Dietary Intake in Population with Metabolic Syndrome: Is the Prevalence of Inadequate Intake Influenced by Geographical Area? Cross-Sectional Analysis from PREDIMED-Plus Study
Abstract
1. Introduction
2. Materials and Methods
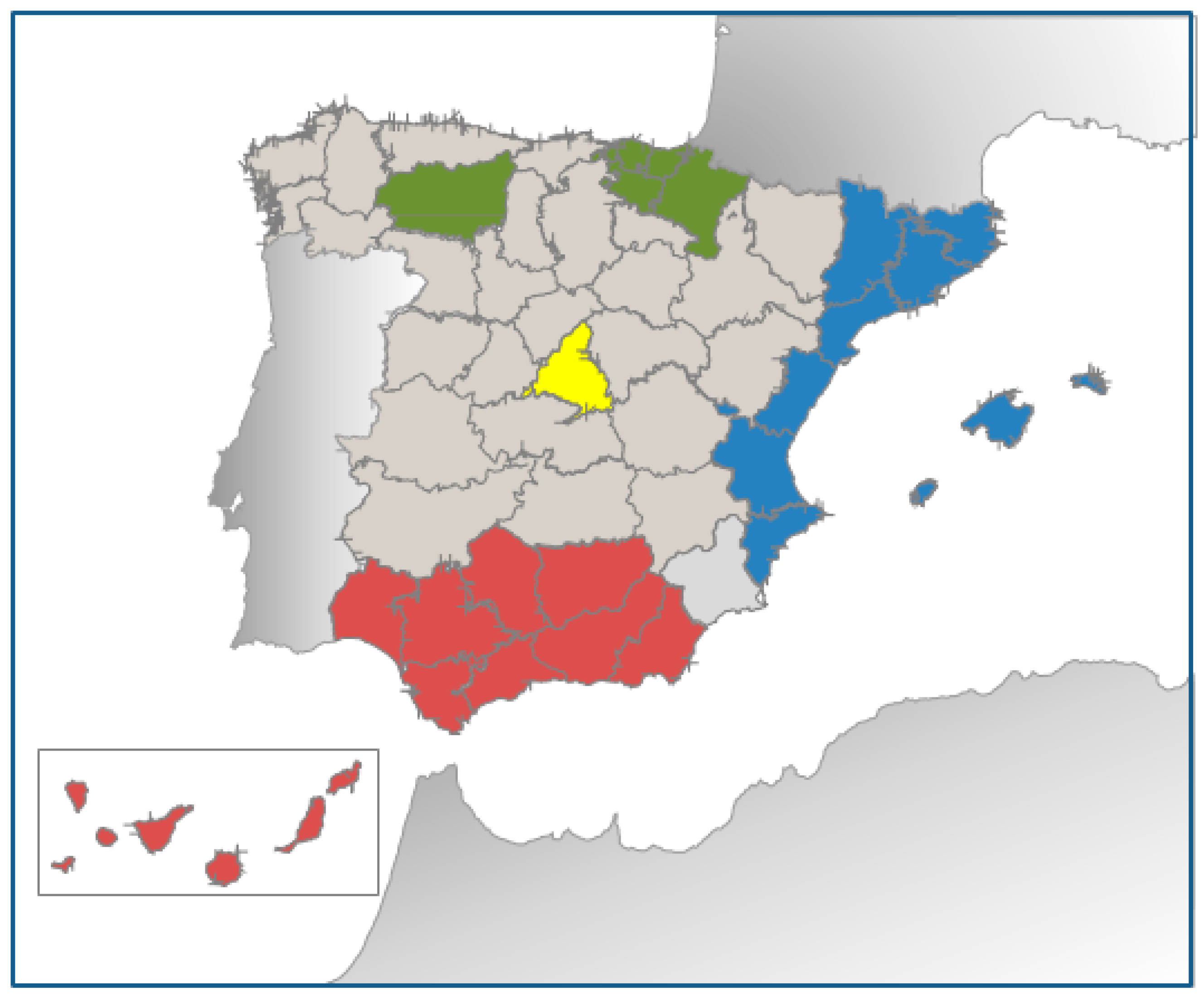
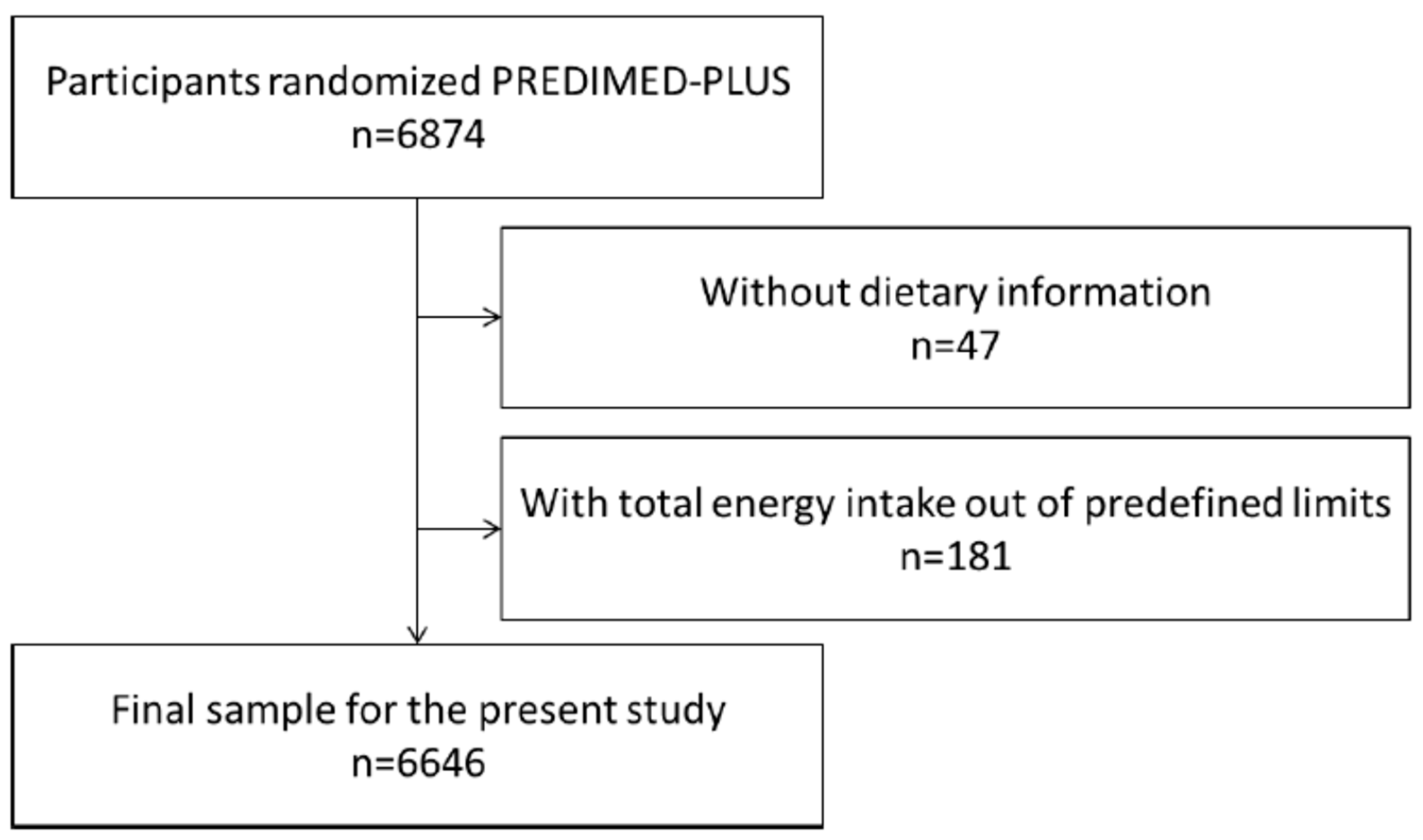
2.1. Study Design
2.2. Participants and Data Collection Procedures
2.3. Assessment of Dietary Intake
2.4. Assessment of Non-Dietary Intake
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics of the Population and Food Intake
3.2. Description of Food Intake, Adherence to MedDiet and Nutrient Profiles in the Different Geographical Areas Analysed
3.3. Evaluation of Inadequate Nutrient Intake According to Recommended Intakes
3.4. Assessment of the Influence of the Geographical Area on Inadequate Nutrient Intake
3.5. Multivariable Logistic Regression Model for Inadequate Intake of 3 or More out 6 Micronutrients According to Place of Residence
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Abarca-Gómez, L.; Abdeen, Z.A.; Hamid, Z.A.; Abu-Rmeileh, N.M.; Acosta-Cazares, B.; Acuin, C.; Adams, R.J.; Aekplakorn, W.; Afsana, K.; Aguilar-Salinas, C.A.; et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef]
- Basterra-Gortari, F.J.; Bes-Rastrollo, M.; Ruiz-Canela, M.; Gea, A.; Martinez-Gonzalez, M.Á. Prevalence of obesity and diabetes in Spanish adults 1987–2012. Med. Clin. 2017, 148, 250–256. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Rodrigo, C.; Gianzo-Citores, M.; Gil, Á.; González-Gross, M.; Ortega, R.M.; Serra-Majem, L.; Varela-Moreiras, G.; Aranceta-Bartrina, J. Lifestyle patterns and weight status in Spanish adults: The ANIBES study. Nutrients 2017, 9, 606. [Google Scholar] [CrossRef] [PubMed]
- Kimokoti, R.W.; Millen, B.E. Nutrition for the Prevention of Chronic Diseases. Med. Clin. N. Am. 2016, 100, 1185–1198. [Google Scholar] [CrossRef] [PubMed]
- Varela-Moreiras, G.; Ávila, J.M.; Cuadrado, C.; del Pozo, S.; Ruiz, E.; Moreiras, O. Evaluation of food consumption and dietary patterns in Spain by the Food Consumption Survey: Updated information. Eur. J. Clin. Nutr. 2010, 64, S37–S43. [Google Scholar] [CrossRef] [PubMed]
- Trichopoulou, A.; Corella, D.; Martínez-González, M.A.; Soriguer, F.; Ordovas, J.M. The Mediterranean diet and cardiovascular epidemiology. Nutr. Rev. 2006, 64 (Suppl. 101), S13–S19. [Google Scholar] [CrossRef]
- Dinu, M.; Pagliai, G.; Casini, A.; Sofi, F. Mediterranean diet and multiple health outcomes: An umbrella review of meta-analyses of observational studies and randomised trials. Eur. J. Clin. Nutr. 2018, 72, 30–43. [Google Scholar] [CrossRef] [PubMed]
- Knight, A.; Bryan, J.; Murphy, K. The Mediterranean diet and age-related cognitive functioning: A systematic review of study findings and neuropsychological assessment methodology. Nutr. Neurosci. 2017, 20, 449–468. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Hao, Q.; Su, L.; Liu, Y.; Liu, S.; Dong, B. Adherence to the Mediterranean Diet and the Risk of Frailty in Old People: A Systematic Review and Meta-Analysis. J. Nutr. Health Aging 2018, 22, 613–618. [Google Scholar] [CrossRef] [PubMed]
- Godos, J.; Zappalà, G.; Bernardini, S.; Giambini, I.; Bes-Rastrollo, M.; Martinez-Gonzalez, M. Adherence to the Mediterranean diet is inversely associated with metabolic syndrome occurrence: A meta-analysis of observational studies. Int. J. Food Sci. Nutr. 2017, 68, 138–148. [Google Scholar] [CrossRef] [PubMed]
- Grosso, G.; Marventano, S.; Yang, J.; Micek, A.; Pajak, A.; Scalfi, L.; Galvano, F.; Kales, S.N. A comprehensive meta-analysis on evidence of Mediterranean diet and cardiovascular disease: Are individual components equal? Crit. Rev. Food Sci. Nutr. 2017, 57, 3218–3232. [Google Scholar] [CrossRef] [PubMed]
- Martínez-González, M.A.; Salas-Salvadó, J.; Estruch, R.; Corella, D.; Fitó, M.; Ros, E. Benefits of the Mediterranean Diet: Insights from the PREDIMED Study. Prog. Cardiovasc. Dis. 2015, 58, 50–60. [Google Scholar] [CrossRef] [PubMed]
- Alberti, K.G.; International Diabetes Federation Task Force on Epidemiology and Prevention; Hational Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; International Association for the Study of Obesity. Harmonizing the metabolic syndrome: A joint interim statement of the international diabetes federation task force on epidemiology and prevention; National heart, lung, and blood institute; American heart association; World heart federation; International atherosclerosis society; And international association for the study of obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [PubMed]
- Agarwal, S.; Reider, C.; Brooks, J.R.; Fulgoni, V.L. Comparison of Prevalence of Inadequate Nutrient Intake Based on Body Weight Status of Adults in the United States: An Analysis of NHANES 2001–2008. J. Am. Coll. Nutr. 2015, 34, 126–134. [Google Scholar] [CrossRef] [PubMed]
- Martí, A.Z.; Ferrer Cascales, R.; Sánchez, J.A.H.; Pérez, A.L. Adherence to the mediterranean diet and its relation to nutritional status in older people. Nutr. Hosp. 2015, 31, 1667–1674. [Google Scholar]
- Fávaro-Moreira, N.C.; Krausch-Hofmann, S.; Matthys, C.; Vereecken, C.; Vanhauwaert, E.; Declercq, A.; Bekkering, G.E.; Duyck, J. Risk factors for malnutrition in older adults: A systematic review of the literature based on longitudinal data. Adv. Nutr. 2016, 7, 507–522. [Google Scholar] [CrossRef] [PubMed]
- Bernstein, M. Nutritional Needs of the Older Adult. Phys. Med. Rehab. Clin. N. Am. 2017, 28, 747–766. [Google Scholar] [CrossRef] [PubMed]
- Benhammou, S.; Heras-González, L.; Ibáñez-Peinado, D.; Barceló, C.; Hamdan, M.; Rivas, A.; Mariscal-Arcas, M.; Olea-Serrano, F.; Monteagudo, C. Comparison of Mediterranean diet compliance between European and non-European populations in the Mediterranean basin. Appetite 2016, 107, 521–526. [Google Scholar] [CrossRef] [PubMed]
- León-Munoz, L.M.; Guallar-Castillón, P.; Graciani, A.; López-García, E.; Mesas, A.E.; Aguilera, M.T.; Banegas, J.R.; Rodríguez-Artalejo, F. Adherence to the mediterranean diet pattern has declined in Spanish adults. J. Nutr. 2012, 142, 1843–1850. [Google Scholar] [CrossRef] [PubMed]
- Abellán Alemán, J.; Zafrilla Rentero, M.P.; Montoro-García, S.; Mulero, J.; Pérez Garrido, A.; Leal, M.; Guerrero, L.; Ramos, E.; Ruilope, L.M. Adherence to the “Mediterranean diet” in Spain and its relationship with cardiovascular risk (DIMERICA study). Nutrients 2016, 8, 680. [Google Scholar] [CrossRef] [PubMed]
- Katsarou, A.; Tyrovolas, S.; Psaltopoulou, T.; Zeimbekis, A.; Tsakountakis, N.; Bountziouka, V.; Gotsis, E.; Metallinos, G.; Polychronopoulos, E.; Lionis, C.; et al. Socio-economic status, place of residence and dietary habits among the elderly: The Mediterranean islands study. Public Health Nutr. 2010, 13, 1614–1621. [Google Scholar] [CrossRef] [PubMed]
- Samaniego-Vaesken, M.D.; Partearroyo, T.; Ruiz, E.; Aranceta-Bartrina, J.; Gil, Á.; González-Gross, M.; Ortega, R.M.; Serra-Majem, L.; Varela-Moreiras, G. The influence of place of residence, gender and age influence on food group choices in the Spanish population: Findings from the ANIBES study. Nutrients 2018, 10, 392. [Google Scholar] [CrossRef] [PubMed]
- Bertomeu, V.; Castillo-Castillo, J. Cardiovascular disease in Spain today. From risk factors to morbidity. Rev. Esp. Cardiol. Supl. 2008, 8, 2E–9E. [Google Scholar]
- Martínez-González, M.Á.; Corella, D.; Salas-Salvadó, J.; Ros, E.; Covas, M.I.; Fiol, M.; Wärnberg, J.; Arós, F.; Ruíz-Gutiérrez, V.; Lamuela-Raventós, R.M.; et al. Cohort Profile: Design and methods of the PREDIMED study. Int. J. Epidemiol. 2018, 41, 377–385. [Google Scholar] [CrossRef] [PubMed]
- Willet, W. Nutritional Epidemiology, 3rd ed.; Oxford University Press: New York, NY, USA, 2013. [Google Scholar]
- Martin-moreno, J.M.; Boyle, P.; Gorgojo, L.; Maisonneuve, P.; Fernandez-rodriguez, J.C.; Salvini, S.; Willett, W.C. Development and validation of a food frequency questionnaire in Spain. Int. J. Epidemiol. 1993, 22, 512–519. [Google Scholar] [CrossRef] [PubMed]
- De La Fuente-Arrillaga, C.; Vzquez Ruiz, Z.; Bes-Rastrollo, M.; Sampson, L.; Martinez-González, M.A. Reproducibility of an FFQ validated in Spain. Public Health Nutr. 2010, 13, 1364–1372. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Ballart, J.D.; Piñol, J.L.; Zazpe, I.; Corella, D.; Carrasco, P.; Toledo, E.; Perez-Bauer, M.; Martínez-González, M.Á.; Salas-Salvadó, J.; Martín-Moreno, J.M. Relative validity of a semi-quantitative food-frequency questionnaire in an elderly Mediterranean population of Spain. Br. J. Nutr. 2010, 103, 1808–1816. [Google Scholar] [CrossRef] [PubMed]
- Moreiras, O.C.A.; Cabrera, L.; Cuadrado, C. Tablas de Composición de Alimentos; (Spanish Food Composition Tables); Pirámide: Madrid, Spain, 2003. [Google Scholar]
- Mataix-Verdú, J.; García Diz, L.; Mañas Almendros, M.; Emilio, M.d.V.; Llopis González, J. Tablas de Composición de Alimentos, 4th ed.; Universidad de Granada: Granada, Spain, 2009. [Google Scholar]
- Schröder, H.; Fitó, M.; Estruch, R.; Martínez-González, M.A.; Corella, D.; Salas-Salvadó, J.; Lamuela-Raventós, R.; Ros, E.; Salaverría, I.; Fiol, M.; et al. A Short Screener Is Valid for Assessing Mediterranean Diet Adherence among Older Spanish Men and Women. J. Nutr. 2011, 141, 1140–1145. [Google Scholar] [CrossRef] [PubMed]
- IOM. Nutrient Recommendations: Dietary Reference Intakes. Available online: https://www.ncbi.nlm.nih.gov/books/NBK56068/table/summarytables.t2/?report=objectonly (accessed on 10 May 2018).
- Health NIo. Nutrient Recommendations: Dietary Reference Intakes (DRI) 2018. Available online: https://ods.od.nih.gov/Health_Information/Dietary_Reference_Intakes.aspx (accessed on 10 May 2018).
- Ortiz-Andrellucchi, A.; Sánchez-Villegas, A.; Doreste-Alonso, J.; de Vries, J.; de Groot, L.; Serra-Majem, L. Dietary assessment methods for micronutrient intake in elderly people: A systematic review. Br. J. Nutr. 2009, 102 (Suppl. 1), S118–S149. [Google Scholar] [CrossRef] [PubMed]
- EFSA. Dietary Reference Values and Dietary Guidelines. Available online: https://www.efsa.europa.eu/en/topics/topic/dietary-reference-values (accessed on 26 September 2018).
- Elosua, R.; Marrugat, J.; Molina, L.; Pons, S.; Pujol, E. Validation of the minnesota leisure time physical activity questionnaire in Spanish men. Am. J. Epidemiol. 1994, 139, 1197–1209. [Google Scholar] [CrossRef] [PubMed]
- Elosua, R.; Garcia, M.; Aguilar, A.; Molina, L.; Covas, M.I.; Marrugat, J. Validation of the Minnesota leisure time physical activity questionnaire in Spanish women. Med. Sci. Sports Exerc. 2000, 32, 1431–1437. [Google Scholar] [CrossRef] [PubMed]
- Martínez-González, M.Á.; Hershey, M.S.; Zazpe, I.; Trichopoulou, A. Transferability of the Mediterranean diet to non-Mediterranean countries. What is and what is not the Mediterranean diet. Nutrients 2017, 9, 1226. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, E.; Ávila, J.M.; Valero, T.; del Pozo, S.; Rodriguez, P.; Aranceta-Bartrina, J.; Gil, Á.; González-Gross, M.; Ortega, R.M.; Serra-Majem, L.; et al. Energy intake, profile, and dietary sources in the spanish population: Findings of the ANIBES study. Nutrients 2015, 7, 4739–4762. [Google Scholar] [CrossRef] [PubMed]
- Varela-Moreiras, G.; Ruiz, E.; Valero, T.; Ávila, J.M.; del Pozo, S. The Spanish diet: An update. Nutr. Hosp. 2013, 28 (Suppl. 5), 13–20. [Google Scholar] [PubMed]
- Aranceta, J.B.; Arija, V.V.; Maíz, E.A.; Martínez, E.D.; Ortega, R.A.; Pérez-Rodrigo, C.; Quiles, J.I.; Rodríguez, A.M.; Román, B.V.; Salvador, G.C.; et al. Dietary Guidelines for the Spanish population (SENC, diciembre 2016); the new graphic icon of healthy food. Nutr. Hosp. 2016, 33, 1–48. [Google Scholar]
- Vazquez-Ruiz, Z.; de la Fuente-Arrillaga, C.; Bes-Rastrollo, M.; Zazpe, I.; Santiago, S.; Razquin, C.; Toledo, E.; Martinez-Gonzalez, M.Á. Egg consumption and dyslipidemia in a mediterranean cohort. Nutr. Hosp. 2018, 35, 153–161. [Google Scholar] [PubMed]
- Beydoun, M.A.; Fanelli-Kuczmarski, M.T.; Allen, A.; Beydoun, H.A.; Popkin, B.M.; Evans, M.K.; Zonderman, A.B. Monetary value of diet is associated with dietary quality and nutrient adequacy among urban adults, differentially by sex, race and poverty status. PLoS ONE 2015, 10, e0140905. [Google Scholar] [CrossRef] [PubMed]
- Oconnor, L.; Walton, J.; Flynn, A. Dietary energy density: Estimates, trends and dietary determinants for a nationally representative sample of the Irish population (aged 5–90 years). Br. J. Nutr. 2015, 113, 172–180. [Google Scholar] [CrossRef] [PubMed]
- Schuh, D.S.; Pellanda, L.C.; Guessous, I.; Marques-Vidal, P. Trends and determinants of change in compliance to dietary guidelines in a Swiss community-dwelling sample. Prev. Med. 2018, 111, 198–203. [Google Scholar] [CrossRef] [PubMed]
- Bonaccio, M.; Bes-Rastrollo, M.; de Gaetano, G.; Iacoviello, L. Challenges to the Mediterranean diet at a time of economic crisis. Nutr. Metab. Cardiovasc. Dis. 2016, 26, 1057–1063. [Google Scholar] [CrossRef] [PubMed]
- Zazpe, I.; Sanchez-Tainta, A.; Estruch, R.; Lamuela-Raventos, R.M.; Schröder, H.; Salas-Salvado, J.; Corella, D.; Fiol, M.; Gomez-Gracia, E.; Aros, F.; et al. A Large Randomized Individual and Group Intervention Conducted by Registered Dietitians Increased Adherence to Mediterranean-Type Diets: The PREDIMED Study. J. Am. Diet. Assoc. 2008, 108, 1134–1144. [Google Scholar] [CrossRef] [PubMed]
- Jurado, D.; Burgos-Garrido, E.; Diaz, F.J.; Martínez-Ortega, J.M.; Gurpegui, M. Adherence to the Mediterranean Dietary Pattern and Personality in Patients Attending a Primary Health Center. J. Acad. Nutr. Diet. 2012, 112, 887–891. [Google Scholar] [CrossRef] [PubMed]
- Patino-Alonso, M.C.; Recio-Rodríguez, J.I.; Belio, J.F.; Colominas-Garrido, R.; Lema-Bartolomé, J.; Arranz, A.G.; Agudo-Conde, C.; Gomez-Marcos, M.A.; García-Ortiz, L.; EVIDENT Group. Factors associated with adherence to the mediterranean diet in the adult population. J. Acad. Nutr. Diet. 2014, 114, 583–589. [Google Scholar] [CrossRef] [PubMed]
- Dietary Reference Intakes. Dietary Reference Intakes: Applications in Dietary Assessment; National Academy Press: Washington, DC, USA, 2000. [Google Scholar]
- Ruiz, E.; Ávila, J.M.; Valero, T.; del Pozo, S.; Rodriguez, P.; Aranceta-Bartrina, J.; Gil, Á.; González-Gross, M.; Ortega, R.M.; Serra-Majem, L.; et al. Macronutrient distribution and dietary sources in the spanish population: Findings from the ANIBES study. Nutrients 2016, 8, 177. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Tainta, A.; Zazpe, I.; Bes-Rastrollo, M.; Salas-Salvadó, J.; Bullo, M.; Sorlí, J.V.; Corella, D.; Covas, M.I.; Arós, F.; Gutierrez-Bedmar, M.; et al. Nutritional adequacy according to carbohydrates fat quality. Eur. J. Nutr. 2016, 55, 93–106. [Google Scholar] [CrossRef] [PubMed]
- Guasch-Ferré, M.; Babio, N.; Martínez-González, M.A.; Corella, D.; Ros, E.; Martín-Peláez, S.; Estruch, R.; Arós, F.; Gómez-Gracia, E.; Fiol, M.; et al. Dietary fat intake risk of cardiovascular disease all-cause mortality in a population at high risk of cardiovascular disease. Am. J. Clin. Nutr. 2015, 102, 1563–1573. [Google Scholar] [PubMed]
- Naska, A.; Trichopoulou, A. Back to the future: The Mediterranean diet paradigm. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 216–219. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, E.; Miller, M.; Yaxley, A.; Isenring, E. Malnutrition in the elderly: A narrative review. Maturitas 2013, 76, 296–302. [Google Scholar] [CrossRef] [PubMed]
- ter Borg, S.; Verlaan, S.; Hemsworth, J.; Mijnarends, D.M.; Schols, J.M.; Luiking, Y.C.; de Groot, L.C. Micronutrient intakes and potential inadequacies of community-dwelling older adults: A systematic review. Br. J. Nutr. 2015, 113, 1195–1206. [Google Scholar] [CrossRef] [PubMed]
- Roussel, A.M. Micronutrient deficiencies in obesity: Metabolic and clinical consequences. Nutr. Clin. Metab. 2017, 31, 268–275. [Google Scholar] [CrossRef]
- Hallkvist, O.M.; Johansson, J.; Nordström, A.; Nordström, P.; Hult, A. Dairy product intake and bone properties in 70-year-old men and women. Arch. Osteoporos. 2018, 13, 9. [Google Scholar] [CrossRef] [PubMed]
- Shatenstein, B.; Gauvin, L.; Keller, H.; Richard, L.; Gaudreau, P.; Giroux, F.; Gray-Donald, K.; Jabbour, M.; Morais, J.A.; Payette, H. Baseline determinants of global diet quality in older men and women from the NuAge cohort. J. Nutr. Health Aging 2013, 17, 419–425. [Google Scholar] [CrossRef] [PubMed]
- Newby, P.K.; Noel, S.E.; Grant, R.; Judd, S.; Shikany, J.M.; Ard, J. Race and region have independent and synergistic effects on dietary intakes in black and white women. Nutr. J. 2012, 11, 25. [Google Scholar] [CrossRef] [PubMed]
- Sales, C.H.; Fontanelli, M.D.M.; Vieira, D.A.S.; Marchioni, D.M.; Fisberg, R.M. Inadequate dietary intake of minerals: Prevalence and association with socio-demographic and lifestyle factors. Br. J. Nutr. 2017, 117, 267–277. [Google Scholar] [CrossRef] [PubMed]
- de Souza Fernandes, D.P.; Duarte, M.S.L.; Pessoa, M.C.; Franceschini, S.D.C.C.; Ribeiro, A.Q. Evaluation of diet quality of the elderly and associated factors. Arch. Gerontol. Geriatr. 2017, 72, 174–180. [Google Scholar] [CrossRef] [PubMed]
- Mercille, G.; Richard, L.; Gauvin, L.; Kestens, Y.; Shatenstein, B.; Daniel, M.; Payette, H. The food environment and diet quality of urban-dwelling older women and men: Assessing the moderating role of diet knowledge. Can. J. Public Health 2016, 107, 5309. [Google Scholar] [CrossRef] [PubMed]
- Mendonça, N.; Hill, T.R.; Granic, A.; Davies, K.; Collerton, J.; Mathers, J.C.; Siervo, M.; Wrieden, W.L.; Seal, C.J.; Kirkwood, T.B.; et al. Micronutrient intake and food sources in the very old: Analysis of the Newcastle 85+ Study. Br. J. Nutr. 2016, 116, 751–761. [Google Scholar] [CrossRef] [PubMed]
- Schoufour, J.D.; de Jonge, E.A.; Kiefte-de Jong, J.C.; van Lenthe, F.J.; Hofman, A.; Nunn, S.P.; Franco, O.H. Socio-economic indicators and diet quality in an older population. Maturitas 2018, 107, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Arbucias, J.S. The evolution of internal migration in Spain: An assessment of available demographic sources. Papers 2011, 96, 853–881. [Google Scholar]
- (INE) INE. Estadística de Variaciones Regionales en España. Variaciones Residenciales Interiores. Serie 1998–2017. Available online: https://www.ine.es/dynt3/inebase/es/index.htm?type=pcaxis&path=/t20/p307/serie&file=pcaxis&dh=0&capsel=02018 (accessed on 11 October 2018).
| Total Population (n = 6646) | North Area (n = 1436) | Central Area (n = 493) | East Area (n = 2938) | South Area (n = 1779) | p Value | |
|---|---|---|---|---|---|---|
| Sex, n (%) | ||||||
| Male | 3431 (51.6) | 823 (57.3) | 264 (53.6) | 1478 (50.3) | 866 (48.7) | <0.001 |
| Female | 3215 (48.4) | 613 (42.7) | 229 (46.5) | 1460 (49.7) | 913 (51.3) | |
| Age, n (%) | ||||||
| 55–70 years | 5673 (85.4) | 1203 (83.8) | 444 (90.0) | 2478 (84.3) | 1548 (87.0) | <0.001 |
| >70 years | 973 (14.6) | 233 (16.2) | 49 (9.9) | 460 (15.7) | 231 (13.0) | |
| Mean ± SD | 65.0 ± 4.9 | 65.2 ± 5.0 | 64.1 ± 4.9 | 65.2 ± 4.9 | 64.6 ± 4.8 | <0.001 |
| Smoking habits, n (%) | ||||||
| Current smoker | 825 (12.4) | 180 (12.5) | 53 (10.8) | 357 (12.2) | 235 (13.2) | <0.001 |
| Former smoker | 2883 (43.4) | 690 (48.3) | 256 (51.9) | 1251 (42.6) | 683 (38.4) | |
| Never smoker | 2910 (43.8) | 555 (38.7) | 180 (36.5) | 1325 (45.1) | 850 (47.8) | |
| Insufficient data | 28 (0.4) | 8 (0.6) | 4 (0.8) | 5 (0.2) | 11 (0.6) | |
| Diabetes mellitus, n (%) | 1818 (27.4) | 349 (24.3) | 125 (25.4) | 846 (28.8) | 498 (28.0) | 0.001 |
| Physical Activity, n (%) | ||||||
| Less active | 3961 (59.8) | 712 (49.8) | 350 (71.4) | 1720 (58.6) | 1179 (66.7) | <0.001 |
| Moderately active | 1249 (18.9) | 261 (18.3) | 71 (14.5) | 584 (19.9) | 333 (18.8) | |
| Active | 1412 (21.3) | 457 (32.0) | 69 (14.1) | 629 (21.5) | 257 (14.5) | |
| Education level, n (%) | ||||||
| Tertiary | 1463 (22.0) | 305 (21.2) | 181 (37.0) | 654 (22.3) | 323 (18.2) | <0.001 |
| Secondary | 1912 (28.8) | 443 (30.9) | 184 (37.6) | 827 (28.2) | 458 (25.7) | |
| Primary | 3207 (48.3) | 674 (46.9) | 121 (24.7) | 1436 (48.9) | 976 (54.9) | |
| Insufficient data | 60 (0.9) | 14 (1.0) | 3 (0.6) | 21 (0.7) | 22 (1.2) | |
| Civil status, n (%) | ||||||
| Married | 5072 (76.6) | 1109 (77.9) | 351 (72.1) | 2240 (76.5) | 1372 (77.1) | <0.001 |
| Widowed | 690 (10.4) | 150 (10.5) | 38 (7.8) | 313 (10.7) | 189 (10.2) | |
| Divorced/Separated | 519 (7.8) | 82 (5.8) | 53 (10.9) | 244 (8.3) | 140 (7.9) | |
| Others a | 339 (5.1) | 83 (5.8) | 45 (9.2) | 133 (4.5) | 78 (4.4) | |
| Living alone, n (%) | 826 (12.5) | 180 (12.6) | 77 (15.7) | 365 (12.4) | 204 (11.5) | 0.100 |
| Diabetic, n (%) | 1818 (27.4) | 349 (24.3) | 125 (25.4) | 846 (28.8) | 498 (28.0) | 0.001 |
| North Area | Central Area | East Area | South Area | p Value | |||||
|---|---|---|---|---|---|---|---|---|---|
| n | (n = 1436) | (n = 493) | (n = 2938) | (n = 1779) | |||||
| Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | ||
| Food group intake | |||||||||
| Vegetables (g/day) | 291.1 | 284.1–298.2 | 327.8 | 315.1–340.5 | 335.8 | 330.8–34.7 | 331.5 | 325.1–337.9 | <0.001 |
| Fruits (g/day) | 389.6 | 380.0–400.1 | 366.0 | 347.0–385.0 | 332.5 | 325.1–339.8 | 366.9 | 357.4–376.5 | 0.001 |
| Legumes (g/day) | 18.8 | 18.2–19.4 | 20.6 | 19.6–21.7 | 19.7 | 19.3–20.1 | 23.2 | 22.7–23.8 | <0.001 |
| Cereals (g/day) | 173.4 | 169.4–177.4 | 150.2 | 143.0–157.3 | 142.8 | 140.0–145.5 | 143.8 | 140.2–147.4 | <0.001 |
| Milk/dairy products (g/day) | 367.0 | 356.6–377.3 | 387.3 | 368.7–405.9 | 320.8 | 313.6–328.1 | 357.9 | 348.6–367.3 | <0.001 |
| Meat/meat products (g/day) | 150.8 | 147.9–153.7 | 143.6 | 138.4–148.8 | 155.4 | 153.4–157.5 | 125.7 | 123.1–128.3 | <0.001 |
| Olive oil (g/day) | 42.9 | 42.0–43.8 | 35.9 | 34.4–37.5 | 40.6 | 40.0–41.2 | 37.0 | 36.2–37.8 | <0.001 |
| Fish/seafood (g/day) | 95.7 | 93.3–98.1 | 109.8 | 105.4–114.1 | 102.5 | 100.9–104.2 | 99.5 | 97.3–101.7 | <0.001 |
| Nuts (g/day) | 12.9 | 12.–13.8 | 16.3 | 14.7–17.9 | 15.0 | 14.4–15.6 | 15.5 | 14.7–16.3 | <0.001 |
| Sugar/sweets (g/day) | 32.6 | 31.1–34.2 | 29.5 | 26.7–32.2 | 25.5 | 24.5–26.6 | 23.2 | 21.8–24.6 | <0.001 |
| Eggs (g/day) | 25.9 | 25.3–26.5 | 24.1 | 23.0–25.2 | 22.6 | 22.1–23.0 | 23.0 | 22.5–23.6 | <0.001 |
| Adherence to MedDiet | |||||||||
| MedDiet Q-P17 a, mean | 8.6 | 8.4–8.7 | 9.2 | 9.0–9.5 | 8.1 | 8.0–8.2 | 8.9 | 8.8–9.0 | <0.001 |
| Energy intake and nutrient profiles, mean | |||||||||
| Total energy intake (kcal/day) | 2425.0 | 2397.6–2452.3 | 2398.8 | 2349.7–2447.9 | 2357.6 | 2338.5–2376.6 | 2301.0 | 2276.3–2325.7 | <0.001 |
| Total fat intake (%) | 38.3 | 38.0–38.6 | 38.5 | 37.9–39.1 | 40.4 | 40.1–40.6 | 39.0 | 38.7–39.3 | <0.001 |
| Monounsaturated fat (%) | 19.9 | 19.7–20.2 | 19.5 | 19.1–19.9 | 21.0 | 20.8–21.1 | 20.3 | 20.1–20.5 | <0.001 |
| Polyunsaturated fat (%) | 6.1 | 6.0–6.2 | 6.3 | 6.1–6.5 | 6.4 | 6.3–6.4 | 6.5 | 6.4–6.6 | <0.001 |
| Saturate fat (%) | 9.5 | 9.4–9.6 | 10.1 | 9.9–10.2 | 10.3 | 10.2–10.3 | 9.6 | 9.5–9.6 | <0.001 |
| Carbohydrate intake (%) | 41.8 | 41.1–42.1 | 41.6 | 41.0–42.3 | 39.8 | 39.6–40.1 | 41.8 | 41.5–42.1 | <0.001 |
| Protein intake (%) | 16.3 | 16.1–16.4 | 17.0 | 16.7–17.2 | 16.8 | 16.7–16.9 | 16.4 | 16.3–16.5 | <0.001 |
| Alcohol intake (g/day) | 13.5 | 12.8–14.2 | 10.4 | 9.1–11.6 | 10.6 | 10.1–11.1 | 9.7 | 9.1–10.4 | <0.001 |
| Fibre intake (g/day) | 25.8 | 25.4–26.3 | 26.4 | 25.6–27.3 | 25.8 | 25.4–26.1 | 26.2 | 25.8–26.6 | 0.191 |
| Nutrient | Group | DRI a | North Area | Central Area | East Area | South Area | p Value 1 |
|---|---|---|---|---|---|---|---|
| Dietary fibre | Male 55–70 | 30 g/day | 28.1 | 28.4 | 27.0 | 29.2 | 0.744 |
| Male >70 | 30 g/day | 19.4 | 27.8 | 24.0 | 29.4 | 0.442 | |
| Female 60–70 | 21 g/day | 2.3 | 4.6 | 4.1 | 4.0 | 0.310 | |
| Female >70 | 21 g/day | 3.7 | 6.9 | 5.6 | 2.2 | 0.383 | |
| p value 2 | <0.001 | <0.001 | <0.001 | <0.001 | |||
| Vitamin A | Male 55–70 | 900 µg/day | 28.8 | 21.2 | 15.8 | 16.6 | <0.001 |
| Male >70 | 900 µg/day | 25.5 | 16.7 | 17.3 | 17.4 | 0.353 | |
| Female 60–70 | 700 µg/day | 8.6 | 5.8 | 5.6 | 5.2 | 0.078 | |
| Female >70 | 700 µg/day | 8.2 | 6.9 | 10.4 | 5.1 | 0.341 | |
| p value 2 | <0.001 | <0.001 | <0.001 | <0.001 | |||
| Vitamin B9 | Male 60–70 | 400 µg/day | 19.3 | 18.5 | 22.2 | 22.6 | 0.250 |
| Male >70 | 400 µg/day | 17.4 | 22.2 | 18.8 | 23.9 | 0.667 | |
| Female 55–70 | 400 µg/day | 15.7 | 17.3 | 17.4 | 20.2 | 0.204 | |
| Female >70 | 400 µg/day | 11.9 | 24.1 | 21.9 | 21.0 | 0.092 | |
| p value 2 | 0.128 | 0.819 | 0.020 | 0.649 | |||
| Vitamin D | Male 60–70 | 15 µg/day | 89.0 | 75.7 | 83.6 | 83.0 | <0.001 |
| Male >70 | 20 µg/day | 99.0 | 100.0 | 97.6 | 97.8 | 0.786 | |
| Female 55–70 | 15 µg/day | 87.9 | 77.5 | 82.0 | 85.0 | 0.002 | |
| Female >70 | 20 µg/day | 98.5 | 93.1 | 97.2 | 100.0 | 0.061 | |
| p value 2 | <0.001 | 0.021 | <0.001 | <0.001 | |||
| Vitamin E | Male 55–70 | 15 mg/day | 63.7 | 52.3 | 43.3 | 43.6 | <0.001 |
| Male >70 | 15 mg/day | 56.1 | 50.0 | 44.7 | 54.4 | 0.214 | |
| Female 60–70 | 15 mg/day | 63.1 | 48.6 | 49.0 | 50.4 | <0.001 | |
| Female >70 | 15 mg/day | 70.2 | 44.8 | 61.8 | 61.6 | 0.062 | |
| p value 2 | 0.178 | 0.826 | <0.001 | <0.001 | |||
| Calcium | Male 55–70 | 1000 mg/day | 14.2 | 8.6 | 11.7 | 13.5 | 0.090 |
| Male >70 | 1200 mg/day | 22.5 | 11.1 | 30.8 | 30.4 | 0.163 | |
| Female 60–70 | 1200 mg/day | 25.3 | 19.7 | 26.7 | 25.7 | 0.268 | |
| Female >70 | 1200 mg/day | 21.6 | 27.6 | 24.3 | 28.3 | 0.625 | |
| p value 2 | <0.001 | 0.002 | <0.001 | <0.001 | |||
| Magnesium | Male 55–70 | 420 mg/day | 10.2 | 8.1 | 7.6 | 7.7 | 0.206 |
| Male >70 | 420 mg/day | 12.2 | 5.6 | 8.7 | 9.8 | 0.718 | |
| Female 60–70 | 320 mg/day | 1.0 | 1.7 | 1.2 | 1.5 | 0.846 | |
| Female >70 | 320 mg/day | 1.5 | 3.5 | 1.2 | 1.5 | 0.819 | |
| p value 2 | <0.001 | 0.042 | <0.001 | <0.001 |
| Nutrient | North Area | Central Area | East Area | South Area | |
|---|---|---|---|---|---|
| Dietary fibre | Model 1 | 1 (Ref.) | 1.08 (0.81−1.43) | 0.92 (0.78−1.10) | 0.97 (0.80−1.17) |
| Model 2 | 1 (Ref.) | 1.03 (0.72−1.46) | 0.80 (0.65−0.98) | 0.92 (0.73−1.15) | |
| Vitamin A | Model 1 | 1 (Ref.) | 0.66 (0.49−0.89) | 0.51 (0.43−0.61) | 0.49 (0.40−0.59) |
| Model 2 | 1 (Ref.) | 0.57 (0.41−0.80) | 0.43 (0.35−0.52) | 0.40 (0.32−0.50) | |
| Vitamin B9 | Model 1 | 1 (Ref.) | 1.09 (0.83−1.44) | 1.19 (1.01−1.41) | 1.31 (1.10−1.57) |
| Model 2 | 1 (Ref.) | 0.98 (0.70−1.36) | 0.97 (0.80−1.17) | 1.09 (0.88−1.34) | |
| Vitamin E | Model 1 | 1 (Ref.) | 0.58 (0.47−0.72) | 0.52 (0.45−0.59) | 0.54 (0.47−0.62) |
| Model 2 | 1 (Ref.) | 0.47 (0.36−0.61) | 0.30 (0.26−0.35) | 0.30 (0.25−0.36) | |
| Calcium | Model 1 | 1 (Ref.) | 0.70 (0.52−0.94) | 1.07 (0.91−1.26) | 1.11 (0.93−1.32) |
| Model 2 | 1 (Ref.) | 0.53 (0.38−0.76) | 0.86 (0.72−1.04) | 0.80 (0.65−0.98) | |
| Magnesium | Model 1 | 1 (Ref.) | 0.80 (0.50−1.28) | 0.68 (0.52−0.89) | 0.70 (0.51−0.95) |
| Model 2 | 1 (Ref.) | 0.39 (0.21−0.75) | 0.35 (0.25−0.50) | 0.33 (0.22−0.49) |
| ≥3 Inadequate Intake % Prevalence (95% CI) | Adjusted Odds Ratio (95% CI) | pValue | |
| Geographical area | |||
| North area | 19.0 (17.0–21.1) | 1 (Ref.) | |
| Central area | 16.3 (12.8–19.7) | 0.65 (0.46–0.94) | 0.021 |
| East area | 15.9 (14.6–17.2) | 0.57 (0.47–0.70) | <0.001 |
| South area | 16.8 (15.0–18.5) | 0.59 (0.47–0.74) | <0.001 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cano-Ibáñez, N.; Bueno-Cavanillas, A.; Martínez-González, M.A.; Corella, D.; Salas-Salvadó, J.; Zomeño, M.D.; García-de-la-Hera, M.; Romaguera, D.; Martínez, J.A.; Barón-López, F.J.; et al. Dietary Intake in Population with Metabolic Syndrome: Is the Prevalence of Inadequate Intake Influenced by Geographical Area? Cross-Sectional Analysis from PREDIMED-Plus Study. Nutrients 2018, 10, 1661. https://doi.org/10.3390/nu10111661
Cano-Ibáñez N, Bueno-Cavanillas A, Martínez-González MA, Corella D, Salas-Salvadó J, Zomeño MD, García-de-la-Hera M, Romaguera D, Martínez JA, Barón-López FJ, et al. Dietary Intake in Population with Metabolic Syndrome: Is the Prevalence of Inadequate Intake Influenced by Geographical Area? Cross-Sectional Analysis from PREDIMED-Plus Study. Nutrients. 2018; 10(11):1661. https://doi.org/10.3390/nu10111661
Chicago/Turabian StyleCano-Ibáñez, Naomi, Aurora Bueno-Cavanillas, Miguel A. Martínez-González, Dolores Corella, Jordi Salas-Salvadó, M. Dolors Zomeño, Manoli García-de-la-Hera, Dora Romaguera, J. Alfredo Martínez, F. Javier Barón-López, and et al. 2018. "Dietary Intake in Population with Metabolic Syndrome: Is the Prevalence of Inadequate Intake Influenced by Geographical Area? Cross-Sectional Analysis from PREDIMED-Plus Study" Nutrients 10, no. 11: 1661. https://doi.org/10.3390/nu10111661
APA StyleCano-Ibáñez, N., Bueno-Cavanillas, A., Martínez-González, M. A., Corella, D., Salas-Salvadó, J., Zomeño, M. D., García-de-la-Hera, M., Romaguera, D., Martínez, J. A., Barón-López, F. J., García-Ríos, A., Estruch, R., García-Molina, L., Alonso Gómez, Á., Tur, J. A., Tinahones, F., Serra-Majem, L., Cubelos-Fernández, N., Lapetra, J., ... Gea, A. (2018). Dietary Intake in Population with Metabolic Syndrome: Is the Prevalence of Inadequate Intake Influenced by Geographical Area? Cross-Sectional Analysis from PREDIMED-Plus Study. Nutrients, 10(11), 1661. https://doi.org/10.3390/nu10111661













