Mood Disorders and Gluten: It’s Not All in Your Mind! A Systematic Review with Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
- All studies evaluating the effect of gluten ingestion or elimination on the presence or severity of depressive symptoms and other mood disorders, with any gluten-related intervention for any length of time.
- All prospective intervention studies—randomised, non-randomised, longitudinal—which investigated the change in the severity of mood symptoms as a primary or secondary outcome using a validated questionnaire. We excluded retrospective and cross-sectional studies, as we aimed to investigate the relationship between mood and gluten over a specified amount of time while measuring adherence.
- Published studies in English.
- Data must be reported as means and standard deviations (SDs), or these values must be calculatable or estimable using the available data by methods outlined in the Cochrane Handbook [45].
- Each study should report a different sample; for different studies utilising the same sample, as part of a follow-up study or ad-hoc analysis for example, only data from the most relevant study or the study reporting the largest sample were included.
- For comparisons between patients and healthy controls, control and patient groups must be demographically matched by age and gender.
2.2. Search Strategy and Selection Criteria
2.3. Data Extraction and Quality Assessment
2.4. Statistical Analysis
2.5. Heterogeneity and Sensitivity Analyses
2.6. Missing Data
3. Results
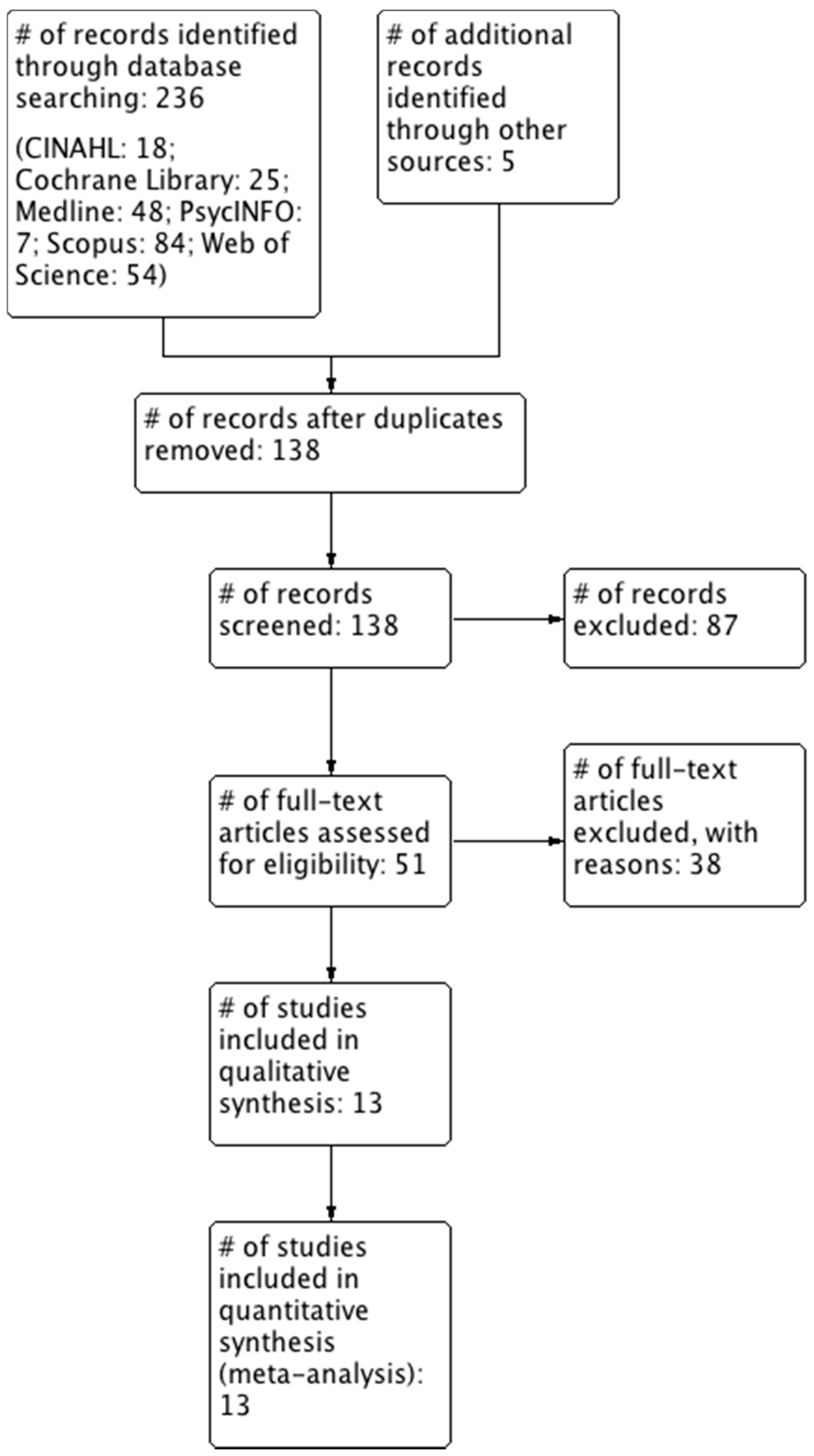
3.1. Literature Search
3.2. Characteristics of the Included Studies
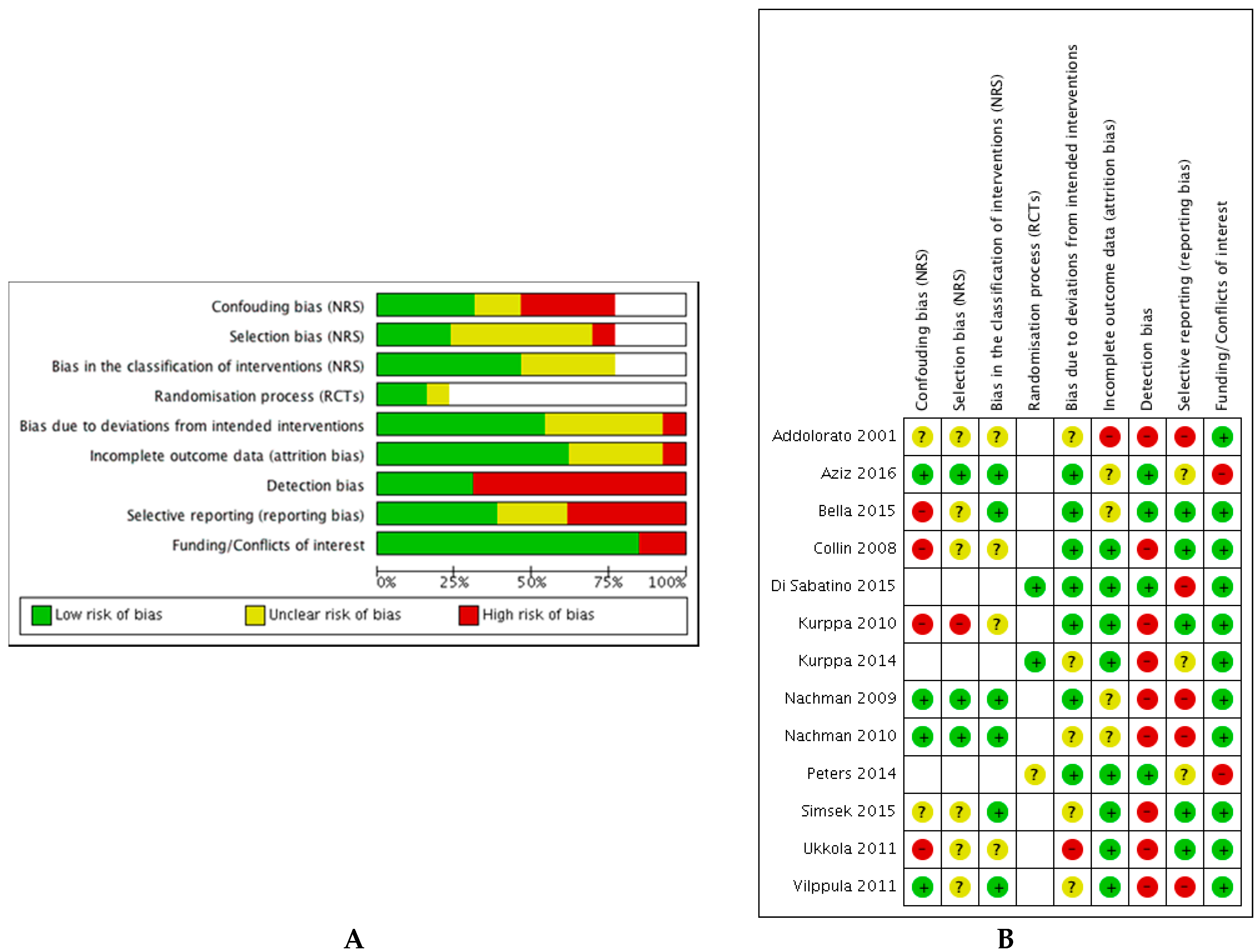
3.3. Quality Assessment
3.4. Data and Analyses
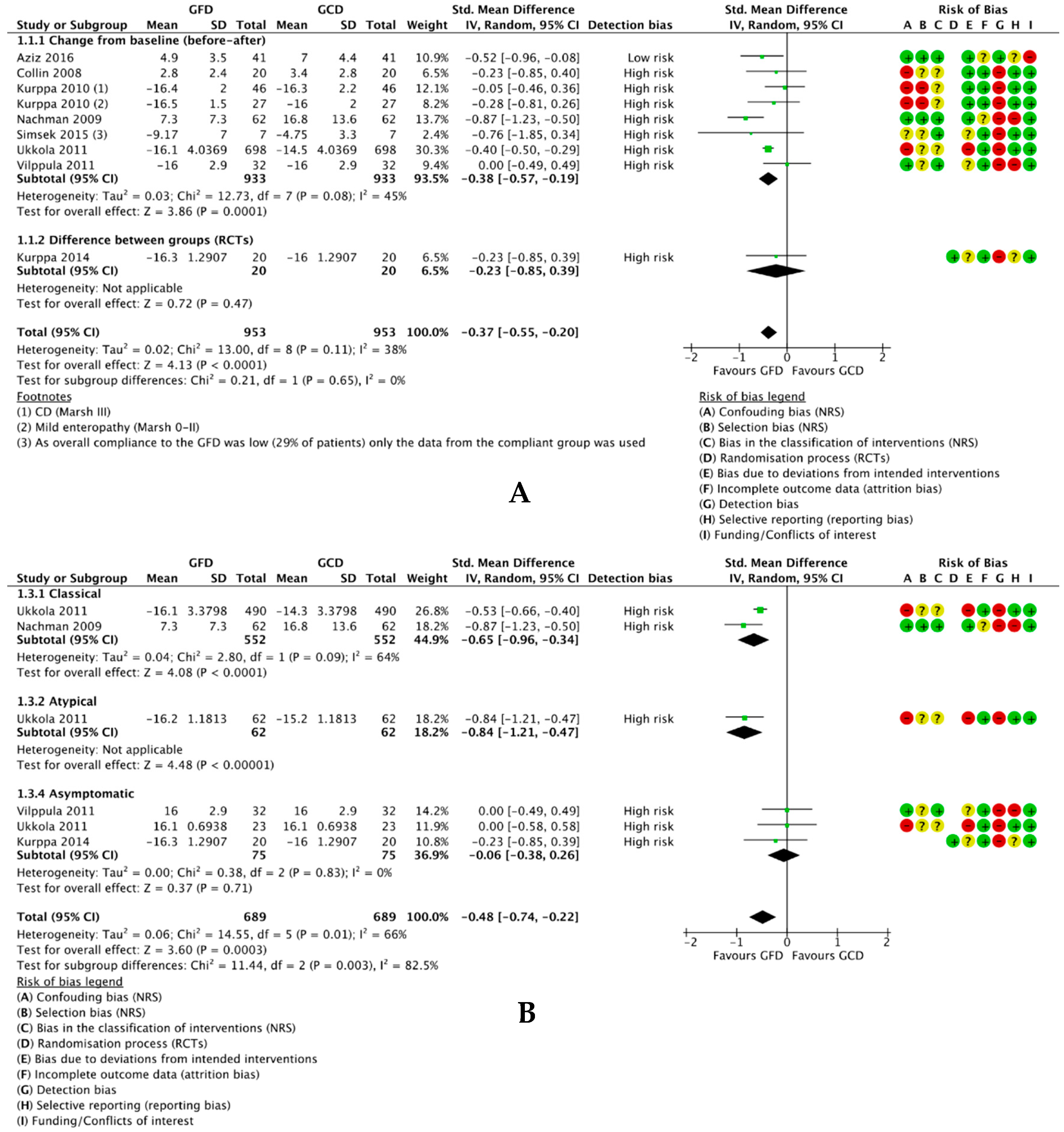
3.4.1. A GFD vs. A Gluten-Containing Diet
3.4.1.1. Difference in Mean Depression Scores
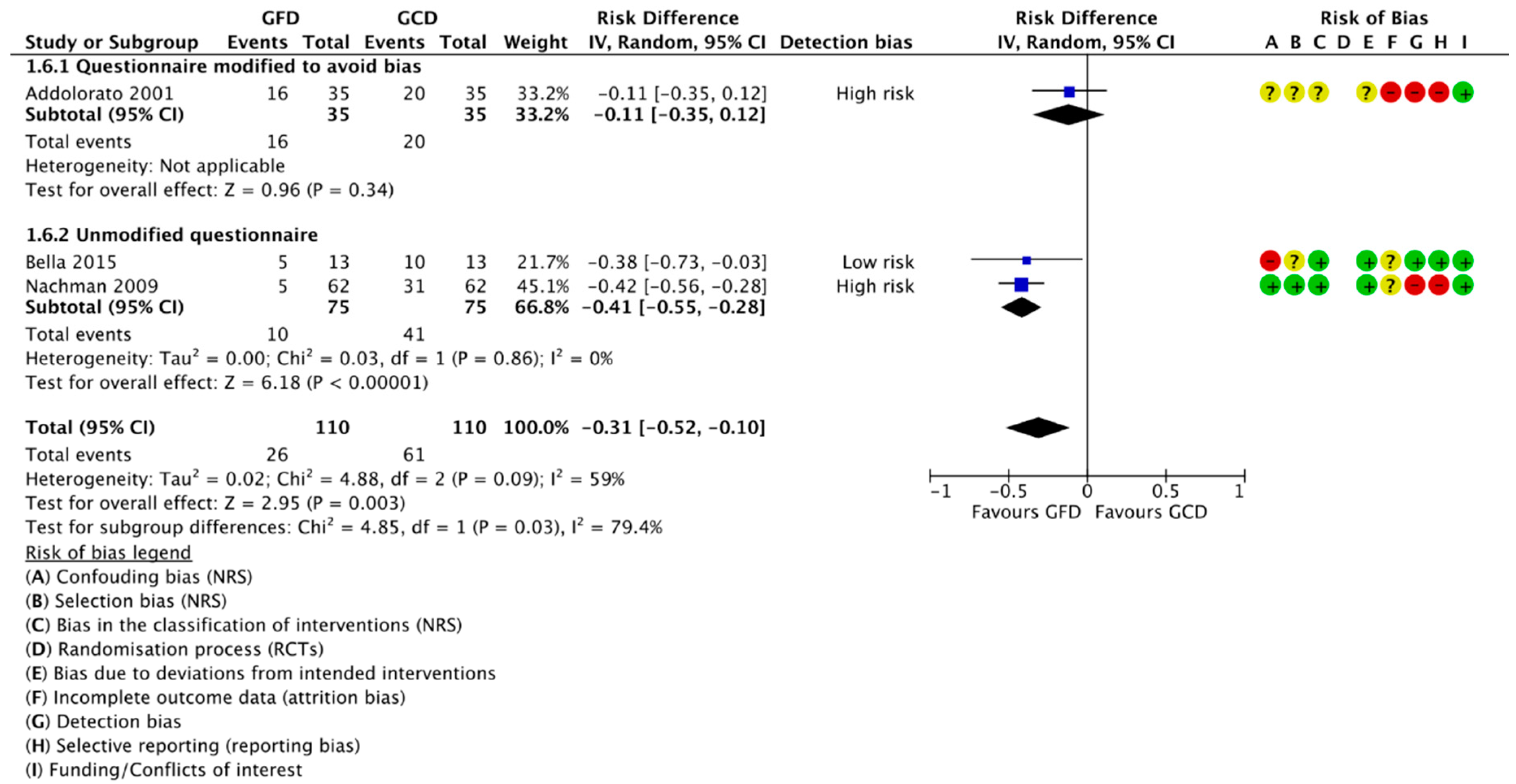
3.4.1.2. Change in Number of Participants Positive for Depression
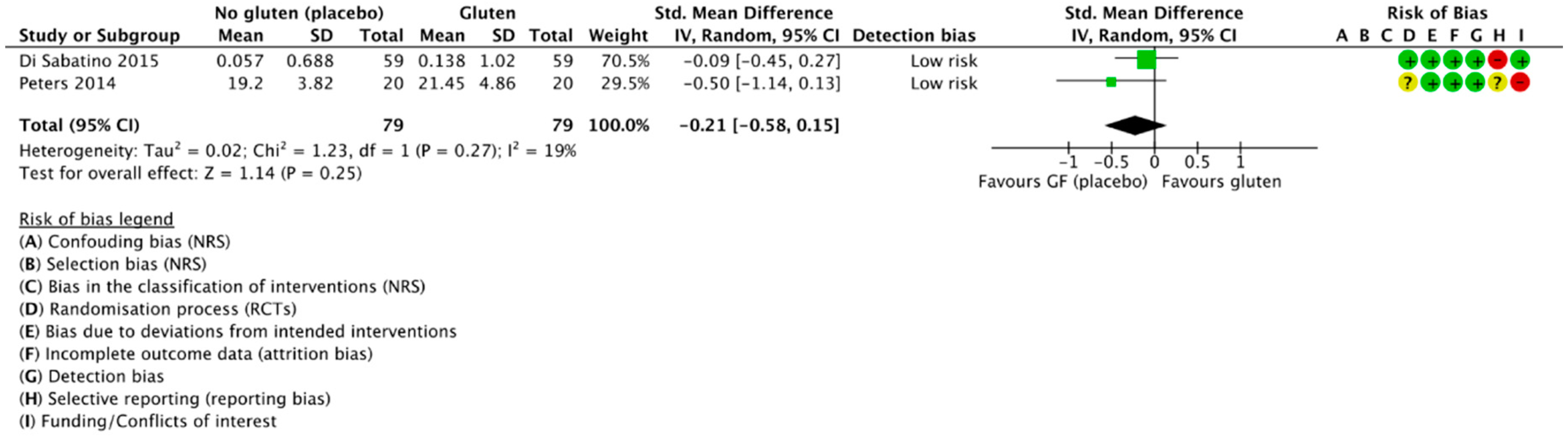
3.4.2. Gluten Challenge vs. Placebo (GFD)
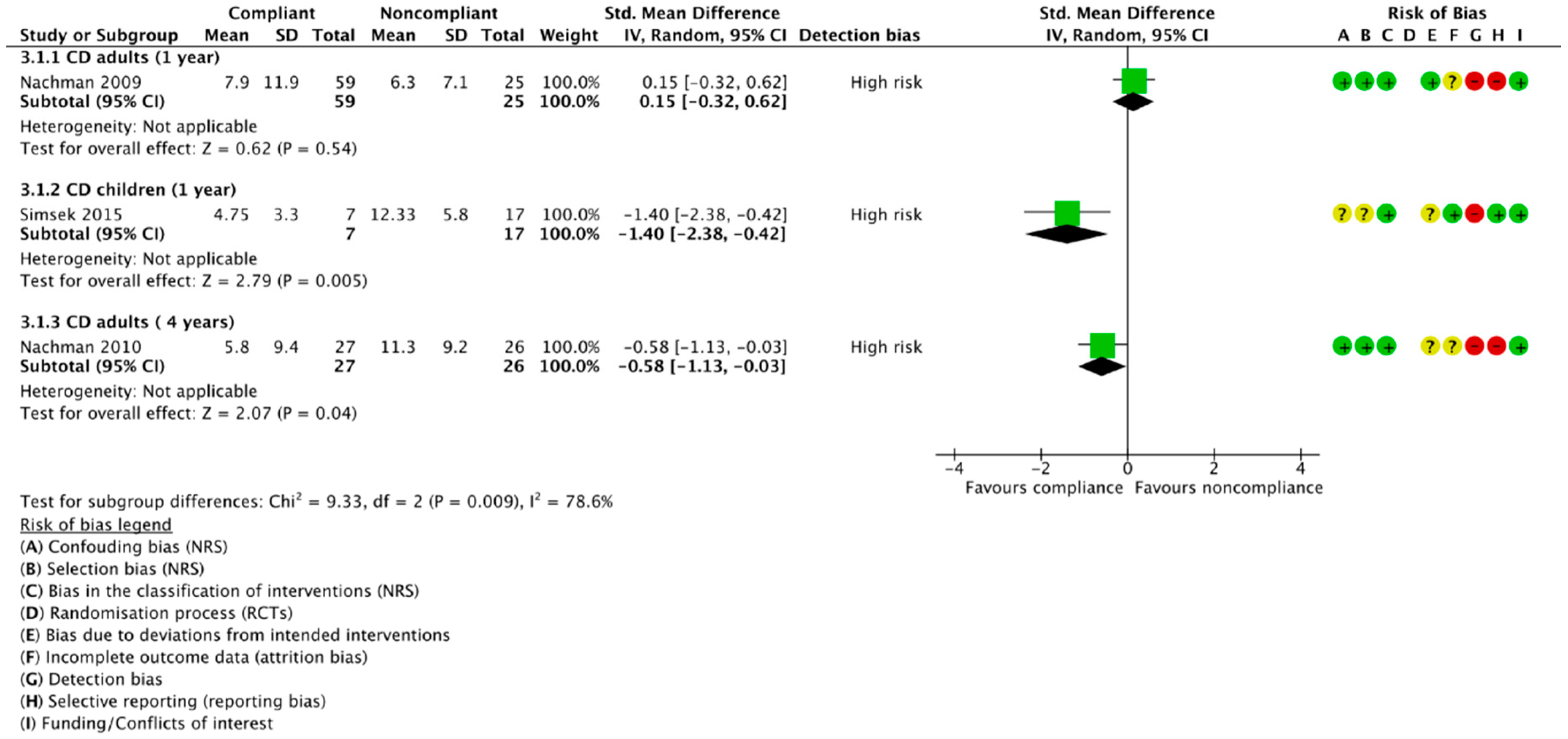
3.4.3. Compliant vs. Noncompliant Participants
3.4.4. GFD-Treated Patients vs. Healthy Controls
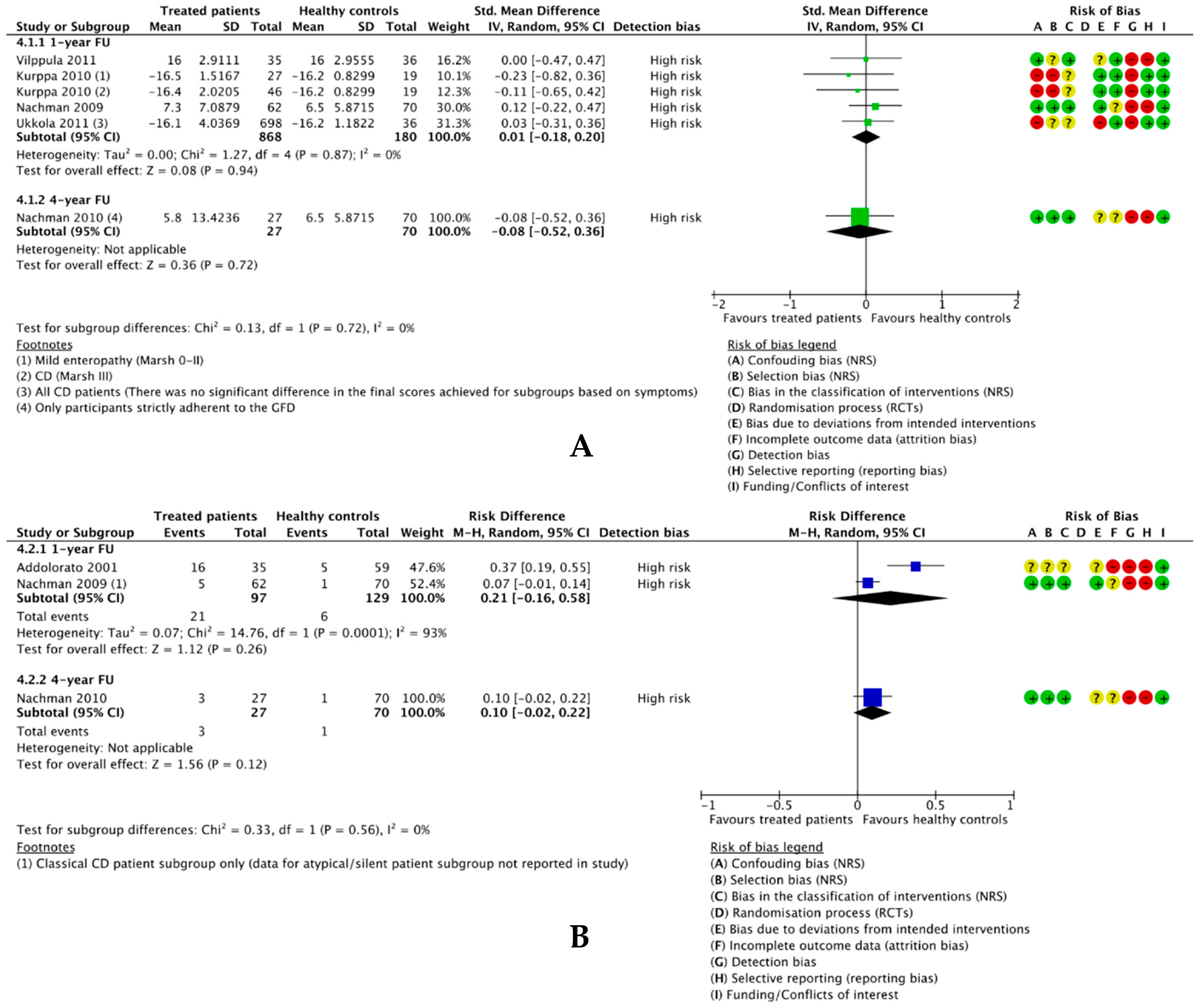
3.4.4.1. Difference in Mean Depression Scores
3.4.4.2. Difference in Number Participants Positive for Depression
3.5. Sensitivity Analyses
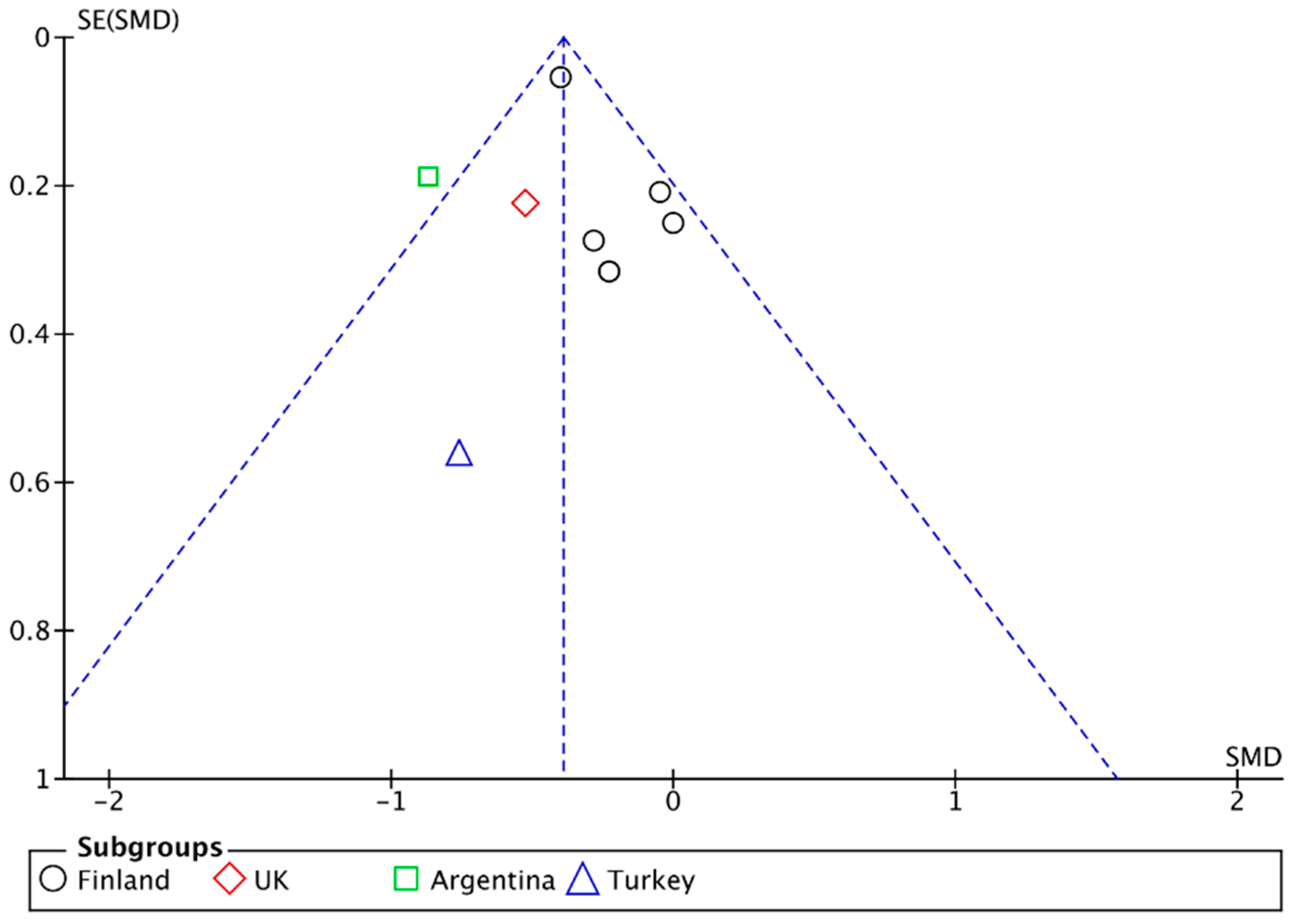
3.6. Publication Bias
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Depression. Available online: http://www.who.int/news-room/fact-sheets/detail/depression (accessed on 22 October 2018).
- NHS. Statistics for England, 2002–2012; Prescriptions Dispensed in the Community; NHS: London, UK, 2013.
- World Health Organization. Depression and Other Common Mental Disorders; Global Health Estimates; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Sapone, A.; Bai, J.C.; Ciacci, C.; Dolinsek, J.; Green, P.H.; Hadjivassiliou, M.; Kaukinen, K.; Rostami, K.; Sanders, D.S.; Schumann, M.; et al. Spectrum of gluten-related disorders: Consensus on new nomenclature and classification. BMC Med. 2012, 10, 13. [Google Scholar] [CrossRef] [PubMed]
- NIH. In Proceedings of the NIH Consensus Development Conference on Celiac Disease, Bethesda, MD, USA, 28–30 June 2004; Volume 21, pp. 1–23.
- Black, J.L.; Orfila, C. Impact of coeliac disease on dietary habits and quality of life. J. Hum. Nutr. Diet. 2011, 24, 582–587. [Google Scholar] [CrossRef] [PubMed]
- Tack, G.J.; Verbeek, W.H.M.; Schreurs, M.W.J.; Mulder, C.J.J. The spectrum of celiac disease: Epidemiology, clinical aspects and treatment. Nat. Rev. Gastroenterol. Hepatol. 2010, 7, 204–213. [Google Scholar] [CrossRef] [PubMed]
- Addolorato, G.; Di Giuda, D.; De Rossi, G.; Valenza, V.; Domenicali, M.; Caputo, F.; Gasbarrini, A.; Capristo, E.; Gasbarrini, G. Regional cerebral hypoperfusion in patients with celiac disease. Am. J. Med. 2004, 116, 312–317. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.F.; Gerdes, L.U. Meta-analysis on anxiety and depression in adult celiac disease: Anxiety and depression in celiac disease. Acta Psychiatr. Scand. 2012, 125, 189–193. [Google Scholar] [CrossRef] [PubMed]
- Ludvigsson, J.F.; Leffler, D.A.; Bai, J.; Biagi, F.; Fasano, A.; Green, P.H.; Hadjivassiliou, M.; Kaukinen, K.; Kelly, C.; Leonard, J.N.; et al. The Oslo definitions for coeliac disease and related terms. Gut 2013, 62, 43. [Google Scholar] [CrossRef] [PubMed]
- Simsek, S.; Baysoy, G.; Gencoglan, S.; Uluca, U. Effects of Gluten-Free Diet on Quality of Life and Depression in Children with Celiac Disease. J. Pediatr. Gastroenterol. Nutr. 2015, 61, 303. [Google Scholar] [CrossRef] [PubMed]
- Liester, M.B.; Liester, M.G. A Review of Psychiatric Disorders Associated with Celiac Disease. Dual Diagn. Open Access 2017, 3. [Google Scholar] [CrossRef]
- Catassi, C.; Elli, L.; Bonaz, B.; Bouma, G.; Carroccio, A.; Castillejo, G.; Cellier, C.; Cristofori, F.; de Magistris, L.; Dolinsek, J.; et al. Diagnosis of Non-Celiac Gluten Sensitivity (NCGS): The Salerno Experts’ Criteria. Nutrients 2015, 7, 4966–4977. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Catassi, C. Gluten Sensitivity. Ann. Nutr. Metab. 2015, 67 (Suppl. S2), 16–26. [Google Scholar] [CrossRef] [PubMed]
- Volta, U.; Tovoli, F.; Cicola, R.; Parisi, C.; Fabbri, A.; Piscaglia, M.; Fiorini, E.; Caio, G. Serological tests in gluten sensitivity (nonceliac gluten intolerance). J. Clin. Gastroenterol. 2012, 46, 680–685. [Google Scholar] [CrossRef] [PubMed]
- Daynes, G. Bread and Tears—Naughtiness, Depression and Fits Due to Wheat Sensitivity. Proc. R. Soc. Med. 1956, 49, 391–394. [Google Scholar] [PubMed]
- Carroccio, A.; Giambalvo, O.; Blasca, F.L.; Iacobucci, R.; D’Alcamo, A.; Mansueto, P. Self-Reported Non-Celiac Wheat Sensitivity in High School Students: Demographic and Clinical Characteristics. Nutrients 2017, 9, 771. [Google Scholar] [CrossRef] [PubMed]
- Harper, L.; Bold, J.S. An exploration into the motivation for gluten avoidance in the absence of coeliac disease. Gastroenterol. Hepatol. Bed Bench 2018. [Google Scholar] [CrossRef]
- Porcelli, B.; Verdino, V.; Ferretti, F.; Bizzaro, N.; Terzuoli, L.; Cinci, F.; Bossini, L.; Fagiolini, A. A study on the association of mood disorders and gluten-related diseases. Psychiatry Res. 2018, 260, 366–370. [Google Scholar] [CrossRef] [PubMed]
- Karakula-Juchnowicz, H.; Gałęcka, M.; Rog, J.; Bartnicka, A.; Łukaszewicz, Z.; Krukow, P.; Morylowska-Topolska, J.; Skonieczna-Zydecka, K.; Krajka, T.; Jonak, K.; et al. The Food-Specific Serum IgG Reactivity in Major Depressive Disorder Patients, Irritable Bowel Syndrome Patients and Healthy Controls. Nutrients 2018, 10, 548. [Google Scholar] [CrossRef] [PubMed]
- Jackson, J.; Eaton, W.; Cascella, N.; Fasano, A.; Santora, D.; Sullivan, K.; Feldman, S.; Raley, H.; McMahon, R.P.; Carpenter, W.T.J.; et al. Gluten sensitivity and relationship to psychiatric symptoms in people with schizophrenia. Schizophr. Res. 2014, 159, 539–542. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dickerson, F.; Stallings, C.; Origoni, A.; Vaughan, C.; Khushalani, S.; Yolken, R. Markers of gluten sensitivity in acute mania: A longitudinal study. Psychiatry Res. 2012, 196, 68–71. [Google Scholar] [CrossRef] [PubMed]
- Karakuła-Juchnowicz, H.; Szachta, P.; Opolska, A.; Morylowska-Topolska, J.; Gałęcka, M.; Juchnowicz, D.; Krukow, P.; Lasik, Z. The role of IgG hypersensitivity in the pathogenesis and therapy of depressive disorders. Nutr. Neurosci. 2017, 20, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Fera, T.; Cascio, B.; Angelini, G.; Martini, S.; Guidetti, C. Affective disorders and quality of life in adult coeliac disease patients on a gluten-free diet. Eur. J. Gastroenterol. Hepatol. 2003, 15, 1287–1292. [Google Scholar] [CrossRef] [PubMed]
- Roos, S.; Kärner, A.; Hallert, C. Gastrointestinal symptoms and well-being of adults living on a gluten-free diet: A case for nursing in celiac disease. Gastroenterol. Nurs. 2009, 32, 196–201. [Google Scholar] [CrossRef] [PubMed]
- Ruepert, L.; Quartero, A.O.; de Wit, N.J.; van der Heijden, G.J.; Rubin, G.; Muris, J.W. Bulking agents, antispasmodics and antidepressants for the treatment of irritable bowel syndrome. Cochrane Database Syst. Rev. 2011, CD003460. [Google Scholar] [CrossRef] [PubMed]
- Hallert, C.; Svensson, M.; Tholstrup, J.; Hultberg, B. Clinical trial: B vitamins improve health in patients with coeliac disease living on a gluten-free diet. Aliment. Pharmacol. Therapeut. 2009, 29, 811–816. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Biesiekierski, J.R.; Peters, S.L.; Newnham, E.D.; Rosella, O.; Muir, J.G.; Gibson, P.R. No effects of gluten in patients with self-reported non-celiac gluten sensitivity after dietary reduction of fermentable, poorly absorbed, short-chain carbohydrates. Gastroenterology 2013, 145, 320–328. [Google Scholar] [CrossRef] [PubMed]
- Dieterich, W.; Schuppan, D.; Schink, M.; Schwappacher, R.; Wirtz, S.; Agaimy, A.; Neurath, M.F.; Zopf, Y. Influence of low FODMAP and gluten-free diets on disease activity and intestinal microbiota in patients with non-celiac gluten sensitivity. Clin. Nutr. 2018. [Google Scholar] [CrossRef] [PubMed]
- Horvath-Stolarczyk, A.; Sidor, K.; Dziechciarz, P.; Siemińska, J. Assessment of emotional status, selected personality traits and depression in young adults with celiac disease. Pediatr. Wspolczesna 2002, 4, 241–246. [Google Scholar]
- Cicarelli, G.; Della Rocca, G.; Amboni, M.; Ciacci, C.; Mazzacca, G.; Filla, A.; Barone, P. Clinical and neurological abnormalities in adult celiac disease. Neurol. Sci. 2003, 24, 311–317. [Google Scholar] [CrossRef] [PubMed]
- Burger, J.P.W.; de Brouwer, B.; IntHout, J.; Wahab, P.J.; Tummers, M.; Drenth, J.P.H. Systematic review with meta-analysis: Dietary adherence influences normalization of health-related quality of life in coeliac disease. Clin. Nutr. 2017, 36, 399–406. [Google Scholar] [CrossRef] [PubMed]
- Shahbazkhani, B.; Sadeghi, A.; Malekzadeh, R.; Khatavi, F.; Etemadi, M.; Kalantri, E.; Rostami-Nejad, M.; Rostami, K. Non-Celiac Gluten Sensitivity Has Narrowed the Spectrum of Irritable Bowel Syndrome: A Double-Blind Randomized Placebo-Controlled Trial. Nutrients 2015, 7, 4542–4554. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caio, G.; Volta, U.; Tovoli, F.; De Giorgio, R. Effect of gluten free diet on immune response to gliadin in patients with non-celiac gluten sensitivity. BMC Gastroenterol. 2014, 14, 26. [Google Scholar] [CrossRef] [PubMed]
- Sainsbury, K.; Marques, M.M. The relationship between gluten free diet adherence and depressive symptoms in adults with coeliac disease: A systematic review with meta-analysis. Appetite 2018, 120, 578–588. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vazquez-Roque, M.I.; Camilleri, M.; Smyrk, T.; Murray, J.A.; Marietta, E.; O’Neill, J.; Carlson, P.; Lamsam, J.; Janzow, D.; Eckert, D.; et al. A controlled trial of gluten-free diet in patients with irritable bowel syndrome-diarrhea: Effects on bowel frequency and intestinal function. Gastroenterology 2013, 144, 903–911. [Google Scholar] [CrossRef] [PubMed]
- Soares, F.L.P.; de Oliveira Matoso, R.; Teixeira, L.G.; Menezes, Z.; Pereira, S.S.; Alves, A.C.; Batista, N.V.; de Faria, A.M.C.; Cara, D.C.; Ferreira, A.V.M.; et al. Gluten-free diet reduces adiposity, inflammation and insulin resistance associated with the induction of PPAR-alpha and PPAR-gamma expression. J. Nutr. Biochem. 2013, 24, 1105–1111. [Google Scholar] [CrossRef] [PubMed]
- Mulloy, A.; Lang, R.; O’Reilly, M.; Sigafoos, J.; Lancioni, G.; Rispoli, M. Gluten-free and casein-free diets in the treatment of autism spectrum disorders: A systematic review. Res. Autism Spectr. Disord. 2010, 4, 328–339. [Google Scholar] [CrossRef]
- Piwowarczyk, A.; Horvath, A.; Łukasik, J.; Pisula, E.; Szajewska, H. Gluten- and casein-free diet and autism spectrum disorders in children: A systematic review. Eur. J. Nutr. 2018, 57, 433–440. [Google Scholar] [CrossRef] [PubMed]
- Brietzke, E.; Cerqueira, R.O.; Mansur, R.B.; McIntyre, R.S. Gluten related illnesses and severe mental disorders: A comprehensive review. Neurosci. Biobehav. Rev. 2018, 84, 368–375. [Google Scholar] [CrossRef] [PubMed]
- Losurdo, G.; Principi, M.; Iannone, A.; Amoruso, A.; Ierardi, E.; Leo, A.D.; Barone, M. Extra-intestinal manifestations of non-celiac gluten sensitivity: An expanding paradigm. World J. Gastroenterol. 2018, 24, 1521–1530. [Google Scholar] [CrossRef] [PubMed]
- Peters, S.L.; Biesiekierski, J.R.; Yelland, G.W.; Muir, J.G.; Gibson, P.R. Randomised clinical trial: Gluten may cause depression in subjects with non-coeliac gluten sensitivity—An exploratory clinical study. Aliment. Pharmacol. Therapeut. 2014, 39, 1104–1112. [Google Scholar] [CrossRef] [PubMed]
- Joelson, A.M.; Geller, M.G.; Zylberberg, H.M.; Green, P.H.R.; Lebwohl, B. The Effect of Depressive Symptoms on the Association between Gluten-Free Diet Adherence and Symptoms in Celiac Disease: Analysis of a Patient Powered Research Network. Nutrients 2018, 10, 538. [Google Scholar] [CrossRef] [PubMed]
- Wolf, R.L.; Lebwohl, B.; Lee, A.R.; Zybert, P.; Reilly, N.R.; Cadenhead, J.; Amengual, C.; Green, P.H.R. Hypervigilance to a Gluten-Free Diet and Decreased Quality of Life in Teenagers and Adults with Celiac Disease. Digest. Dis. Sci. 2018, 63, 1438–1448. [Google Scholar] [CrossRef] [PubMed]
- The Cochrane Collaboration. Cochrane Handbook for Systematic Reviews of Interventions; Higgins, J., Green, S., Eds.; The Cochrane Collaboration: London, UK, 2011. [Google Scholar]
- Higgins, J.; Sterne, J.A.; Savović, J.; Page, M.; Hróbjartsson, A.; Boutron, I.; Reeves, B.C.; Eldridge, S. A revised tool for assessing risk of bias in randomized trials. Cochrane Database Syst. Rev. 2016, 10 (Suppl. S1). [Google Scholar] [CrossRef]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef] [PubMed]
- The GRADE Working Group. GRADE Handbook for Grading Quality of Evidence and Strength of Recommendations; Updated October 2013; Schünemann, H., Brożek, J., Guyatt, G., Oxman, A., Eds.; The GRADE Working Group: Hamilton, ON, Canada, 2013. [Google Scholar]
- Evidence Prime, Inc. GRADEpro GDT: GRADEpro Guideline Development Tool [Software]; McMaster University: Hamilton, ON, Canada, 2015. [Google Scholar]
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rohatgi, A. WebPlotDigitizer. Available online: https://automeris.io/WebPlotDigitizer/ (accessed on 22 October 2018).
- Kurppa, K.; Paavola, A.; Collin, P.; Sievänen, H.; Laurila, K.; Huhtala, H.; Saavalainen, P.; Mäki, M.; Kaukinen, K. Benefits of a gluten-free diet for asymptomatic patients with serologic markers of celiac disease. Gastroenterology 2014, 147, 610–617. [Google Scholar] [CrossRef] [PubMed]
- Elli, L.; Tomba, C.; Branchi, F.; Roncoroni, L.; Lombardo, V.; Bardella, M.T.; Ferretti, F.; Conte, D.; Valiante, F.; Fini, L.; et al. Evidence for the Presence of Non-Celiac Gluten Sensitivity in Patients with Functional Gastrointestinal Symptoms: Results from a Multicenter Randomized Double-Blind Placebo-Controlled Gluten Challenge. Nutrients 2016, 8. [Google Scholar] [CrossRef] [PubMed]
- Paavola, A.; Kurppa, K.; Ukkola, A.; Collin, P.; Lähdeaho, M.-L.; Huhtala, H.; Mäki, M.; Kaukinen, K. Gastrointestinal symptoms and quality of life in screen-detected celiac disease. Dig. Liver Dis. 2012, 44, 814–818. [Google Scholar] [CrossRef] [PubMed]
- Di Sabatino, A.; Volta, U.; Salvatore, C.; Biancheri, P.; Caio, G.; De Giorgio, R.; Di Stefano, M.; Corazza, G.R. Small Amounts of Gluten in Subjects With Suspected Nonceliac Gluten Sensitivity: A Randomized, Double-Blind, Placebo-Controlled, Cross-Over Trial. Clin. Gastroenterol. Hepatol. 2015, 13, 1604–1612. [Google Scholar] [CrossRef] [PubMed]
- Nachman, F.; del Campo, M.P.; González, A.; Corzo, L.; Vázquez, H.; Sfoggia, C.; Smecuol, E.; Sánchez, M.I.P.; Niveloni, S.; Sugai, E.; et al. Long-term deterioration of quality of life in adult patients with celiac disease is associated with treatment noncompliance. Dig. Liver Dis. 2010, 42, 685–691. [Google Scholar] [CrossRef] [PubMed]
- Nachman, F.; Mauriño, E.; Vázquez, H.; Sfoggia, C.; Gonzalez, A.; Gonzalez, V.; del Campo, M.P.; Smecuol, E.; Niveloni, S.; Sugai, E.; et al. Quality of life in celiac disease patients. Prospective analysis on the importance of clinical severity at diagnosis and the impact of treatment. Dig. Liver Dis. 2009, 41, 15–25. [Google Scholar] [CrossRef] [PubMed]
- Bella, R.; Lanza, G.; Cantone, M.; Giuffrida, S.; Puglisi, V.; Vinciguerra, L.; Pennisi, M.; Ricceri, R.; D’Agate, C.C.; Malaguarnera, G.; et al. Effect of a Gluten-Free Diet on Cortical Excitability in Adults with Celiac Disease. PLoS ONE 2015, 10, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Kurppa, K.; Collin, P.; Sievänen, H.; Huhtala, H.; Mäki, M.; Kaukinen, K. Gastrointestinal symptoms, quality of life and bone mineral density in mild enteropathic coeliac disease: A prospective clinical trial. Scand. J. Gastroenterol. 2010, 45, 305–314. [Google Scholar] [CrossRef] [PubMed]
- Ukkola, A.; Mäki, M.; Kurppa, K.; Collin, P.; Huhtala, H.; Kekkonen, L.; Kaukinen, K. Diet Improves Perception of Health and Well-being in Symptomatic, but Not Asymptomatic, Patients With Celiac Disease. Clin. Gastroenterol. Hepatol. 2011, 9, 118–123. [Google Scholar] [CrossRef] [PubMed]
- Vilppula, A.; Kaukinen, K.; Luostarinen, L.; Krekelä, I.; Patrikainen, H.; Valve, R.; Luostarinen, M.; Laurila, K.; Mäki, M.; Collin, P. Clinical benefit of gluten-free diet in screen-detected older celiac disease patients. BMC Gastroenterol. 2011, 11. [Google Scholar] [CrossRef] [PubMed]
- Aziz, I.; Trott, N.; Briggs, R.; North, J.R.; Hadjivassiliou, M.; Sanders, D.S. Efficacy of a Gluten-Free Diet in Subjects With Irritable Bowel Syndrome-Diarrhea Unaware of Their HLA-DQ2/8 Genotype. Clin. Gastroenterol. Hepatol. 2016, 14, 696–703. [Google Scholar] [CrossRef] [PubMed]
- Collin, P.; Kaukinen, K.; Mattila, A.K.; Joukamaa, M. Psychoneurotic symptoms and alexithymia in coeliac disease. Scand. J. Gastroenterol. 2008, 43, 1329–1333. [Google Scholar] [CrossRef] [PubMed]
- Addolorato, G.; Capristo, E.; Ghittoni, G.; Valeri, C.; Mascianà, R.; Ancona, C.; Gasbarrini, G. Anxiety but not depression decreases in coeliac patients after one-year gluten-free diet: A longitudinal study. Scand. J. Gastroenterol. 2001, 36, 502–506. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, V.; Kurppa, K.; Huhtala, H.; Mäki, M.; Kekkonen, L.; Kaukinen, K. Delayed celiac disease diagnosis predisposes to reduced quality of life and incremental use of health care services and medicines: A prospective nationwide study. United Eur. Gastroenterol. J. 2018, 6, 567–575. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peters, S.; Yelland, G.; Moore, J.; Ward, M. No effect of gluten on anxiety or depression in patients with NCGS, but could it be brain fog? J. Gastroenterol. Hepatol. 2016, 31, 175–176. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Sutton, A.J.; Ioannidis, J.P.A.; Terrin, N.; Jones, D.R.; Lau, J.; Carpenter, J.; Rücker, G.; Harbord, R.M.; Schmid, C.H.; et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 2011, 343, d4002. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis in the Behavioral Sciences, 2nd ed.; Routledge: Hillsdale, MJ, USA, 1988; ISBN 978-0-8058-0283-2. [Google Scholar]
- Admou, B.; Essaadouni, L.; Krati, K.; Zaher, K.; Sbihi, M.; Chabaa, L.; Belaabidia, B.; Alaoui-Yazidi, A. Atypical Celiac Disease: From Recognizing to Managing. Gastroenterol. Res. Pract. 2012, 2012. [Google Scholar] [CrossRef] [PubMed]
- Concerto, C.; Lanza, G.; Cantone, M.; Pennisi, M.; Giordano, D.; Spampinato, C.; Ricceri, R.; Pennisi, G.; Aguglia, E.; Bella, R. Different patterns of cortical excitability in major depression and vascular depression: A transcranial magnetic stimulation study. BMC Psychiatry 2013, 13, 300. [Google Scholar] [CrossRef] [PubMed]
- Hall, N.J.; Rubin, G.; Charnock, A. Systematic review: Adherence to a gluten-free diet in adult patients with coeliac disease. Aliment. Pharmacol. Therapeut. 2009, 30, 315–330. [Google Scholar] [CrossRef] [PubMed]
- Zysk, W.; Głąbska, D.; Guzek, D.; Zysk, W.; Głąbska, D.; Guzek, D. Social and Emotional Fears and Worries Influencing the Quality of Life of Female Celiac Disease Patients Following a Gluten-Free Diet. Nutrients 2018, 10, 1414. [Google Scholar] [CrossRef] [PubMed]
- Leonard, M.; Cureton, P.; Fasano, A.; Leonard, M.M.; Cureton, P.; Fasano, A. Indications and Use of the Gluten Contamination Elimination Diet for Patients with Non-Responsive Celiac Disease. Nutrients 2017, 9, 1129. [Google Scholar] [CrossRef] [PubMed]
- Hollon, J.R.; Cureton, P.A.; Martin, M.L.; Puppa, E.L.L.; Fasano, A. Trace gluten contamination may play a role in mucosal and clinical recovery in a subgroup of diet-adherent non-responsive celiac disease patients. BMC Gastroenterol. 2013, 13, 40. [Google Scholar] [CrossRef] [PubMed]
- Rostami, K.; Bold, J.; Parr, A.; Johnson, M.; Rostami, K.; Bold, J.; Parr, A.; Johnson, M.W. Gluten-Free Diet Indications, Safety, Quality, Labels, and Challenges. Nutrients 2017, 9, 846. [Google Scholar] [CrossRef] [PubMed]
- Roncoroni, L.; Bascuñán, K.; Doneda, L.; Scricciolo, A.; Lombardo, V.; Branchi, F.; Ferretti, F.; Dell’Osso, B.; Montanari, V.; Bardella, M.; et al. A Low FODMAP Gluten-Free Diet Improves Functional Gastrointestinal Disorders and Overall Mental Health of Celiac Disease Patients: A Randomized Controlled Trial. Nutrients 2018, 10, 1023. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.; Ling, Z.; Zhang, Y.; Mao, H.; Ma, Z.; Yin, Y.; Wang, W.; Tang, W.; Tan, Z.; Shi, J.; et al. Altered fecal microbiota composition in patients with major depressive disorder. Brain Behav. Immun. 2015, 48, 186–194. [Google Scholar] [CrossRef] [PubMed]
- Majeed, M.; Nagabhushanam, K.; Arumugam, S.; Majeed, S.; Ali, F. Bacillus coagulans MTCC 5856 for the management of major depression with irritable bowel syndrome: A randomised, double-blind, placebo controlled, multi-centre, pilot clinical study. Food Nutr. Res. 2018, 62. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Mazcorro, J.; Noratto, G.; Remes-Troche, J.; Garcia-Mazcorro, J.F.; Noratto, G.; Remes-Troche, J.M. The Effect of Gluten-Free Diet on Health and the Gut Microbiota Cannot Be Extrapolated from One Population to Others. Nutrients 2018, 10, 1421. [Google Scholar] [CrossRef] [PubMed]
- Biesiekierski, J.R.; Newnham, E.D.; Irving, P.M.; Barrett, J.S.; Haines, M.; Doecke, J.D.; Shepherd, S.J.; Muir, J.G.; Gibson, P.R. Gluten Causes Gastrointestinal Symptoms in Subjects Without Celiac Disease: A Double-Blind Randomized Placebo-Controlled Trial. Am. J. Gastroenterol. 2011, 106, 508–514. [Google Scholar] [CrossRef] [PubMed]
- Skodje, G.I.; Sarna, V.K.; Minelle, I.H.; Rolfsen, K.L.; Muir, J.G.; Gibson, P.R.; Veierød, M.B.; Henriksen, C.; Lundin, K.E.A. Fructan, Rather Than Gluten, Induces Symptoms in Patients With Self-Reported Non-Celiac Gluten Sensitivity. Gastroenterology 2018, 154, 529–539. [Google Scholar] [CrossRef] [PubMed]
- Catassi, C.; Alaedini, A.; Bojarski, C.; Bonaz, B.; Bouma, G.; Carroccio, A.; Castillejo, G.; De Magistris, L.; Dieterich, W.; Di Liberto, D.; et al. The Overlapping Area of Non-Celiac Gluten Sensitivity (NCGS) and Wheat-Sensitive Irritable Bowel Syndrome (IBS): An Update. Nutrients 2017, 9, 1268. [Google Scholar] [CrossRef] [PubMed]
- Aziz, I.; Hadjivassiliou, M.; Sanders, D.S. The spectrum of noncoeliac gluten sensitivity. Nat. Rev. Gastroenterol. Hepatol. 2015, 12, 516–526. [Google Scholar] [CrossRef] [PubMed]
- Ford, R.P.K. The gluten syndrome: A neurological disease. Med. Hypotheses 2009, 73, 438–440. [Google Scholar] [CrossRef] [PubMed]
- Morales-Muñoz, I.; Koskinen, S.; Partonen, T. Differences in clinical and cognitive variables in seasonal affective disorder compared to depressive-related disorders: Evidence from a population-based study in Finland. Eur. Psychiatry 2017, 44, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Kurppa, K.; Lauronen, O.; Collin, P.; Ukkola, A.; Laurila, K.; Huhtala, H.; Mäki, M.; Kaukinen, K. Factors Associated with Dietary Adherence in Celiac Disease: A Nationwide Study. DIG 2012, 86, 309–314. [Google Scholar] [CrossRef] [PubMed]
- Addolorato, C.; De Lorenzi, C.; Abenavoli, L.; Leccio, L.; Capristo, E.; Casbarrini, C. Psychological support counselling improves gluten-free diet compliance in coeliac patients with affective disorders. Aliment. Pharmacol. Therapeut. 2004, 20, 777–782. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fueyo-Díaz, R.; Magallón-Botaya, R.; Gascón-Santos, S.; Asensio-Martínez, Á.; Palacios-Navarro, G.; Sebastián-Domingo, J.J. Development and Validation of a Specific Self-Efficacy Scale in Adherence to a Gluten-Free Diet. Front. Psychol. 2018, 9. [Google Scholar] [CrossRef] [PubMed]
| Author (Year) | Country of Origin/Study Design | Participants | Healthy Controls | Interventions | Outcomes | Method of Measuring Adherence * | Notes |
|---|---|---|---|---|---|---|---|
| Addolorato et al. (2001) [65] | Italy Single centre BA comparison | 35 newly diagnosed classical CD patients | 59 HC recruited from hospital staff members | GFD for 1 y | Changes in depression score BA a GFD (M-SDS) Changes in no. patients positive for depression BA a GFD (M-SDS score > 49) | 1—validated 2—family member interview 3—AGA, EmA 4—biopsy at 6–8 mo | |
| Aziz et al. (2016) [63] | UK Single centre BA comparison | 41 IBS-D patients; 20 HLA-DQ2/8+ and 21 HLA-DQ2/8− | NC | GFD for 6 wk; FU at 18 mo for those who continued on GFD | Changes in HADS before and after a GFD Difference between HLA-DQ2/8+/− groups | 1—validated (“Patients scoring 0 or 1 do not follow a strict GFD. Patients scoring 2 follow a GFD but with errors necessitating correction. Finally, patients scoring three or four follow a strict GFD.”) | Educational grant from Dr. Schär (a gluten-free food manufacturer) to undertake investigator-conceived and -led research on gluten sensitivity |
| Bella et al. (2015) [59] | Italy Single centre BA comparison (FU study from Pennisi et al. (2014)) | 13 CD patients | NC | GFD for 16 mo | Changes in depression score BA a GFD (HDRS) Changes in no. patients positive for depression (dysthymia) BA a GFD (SCID-I) | 1—validated 3—EmA, tTG | |
| Collin et al. (2008) [64] | Finland Single centre BA comparison | 20 biopsy-proven CD patients | HCs not recruited from same community (female students/male workers) | GFD for 1 y | Changes in depression score BA a GFD (sub-score of CCEI/Middlesex Hospital Questionnaire) | 3—EmA 4—Vh/CrD | |
| Di Sabatino et al. (2015) [56] | Italy Multicentre DB, PC, CO RCT | 59 patients suspected of having NCGS (CD and WA excluded) | NA | 2 arms; GFD (1 wk baseline period) followed by 1 wk: (a) 4.375 g/day gluten (b) rice starch placebo with 1 wk wash-out periods inbetween | Difference in mean daily depression scores (unvalidated questionnaire) between gluten and placebo groups | 1—validated 6—unused capsules counted | |
| Kurppa et al. (2010) [60] | Finland Single centre Cohort | 73 EmA-positive adults; 27 mild enteropathy (Marsh I-II), 46 CD (Marsh III) | 110 HCs (age and gender matched) | GFD for 1 y | Changes in depression score BA a GFD (sub-score of PGWB) | 3—EmA, tTG 4—Vh/CrD | |
| Kurppa et al. (2014) [53] | Finland Multicentre DB, CO RCT | 40 asymptomatic EmA-positive adults (CD excluded) | NA | 2 arms; participants randomised to a GFD or gluten-containing diet for 1 y then cross-over | Difference in mean depression score between gluten and GFD groups at 1 y (sub-score of PGWB) | 2—NI on who conducted 3—EmA, tTG 4—Vh/CrD | Deviations from protocol: No-one in GFD group willing to restart gluten-containing diet so only data from 1 y FU used |
| Nachman et al. (2009) [58] | Argentina Single centre BA comparison/time-interrupted study | 84 newly diagnosed biopsy-proven CD patients; 62 classical, 14 atypical and 8 asymptomatic | 70 HCs recruited from hospital staff members (age and gender matched) | GFD for 1 y | At baseline, 3, 6, 9 and 12 mo: Changes in depression score BA a GFD (BDI) Changes in no. patients positive for depression BA a GFD (BDI score ≥ 18) Subgroup analysis: Compliant vs. noncompliant | Opinion of physician in charge, based on: 1—self-rated questionnaire 2—“meticulous enquiry by an experienced dietician” 3—tTG, DGP, EmA, AGA 4—Vh/CrD 5—4 day (self-reported) | |
| Nachman et al. (2010) [57] | Argentina Single centre BA comparison/FU from Nachman et al. (2009) | 53 CD patients; 37 classical and 16 atypical/asymptomatic | 70 HCs recruited from hospital staff members (age and gender matched) (same as Nachman et al. (2009)) | GFD for 4 y | At baseline, 1 y and 4 y: Changes in depression score BA a GFD (BDI) Changes in no. patients positive for depression BA a GFD (BDI score ≥ 18) Subgroup analysis: Compliant vs. noncompliant | Opinion of physician in charge, based on: 1—self-rated questionnaire 2—“meticulous enquiry by an experienced dietician” 3—tTG, DGP, EmA, AGA 4—Vh/CrD 5—4 day (self-reported) | |
| Peters et al. (2014) [42] | Australia Single centre DB, PC, CO RCT | 20 IBS patients (CD excluded by biospy); recruited from a preceding study in which subjects with self-reported NCGS were challenged with diets containing varying amounts of gluten (Biesiekierski et al., 2013) | NA | 3 arms; low-FODMAPs + GFD (3 day baseline period) followed by 3 day: (a) gluten (16 g/day) (b) whey (16 g/day) (protein control) (c) placebo with 3–14 day washout period in between | Difference in depression scores following each dietary challenge (sub-score of STPI) | 1—validated 5—3 day (self-reported) 6—unused/additional food counted | Peter R. Gibson has published two books on a diet for IBS. This study was supported by George Weston Foods as part of a partnership in an Australian Research Council Linkage Project and the National Health and Medical Research Council (NHMRC) of Australia. |
| Simsek et al. (2015) [11] | Turkey Single centre BA comparison | 24 newly diagnosed biopsy-proven paediatric CD patients; age limit 9–16 y | 25 HCs recruited from same centre; EmA-negative | GFD for 6–20 mo | Changes in depression score BA a GFD (CDI) Subgroup analysis: Compliant vs. noncompliant | 3—EmA, tTG | |
| Ukkola et al. (2011) [61] | Finland Nationwide BA comparison | 698 newly diagnosed (within 1 y) biopsy-proven CD patients; 490 classical, 62 atypical and 146 screen-detected | 110 HCs (age and gender matched) | GFD for 1 y | Changes in depression score BA a GFD (subscore of PGWB) | 1—unvalidated FU question (“strict diet” or “dietary lapses”) | |
| Vilppula et al. (2011) [62] | Finland Nationwide BA comparison | 32 screen-detected biopsy-proven CD patients; age > 50 y | 110 HCs recruited from neighbourhoods of CD patients (age and gender matched) | GFD for 1–2 y | Changes in depression score BA a GFD (subscore of PGWB) | 2—with dietician 3—tTG, EmA 4—Vh/CrD (“Diet considered strict when there were no signs of dietary transgressions upon the interview. Occasional GFD defined as a gluten intake occurring less often than once in the month.”) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Busby, E.; Bold, J.; Fellows, L.; Rostami, K. Mood Disorders and Gluten: It’s Not All in Your Mind! A Systematic Review with Meta-Analysis. Nutrients 2018, 10, 1708. https://doi.org/10.3390/nu10111708
Busby E, Bold J, Fellows L, Rostami K. Mood Disorders and Gluten: It’s Not All in Your Mind! A Systematic Review with Meta-Analysis. Nutrients. 2018; 10(11):1708. https://doi.org/10.3390/nu10111708
Chicago/Turabian StyleBusby, Eleanor, Justine Bold, Lindsey Fellows, and Kamran Rostami. 2018. "Mood Disorders and Gluten: It’s Not All in Your Mind! A Systematic Review with Meta-Analysis" Nutrients 10, no. 11: 1708. https://doi.org/10.3390/nu10111708
APA StyleBusby, E., Bold, J., Fellows, L., & Rostami, K. (2018). Mood Disorders and Gluten: It’s Not All in Your Mind! A Systematic Review with Meta-Analysis. Nutrients, 10(11), 1708. https://doi.org/10.3390/nu10111708






