Changes in Sport Nutrition Knowledge, Attitudes/Beliefs and Behaviors Following a Two-Year Sport Nutrition Education and Life-Skills Intervention among High School Soccer Players
Abstract
1. Introduction
2. Materials and Methods
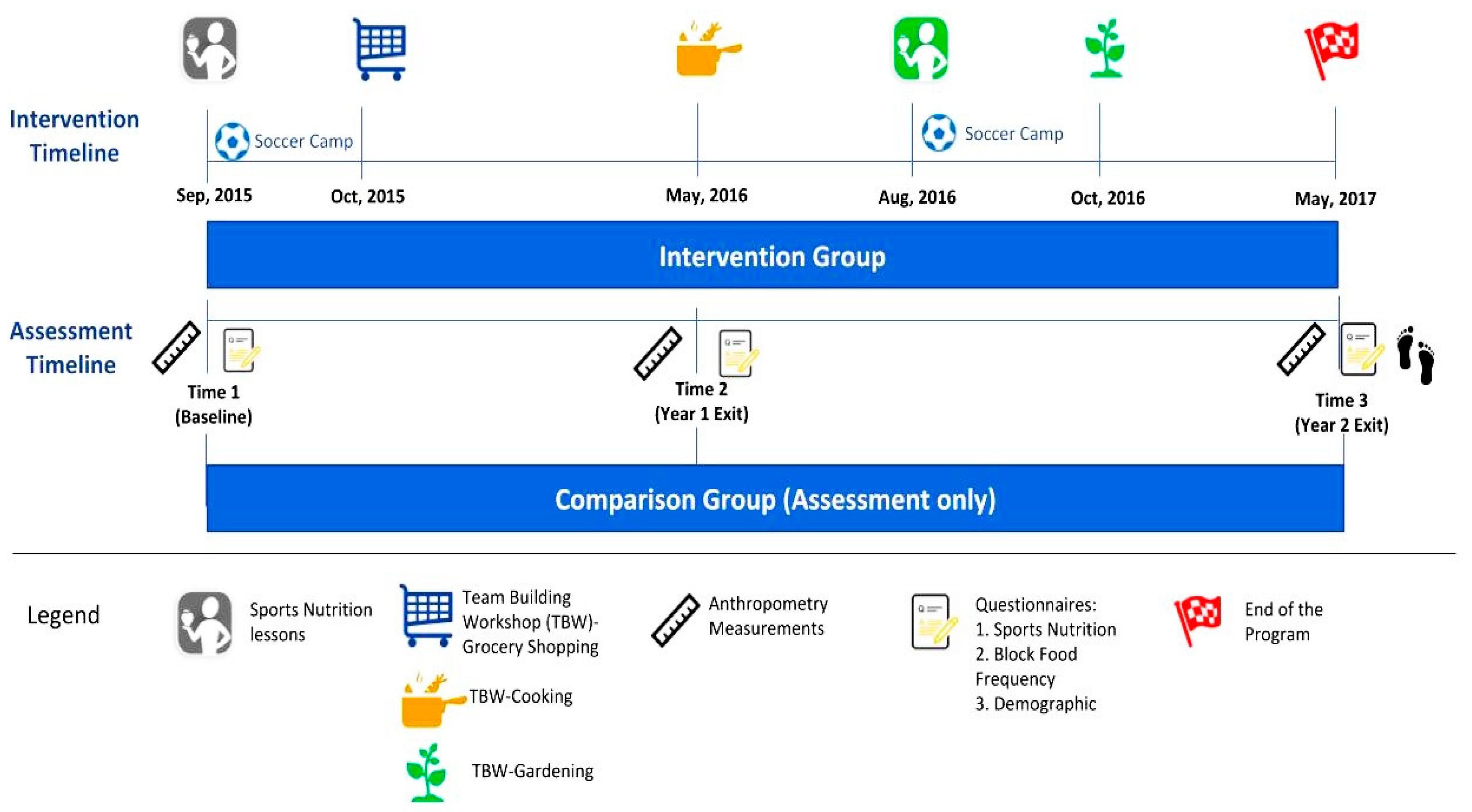
2.1. WAVE Program Overview
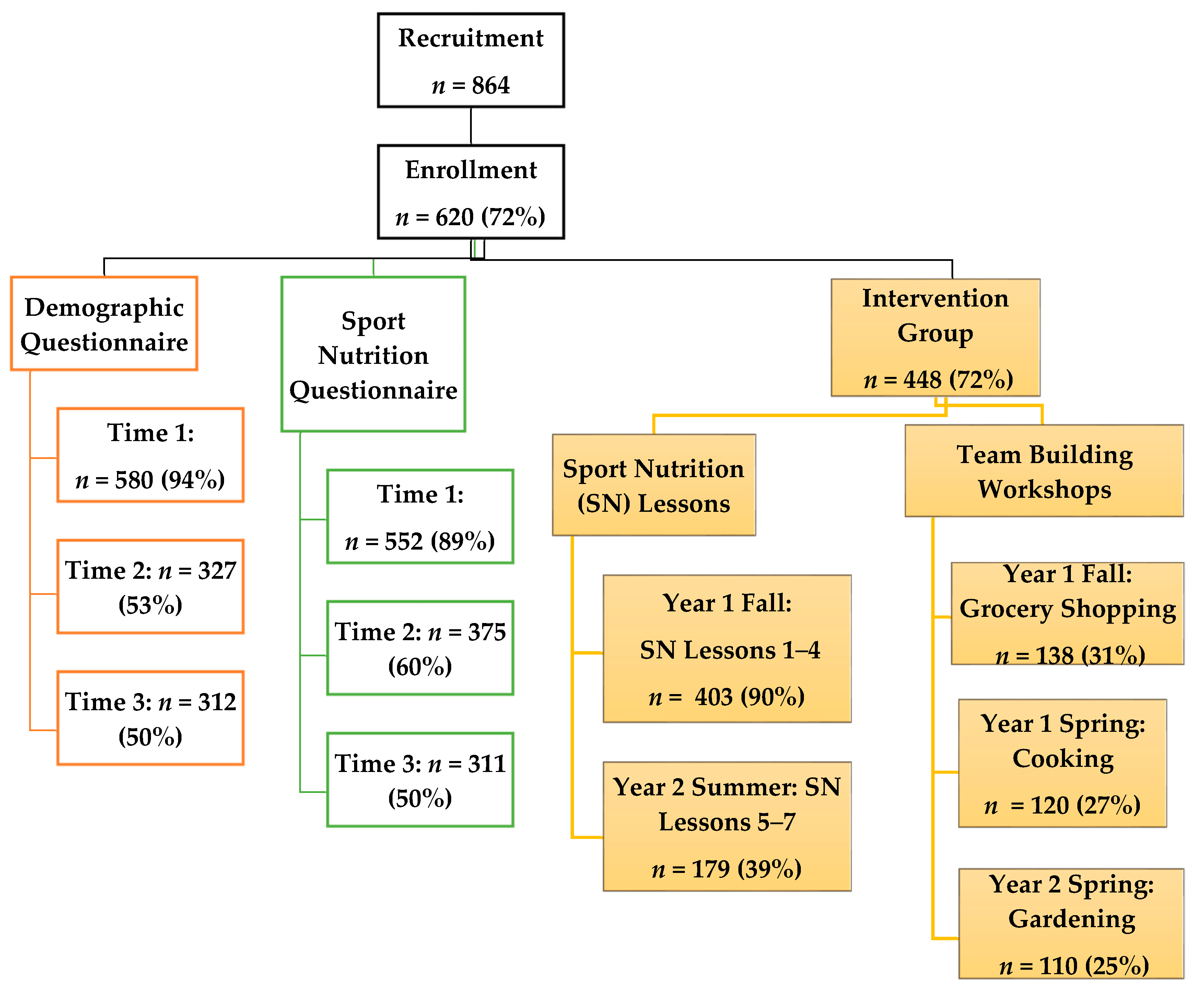
2.2. Recruitment and Participants
2.3. Assessments and Questionnaires
2.4. Intervention
2.5. Statistical Analysis
3. Results
3.1. Sport Nutrition Knowledge
3.2. Attitudes and Beliefs Relevant to Sport Nutrition
3.3. Dietary Behaviors Related to Sport Performance
4. Discussion
4.1. Changes in Sport Nutrition Knowledge
4.2. Changes in Dietary Attitudes/Beliefs Relevant to Sport Performance
4.3. Dietary Behaviors Relevant to Sport Performance
4.4. Participant Engagement and Retention
4.5. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Sawyer, S.M.; Afifi, R.A.; Bearinger, L.H.; Blakemore, S.-J.; Dick, B.; Ezeh, A.C.; Patton, G.C. Adolescence: A foundation for future health. Lancet 2012, 379, 1630–1640. [Google Scholar] [CrossRef]
- Belton, S.; O’Brien, W.; Meegan, S.; Woods, C.; Issartel, J. Youth-Physical Activity towards Health: Evidence and background to the development of the Y-PATH physical activity intervention for adolescents. BMC Public Health 2014, 14, 122. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, C.; Reilly, J.J.; Huang, W.Y. Longitudinal changes in objectively measured sedentary behaviour and their relationship with adiposity in children and adolescents: Systematic review and evidence appraisal. Obes. Rev. 2014, 15, 791–803. [Google Scholar] [CrossRef] [PubMed]
- Nader, P.R.; Bradley, R.H.; Houts, R.M.; Mcritchie, S.L.; O’brien, M. Moderate-to-Vigorous Physical Activity from Ages 9 to 15 Years. JAMA 2008, 300, 295–305. [Google Scholar] [CrossRef] [PubMed]
- Nelson, M.C.; Story, M.; Larson, N.I.; Neumark-Sztainer, D.; Lytle, L.A. Emerging adulthood and college-aged youth: An overlooked age for weight-related behavior change. Obesity 2008, 16, 2205–2211. [Google Scholar] [CrossRef] [PubMed]
- Das, J.K.; Salam, R.A.; Thornburg, K.L.; Prentice, A.M.; Campisi, S.; Lassi, Z.S.; Koletzko, B.; Bhutta, Z.A. Nutrition in adolescents: Physiology, metabolism, and nutritional needs. Ann. N. Y. Acad. Sci. 2017, 13931, 21–33. [Google Scholar] [CrossRef] [PubMed]
- Gootman, J.A.; Lawrence, R.S.; Sim, L.J.; Institute of Medicine (U.S.); National Research Council (U.S.); Committee on Adolescent Health Care Services and Models of Care for Treatment, Prevention, and Healthy Development. Adolescent Health Services Missing Opportunities; National Academies Press: Washington, DC, USA, 2009. [Google Scholar]
- Neumark-Sztainer, D.; Story, M.; Resnick, M.; Blum, R. Lessons learned about adolescent nutrition from the Minnesota Adolescent Health Survey. J. Am. Diet. Assoc. 1998, 98, 1449–1456. [Google Scholar] [CrossRef]
- Banfield, E.C.; Liu, Y.; Davis, J.S.; Chang, S.; Frazier-Wood, A.C. Poor Adherence to US Dietary Guidelines for Children and Adolescents in the National Health and Nutrition Examination Survey Population. J. Acad. Nutr. Diet. 2016, 116, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Elliot, D.L.; Goldberg, L.; Moe, E.L.; Defrancesco, C.A.; Durham, M.B.; Hix-Small, H. Preventing substance use and disordered eating: Initial outcomes of the ATHENA (athletes targeting healthy exercise and nutrition alternatives) program. Arch. Pediatr. Adolesc. Med. 2004, 158, 1043–1049. [Google Scholar] [CrossRef] [PubMed]
- Kann, L.; McManus, T.; Harris, W.A. Youth Risk Behavior Surveillance—United States, 2017; Surveillance Summaries; Centers for Disease Control (CDC), U.S. Department of Health & Human Services: Atlanta, GA, USA, 2018; p. 479.
- Turner, R.W.; Perrin, E.M.; Coyne-Beasley, T.; Peterson, C.J.; Skinner, A.C. Reported Sports Participation, Race, Sex, Ethnicity, and Obesity in US Adolescents from NHANES Physical Activity (PAQ_D). Glob. Pediatr. Health 2015, 2. [Google Scholar] [CrossRef] [PubMed]
- National Federation of State High School Associations. High School Sports Participation Increases for 28th Straight Year, Nears 8 Million Mark. Available online: https://www.nfhs.org/articles/high-school-sports-participation-increases-for-28th-straight-year-nears-8-million-mark/ (accessed on 1 August 2018).
- Cavadini, C.; Decarli, B.; Grin, J.; Narring, F.; Michaud, P.-A. Food habits and sport activity during adolescence: Differences between athletic and non-athletic teenagers in Switzerland. Eur. J. Clin. Nutr. 2000, 54, S16. [Google Scholar] [CrossRef] [PubMed]
- Nelson, T.F.; Stovitz, S.D.; Thomas, M.; LaVoi, N.M.; Bauer, K.W.; Neumark-Sztainer, D. Do youth sports prevent pediatric obesity? A systematic review and commentary. Curr. Sports Med. Rep. 2011, 10, 360–370. [Google Scholar] [CrossRef] [PubMed]
- Caswell, M.S.; Hanning, R.M. Adolescent perspectives of the recreational ice hockey food environment and influences on eating behaviour revealed through photovoice. Public Health Nutr. 2018, 21, 1255–1265. [Google Scholar] [CrossRef] [PubMed]
- Desbrow, B.; McCormack, J.; Burke, L.M.; Cox, G.R.; Fallon, K.; Hislop, M.; Logan, R.; Marino, N.; Sawyer, S.M.; Shaw, G.; et al. Sports Dietitians Australia position statement: Sports nutrition for the adolescent athlete. Int. J. Sport Nutr. Exerc. Metab. 2014, 24, 570–584. [Google Scholar] [CrossRef] [PubMed]
- Aerenhouts, D.; Deriemaeker, P.; Hebbelinck, M.; Clarys, P. Energy and macronutrient intake in adolescent sprint athletes: A follow-up study. J. Sports Sci. 2011, 29, 73–82. [Google Scholar] [CrossRef] [PubMed]
- Petrie, H.J.; Stover, E.A.; Horswill, C.A. Nutritional concerns for the child and adolescent competitor. Nutrition 2004, 20, 620–631. [Google Scholar] [CrossRef] [PubMed]
- Unnithan, V.B.; Goulopoulou, S. Styliani Nutrition for the Pediatric Athlete. Curr. Sports Med. Rep. 2004, 3, 206–211. [Google Scholar] [CrossRef] [PubMed]
- Nattiv, A.; Loucks, A.B.; Manore, M.M.; Sanborn, C.F.; Sundgot-Borgen, J.; Warren, M.P. American College of Sports Medicine position stand. The female athlete triad. Med. Sci. Sports Exerc. 2007, 39, 1867–1882. [Google Scholar] [PubMed]
- Cialdella-Kam, L.; Kulpins, D.; Manore, M. Vegetarian, Gluten-Free, and Energy Restricted Diets in Female Athletes. Sports 2016, 4, 50. [Google Scholar] [CrossRef] [PubMed]
- Beals, K.A.; Manore, M.M. Nutritional Status of Female Athletes with Subclinical Eating Disorders. J. Am. Diet. Assoc. 1998, 98, 419–425. [Google Scholar] [CrossRef]
- Woolf, K.; Manore, M.M. B-vitamins and exercise: Does exercise alter requirements? Int. J. Sport Nutr. Exerc. Metab. 2006, 16, 453–484. [Google Scholar] [CrossRef] [PubMed]
- Van Der Beek, E.J.; van Dokkum, W.; Schrijver, J.; Wedel, M.; Gaillard, A.W.; Wesstra, A.; van de Weerd, H.; Hermus, R.J. Thiamin, riboflavin, and vitamins B-6 and C: Impact of combined restricted intake on functional performance in man. Am. J. Clin. Nutr. 1988, 48, 1451–1462. [Google Scholar] [CrossRef] [PubMed]
- Mountjoy, M.; Sundgot-Borgen, J.; Burke, L.; Carter, S.; Constantini, N.; Lebrun, C.; Meyer, N.; Sherman, R.; Steffen, K.; Budgett, R.; et al. The IOC consensus statement: Beyond the Female Athlete Triad—Relative Energy Deficiency in Sport (RED-S). Br. J. Sports Med. 2014, 48, 491–497. [Google Scholar] [CrossRef] [PubMed]
- Mountjoy, M.; Sundgot-Borgen, J.; Burke, L.; Ackerman, K.E.; Blauwet, C.; Constantini, N.; Lebrun, C.; Lundy, B.; Melin, A.; Meyer, N.; et al. International Olympic Committee (IOC) Consensus Statement on Relative Energy Deficiency in Sport (RED-S): 2018 Update. Int. J. Sport Nutr. Exerc. Metab. 2018, 28, 316–331. [Google Scholar] [CrossRef] [PubMed]
- Gibson, J.C.; Stuart-Hill, L.; Martin, S.; Gaul, C. Nutrition status of junior elite Canadian female soccer athletes. Int. J. Sport Nutr. Exerc. Metab. 2011, 21, 507–514. [Google Scholar] [CrossRef] [PubMed]
- Juzwiak, C.R.; Ancona-Lopez, F. Evaluation of Nutrition Knowledge and Dietary Recommendations by Coaches of Adolescent Brazilian Athletes. Int. J. Sport Nutr. Exerc. Metab. 2004, 14, 222–235. [Google Scholar] [CrossRef] [PubMed]
- Martínez, S.; Pasquarelli, B.N.; Romaguera, D.; Arasa, C.; Tauler, P.; Aguiló, A. Anthropometric Characteristics and Nutritional Profile of Young Amateur Swimmers. J. Strength Cond. Res. 2011, 25, 1126–1133. [Google Scholar] [CrossRef] [PubMed]
- Woolf, K.; LoBuono, D.; Manore, M.M. B-vitamins and the Female Athlete. In Nutrition and the Female Athlete. From Research to Practice, 2nd ed.; CRC Press: Boca Raton, FL, USA, 2013. [Google Scholar]
- Hinton, P. Trace minerals of concern for female athletes: Iron and Zinc. In Nutrition and the Female Athlete. From Research to Practice, 2nd ed.; CRC Press: Boca Raton, FL, USA, 2013. [Google Scholar]
- La Bounty, P.; Campbell, B.; Wilson, J.; Galvan, E.; Berardi, J.; Kleiner, S.; Kreider, R.; Stout, J.; Ziegenfuss, T.; Spano, M.; et al. International Society of Sports Nutrition position stand: Meal frequency. J. Int. Soc. Sports Nutr. 2011, 8, 4. [Google Scholar] [CrossRef] [PubMed]
- Rampersaud, G.C.; Pereira, M.A.; Girard, B.L.; Adams, J.; Metzl, J.D. Breakfast habits, nutritional status, body weight, and academic performance in children and adolescents. J. Am. Diet. Assoc. 2005, 105, 743–760. [Google Scholar] [CrossRef] [PubMed]
- Bruening, M.; Larson, N.; Story, M.; Neumark-Sztainer, D.; Hannan, P. Predictors of Adolescent Breakfast Consumption: Longitudinal Findings from Project EAT. J. Nutr. Educ. Behav. 2011, 43, 390–395. [Google Scholar] [CrossRef] [PubMed]
- Merten, M.J.; Williams, A.L.; Shriver, L.H. Breakfast Consumption in Adolescence and Young Adulthood: Parental Presence, Community Context, and Obesity. J. Am. Diet. Assoc. 2009, 109, 1384–1391. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.T.; Erdman, K.A.; Burke, L.M. American College of Sports Medicine Joint Position Statement. Nutrition and Athletic Performance. Med. Sci. Sports Exerc. 2016, 48, 543–568. [Google Scholar] [CrossRef] [PubMed]
- Perron, M.; Endres, J. Knowledge, attitudes, and dietary practices of female athletes. J. Am. Diet. Assoc. 1985, 85, 573–576. [Google Scholar] [PubMed]
- Walsh, M.; Cartwright, L.; Corish, C.; Sugrue, S.; Wood-Martin, R. The Body Composition, Nutritional Knowledge, Attitudes, Behaviors, and Future Education Needs of Senior Schoolboy Rugby Players in Ireland. Int. J. Sport Nutr. Exerc. Metab. 2011, 21, 365–376. [Google Scholar] [CrossRef] [PubMed]
- Cupisti, A.; D’Alessandro, C.; Castrogiovanni, S.; Barale, A.; Morelli, E. Nutrition Knowledge and Dietary Composition in Italian Adolescent Female Athletes and Non-athletes. Int. J. Sport Nutr. Exerc. Metab. 2002, 12, 207–219. [Google Scholar] [CrossRef] [PubMed]
- Wiita, B.G.; Stombaugh, I.A. Nutrition Knowledge, Eating Practices, and Health of Adolescent Female Runners: A 3-Year Longitudinal Study. Int. J. Sport Nutr. 1996, 6, 414–425. [Google Scholar] [CrossRef] [PubMed]
- Manore, M.M.; Patton-Lopez, M.M.; Meng, Y.; Wong, S.S. Sport Nutrition Knowledge, Behaviors and Beliefs of High School Soccer Players. Nutrients 2017, 9, 350. [Google Scholar] [CrossRef] [PubMed]
- Ranby, K.W.; Aiken, L.S.; Mackinnon, D.P.; Elliot, D.L.; Moe, E.L.; McGinnis, W.; Goldberg, L. A mediation analysis of the ATHENA intervention for female athletes: Prevention of athletic-enhancing substance use and unhealthy weight loss behaviors. J. Pediatr. Psychol. 2009, 34, 1069–1083. [Google Scholar] [CrossRef] [PubMed]
- Francisco, R.; Narciso, I.; Alarcão, M. Individual and relational risk factors for the development of eating disorders in adolescent aesthetic athletes and general adolescents. Eat. Weight Disord. EWD 2013, 18, 403–411. [Google Scholar] [CrossRef] [PubMed]
- Larson, N.; MacLehose, R.; Fulkerson, J.A.; Berge, J.M.; Story, M.; Neumark-Sztainer, D. Eating breakfast and dinner together as a family: Associations with sociodemographic characteristics and implications for diet quality and weight status. J. Acad. Nutr. Diet. 2013, 113, 1601–1609. [Google Scholar] [CrossRef] [PubMed]
- Buscemi, J.; Beech, B.; Relyea, G. Predictors of Obesity in Latino Children: Acculturation as a Moderator of the Relationship between Food Insecurity and Body Mass Index Percentile. J. Immigr. Minor. Health 2011, 13, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Colby, S.L.; Ortman, J.M. Projections of the Size and Composition of the U.S. Population: 2014 to 2060; U.S. Department of Commerce, Economics and Statistics Administration, U.S. Census Bureau: Washington, DC, USA, 2015. [Google Scholar]
- Grech, A.; Rangan, A.; Allman-Farinelli, M. Social Determinants and Poor Diet Quality of Energy-Dense Diets of Australian Young Adults. Healthcare 2017, 5, 70. [Google Scholar] [CrossRef] [PubMed]
- Laramée, C.; Drapeau, V.; Valois, P.; Goulet, C.; Jacob, R.; Provencher, V.; Lamarche, B. Evaluation of a Theory-Based Intervention Aimed at Reducing Intention to Use Restrictive Dietary Behaviors Among Adolescent Female Athletes. J. Nutr. Educ. Behav. 2017, 49, 497.e1–504.e1. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, L.; MacKinnon, D.P.; Elliot, D.L.; Moe, E.L.; Clarke, G.; Cheong, J. The adolescents training and learning to avoid steroids program: Preventing drug use and promoting health behaviors. Arch. Pediatr. Adolesc. Med. 2000, 154, 332–338. [Google Scholar] [CrossRef] [PubMed]
- Kavouras, S.A.; Arnaoutis, G.; Makrillos, M.; Garagouni, C.; Nikolaou, E.; Chira, O.; Ellinikaki, E.; Sidossis, L.S. Educational intervention on water intake improves hydration status and enhances exercise performance in athletic youth. Scand. J. Med. Sci. Sports 2012, 22, 684–689. [Google Scholar] [CrossRef] [PubMed]
- Cleary, M.A.; Hetzler, R.K.; Wasson, D.; Wages, J.J.; Stickley, C.; Kimura, I.F. Hydration behaviors before and after an educational and prescribed hydration intervention in adolescent athletes. J. Athl. Train. 2012, 47, 273–281. [Google Scholar] [CrossRef] [PubMed]
- Nascimento, M.; Silva, D.; Ribeiro, S.; Nunes, M.; Almeida, M.; Mendes-Netto, R. Effect of a Nutritional Intervention in Athlete’s Body Composition, Eating Behaviour and Nutritional Knowledge: A Comparison between Adults and Adolescents. Nutrients 2016, 8, 535. [Google Scholar] [CrossRef] [PubMed]
- Philippou, E.; Middleton, N.; Pistos, C.; Andreou, E.; Petrou, M. The impact of nutrition education on nutrition knowledge and adherence to the Mediterranean Diet in adolescent competitive swimmers. J. Sci. Med. Sport 2017, 20, 328–332. [Google Scholar] [CrossRef] [PubMed]
- Walter, O.; Bobrov, A.; Tamir, S. Surprising Advantages of Low Self-Efficacy Revealed in a Sports Nutrition Education. Am. J. Health Behav. 2018, 42, 23–33. [Google Scholar] [CrossRef] [PubMed]
- Meng, Y.; Wong, S.S.; Manore, M.M.; Patton-López, M. WAVE~Ripples for Change Obesity Two-Year Intervention in High School Soccer Players: Process Evaluation, Best Practices, and Youth Engagement. Nutrients 2018, 10, 711. [Google Scholar] [CrossRef] [PubMed]
- Wong, S.S.; Manore, M.M.; Pilolla, K.; Skoog, I.; Hill, D.; Hand, T. WAVE Project: Sport Nutrition Education Resources. J. Youth Dev. 2018, 13, 275–283. [Google Scholar] [CrossRef]
- Johnson, T.; Wong, S.S.; Manore, M.M. The WAVE Experience: Best practices for engaging high school soccer players in life-skills team building competitions. J. Natl. Ext. Assoc. Fam. Consum. Sci. 2018, 13, 44–58. [Google Scholar]
- Meng, Y.; Manore, M.M.; Schuna, J.M., Jr.; Patton-Lopez, M.M.; Branscum, A.; Wong, S.S. Promoting Healthy Diet, Physical Activity, and Life-Skills in High School Athletes: Results from the WAVE Ripples for Change Childhood Obesity Prevention Two-Year Intervention. Nutrients 2018, 10, 947. [Google Scholar] [CrossRef] [PubMed]
- Manore, M.M.; Pilolla, K.; Skoog, I.; Hill, D.; Hand, T.; Wong, S.S. WAVE Sport Nutrition Curriculum. WAVE~Ripples for Change: Obesity Prevention in Active Youth. Oregon State University Extension Service 2018. Available online: https://catalog.extension.oregonstate.edu/em9218 (accessed on 31 October 2018).
- Chapman, P.; Toma, R.B.; Tuveson, R.V.; Jacob, M. Nutrition knowledge among adolescent high school female athletes. Adolescence 1997, 32, 437–446. [Google Scholar] [PubMed]
- Spendlove, J.K.; Heaney, S.E.; Gifford, J.A.; Prvan, T.; Denyer, G.S.; O’Connor, H.T. Evaluation of general nutrition knowledge in elite Australian athletes. Br. J. Nutr. 2012, 107, 1871–1880. [Google Scholar] [CrossRef] [PubMed]
- Little, J.C.; Perry, D.R.; Volpe, S.L. Effect of nutrition supplement education on nutrition supplement knowledge among high school students from a low-income community. J. Community Health 2002, 27, 433–450. [Google Scholar] [CrossRef] [PubMed]
- Neumark-Sztainer, D.; Croll, J.; Story, M.; Hannan, P.J.; French, S.A.; Perry, C. Ethnic/racial differences in weight-related concerns and behaviors among adolescent girls and boys: Findings from Project EAT. J. Psychosom. Res. 2002, 53, 963–974. [Google Scholar] [CrossRef]
- Trakman, G.L.; Forsyth, A.; Hoye, R.; Belski, R. Development and validation of a brief general and sports nutrition knowledge questionnaire and assessment of athletes’ nutrition knowledge. J. Int. Soc. Sports Nutr. 2018, 15, 17. [Google Scholar] [CrossRef] [PubMed]
- Story, M.; Neumark-Sztainer, D.; French, S. Individual and Environmental Influences on Adolescent Eating Behaviors. J. Am. Diet. Assoc. 2002, 102, S40–S51. [Google Scholar] [CrossRef]
- Birkenhead, K.L.; Slater, G. A Review of Factors Influencing Athletes’ Food Choices. Sports Med. 2015, 45, 1511–1522. [Google Scholar] [CrossRef] [PubMed]
- Boutelle, K.N.; Birkeland, R.W.; Hannan, P.J.; Story, M.; Neumark-Sztainer, D. Associations between Maternal Concern for Healthful Eating and Maternal Eating Behaviors, Home Food Availability, and Adolescent Eating Behaviors. J. Nutr. Educ. Behav. 2007, 39, 248–256. [Google Scholar] [CrossRef] [PubMed]
- Neumark-Sztainer, D.; Story, M.; Perry, C.; Casey, M.A. Factors Influencing Food Choices of Adolescents: Findings from Focus-Group Discussions with Adolescents. J. Am. Diet. Assoc. 1999, 99, 929–937. [Google Scholar] [CrossRef]
- Bean, C.N.; Fortier, M.; Post, C.; Chima, K. Understanding How Organized Youth Sport May Be Harming Individual Players within the Family Unit: A Literature Review. Int. J. Environ. Res. Public Health 2014, 11, 10226–10268. [Google Scholar] [CrossRef] [PubMed]
- Drewnowski, A.; Rehm, C.; Vieux, F. Breakfast in the United States: Food and Nutrient Intakes in Relation to Diet Quality in National Health and Examination Survey 2011–2014. A Study from the International Breakfast Research Initiative. Nutrients 2018, 10, 1200. [Google Scholar] [CrossRef] [PubMed]
- Deshmukh-Taskar, P.R.; Nicklas, T.A.; O’Neil, C.E.; Keast, D.R.; Radcliffe, J.D.; Cho, S. The Relationship of Breakfast Skipping and Type of Breakfast Consumption with Nutrient Intake and Weight Status in Children and Adolescents: The National Health and Nutrition Examination Survey 1999–2006. J. Am. Diet. Assoc. 2010, 110, 869–878. [Google Scholar] [CrossRef] [PubMed]
- Tawfik, S.; El Koofy, N.; Moawad, E.M.I. Patterns of Nutrition and Dietary Supplements Use in Young Egyptian Athletes: A Community-Based Cross-Sectional Survey. PLoS ONE 2016, 11, e0161252. [Google Scholar] [CrossRef] [PubMed]
- Murimi, M.W.; Kanyi, M.; Mupfudze, T.; Amin, M.R.; Mbogori, T.; Aldubayan, K. Factors Influencing Efficacy of Nutrition Education Interventions: A Systematic Review. J. Nutr. Educ. Behav. 2017, 49, 142–165.e1. [Google Scholar] [CrossRef] [PubMed]
- Wesche-Thobaben, J. The development and description of the comparison group in the Look AHEAD trial. Clin. Trials 2011, 8, 320–329. [Google Scholar] [CrossRef] [PubMed]
- Olander, C. Nutrition Education and the Role of Dosage; Food and Nutrition Services, USDA: Alexandria, VA, USA, 2007; p. 14. [Google Scholar]
| Theme | Topics Addressed by the Questions |
|---|---|
| Training Schedule | Position played, training schedule, hours of training during and outside school. |
| Eating practices and behaviors around sport | Typical eating patterns (breakfast, lunch, dinner, snacks); types of fluids consumed; timing of food/beverage intake before/after exercise; typical foods consumed. |
| Attitudes and beliefs about food/nutrition relative to sport | Importance of food/beverages consumed for sport performance; statements about diet that apply to them; nutritional needs of athletes are different from non-athlete peers. |
| Sport Nutrition Knowledge |
|
| Lesson | Title | Lesson Goals (30 Min Lessons) |
|---|---|---|
| Year 1: Fall 2015 | ||
| 1 | Hydration | To provide athletes with the knowledge to understand the purpose of proper hydration for sport and exercise, and give them the tools and skills needed to implement a hydration plan to delay onset of dehydration, improve and maintain training and performance, and decrease risk of illness and injury related to dehydration. |
| 2 | Pre-Exercise Fueling | To provide athletes with the knowledge necessary to understand the purpose of proper fueling prior to exercise, and give them the tools and skills necessary to implement a pre-exercise fueling plan to delay onset of fatigue and dehydration, improve and maintain training and performance, and avoid gastrointestinal (GI) discomfort. |
| 3 | During Exercise Fueling | To provide athletes with the knowledge to understand the purpose of proper fueling during exercise, and give them the tools and skills necessary to implement a during-exercise fueling plan to improve and maintain training and performance, and avoid GI discomfort. |
| 4 | Recovery Nutrition | To provide athletes with the knowledge to understand the purpose of proper recovery nutrition and the skills to implement a recovery nutrition plan. Key components included replete glycogen stores, rehydrate, initiate recovery and adaptation processes in the body that require carbohydrate, protein, and water, and achieve the maximum gains from training to maintain and/or improve performance. |
| Year 2: Summer 2016 | ||
| 5 | Body Composition and Image | Lessons were different for males and females. Males: To provide athletes with an understanding of body composition, how it is measured, and factors that influence body size and composition. Females: To provide athletes with an understanding of body composition and a heathy perspective on body image in order to develop body appreciation and acceptance. |
| 6 | Maintaining Muscle and Staying Well | To provide athletes with the knowledge to understand how nutrient timing and composition of foods/meals will help them meet their protein needs; maintain a strong immune system and stay healthy while participating in sports. |
| 7 | Eating Well while Eating Out | Help athletes understand how to make better food selections outside the home that are within their budgets. Raise awareness that cooking and eating food from home can be the most affordable and ‘healthy’ option. |
| Total Sample (n = 217) | Intervention Group (IG) (n = 153) | Comparison Group (CG) (n = 64) | |||
|---|---|---|---|---|---|
| Mean (SD) | |||||
| Female | Male | Female | Male | ||
| Height (cm) | 161.8 (7.0) | 171.2 (7.8) | 160.1 (5.6) | 172.8 (8.9) | |
| Weight (kg) a | 58.7 (10.6) | 62.9 (12.5) | 59.9 (9.0) | 68.2 (16.7) | |
| Body Mass Index (kg/m2) | 22.4 (3.6) | 21.4 (3.7) | 23.3 (3.1) | 22.7 (5.2) | |
| Total Sample (n = 217) | Intervention Group (IG) (n = 153) | Comparison Group (CG) (n = 64) | |||
| Age (y) | 14.9 (0.91) | 14.9 (0.91) | 14.9 (0.91) | ||
| Age preparing meals for self (y) | 11.0 (2.1) | 11.0 (2.1) | 11.1 (2.2) | ||
| Years playing soccer | 6.9 (3.8) | 7.3 (3.7) | 5.8 (3.6) * | ||
| n size (%) | |||||
| Sex | |||||
| Female | 138 (64.0) ** | 94 (61.4) | 44 (68.8) | ||
| Male | 79 (36.4) | 59 (38.6) | 20 (31.2) | ||
| Race/Ethnicity * | |||||
| Latino | 103 (47.5) | 69 (45.1) | 34 (53.1) | ||
| White | 96 (44.2) | 61(44.4) | 28 (43.8) | ||
| Other b | 18 (8.3) | 16 (10.5) | 2 (3.1) | ||
| Year in School | |||||
| 9th grade | 92 (42.4) | 64 (42.1) | 28(44.4) | ||
| 10th grade | 63 (29.03) | 47 (30.9) | 16 (25.4) | ||
| 11th grade | 56 (25.81) | 39 (25.7) | 17 (27) | ||
| 12th | 4 (1.84) ** | 2 (1.3) | 2 (3.2) | ||
| No injuries past 12-months | 142 (65.4) | 97 (63.8) | 45 (72.6) | ||
| Participate in NSLP c | 100 (46.5) | 67(44.4) | 33 (51.6) | ||
| Latino NSLP | 82 (38.1) | 56 (37.1) | 26 (40.6) | ||
| White NSLP | 14 (6.5) | 8 (5.3) | 6 (9.4) | ||
| Other NSLP | 4 (1.9) | 3 (2.0) | 1 (1.6) | ||
| Prepares meals for self (%) | 56.9 | 55.9 | 59.4 | ||
| Intervention Group (n = 153) | Comparison Group (n = 64) | |||||||
|---|---|---|---|---|---|---|---|---|
| Variable | Time 1 a | Time 2 | Time 3 | Change b | Time 1 | Time 2 | Time 3 | Change b |
| Total SNK score | 5.16 (1.80) | 5.99 (1.93) ** | 6.09 (1.59) | 0.93 *** | 5.00 (1.62) | 4.98 (1.79) | 5.08 (1.38) | 0.09 |
| Hydration | 2.27 (0.74) | 2.41 (0.73) * | 2.48 (0.64) ** | 0.21 ** | 2.19 (0.64) | 2.17 (0.66) | 2.19 (0.67) | 0.00 |
| Pre/Post Exercise Food Selection | 0.42 (0.50) * | 0.59 (0.49) ** | 0.62 (0.49) ** | 0.20 *** | 0.27 (0.45) | 0.34 (0.48) | 0.35 (0.48) | 0.08 |
| Protein/Carbohydrate Knowledge | 1.43 (0.96) | 1.86 (0.93) ** | 1.85 (0.96) ** | 0.42 *** | 1.21 (0.96) | 1.38 (1.12) | 1.44 (0.95) | 0.21 |
| Supplement Knowledge | 1.04 (0.62) | 1.09 (0.69) | 1.13 (0.62) | 0.09 | 1.19 (0.71) | 1.10 (0.73) | 1.10(0.64) | −0.08 |
| Time 1 | Time 2 | Time 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Comparison n (%) | Intervention n (%) a | OR b | Comparison n (%) | Intervention n (%) a | OR (95% CI; p-value) | Comparison n (%) | Intervention n (%) a | OR (95% CI; p-Value) | |
| Diet is important to performance | 56 (88.9) | 120 (84.5) | 1.00 | 59 (92.3) | 132 (88.0) | 0.92 (0.27, 3.16); 0.90 | 59 (93.6) | 140 (92.1) | 1.15 (0.30, 4.34); 0.83 |
| As an athlete, my nutritional requirements are different | 26 (41.3) | 86 (60.6) ** | 1.00 | 30 (46.9) | 103 (68.7) ** | 1.27 (0.64, 2.52), 0.50 | 33 (51.6) | 111 (73.0) ** | 1.23 (0.62, 2.49); 0.55 |
| I have trouble knowing what to eat | 14 (22.6) | 43 (30.5) | 1.00 | 15 (23.8) | 33 (22.0) | 0.61 (0.25, 1.49); 0.28 | 14 (22.2) | 26 (17.1) | 0.50 (0.20, 1.25); 0.14 |
| My eating plan/diet meets my nutritional requirements | 16 (25.8) | 37 (26.2) | 1.00 | 26 (41.3) | 46 (30.7) | 0.57 (0.24, 1.31); 0.19 | 30 (47.6) | 48 (31.6) * | 0.43 (0.18, 0.99); 0.05 |
| Muscle mass is important to my performance | 33 (52.4) | 97 (68.3) * | 1.00 | 32 (50.0) | 106 (70.7) ** | 1.26 (0.62, 2.56); 0.52 | 32 (50.0) | 94 (62.2) | 0.95 (0.47, 1.92); 0.83 |
| Nutritional supplements are necessary to support my training | 35 (44.6) | 71 (49.6) | 1.00 | 24 (37.5) | 64 (42.7) | 1.82 (0.90, 3.71); 0.10 | 25 (39.1) | 65 (42.8) | 1.82 (0.89, 3.71); 0.10 |
| I try to eat for performance | 32 (51.6) | 59 (41.8) | 1.00 | 21 (33.3) | 69 (46.0) | 2.62 (1.20, 5.70); 0.02 | 19 (30.2) | 74 (48.68) * | 3.51 (1.59, 7.77); 0.02 |
| Time 1 | Time 2 | Time 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Comparison n (%) | Intervention n (%) a | OR b | Comparison n (%) | Intervention n (%) a | OR (95% CI; p-Value) | Comparison n (%) | Intervention n (%) a | OR (95% CI; p-Value) | |
| Eat breakfast every day | 35 (55.6) | 83 (58.4) | 1.00 | 31 (48.4) | 81 (54.0) | 1.14 (0.62, 2.10); 0.67 | 34 (53.1) | 82 (54.0) | 0.90 (0.49, 1.64); 0.72 |
| Eat lunch 5 or more days a week | 61 (98.4) | 130 (92.2) | 1.00 | 56 (87.5) | 139 (92.7) * | 9.97 (1.30, 76.6); 0.27 | 58 (90.6) | 142 (93.4) * | 8.62 (1.10, 67.57); 0.04 |
| Eat within 1 h before physical activity (PA) | 24 (38.7) | 47 (33.1) | 1.00 | 26 (41.3) | 49 (33.1) | 0.84 (0.41, 1.73); 0.65 | 21 (33.3) | 66 (43.7) | 1.89 (0.91, 3.91); 0.09 |
| Eat within 1 h after PA | 46 (71.8) | 118 (77.1) | 1.00 | 52 (81.2) | 126 (82.4) | 0.73 (0.29, 1.81); 0.50 | 51 (79.7) | 117 (76.5) | 0.58 (0.24, 1.41); 0.23 |
| Consumption of any sugar sweetened beverage 1–4 h before PA | 33 (51.6) | 105 (68.6) * | 1.00 | 34 (53.1) | 97 (63.4) | 0.75 (0.36, 1.55); 0.44 | 26 (40.6) | 79 (51.6) | 0.75 (0.36, 1.58); 0.45 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Patton-Lopez, M.M.; Manore, M.M.; Branscum, A.; Meng, Y.; Wong, S.S. Changes in Sport Nutrition Knowledge, Attitudes/Beliefs and Behaviors Following a Two-Year Sport Nutrition Education and Life-Skills Intervention among High School Soccer Players. Nutrients 2018, 10, 1636. https://doi.org/10.3390/nu10111636
Patton-Lopez MM, Manore MM, Branscum A, Meng Y, Wong SS. Changes in Sport Nutrition Knowledge, Attitudes/Beliefs and Behaviors Following a Two-Year Sport Nutrition Education and Life-Skills Intervention among High School Soccer Players. Nutrients. 2018; 10(11):1636. https://doi.org/10.3390/nu10111636
Chicago/Turabian StylePatton-Lopez, Megan M., Melinda M. Manore, Adam Branscum, Yu Meng, and Siew Sun Wong. 2018. "Changes in Sport Nutrition Knowledge, Attitudes/Beliefs and Behaviors Following a Two-Year Sport Nutrition Education and Life-Skills Intervention among High School Soccer Players" Nutrients 10, no. 11: 1636. https://doi.org/10.3390/nu10111636
APA StylePatton-Lopez, M. M., Manore, M. M., Branscum, A., Meng, Y., & Wong, S. S. (2018). Changes in Sport Nutrition Knowledge, Attitudes/Beliefs and Behaviors Following a Two-Year Sport Nutrition Education and Life-Skills Intervention among High School Soccer Players. Nutrients, 10(11), 1636. https://doi.org/10.3390/nu10111636





