSL# 3) in maintaining remission after attack of acute, uncomplicated diverticulitis of the colon. Int. J. Colorectal Dis. 2007, 22, 1103–1108. [Google Scholar] [PubMed]
- Ünlü, C.; Daniels, L.; Vrouenraets, B.C.; Boermeester, M.A. A systematic review of high-fibre dietary therapy in diverticular disease. Int. J. Colorectal Dis. 2012, 27, 419–427. [Google Scholar] [CrossRef] [PubMed]
- Carabotti, M.; Annibale, B.; Severi, C.; Lahner, E. Role of Fiber in Symptomatic Uncomplicated Diverticular Disease: A Systematic Review. Nutrients 2017, 9, 161. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Crichton, M.; Dahl, C.; Nucera, R.; Jenkins, J.; Marx, W.; Marshall, S. Can dietary fibre with or without probiotics and antibiotics prevent and manage diverticular disease? A systematic review and meta-analysis. Nutrients 2018. submitted for publication. [Google Scholar]
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.; Cochrane Bias Methods Group; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, D5928. [Google Scholar] [CrossRef] [PubMed]
- Guyatt, G.H.; Oxman, A.D.; Schünemann, H.J.; Tugwell, P.; Knottnerus, A. GRADE guidelines: A new series of articles in the Journal of Clinical Epidemiology. J. Clin. Epidemiol. 2011, 64, 380–382. [Google Scholar] [CrossRef] [PubMed]
- Schünemann, H.; Brożek, J.; Guyatt, G.; Oxman, A. (Eds.) Handbook for Grading the Quality of Evidence and the Strength of Recommendations Using the GRADE Approach. Updated October 2013. 2013. Available online: http://gdt.guidelinedevelopment.org (accessed on 1 September 2017).
- Park, H.C.; Kim, B.S.; Lee, B.H. Management of right colonic uncomplicated diverticulitis: Outpatient versus inpatient management. World J. Surg. 2011, 35, 1118–1122. [Google Scholar] [CrossRef] [PubMed]
- Ridgway, P.F.; Latif, A.; Shabbir, J.; Ofriokuma, F.; Hurley, M.J.; Evoy, D.; O’Mahony, J.B.; Mealy, K. Randomized controlled trial of oral vs. intravenous therapy for the clinically diagnosed acute uncomplicated diverticulitis. Colorectal Dis. 2009, 11, 941–946. [Google Scholar] [CrossRef] [PubMed]
- Moya, P.; Arroyo, A.; Pérez-Legaz, J.; Serrano, P.; Candela, F.; Soriano-Irigaray, L.; Calpena, R. Applicability, safety and efficiency of outpatient treatment in uncomplicated diverticulitis. Tech. Coloproctol. 2012, 16, 301–307. [Google Scholar] [CrossRef] [PubMed]
- Hinchey, E.J.; Schaal, P.G.; Richards, G.K. Treatment of perforated diverticular disease of the colon. Adv. Surg. 1978, 12, 85–109. [Google Scholar] [PubMed]
- Lanas, A.; Ponce, J.; Bignamini, A.; Mearin, F. One year intermittent rifaximin plus fibre supplementation vs. fibre supplementation alone to prevent diverticulitis recurrence: A proof-of-concept study. Dig. Liver Dis. 2013, 45, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Taylor, I.; Duthie, H.L. Bran Tablets and diverticular-disease. Br. Med. J. 1976, 1, 988–990. [Google Scholar] [CrossRef] [PubMed]
- Leahy, A.; Ellis, R.; Quill, D.; Peel, A. High fibre diet in symptomatic diverticular disease of the colon. Ann. R. Coll. Surg. Engl. 1985, 67, 173. [Google Scholar] [PubMed]
- Guyatt, G.; Gutterman, D.; Baumann, M.H.; Addrizzo-Harris, D.; Hylek, E.M.; Phillips, B.; Raskob, G.; Lewis, S.Z.; Schünemann, H. Grading strength of recommendations and quality of evidence in clinical guidelines: Report from an American College of Chest Physicians task force. CHEST J. 2006, 129, 174–181. [Google Scholar] [CrossRef] [PubMed]
- National Health and Medical Research Council (NHMRC). Australian Dietary Guidelines; NHMRC, Australian Government: Canberra, Australia, 2013.
- Public Health England; Welsh Government; Food Standards Scotland; Food Standaryds Agency in Northern Ireland. The Eatwell Guide; Public Health England: London, United Kingdom, 2016.
- Roberto, C.A.; Swinburn, B.; Hawkes, C.; Huang, T.T.; Costa, A.S.; Ashe, M.; Zwicker, L.; Cawley, J.H.; Brownell, K.D. Patchy progress on obesity prevention: Emerging examples, entrenched barriers, and new thinking. Lancet 2015, 385, 2400–2409. [Google Scholar] [CrossRef]
- Lawrence, J. Model and process for nutrition and dietetic practice. Diet. Nutr. Case Stud. 2016, 1–7. [Google Scholar] [CrossRef]
- National Health and Medical Resarch Council (NHMRC). Nutrient Reference Values for Australia and New Zealand Including Recommended Dietary Intakes; National Health and Medical Resarch Council: Canberra, Australia, 2005.
- Staudacher, H.M.; Whelan, K.; Irving, P.M.; Lomer, M.C. Comparison of symptom response following advice for a diet low in fermentable carbohydrates (FODMAPs) versus standard dietary advice in patients with irritable bowel syndrome. J. Hum. Nutr. Diet. 2011, 24, 487–495. [Google Scholar] [CrossRef] [PubMed]
- Darmon, N.; Drewnowski, A. Does social class predict diet quality? Am. J. Clin. Nutr. 2008, 87, 1107–1117. [Google Scholar] [PubMed]
- Parmenter, K.; Waller, J.; Wardle, J. Demographic variation in nutrition knowledge in England. Health Educ. Res. 2000, 15, 163–174. [Google Scholar] [CrossRef] [PubMed]
- Reichert, M.C.; Lammert, F. The genetic epidemiology of diverticulosis and diverticular disease: Emerging evidence. United Eur. Gastroenterol. J. 2015, 3, 409–418. [Google Scholar] [CrossRef] [PubMed]
| Study | Setting | Study Design | Population | Intervention | Comparator | Results |
|---|---|---|---|---|---|---|
| Ridgway et al. [31] |
|
|
| Inpatient treatment liberalised diet (“food and fluid as tolerated”) + oral abx upon admission (Ciprofloxacin 500 mg BD + Metronidazole 400 mg TDS). n = 41 participants | Inpatient treatment bowel rest (NBM) and IV fluids for 24 h with progression to full diet as tolerated according to daily physician consultations + oral abx introduced after 24 h (Ciprofloxacin 400 mg BD + Metronidazole 500 mg TDS). n = 38 participants | Hospital LOS:
Reoccurrence: 30-day readmission rate:
Not compared statistically Gastrointestinal symptoms: Wexford Tenderness Score (score 0–4; higher score indicates higher tenderness/rigidity) at 3-days post-admission:
Recovery: no treatment failures (cessation of oral therapy/crossovers) identified in either group. |
| Park et al. [30] |
|
|
| Outpatient treatment liberalised diet + of 4-days of oral abx (second generation cephalosporins and metronidazole, with progression to ciprofloxacin monotherapy if adverse event suspected; not further specified) n = 40 participants | Inpatient treatment with bowel rest (nil by mouth) until symptom resolution followed by full diet (unclear if progressive stages or immediate move to full diet) + 7–10 days of IV abx (second generation cephalosporins and metronidazole, with progression to ciprofloxacin monotherapy if adverse event suspected; not further specified) n = 63 participants | Hospital LOS:
No difference between groups; P = 0.808. Outpatient visits: visits to the outpatient clinic within 1-week post-diagnosis:
Health care costs: items included and currency not described; assumed USD:
Recovery: Treatment failure (no response to therapy):
|
| van de Wall et al. [12] |
|
|
| Inpatient liberalised diet + 26% treated with abx (not further specified) n = 27 participants | Inpatient bowel rest (NBM) + 40% treated with abx (not further specified). Followed by a median of 3 (range 2–4) successive inpatient diet regimens. n = 65 participants | Hospital LOS
Recovery: treatment failure (development of complications including abscess, perforation or requiring surgery):
Not compared statistically. |
| Inpatient liberalised diet + 26% treated with abx (not further specified) | Inpatient restricted diet: clear liquids + 28% treated with abx (not further specified). Followed by a median of 3 (range 1–3) successive inpatient diet regimens. n = 89 participants | Hospital LOS
Recovery: treatment failure (development of complications including abscess, perforation or requiring surgery):
Not compared statistically. | ||||
| Inpatient liberalised diet + 26% treated with abx (not further specified) | Inpatient restricted diet: liquids + 32% treated with abx (not further specified). Followed by a median of 2 (range 1–2) successive inpatient diet regimens. n = 75 participants | Hospital LOS
Recovery: treatment failure (development of complications including abscess, perforation or requiring surgery): n = 0/27 (0%) in liberalised diet, n = 1/75 (1.3%) in liquid group; not compared statistically. | ||||
| Moya et al. [32] |
|
|
| Outpatient treatment: Restricted diet (liquid only) for 4-days followed by low dietary fibre diet for 3-days with high dietary fibre diet + oral abx (Metronidazole 500 mg/8 h and Ciprofloxacin 500 mg/12 h) + IV analgesics (Acetaminophen 1 g/6 h). Patients reviewed by physician for need of hospitalisation. n = 32 participants | Inpatient treatment: Restricted diet (liquid only) for 3-days followed by low dietary fibre diet for 2-days with high dietary fibre diet upon discharge (5-days post diagnosis) + IV abx (Metronidazole 500 mg/8 h and Ciprofloxacin 400 mg/12 h) + IV analgesics (Acetaminophen 1 g/6 h) for 5-days followed by oral abx (Metronidazole 500 mg/8 h and Ciprofloxacin 500 mg/12 h) for 7-days n = 44 participants. | Hospital LOS:
Reoccurrence: subsequent presentation and diagnosis within average 8–9-months post-diagnosis:
No difference between groups; P = 0.86. Health care costs: direct health costs include ward accommodation, pharmaceutical treatment, laboratory tests and radiology:
|
| Stam et al. [13] |
|
|
| Outpatient treatment liberalised diet (no restrictions of any kind) c + analgesics (acetaminophen or opioids if pain score over 40 on scale 0–100) + iso-osmotic laxative. Nil abx. Patients reviewed by physician for need of hospitalisation. | N/A | Outcomes assessed 6-months post-diagnosis. Hospital admission rate: at the time of first diagnosis:
Hospital LOS: for first diagnosis:
Reoccurrence: subsequent presentation and diagnosis between 3–6 months after initial diagnosis:
|
| Study | Setting | Study Design | Population | Intervention | Comparator | Results |
|---|---|---|---|---|---|---|
| Taylor and Duthie [35] |
|
|
| One month of high fibre diet (termed high-roughage diet) with 18 g dietary fibre from supplements (9 × 2 g bran tables per day). Written educational material provided for high-roughage diet. | One month of dietary fibre supplement with laxative (Normacol: sterculia with frangula bark—dosage not specified) with anti-spasmodic | Gastrointestinal symptoms: at one-month post intervention: gastrointestinal symptom scores (scale 0–17; higher score indicating worse symptoms):
Ongoing gastrointestinal symptoms
Stool weight:
Transit time:
|
| One month of 18g dietary fibre from supplements (9 × 2 g bran tables per day) with no education regarding dietary change. | One month of dietary fibre supplement with laxative (Normacol: sterculia with frangula bark—dosage not specified) with anti-spasmodic | Gastrointestinal symptoms: at one-month post intervention: gastrointestinal symptom scores (scale 0–17; higher score indicating worse symptoms):
Ongoing gastrointestinal symptoms
Stool weight:
Transit time:
| ||||
| One month of high-roughage diet with 18 g dietary fibre from supplements (9 × 2 g bran tables per day). Written educational material provided for high-roughage diet. | One month of 18 g dietary fibre from supplements (9 × 2 g bran tables per day) with no education regarding dietary change. | Gastrointestinal symptoms: at one-month post intervention: gastrointestinal symptom scores (scale 0–17; higher score indicating worse symptoms):
Ongoing gastrointestinal symptoms
Stool weight:
Transit time:
| ||||
| Leahy et al. [36] |
|
|
| Adhering to a high fibre diet (≥25 g dietary fibre/day with or without dietary fibre supplements) 2–11 years after initial hospitalisation. Education was initially given during hospital admission patient counselled by medical and dietetic staff with written educational material. Other in-hospital treatments not described. | Low fibre diet (<25 g/day) allocated by not adhering to high fibre diet recommended in hospital or were not educated regarding high fibre diet). | Reoccurrence: readmission rate at 54–76 months post-diagnosis:
Gastrointestinal symptoms: patient reported ongoing symptoms (dichotomous, no scale/tool used) at 54–76 months post-diagnosis:
|
| Lanas et al. [34] |
|
|
| 7 g dietary fibre supplementation (3.5 g plantago ovata husk [psyllium]] consumed as effervescent granulate BD) consumed daily for 48 weeks. Dietary fibre consumed from diet not measured. | 7 g dietary fibre supplementation (3.5 g plantago ovata husk [psyllium]] consumed as effervescent granulate BD) consumed daily for 48 weeks + poorly absorbed oral abx (400 mg rifaximin polymorph alpha BD) consumed for one week of each month for 48 week. Dietary fibre consumed from diet not measured. | Reoccurrence: readmission rate at 48 weeks from baseline:
Gastrointestinal symptoms: unknown score (scored 0–10, 10 worse symptoms; using visual analogue scale and number of diarrhoea episodes) reflecting gastrointestinal symptoms at 48 weeks from baseline:
|
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dahl, C.; Crichton, M.; Jenkins, J.; Nucera, R.; Mahoney, S.; Marx, W.; Marshall, S. Evidence for Dietary Fibre Modification in the Recovery and Prevention of Reoccurrence of Acute, Uncomplicated Diverticulitis: A Systematic Literature Review. Nutrients 2018, 10, 137. https://doi.org/10.3390/nu10020137
Dahl C, Crichton M, Jenkins J, Nucera R, Mahoney S, Marx W, Marshall S. Evidence for Dietary Fibre Modification in the Recovery and Prevention of Reoccurrence of Acute, Uncomplicated Diverticulitis: A Systematic Literature Review. Nutrients. 2018; 10(2):137. https://doi.org/10.3390/nu10020137
Chicago/Turabian StyleDahl, Camilla, Megan Crichton, Julie Jenkins, Romina Nucera, Sophie Mahoney, Wolfgang Marx, and Skye Marshall. 2018. "Evidence for Dietary Fibre Modification in the Recovery and Prevention of Reoccurrence of Acute, Uncomplicated Diverticulitis: A Systematic Literature Review" Nutrients 10, no. 2: 137. https://doi.org/10.3390/nu10020137
APA StyleDahl, C., Crichton, M., Jenkins, J., Nucera, R., Mahoney, S., Marx, W., & Marshall, S. (2018). Evidence for Dietary Fibre Modification in the Recovery and Prevention of Reoccurrence of Acute, Uncomplicated Diverticulitis: A Systematic Literature Review. Nutrients, 10(2), 137. https://doi.org/10.3390/nu10020137






