An Investigation of the Clinical Utility of the Proposed ICD-11 and DSM-5 Diagnostic Schemes for Eating Disorders Characterized by Recurrent Binge Eating in People with a High BMI
Abstract
1. Introduction
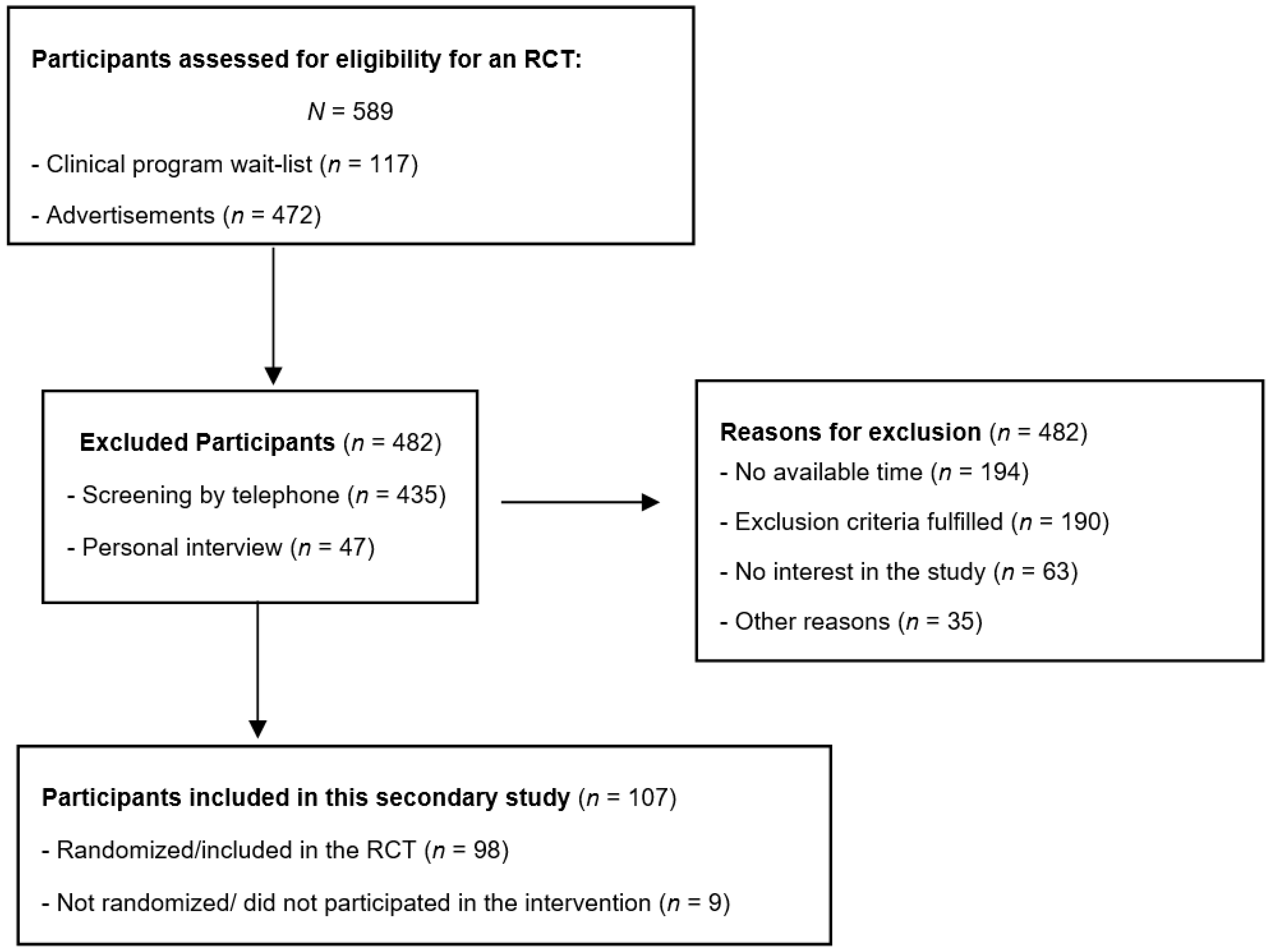
2. Materials and Methods
2.1. Procedures
2.2. Measures
- Mini International Neuropsychiatric Interview (MINI) [18,19]: this structured interview is reliable and validated for diagnoses according to the DSM-5 [1]. The MINI version 5 [21] assessing DSM-IV diagnoses [22] has been translated into Portuguese. Thus, the MINI-5 was used in this study, with modifications to coding according to DSM-5 criteria, as in the MINI-7 [19].
- Eating Disorder Examination (EDE) Edition 17.0D [20]: the EDE is a semi-structured interview. It assesses eating disorder features. It has four subscales measuring levels of dietary restraint, eating, shape and weight concerns. The global score is a mean of subscale scores. In this study, the new Version 17.0D item scoring, that included “being in control” as a reason for the behavior or cognition, was used. EDE version 16.0 [23] has been translated to Brazilian/Portuguese by researchers from the Universidade Federal do Rio de Janeiro (Silvia Freitas, José Carlos Appolinario), by authors of this paper (MAP, AC) and by an eating disorder specialist and member of the Eating Disorder Program (Christina Morgan—CM). A certified translator then back translated it into English. An author of the EDE (O’Connor, M) approved the final version. The translated EDE interrater reliability and concurrent validity were tested and found to be satisfactory. In the validity study, the diagnoses were made according to the eating disorder module of the SCID-I/P interview [24] (Portuguese version) [25]. Diagnostic agreement between the Portuguese EDE version 16.0 and the SCID I/P (both testing DSM-IV diagnoses) was found to be moderate (Kappa = 0.66; n = 149), with a Cronbach α of 0.91 (95% CI: 0.88 0.92) (unpublished data provided by AC). For the purpose of the present study, small adjustments were made by MAP, so that the Portuguese version used was consistent with the 17th version of the EDE [20], in order to derive DSM-5 categories. Cronbach α in this sample was 0.66, n = 107.
- Binge Eating Scale (BES) [26]: the BES is a 16-item self-report instrument that was translated and validated in a Brazilian sample [27]. The BES measures frequency and severity of binge eating. The Brazilian version has undergone psychometric assessment and has a cut-off point for normality of 17 for the screening of eating disorders in obese individuals seeking treatment for weight loss. Cronbach α in this sample was 0.83, n = 106.
- Loss of Control over Eating Scale (LOCES) [28]. This 24-item self-report scale measures loss of control during binge eating episodes in the last 4 weeks, with a mean score of 1.70 (SD = 5.72). It has been translated into Brazilian/Portuguese. This translated version has adequate psychometric properties (factor analysis and convergent validity) [29]. Cronbach α in this sample was 0.91, n = 107.
- Depression, Anxiety and Stress Scale (DASS-21) [30,31] was used in its translated and validated Brazilian/Portuguese version [32]. The DASS is a 21-item self-report instrument that measures the presence and severity of depressive symptoms, anxiety and stress with a cut-off point for normality of 9 for depression, 7 for anxiety and 14 for stress. Cronbach α in this sample was 0.92, and for each subscale was: stress 0.85, depression 0.89, and anxiety 0.77, n = 107.
- Health-related quality of life was assessed with the 12-item Short Form Health Survey (SF-12) [33]: a self-report questionnaire. It has two scales, the Physical Health Component Summary scale (PCS) and Mental Health Component Summary scale (MCS). The English language version has sound psychometric properties and it has been translated into Brazilian/Portuguese [34]. Cronbach α in this sample was 0.79, n = 106.
- Disability was asked with a question closely similar to the ‘days out of role’ questions employed in the Australian National Survey of Mental Health and Well-Being [35]. Participants were asked to write for the past 4 weeks a response to, “on how many days, if any, were you unable to complete your work, study or household responsibilities because of any problem with your (physical or emotional) health”? An author (MAP) translated this text.
2.3. Statistical Analyses
2.4. Ethics
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Trial Registration
References
- American Psychiatric Association (APA). Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Arlington, VA, USA, 2013. [Google Scholar]
- World Health Organization (WHO). The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines; World Health Organization: Geneva, Switzerland, 1992. [Google Scholar]
- First, M.B.; Reed, G.M.; Hyman, S.E.; Saxena, S. The development of the ICD-11 clinical descriptions and diagnostic guidelines for mental and behavioural disorders. World Psychiatry 2015, 14, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Reed, G.M.; First, M.B.; Medina-Mora, M.E.; Gureje, O.; Pike, K.M.; Saxena, S. Draft diagnostic guidelines for ICD-11 mental and behavioural disorders available for review and comment. World Psychiatry 2016, 15, 112–113. [Google Scholar] [CrossRef] [PubMed]
- Reed, G.M.; Correia, J.M.; Esparza, P.; Saxena, S.; Maj, M. The WPA-WHO global survey of psychiatrists’ attitudes towards mental disorders classification. World Psychiatry 2011, 10, 118–131. [Google Scholar] [CrossRef] [PubMed]
- Al-Adawi, S.; Bax, B.; Bryant-Waugh, R.; Claudino, A.M.; Hay, P.; Monteleone, P.; Norring, C.; Pike, K.M.; Pilon, D.J.; Herscovici, C.R.; et al. Revision of ICD—Status update on feeding and eating disorders. Adv. Eat. Disord. Theory Res. Pract. 2013, 1, 10–20. [Google Scholar] [CrossRef]
- Uher, R.; Rutter, M. Classification of feeding and eating disorders: Review of evidence and proposals for ICD-11. World Psychiatry 2012, 11, 80–92. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). ICD-11 Diagnostic Guidelines for Internet-Based Field Study—Feeding and Eating Disorders (D), Version 6, Unpublished work. 2015.
- Global Clinical Practice Network WHO. ICD-11 Diagnostic Guidelines for Internet Based Field Studies. 2015. Available online: https://gcp.network/en/icd-11-guidelines (accessed on 12 October 2017).
- Brownstone, L.M.; Bardone-Cone, A.M.; Fitzsimmons-Craft, E.E.; Printz, K.S.; Le Grange, D.; Mitchell, J.E.; Crow, S.J.; Peterson, C.B.; Crosby, R.D.; Klein, M.H.; et al. Subjective and objective binge eating in relation to eating disorder symptomatology, negative affect, and personality dimensions. Int. J. Eat. Disord. 2013, 46, 66–76. [Google Scholar] [CrossRef] [PubMed]
- Forney, K.J.; Bodell, L.P.; Haedt-Matt, A.A.; Keel, P.K. The incremental validity of the episode size criterion in binge-eating definitions: An examination in women with purging syndromes. Int. J. Eat. Disord. 2016, 49, 651–662. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, P.E.; Conley, C.S.; Rienecke Hoste, R.; Meyer, C.; Blissett, J.M. Perception of control during episodes of eating: Relationships with quality of life and eating psychopathology. Int. J. Eat. Disord. 2012, 45, 115–119. [Google Scholar] [CrossRef] [PubMed]
- Palavras, M.A.; Hay, P.J.; Lujic, S.; Claudino, A.M. Comparing symptomatic and functional outcomes over 5 years in two nonclinical cohorts characterized by binge eating with and without objectively large episodes. Int. J. Eat. Disord. 2015, 48, 1158–1165. [Google Scholar] [CrossRef] [PubMed]
- Agh, T.; Kovács, G.; Supina, D.; Pawaskar, M.; Herman, B.K.; Vokó, Z.; Sheehan, D.V. A systematic review of the health-related quality of life and economic burdens of anorexia nervosa, bulimia nervosa, and binge eating disorder. Eat. Weight Disord. 2016, 21, 353–364. [Google Scholar] [CrossRef] [PubMed]
- Hay, P.; Mitchison, D.; Collado, A.E.L.; González-Chica, D.A.; Stocks, N.; Touyz, S. Burden and health-related quality of life of eating disorders, including Avoidant/Restrictive Food Intake Disorder (ARFID), in the Australian population. J. Eat. Disord. 2017, 5, 21. [Google Scholar] [CrossRef] [PubMed]
- Mitchison, D.; Touyz, S.; González-Chica, D.A.; Stocks, N.; Hay, P. How abnormal is binge eating? 18-Year time trends in population prevalence and burden. Acta Psychiatry Scand. 2017, 136, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Palavras, M.A.; Hay, P.; Touyz, S.; Sainsbury, A.; da Luz, F.; Swinbourne, J.; Estella, N.M.; Claudino, A. Comparing cognitive behavioural therapy for eating disorders integrated with behavioural weight loss therapy to cognitive behavioural therapy-enhanced alone in overweight or obese people with bulimia nervosa or binge eating disorder: Study protocol for a randomised controlled trial. Trials 2015, 16, 578. [Google Scholar] [CrossRef] [PubMed]
- Lecrubier, Y.; Weiller, E.; Hergueta, T.; Amorim, P.; Bonora, L.I.; Lépine, J.P. Mini International Neuropsychiatric Interview—Brazilian Version 5.0.0. DSM-IV, 2002. Available online: www.bibliotecadigital.ufmg.br (accessed on 2 July 2015).
- Sheehan, D.; Janavs, J.; Baker, R.; Sheehan, K.H.; Knapp, E.; Sheehan, M. Mini International Neuropsychiatric Interview—Version 7.0.0 DSM-5 2014. Available online: http://www.medical-outcomes.com (accessed on 2 July 2015).
- Fairburn, C.G.; Cooper, Z.; O’Connor, M. The Eating Disorder Examination, 17th ed.; The Centre for Research on Eating Disorders at Oxford: Oxford, UK, 2014; Available online: www.credo-oxford.com/pdfs/EDE170D.pdf (accessed on 3 July 2015).
- Sheehan, D.V.; Lecrubier, Y.; Sheehan, K.H.; Amorim, P.; Janavs, J.; Weiller, E.; Hergueta, T.; Baker, R.; Dunbar, G.C. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry 1998, 59 (Suppl. 20), 22–33. [Google Scholar] [PubMed]
- American Psychiatric Association (APA). Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; American Psychiatric Association: Washington, DC, USA, 1994. [Google Scholar]
- Fairburn, C.G. Eating Disorder Examination (Edition 16.0D). In Cognitive Behavior Therapy and Eating Disorders; The Guilford Press: New York, NY, USA, 2008; pp. 270–308. [Google Scholar]
- First, M.B.; Spitzer, R.L.; Gibbon, M.; Williams, J.B.W. Structured Clinical Interview for DSM-IV Axis I Disorders-Patient Edition (SCID-I/P, Version 2.0); Biometric Research, New York State Psychiatric Institute: New York, NY, USA, 1996. [Google Scholar]
- Versiani, M. Entrevista Clínica Estruturada—DSM-IV Transtornos do Eixo I. Tradução da Structured Clinical Interview for DSM-IV Axis I/Patient; Versão 2.1; Programa de Ansiedade e Depressão, Instituto de Psiquiatria IPUB, UFRJ: Rio de Janeiro, Brazil, 1996. [Google Scholar]
- Gormally, J.; Black, S.; Daston, S.; Rardin, D. The assessment of binge eating severity among obese persons. Addict. Behav. 1982, 7, 47–55. [Google Scholar] [CrossRef]
- Freitas, S.; Lopes, C.S.; Coutinho, W.; Appolinario, J.C. Tradução e adaptação para o português da escala de compulsão alimentar periódica. Rev. Bras. Psiquiatr. 2001, 23, 215–220. [Google Scholar] [CrossRef]
- Latner, J.D.; Mond, J.M.; Kelly, M.C.; Haynes, S.N.; Hay, P.J. The Loss of Control Over Eating Scale: Development and psychometric evaluation. Int. J. Eat. Disord. 2014, 47, 647–659. [Google Scholar] [CrossRef] [PubMed]
- Luz, F.Q.; Sainsbury, A.; Estella, N.M.; Cogo, H.; Touyz, S.W.; Palavras, M.A.; Latner, J.D.; Claudino, A.; Hay, P. An empirical evaluation of the translation to Brazilian Portuguese of the Loss of Control Over Eating Scale (LOCES). Arch. Clin. Psychiatry 2016, 43, 1–5. [Google Scholar] [CrossRef]
- Henry, J.D.; Crawford, J.R. The short-form version of the Depression Anxiety Stress Scales (DASS-21): Construct validity and normative data in a large non-clinical sample. Br. J. Clin. Psychol. 2005, 44, 227–239. [Google Scholar] [CrossRef] [PubMed]
- Lovibond, P.F.; Lovibond, S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Vignola, R.C.; Tucci, A.M. Adaptation and validation of the depression, anxiety and stress scale (DASS) to Brazilian Portuguese. J. Affect. Disord. 2014, 155, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Ware, J., Jr.; Kosinski, M.; Keller, S.D. A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Med. Care 1996, 34, 220–233. [Google Scholar] [CrossRef] [PubMed]
- Silveira, M.F.; Almeida, J.C.; Freire, R.S.; Haikal, D.S.; Martins, A.E.B.L. Propriedades psicométricas do instrumento de avaliação da qualidade de vida: 12-item health survey (SF-12). Ciência Saúde Coletiva 2013, 18, 1923–1931. [Google Scholar] [CrossRef] [PubMed]
- Slade, T.; Johnston, A.; Oakley Browne, M.A.; Andrew, G.; Whiteford, H. 2007 National Survey of Mental Health and Wellbeing: Methods and key findings. Aust. N. Z. J. Psychiatry 2009, 43, 594–605. [Google Scholar] [CrossRef] [PubMed]
- IBM Corp. Released 2015. IBM SPSS Statistics for Windows; Version 23.0; IBM Corp: Armonk, NY, USA, 2015. [Google Scholar]
- Reed, G.M. Toward ICD-11: Improving the clinical utility of WHO’s international classification of mental disorders. Prof. Psychol. Res. 2010, 41, 457–464. [Google Scholar] [CrossRef]
- Hudson, J.I.; Hirpi, E.; Pope, H.G., Jr.; Kessler, R.C. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol. Psychiatry 2007, 61, 348–358. [Google Scholar] [CrossRef] [PubMed]
| Clinical Features | Bulimia Nervosa | Binge Eating Disorder | # Osfed/Ufed/Ofed | All | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| DSM–5 (n = 15) | ICD–11 (n = 20) | DSM–5 (n = 70) | ICD–11 (n = 82) | DSM–5 (n = 22) | ICD–11 (n = 5) | N = 107 | ||||
| Median (IQR) | Z (p) † | Median (IQR) | Z (p) | Median (IQR) | MWU Z (p) | |||||
| EDE global | 3.59 (3.27–3.83) | 3.80 (2.35–3.83) | −0.044 (0.965) | 2.48 (1.95–2.88) | 2.27 (1.93–2.41) | −1.233 (0.217) | 2.23 (1.98–2.74) | 2.60 (2.01–2.77) | −0.196 (0.845) | 2.57 (2.03–3.23) |
| EDE restriction | 3.00 (2.70–3.60) | 2.20 (1.00–3.80) | −0.394 (0.694) | 1.60 (0.08–2.40) | 1.40 (0.50–2.20) | −0.994 (0.320) | 1.60 (0.60–2.20) | 1.40 (1.00–1.60) | −0.157 (0.875) | 1.80 (0.80–2.40) |
| EDE eating concern | 2.00 (1.90–2.70) | 3.00 (2.60–3.20) | −1.228 (0.220) | 1.20 (0.60–2.20) | 0.90 (0.20–1.40) | −1.605 (0.108) | 1.20 (0.20–2.40) | 0.60 (0.40–2.40) | −0.197 (0.844) | 1.40 (0.60–2.40) |
| EDE shape concern | 5.00 (4.25–5.37) | 4.62 (2.62–4.75) | −0.961 (0.336) | 3.62 (2.62–4.50) | 3.44 (3.06–4.20) | −0.230 (0.818) | 3.50 (3.00–4.62) | 3.62 (2.88–3.88) | −0.118 (0.906) | 3.75 (2.87–4.62) |
| EDE weight concern | 4.20 (3.30–4.70) | 3.20 (3.20–3.80) | −1.488 (0.137) | 3.20 (2.40–4.20) | 3.20 (2.70–3.67) | −0.263 (0.793) | 3.20 (2.80–3.75) | 2.80 (2.60–3.60) | −0.472 (0.637) | 3.20 (2.60–4.20) |
| Binge Eating Scale | 35.00 (30.50–41.00) | 32.00 (31.00–33.00) | −0.963 (0.335) | 29.00 (22.00–33.00) | 28.00 (21.00–32.50) | −0.677 (0.498) | 28.00 (24.00–33.00) | 25.00 (25.00–25.00) | −1.061 (0.289) | 30.00 (23.00–35.00) |
| LOCES | 3.67 (3.29–4.18) | 3.50 (3.08–3.62) | −0.917 (0.359) | 3.21 (2.79–3.50) | 3.12 (2.62–3.43) | −0.564 (0.573) | 3.33 (2.70–3.54) | 3.45 (3.41–3.50) | −0.746 (0.456) | 3.33 (2.83–3.58) |
| DASS depression | 22.00 (16.50–33.00) | 24.00 (24.00–28.00) | −0.044 (0.965) | 12.00 (6.00–20.00) | 14.00 (7.00–17.00) | −0.066 (0.948) | 16.00 (10.00–24.00) | 10.00 (8.00–12.00) | −1.178 (0.239) | 14.00 (8.00–24.00) |
| DASS anxiety | 12.00 (5.00–14.00) | 22.00 (4.00–26.00) | −0.615 (0.539) | 8.00 (4.00–14.00) | 17.00 (2.00–20.00) | −0.896 (0.370) | 18.00 (2.00–22.00) | 18.00 (6.00–18.00) | −0.277 (0.782) | 10.00 (4.00–16.00) |
| DASS stress | 28.00 (20.00–34.00) | 30.00 (26.00–32.00) | −0.307 (0.799) | 18.00 (12.00–28.00) | 21.00 (14.00–27.00) | −0.059 (0.953) | 26.00 (16.00–28.00) | 20.00 (18.00–22.00) | −0.511 (0.609) | 20.00 (14.00–28.00) |
| SFMCS | 30.12 (26.63–38.70) | 34.35 (34.32–40.81) | −1.702 (0.089) | 36.34 (26.60–42.70) | 37.14 (31.24–42.94) | −0.499 (0.618) | 36.70 (32.61–42.74) | 42.03 (35.74–44.78) | −1.136 (0.256) | 36.02 (27.42–42.71) |
| SFPCS | 46.27 (43.51–52.98) | 47.00 (46.50–55.90) | −0.567 (0.570) | 50.24 (41.97–56.36) | 48.77 (40.64–56.60) | −0.273 (0.785) | 47.00 (41.14–55.90) | 50.39 (47.13–53.58) | −0.431 (0.667) | 49.82 (41.52–56.20) |
| Body Mass Index (kg/m2) | 32.60 (29.72–34.31) | 32.70 (31.30–34.60) | −0.655 (0.513) | 33.60 (31.12–35.85) | 34.65 (32.63–37.02) | −0.964 (0.335) | 33.80 (32.37–36.90) | 33.89 (30.70–35.29) | −0.823 (0.411) | 33.64 (31.08–35.90) |
| Days out of role/28 days | 10.00 (1.00–15.00) | 4.00 (2.00–10.00) | −0.482 (0.630) | 5.00 (2.00–12.00) | 1.00 (0–11.00) | −1.341 (0.180) | 2.00 (0–10.00) | 0 (0–0) | −1.466 (0.143) | 5.00 (0–12.00) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amorim Palavras, M.; Hay, P.; Claudino, A. An Investigation of the Clinical Utility of the Proposed ICD-11 and DSM-5 Diagnostic Schemes for Eating Disorders Characterized by Recurrent Binge Eating in People with a High BMI. Nutrients 2018, 10, 1751. https://doi.org/10.3390/nu10111751
Amorim Palavras M, Hay P, Claudino A. An Investigation of the Clinical Utility of the Proposed ICD-11 and DSM-5 Diagnostic Schemes for Eating Disorders Characterized by Recurrent Binge Eating in People with a High BMI. Nutrients. 2018; 10(11):1751. https://doi.org/10.3390/nu10111751
Chicago/Turabian StyleAmorim Palavras, Marly, Phillipa Hay, and Angélica Claudino. 2018. "An Investigation of the Clinical Utility of the Proposed ICD-11 and DSM-5 Diagnostic Schemes for Eating Disorders Characterized by Recurrent Binge Eating in People with a High BMI" Nutrients 10, no. 11: 1751. https://doi.org/10.3390/nu10111751
APA StyleAmorim Palavras, M., Hay, P., & Claudino, A. (2018). An Investigation of the Clinical Utility of the Proposed ICD-11 and DSM-5 Diagnostic Schemes for Eating Disorders Characterized by Recurrent Binge Eating in People with a High BMI. Nutrients, 10(11), 1751. https://doi.org/10.3390/nu10111751





