Adherence of Malaysian Adults’ Energy and Macronutrient Intakes to National Recommendations: A Review and Meta-Analysis
Abstract
1. Introduction
- Describe the following dietary characteristics, based on findings from food balance sheet, national surveys and individual studies, using a systematic literature review and meta-analysis:
- Malaysian diets in terms of levels of energy and macronutrient (protein, fat, and carbohydrates) intake during adulthood;
- The proportion of the population whose diets adhere to/exceed/fail to achieve Malaysian Recommended Nutrient Intake (RNI) levels for energy and macronutrients;
- Sources of macronutrients observed in these studies.
- Discuss the health implications of current energy and macronutrient intakes in this age group;
- Provide recommendations to improve intake and prevent development of diet-related chronic disease among Malaysians.
2. Materials and Methods
- -
- Energy and protein met at least 80% of the Malaysian RNI;
- -
- Total fat should not exceed 30% of TEI;
- -
- Carbohydrate intake should fall within 50 to 65% TEI.
3. Results
3.1. Levels of Energy and Macronutrient Intake
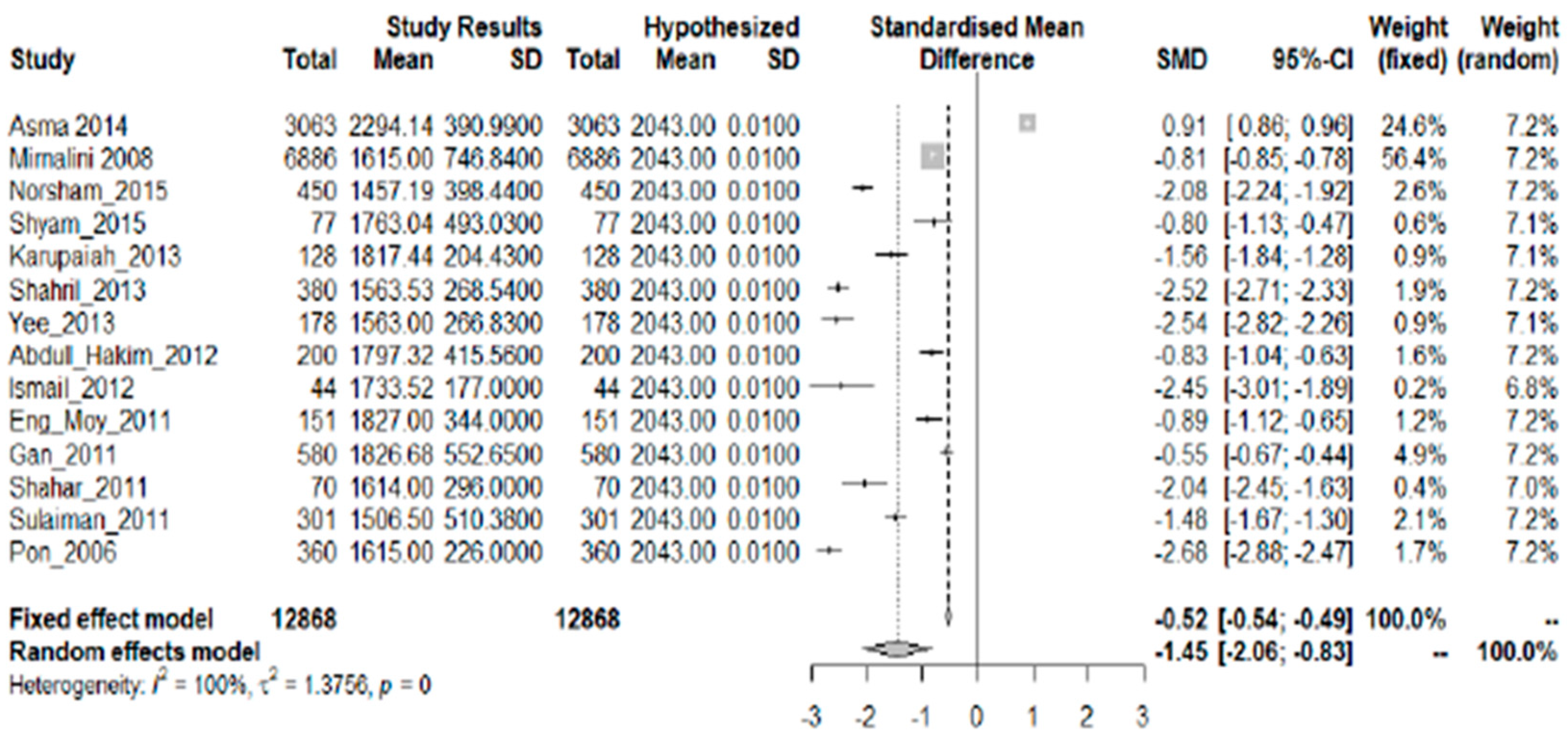
3.1.1. Energy
- Small studies
- Young adults
- Older adultsThree studies [13,15,21] using varied methods showed low energy intake, while two studies [11,24] showed adequate intakes. Women aged 51 to 59 years [13] living in high-rise urban dwellings consumed 78% of energy RNI. Intake of healthy premenopausal Chinese women aged 30 to 45 years was 69% RNI [15]. Women in food secure urban households [21] had low (65% RNI) energy intake. In contrast, women screened for breast cancer showed adequate energy intake (51% met the RNI) [11]. Urban middle-aged Malaysian women showed adequate energy intake (88.5% of the RDA), with postmenopausal women having higher intake (90.3% of RDA) than premenopausal women (87% of RDA) [24].
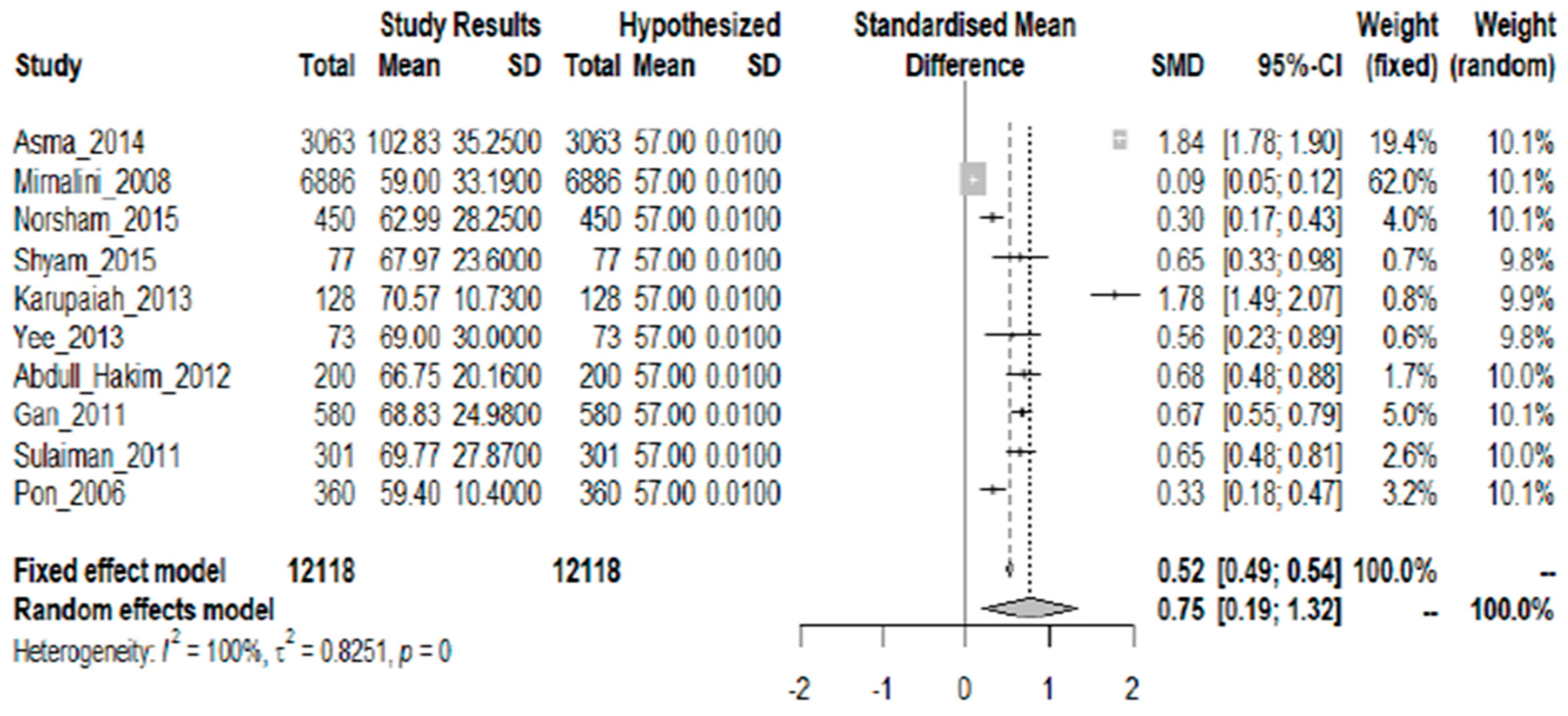
3.1.2. Protein
- Small studies
- Young adults
- Older adultsMost studies on older adults showed a tendency towards high protein intake. Intake among women aged 30 to 59 years was 129% of RNI [13]. Regardless of food security status, urban and rural women in Kelantan had protein intakes at 100% RNI or higher [21]. Among pre- and postmenopausal women, intake was 145% and 143% of RDA, respectively [24].
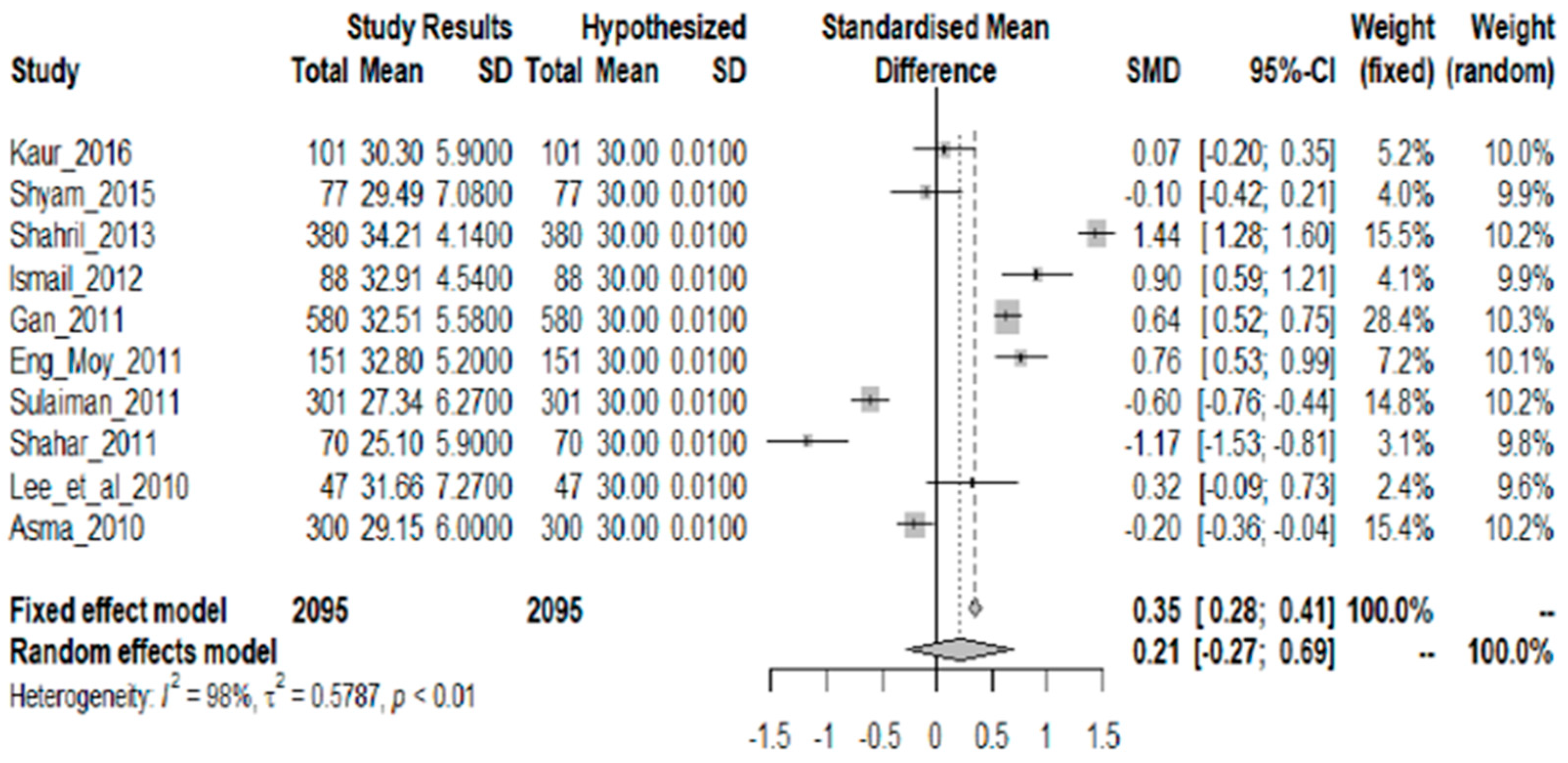
3.1.3. Fat
- Small studiesStudies in different age groups and using different methods consistently showed adequate to high fat intakes among adults. An examination of the habitual diet of Malaysian Punjabis aged 18 to 59 years showed fat intake was 30% TEI [10].
- Young adults
- Older adultsTwo groups of nondiabetic women with a history of gestational diabetes but were currently nondiabetic showed baseline fat intake of 29% and 30% TEI, respectively [12]. Majority of Malay, Chinese, and Indian women screened for breast cancer and found normal showed intake of 25% TEI or higher [11]. Population groups whose fat intakes exceeded 30% TEI were Chinese premenopausal women (36% TEI) [15], male and female Malay subjects (33% TEI) [18], and normal, overweight, and obese women [23]. Rural women with varying levels of food security had higher fat consumption (ranging from 27 to 32% TEI) than urban women (ranging from 24 to 26% TEI) [21]. Among married couples in an urban area in Selangor, consumption of fat was 29% and 30% TEI for husbands and wives, respectively [22]. Healthy men screened for prostate cancer aged 67.8 ± 4.6 years showed adequate fat intake (25% TEI) [20].
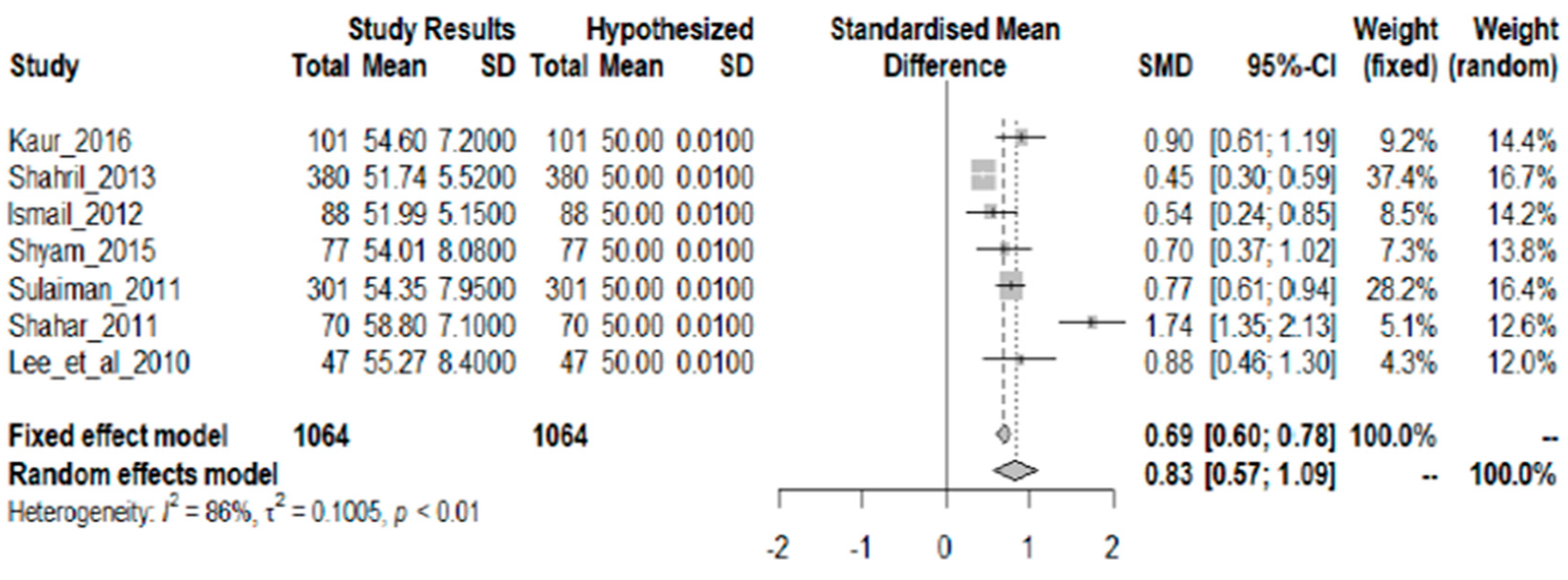
3.1.4. Carbohydrates
3.1.5. Energy
3.1.6. Protein
3.1.7. Fat
3.1.8. Carbohydrate
3.2. Sources of Macronutrients
3.2.1. Carbohydrate Sources
3.2.2. Protein Sources
3.2.3. Fat Sources
4. Discussion
4.1. Energy Intake and Health
4.2. Protein Intake and Health
4.3. Fat Intake and Health
4.4. Carbohydrate Intake and Health
4.5. Limitations of the Present Review
4.5.1. Sources of Dietary Data
4.5.2. Limitations of Nationwide Food Consumption Survey Methods
- Total fat—PUFA, MUFA, and SFA in plasma and red blood cells
- Added sugar—13C in blood glucose; 24-h urinary sucrose and fructose
- Animal protein—24-h urinary nitrogen; 13C in hair; 15N in hair; 24-h urinary creatinine; 24-h urinary levels of taurine, 1-methylhistidine, 3-methylhistidine
5. Conclusions
- (1)
- Use improved dietary assessment methods in national food consumption surveys. Multiple recalls/records (at least 2 nonconsecutive days) in addition to FFQs will provide more accurate dietary data, help reduce under-reporting, and allow estimation of usual or habitual intake.
- (2)
- Conduct randomized intervention trials among Malaysian subjects to determine effects of different types and levels of macronutrient sources on health (e.g., effects of palm oil).
- (3)
- Implement a longitudinal cohort study to establish the association between adult macronutrient intake and development of chronic disease among Malaysians.
- (4)
- In nationwide surveys, use nutrient intake biomarkers to validate self-reported diet measures at least on a subsample. Biomarkers can confirm levels of nutrient intake while self-report measures (i.e., multiple 24-h recalls) can identify food sources of these nutrients.
- (5)
- Update and expand the Malaysian Food Composition Database, for more accurate estimation of energy, macronutrient, and added sugar intake.
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Jamal, R.; Zakaria, S.Z.S.; Kamaruddin, M.A.; Jalal, N.A.; Ismail, N.; Kamil, N.M.; Abdullah, N.; Baharudin, N.; Hussin, N.H.; Othman, H.; et al. Cohort profile: The Malaysian Cohort (TMC) Project: A Prospective Study of Non-communicable Diseases in a Multi-ethnic Population. Int. J. Epidemiol. 2015, 44, 423–431. [Google Scholar] [CrossRef] [PubMed]
- Institute for Health Metrics and Evaluation. Global Burden of Diseases, Injuries, and Risk Factors Study. 2010. Available online: http://www.healthdata.org/sites/default/files/files/country_profiles/GBD/ihme_gbd_country_report_malaysia.pdf (accessed on 7 July 2017).
- WHO. Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020; World Health Organization: Geneva, Switzerland, 2013; pp. 5–6. ISBN 978-92-4-150623-6. [Google Scholar]
- National Coordinating Committee on Food and Nutrition. RNI Recommended Nutrient Intakes for Malaysia. A Report of the Technical Working Group on Nutritional Guidelines; Ministry of Health Malaysia: Putrajaya, Malaysia, 2017; pp. 14–121. ISBN 978-967-12050-4-4.
- FAOSTAT. Food Balance Sheets. Malaysia 2013. Available online: http://www.fao.org/faostat/en/#data/FBS (accessed on 27 September 2017).
- Mahmud, N.A.; Kassim, N.M.; Ahmad, M.H.; Zainuddin, A.A.; Hasani, W.S.R. Nutrient Intake among Malaysian Adults: Do They Meet the Requirement of the Malaysian Recommended Nutrient Intake? Med. J. Malays. 2015, 70 (Suppl. 1), 66. Available online: http://www.e-mjm.org/2015/v70s1/mjm-sept-suppl-2190.html (accessed on 27 September 2017).
- Institute of Public Health. National Health and Morbidity Survey 2014: Malaysian Adult Nutrition Survey (MANS); Survey Findings; Ministry of Health Malaysia: Kuala Lumpur, Malaysia, 2014; Volume 2, pp. 103–110. ISBN 978-983-2387-16-9.
- Asma, A. An Exploration of Dietary Patterns and the Relationship with Obesity in the Malaysian Population. Ph.D. Thesis, Faculty of Medicine, University of Southamption, Southampton, UK, 2014. Available online: https://eprints.soton.ac.uk/382976/ (accessed on 6 July 2017).
- Mirnalini, K.; Zalilah, M.S.; Safiah, M.Y.; Tahir, A.; Siti Haslinda, M.D.; Siti Rohana, D.; Khairul Zarina, M.Y.; Mohd Hasyami, S.; Normah, H. Energy and Nutrient Intakes: Findings from the Malaysian Adult Nutrition Survey (MANS). Malays. J. Nutr. 2008, 14, 1–24. Available online: http://nutriweb.org.my/publications/mjn0014_1/mjn14n1_art1.pdf (accessed on 6 July 2017). [PubMed]
- Kaur, S.; Mohamed, H.J.B.J.; Jalil, R.A.; Yusof, B.-N.M.; Yim, H.S. Validation and Reproducibility of a Culturally Specific Food Frequency Questionnaire (FFQ) for Malaysian Punjabis. Malays. J. Nutr. 2016, 22, 245–255. [Google Scholar]
- Norsham, J.; Shahar, S.; Sahar, M.A.; Ghazali, A.R.; Noah, R.M.D. Trend of Physical Activity, Dietary Intake and Body Composition among Women with High Breast Adiposity. Merit Res. J. Med. Med. Sci. 2015, 3, 361–367. [Google Scholar]
- Shyam, S.; Fatimah, A.; Rohana, A.G.; Norasyikin, A.W.; Nik Shanita, S.; Chinna, K.; Mohd Yusof, B.N.; Nor Azmi, K. Effect of Including Glycaemic Index (GI) Nutrition Education, within the Conventional Healthy Dietary Recommendation Framework, on Body Weight and Composition of Women with Prior Gestational Diabetes Mellitus: Results from a One-Year Randomised Controlled Trial. Malays. J. Nutr. 2015, 21, 269–283. [Google Scholar]
- Karupaiah, T.; Swee, W.C.S.; Liew, S.Y.; Ng, B.K.; Chinna, K. Dietary Health Behaviors of Women Living in High Rise Dwellings: A Case Study of an Urban Community in Malaysia. J. Community Health 2013, 38, 163–171. [Google Scholar] [CrossRef] [PubMed]
- Shahril, M.R.; Dali, W.P.E.W.; Lua, P.L. A 10-Week Multimodal Nutrition Education Intervention Improves Dietary Intake among University Students: Cluster Randomized Controlled Trial. J. Nutr. Metab. 2013, 658642. [Google Scholar] [CrossRef] [PubMed]
- Yee, Y.S.S.; Zaitun, Y.; Chan, Y.M.; Norhaizan, M.E. Association between Anthropometric Status, Dietary Intake and Physical Activity with Bone Health Status among Premenopausal Chinese Women in the Klang Valley, Malaysia. Malays. J. Nutr. 2013, 19, 293–302. [Google Scholar]
- Abdull Hakim, N.H.; Muniandy, N.D.; Danish, A. Nutritional Status and Eating Practices among University Students in Selected Universities in Selangor, Malaysia. Asian J. Clin. Nutr. 2012, 4, 77–87. [Google Scholar] [CrossRef]
- Ismail, N.H.; Manaf, Z.A.; Azizan, N.Z. High Glycemic Load Diet, Milk and Ice Cream Consumption are Related to Acne Vulgaris in Malaysian Young Adults: A Case Control Study. BMC Dermatol. 2012, 12, 13. [Google Scholar] [CrossRef] [PubMed]
- Eng, J.Y.; Moy, F.M. Validation of a Food Frequency Questionnaire to Assess Dietary Cholesterol, Total Fat and Different Types of Fat Intakes among Malay Adults. Asia Pac. J. Clin. Nutr. 2011, 20, 639–645. [Google Scholar] [PubMed]
- Gan, W.Y.; Mohd Nasir, M.T.; Zalilah, M.S.; Hazizi, A.S. Differences in Eating Behaviours, Dietary Intake and Body Weight Status between Male and Female Malaysian University Students. Malays. J. Nutr. 2011, 17, 213–228. [Google Scholar] [PubMed]
- Shahar, S.; Shafurah, S.; Shaari, N.S.A.H.; Rajikan, R.; Rajab, N.F.; Golkhalkhali, B.; Zainuddin, Z.M.D. Roles of Diet, Lifetime Physical Activity and Oxidative DNA Damage in the Occurrence of Prostrate Cancer among Men in Klang Valley, Malaysia. Asian Pac. J. Cancer Prev. 2011, 12, 605–611. [Google Scholar] [PubMed]
- Sulaiman, N.; Shariff, Z.M.; Jalil, R.A.; Taib, M.N.M.; Kandiah, M.; Samah, A.A. Validation of the Malaysian Coping Strategy Instrument to Measure Household Food Insecurity in Kelantan, Malaysia. Food Nutr. Bull. 2011, 32, 354–364. [Google Scholar] [CrossRef] [PubMed]
- Asma, A.; Nawalyah, A.G.; Rokiah, M.Y.; Mohd Nasir, M.T. Assessment of Diet Quality among Married Couples in a Selected Urban Area in Selangor. Malays. J. Community Health 2010, 16, 17–28. [Google Scholar]
- Lee, C.L.; Norimah, A.K.; Ismail, M.N. Association of Energy Intake and Macronutrient Composition with Overweight and Obesity in Malay Women from Klang Valley. Malays. J. Nutr. 2010, 16, 251–260. [Google Scholar] [PubMed]
- Pon, L.W.; Noor-Aini, M.Y.; Ong, F.B.; Adeeb, N.; Seri, S.S.; Shamsuddin, K.; Mohamed, A.L.; Hapizah, N.; Mokhtar, A.; Wan, H.W.H. Diet, Nutritional Knowledge and Health Status of Urban Middle-aged Malaysian Women. Asia Pac. J. Clin. Nutr. 2006, 15, 388–399. [Google Scholar] [PubMed]
- Wan Shakira, R.H.; Hasnan, A.; Ahamad, A.; Nur Liana, A.M.; Shubash, S. Change in Nutrient Intake after a Decade: Comparing Malaysian Adult Nutritional Survey, 2003 and 2014. Med. J. Malays. 2015, 70 (Suppl. 1), 63. Available online: http://www.e-mjm.org/2015/v70s1/mjm-sept-suppl-2185.html (accessed on 7 July 2017).
- Picca, A.; Pesce, V.; Lezza, A.M.S. Does Eating Less Make You Live Longer and Better? An Update on Calorie Restriction. Clin. Interv. Aging 2017, 12, 1887–1902. [Google Scholar] [CrossRef] [PubMed]
- Rizza, W.; Veronese, N.; Fontana, L. What are the Roles of Calorie Restriction and Diet Quality in Promoting Healthy Longevity? Ageing Res. Rev. 2014, 13, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Le Couteur, D.G.; Solon-Biet, S.; Cogger, V.C.; Mitchell, S.J.; Senior, A.; de Cabo, R.; Raubenheimer, D.; Simpson, S.J. The Impact of Low-Protein, High-Carbohydrate Diets on Aging and Lifespan. Cell. Mol. Life Sci. 2016, 73, 1237–1252. [Google Scholar] [CrossRef] [PubMed]
- Lafortune, L.; Martin, S.; Kelly, S.; Kuhn, I.; Remes, O.; Cowan, A.; Brayne, C. Behavioural Risk Factors in Mid-life Associated with Successful Aging, Disability, Dementia and Frailty in Later Life: A Rapid Systematic Review. PLoS ONE 2016, 11, e0144405. [Google Scholar] [CrossRef] [PubMed]
- Stein, P.K.; Soare, A.; Meyer, T.E.; Cangemi, R.; Holloszy, J.O.; Fontana, L. Caloric Restriction may Reverse Age-related Autonomic Decline in Humans. Aging Cell 2012, 11, 644–650. [Google Scholar] [CrossRef] [PubMed]
- Ruetenik, A.; Barrientos, A. Dietary Restriction, Mitochondrial Function and Aging: From Yeast to Humans. Biochim. Biophys. Acta 2015, 1847, 1434–1447. [Google Scholar] [CrossRef] [PubMed]
- Teng, N.I.; Shahar, S.; Manaf, Z.A.; Das, S.K.; Taha, C.S.; Ngah, W.Z. Efficacy of Fasting Calorie Restriction on Quality of Life Among Aging Men. Physiol. Behav. 2011, 104, 1059–1064. [Google Scholar] [CrossRef] [PubMed]
- Vanoh, D.; Shahar, S.; Din, N.C.; Omar, A.; Vyrn, C.A.; Razali, R.; Ibrahim, R.; Hamid, T.A. Predictors of Poor Cognitive Status among Older Malaysian Adults: Baseline Findings from the LRGS TUA Cohort Study. Aging Clin. Exp. Res. 2016, 29, 173–182. [Google Scholar] [CrossRef] [PubMed]
- Baharudin, A. Escalating Prevalence of Overweight and Obesity among Malaysian Adults: After a 10 Years Period. Med. J. Malays. 2015, 70 (Suppl. 1), 16. Available online: http://www.e-mjm.org/2015/v70s1/mjm-sept-suppl-2089.html (accessed on 7 July 2017).
- Yap, R.W.K.; Shidoji, Y.; Hon, W.M.; Masaki, M. Association and Interaction between Dietary Pattern and VEGF Receptor-2 (VEGFR2) Gene Polymorphisms on Blood Lipids in Chinese Malaysian and Japanese Adults. Asia Pac. J. Clin. Nutr. 2012, 21, 302–311. [Google Scholar] [PubMed]
- Chew, W.F.; Masyita, M.; Leong, P.P.; Boo, N.Y.; Zin, T.; Choo, K.B.; Yap, S.F. Prevalence of Obesity and its Associated Risk Factors among Chinese Adults in a Malaysian Suburban Village. Singapore Med. J. 2014, 55, 84–91. [Google Scholar] [CrossRef] [PubMed]
- Ramadas, A.; Kandiah, M. Food Intake and Colorectal Adenomas: A Case-Control Study in Malaysia. Asian Pac. J. Cancer Prev. 2009, 10, 925–932. [Google Scholar] [PubMed]
- Subahir, M.N.; Shah, S.A.; Zainuddin, Z. Risk Factors for Prostate Cancer in Universiti Kebangsaan Medical Centre: A Case-Control Study. Asian Pac. J. Cancer Prev. 2009, 10, 1015–1020. [Google Scholar] [PubMed]
- Mohamad Hasnan, A.; Khoo, Y.Y.; Yusuf, S.; Foo, L.H. Food Intake among Malaysian Adults: Are We Meeting Individualized Recommendations? Med. J. Malays. 2015, 70 (Suppl. 1), 66. [Google Scholar]
- Levine, M.E.; Suarez, J.A.; Brandhorst, S.; Balasubramanian, P.; Cheng, C.-W.; Madia, F.; Fontana, L.; Mirisola, M.G.; Guevara-Aguirre, J.; Wan, J.; et al. Low Protein Intake is Associated with a Major Reduction in IGF-1, Cancer, and Overall Mortality in the 65 and Younger but not Older Population. Cell Metab. 2014, 19, 407–417. [Google Scholar] [CrossRef] [PubMed]
- Willcox, D.C.; Scapagnini, G.; Willcox, B.J. Healthy Aging Diets Other than the Mediterranean: A Focus on the Okinawan Diet. Mech. Ageing Dev. 2014, 137, 148–162. [Google Scholar] [CrossRef] [PubMed]
- Le Couteur, D.G.; Solon-Biet, S.; Wahl, D.; Cogger, V.C.; Willcox, B.J.; Willcox, D.C.; Raubenheimer, D.; Simpson, S.J. New Horizons: Dietary Protein, Ageing and the Okinawan Ratio. Age Ageing 2016, 45, 443–447. [Google Scholar] [CrossRef] [PubMed]
- Index Mundi. Malaysia Palm Oil Domestic Consumption by Year. Available online: https://www.indexmundi.com/agriculture/?country=my&commodity=palm-oil&graph=domestic-consumption (accessed on 12 July 2018).
- Index Mundi. Malaysia Palm Kernel Oil Domestic Consumption by Year. Available online: https://www.indexmundi.com/agriculture/?commodity=palm-kernel-oil&graph=food-use-domestic-consumption-growth-rate (accessed on 12 July 2018).
- Department of Statistics Malaysia. Press Release: Statistics on Causes of Death, Malaysia 2017. Available online: https://www.dosm.gov.my/v1/index.php?r=column/pdfPrev&id=Y3psYUI2VjU0ZzRhZU1kcVFMMThGUT09 (accessed on 12 July 2018).
- Institute for Public Health (IPH). National Health and Morbidity Survey 2015 (NHMS 2015). Non-Communicable Diseases, Risk Factors & Other Health Problems; Ministry of Health: Putrajaya, Malaysia, 2015; Volume II, pp. 47–75. ISBN 978-983-2387-23-7. Available online: http://iku.moh.gov.my/images/IKU/Document/REPORT/nhmsreport2015vol2.pdf (accessed on 7 July 2017).
- Mancini, A.; Imperlini, E.; Nigro, E.; Montagnese, C.; Daniele, A.; Orru, S.; Buono, P. Biological and Nutritional Properties of Palm Oil and Palmitic Acid: Effects on Health. Molecules 2015, 20, 17339–17361. [Google Scholar] [CrossRef] [PubMed]
- DiNicolantonio, J.J.; Lucan, S.C.; O’Keefe, J.H. The Evidence for Saturated Fat and for Sugar Related to Coronary Heart Disease. Prog. Cardiovasc. Dis. 2016, 58, 464–472. [Google Scholar] [CrossRef] [PubMed]
- Chen, B.K.; Seligman, B.; Farquhar, J.W.; Goldhaber-Fiebert, J.D. Multi-country Analysis of Palm Oil Consumption and Cardiovascular Disease Mortality for Countries at Different Stages of Economic Development. Glob. Health 2011, 7, 45. [Google Scholar] [CrossRef] [PubMed]
- Ismail, S.R.; Maarol, S.K.; Ali, S.S.; Ali, A. Systematic Review of Palm Oil Consumption and the Risk of Cardiovascular Disease. PLoS ONE 2018, 13, e0193533. [Google Scholar] [CrossRef] [PubMed]
- Wattanapenpaiboon, N.; Wahlqvist, M.L. Phytonutrient Deficiency: The Place of Palm Fruit. Asia Pac. J. Clin. Nutr. 2003, 12, 363–368. [Google Scholar] [PubMed]
- Odia, O.J.; Ofori, S.; Maduka, O. Palm Oil and the Heart: A Review. World J. Cardiol. 2015, 7, 144–149. [Google Scholar] [CrossRef] [PubMed]
- Edem, D.O. Palm Oil: Biochemical, Physiological, Nutritional, Hematological, and Toxicological Aspects: A Review. Plant Foods Hum. Nutr. 2002, 57, 319–341. [Google Scholar] [CrossRef] [PubMed]
- Matalqah, L.; Radaideh, K.; Yusoff, Z.M.; Awaisu, A. Predictors of Breast Cancer among Women in a Northern State of Malaysia: A Matched Case-Control Study. Asian Pac. J. Cancer Prev. 2011, 12, 1549–1553. [Google Scholar] [PubMed]
- Yary, T.; Soleimannejad, K.; Rahim, F.A.; Kandiah, M.; Aazami, S.; Poor, S.J.; Wee, W.T.; Aazami, G. Contribution of Diet and Major Depression to Incidence of Acute Myocardial Infarction (AMI). Lipids Health Dis. 2010, 9, 133. [Google Scholar] [CrossRef] [PubMed]
- Kasim, N.M.; Ahmad, M.H.; Naidu, B.M.; Baharudin, A. Changes in Food Choices among Malaysian Adults: A Comparison between Malaysian Adults Nutrition Survey (MANS) 2003 and MANS 2014. Med. J. Malays. 2015, 70 (Suppl. 1), 64. [Google Scholar]
- Ahmad, M.H. Food Consumption Patterns: Findings from the Malaysian Adults Nutrition Survey (MANS) 2014. Med. J. Malays. 2015, 70 (Suppl. 1), 16. Available online: http://www.e-mjm.org/2015/v70s1/mjm-sept-suppl-2088.html (accessed on 7 July 2017).
- Pollock, N.K.; Bundy, V.; Kanto, W.; Davis, C.L.; Bernard, P.J.; Zhu, H.; Gutin, B.; Dong, Y. Greater Fructose Consumption is Associated with Cardiometabolic Risk Markers and Visceral Adiposity in Adolescents. J. Nutr. 2012, 142, 251–257. [Google Scholar] [CrossRef] [PubMed]
- Tchernof, A.; Despres, J.-P. Pathophysiology of Human Visceral Obesity: An Update. Physiol. Rev. 2013, 93, 359–404. [Google Scholar] [CrossRef] [PubMed]
- Amarra, M.S.V.; Khor, G.L.; Chan, P. Intake of Added Sugar in Malaysia: A Review. Asia Pac. J. Clin Nutr 2016, 25, 227–240. [Google Scholar] [CrossRef] [PubMed]
- Shahril, M.R.; Sulaiman, S.H.; Akmal, S.N. Healthy Eating Index and Breast Cancer Risk among Malaysian Women. Eur. J. Cancer Prev. 2013, 22, 342–347. [Google Scholar] [CrossRef] [PubMed]
- Shahar, S.; Normah, H.; Fatimah, A.; Nor Fadilah, R.; Ahmad Rohi, G.; Amin, I.; Cham, B.G.; Mohd Rizal, R.; Fairulnizal, M.N. Antioxidants Intake and Status, and Oxidative Stress in Relation to Breast Cancer Risks: A Case-Control Study. Asian Pac. J. Cancer Prev. 2008, 9, 343–349. [Google Scholar]
- Suzana, S., Jr.; Azhar, Y.; Fatimah, A. Association between Dietary Fibre and Cancer: A Case-Control Study in Malaysia. Malays. J. Nutr. 2004, 10, 173–182. [Google Scholar] [PubMed]
- Simpson, S.J.; Le Couteur, D.G.; Raubenheimer, D.; Solon-Biet, S.M.; Cooney, G.J.; Cogger, V.C.; Fontana, L. Dietary Protein, Aging and Nutritional Geometry. Ageing Res. Rev. 2017, 39, 78–86. [Google Scholar] [CrossRef] [PubMed]
- Raubenheimer, D.; Simpson, S.J. Nutritional Ecology and Human Health. Annu. Rev. Nutr. 2016, 36, 603–626. [Google Scholar] [CrossRef] [PubMed]
- Raubenheimer, D.; Simpson, S.J.; Tait, A.H. Match and Mismatch: Conservation Physiology, Nutritional Ecology and the Timescales of Biological Adaptation. Philos. Trans. R. Soc. B 2012, 367, 1628–1646. [Google Scholar] [CrossRef] [PubMed]
- Solon-Biet, S.M.; McMahon, A.C.; Ballard, J.W.O.; Ruohonen, K.; Wu, L.E.; Cogger, V.C.; Warren, A.; Huang, X.; Pichaud, N.; Melvin, R.G.; et al. The Ratio of Macronutrients, Not Caloric Intake, Dictates Cardiometabolic Health, Aging, and Longevity in Ad Libitum-fed Mice. Cell Metab. 2014, 19, 418–430. [Google Scholar] [CrossRef] [PubMed]
- FAO. Food Balance Sheets and the Food Consumption Survey: A Comparison of Methodologies and Results. Available online: http://www.fao.org/economic/the-statistics-division-ess/methodology/methodology-systems/food-balance-sheets-and-the-food-consumption-survey-a-comparison-of-methodologies-and-results/en/ (accessed on 12 July 2018).
- FAO. Uses of Food Consumption and Anthropometric Surveys in the Caribbean; Food and Agriculture Organization: Rome, Italy, 2004; Available online: http://www.fao.org/docrep/008/y5825e/y5825e00.htm#Contents (accessed on 2 July 2018).
- National Cancer Institute. Dietary Assessment Primer. Key Concepts about Measurement Error. Available online: https://dietassessmentprimer.cancer.gov/concepts/error/ (accessed on 7 July 2018).
- Paeratakul, S.; Popkin, B.M.; Kohlmeier, L.; Hertz-Picciotto, I.; Guo, X.; Edwards, L.J. Measurement Error in Dietary Data: Implications for the Epidemiologic Study of the Diet-Disease Relationship. Eur. J. Clin. Nutr. 1998, 52, 722–727. [Google Scholar] [CrossRef] [PubMed]
- National Cancer Institute. Usual Dietary Intakes: The NCI Method. Available online: https://epi.grants.cancer.gov/diet/usualintakes/method.html (accessed on 7 July 2018).
- National Research Council (US) Subcommittee on Criteria for Dietary Evaluation. Nutrient Adequacy: Assessment Using Food Consumption Surveys; National Academies Press (US): Washington, DC, USA, 1986; pp. 10–24. ISBN 0-309-03634-8. [Google Scholar]
- Ismail, M.N.; Ng, K.K.; Chee, S.S.; Roslee, R.; Zawiah, H. Predictive Equations for the Estimation of Basal Metabolic Rate in Malaysian Adults. Malays. J. Nutr. 1998, 4, 81–90. [Google Scholar]
- Hedrick, V.E.; Dietrich, A.M.; Estabrooks, P.A.; Savla, J.; Serrano, E.; Davy, B.M. Dietary Biomarkers: Advances, Limitations and Future Directions. Nutr. J. 2012, 11, 109. [Google Scholar] [CrossRef] [PubMed]
- Wong, W.W.; Roberts, S.B.; Racette, S.B.; Das, S.K.; Redman, L.M.; Rochon, J.; Bhapkar, M.V.; Clarke, L.L.; Kraus, W.E. The Doubly Labeled Water Method Produces Highly Reproducible Longitudinal Results in Nutrition Studies. J. Nutr. 2014, 144, 777–783. [Google Scholar] [CrossRef] [PubMed]
- Buchowski, M.S. Doubly Labeled Water is a Validated and Verified Reference Standard in Nutrition Research. J. Nutr. 2014, 144, 573–574. [Google Scholar] [CrossRef] [PubMed]

| Source (year) | Sample Size, Sample Characteristics, Sampling Method | Study Design | Dietary Assessment Method | Study Excluded Over-/Under Reporters of Energy Intake (Yes/No) | Approach to Determine Adequacy of Macronutrient Intake | Macronutrient (Carbohydrate, Protein, and Fat) Food Sources Identified | |||
|---|---|---|---|---|---|---|---|---|---|
| FAO food balance sheet (2013) [5] | n/a | n/a | Estimate per capita values for the supply of all food commodities (in kg/person/year) and the calories, protein, and fat content | n/a | n/a | Carbohydrate, protein, fat | |||
| Nationwide studies | Energy | Protein | Fat | Carbohydrate (CHO) | |||||
| Mahmud et al. (2015) [6] | MANS 2014 sample | Secondary analysis of MANS 2014 data | Single 24-h recall | --- | Prevalence of adults that met the RNI for energy | Prevalence of adults that met RNI for protein | Prevalence of adults that met RNI for fat | Prevalence of adults that met RNI for CHO | --- |
| MANS 2014 (2014) [7] | 2973 adults (1378 men, 1595 women) aged 18 to 59 y (not pregnant or lactating, no specific diet due to illness); multistage stratified cluster sampling | Cross-sectional survey | Single 24-h recall | Yes | Median (kcal/day), % RNI | Median g/day, % RNI | Median g/day, % energy from fat | Median g/day, % energy from CHO | Carbohydrate, protein |
| Asma (2014) [8] | Secondary analysis of MANS 2003 data; 3063 adults aged 18 to 59 year; multistage stratified cluster sampling | Cross-sectional survey | Semiquantitative FFQ (126 items) | Yes | Mean (kcal/day), % RNI | Mean g/day, % RNI | Mean g/day, % energy from fat | Mean g/day, % energy from CHO | --- |
| Mirnalini et al. (2008) [9] | 7349 adults (51% men, 49% women) aged 18 to 59 year; stratified random sampling | Cross-sectional survey | Single 24-h diet recall | No | Mean (kcal/day), % RNI of mean; median; 25th and 75th percentiles | Mean (g/day), % RNI of mean; median; 25th & 75th percentiles | Mean (g/day); median; 25th & 75th percentiles | Mean g/day; median; 25th and 75th percentiles | --- |
| Small studies | |||||||||
| Kaur et al. (2016) [10] | 101 adult volunteer Punjabis aged 18 to 59 y from central region of Malaysia; convenience sampling | Cross-sectional | 2-day diet record | No | --- | --- | Median (g/day), % energy from fat | Median (g/day), % energy from CHO | --- |
| Norsham et al. (2015) [11] | 450 women aged 30 to 65 year who participated in health screening in Klang Valley, Malays (68%), Chinese (25.1%), Indians (6.1%); convenience sampling | Cross-sectional | Diet history questionnaire (DHQ) | No | Mean (kcal/day), % of subjects meeting/not meeting RNI for energy | Mean (g/day), % of subjects with protein intake 10–35% energy; >35% energy | Mean (g/day), % of subjects with fat intake 25–35% energy; >35% energy | Mean (g/day); % of subjects with CHO intake 55 to 75% energy; >75% energy | --- |
| Shyam et al. (2015) [12] | 77 nondiabetic women with previous gestational diabetes, aged 20 to 40 year; | Experimental parallel group design | 3-day diet records at baseline | No | ---- | ---- | % energy from fat | % energy from CHO | --- |
| Karupaiah et al. (2013) [13] | 128 women (45 Malays, 56 Chinese, 27 Indians) aged 19 to 65 year; random selection of clusters and blocks, convenience sample of volunteer households | Cross-sectional | 3-day diet records for two weekdays, one weekend | Yes | Mean (kcal/day), % RNI | Mean (g/day), % RNI | --- | --- | --- |
| Shahril et al. (2013) [14] | 380 university students from four public universities in East Coast of Malaysia, aged 18 to 24 year, 47 males, 333 females; generally healthy; random sampling | Experimental parallel group design (only baseline data were used) | Diet history in the last 7 days | Yes | --- | --- | % energy from fat | % energy from CHO | Carbohydrate, protein, fat |
| Yee et al. (2013) [15] | 73 healthy Chinese premenopausal women aged 30 to 45 year from Klang Valley; convenience sampling | Cross-sectional | Single 24-h recall | No | Mean (kcal/day) vs. RNI = 2180 kcal/day | Mean (g/day) vs. RNI = 55 g/day | Mean (g/day), % energy from fat | Mean (g/day), % energy from CHO | --- |
| Abdull Hakim et al. (2012) [16] | 200 adult students from Universiti Teknologi MARA (UiTM), Universiti Putra Malaysia (UPM), Universiti of Selangor (UNISEL), Management and Science University (MSU) aged 18 to 24 year, 90 males, 110 females; not pregnant, bedridden, or having major physical activity problem; convenience sampling | Cross-sectional | Single 24-h recall | No | Mean (kcal/day), % of subjects with intake < RNI, meet RNI, >RNI | Mean (g/day), % of subjects with intake < RNI, meet RNI, >RNI | Mean (g/day), % of subjects with intake < RNI, meet RNI, >RNI | --- | Carbohydrates (fruits & vegetables) |
| Ismail et al. (2012) [17] | 88 adults aged 18 to 30 year with and without acne vulgaris attending a tertiary hospital Dermatology Clinic in Kuala Lumpur without chronic disease; purposive sampling | Case control, cross-sectional | 3-day food diary (two weekdays, one weekend) | No | --- | % energy from protein | % energy from fat | % energy from CHO | --- |
| Eng & Moy (2011) [18] | 151 Malay adults, 39 males, 112 females aged 49.9 ± 4.1 year participating in a worksite Wellness Programme in Kuala Lumpur; random sampling | Cross-sectional | 3-day diet record (two weekdays, one weekend) | No | --- | --- | Mean (g/day) for total fat, saturated fat (SFA), & polyunsaturated fat (PUFA), % energy from fat, SFA, PUFA | --- | Fat (saturated, monounsaturated (MUFA), PUFA) |
| Gan et al. (2011) [19] | 584 students aged 18 to 24 year from four universities in Klang Valley, 237 males, 347 females; multistage stratified random sampling | Cross-sectional | Two 24-h recalls for 1 weekday, 1 weekend | Yes | Mean (kcal/day), % RNI, % of subjects with intake < RNI & ≥RNI | Mean (g/day), % RNI, % of subjects with energy from protein at <10%, 10–15%, >15% | Mean (g/day), % energy from fat, % of subjects with energy from fat <20%, 20–30%, >30% | Mean (g/day), % energy from CHO, % of subjects with energy from CHO at <55%, 55–70%, >70% | Carbohydrate, protein |
| Shahar et al. (2011) [20] | 70 healthy men aged 40 to 80 year, without past medical history of prostate cancer and not suffering from any unstable chronic diseases, recruited from Kuala Lumpur Hospital and Universiti Kebangsaan Malaysia Medical Centre in Klang Valley; purposive sampling | Case control, cross-sectional | Validated diet history questionnaire | No | --- | --- | Mean (g/day), % energy from fat | Mean (g/day), % energy from CHO | --- |
| Sulaiman et al. (2011) [21] | 301 Malay women aged 21 to 49 year, not pregnant or lactating, living in rural (n = 151) and urban (n = 150) areas in Kelantan; multistage random sampling | Cross-sectional | Single 24-h recall | No | Mean (kcal/day), % RNI | Mean (g/day), % RNI | Mean (g/day), % energy from fat | Mean (g/day), % energy from CHO | Carbohydrate, protein |
| Asma et al. (2010) [22] | 150 married couples from Selangor aged 20 y and above; not practicing any special diet; purposive sampling | Cross-sectional | Two 24-h recalls | No | --- | --- | Mean (g/day), % energy from fat and saturated fat | --- | Carbohydrate, fat (saturated) |
| Lee et al. (2010) [23] | 115 women aged 18 to 59 year working in Klang Valley (six offices of the Employees Provident Fund); purposive sampling | Cross-sectional | Diet history over 7 days | Yes | --- | --- | Mean (g/day), % energy from fat | Mean (g/day), % energy from CHO | --- |
| Pon et al. (2006) [24] | 360 disease-free women aged ≥ 45 year, non-HRT users with intact uterus; living in a suburb in Kuala Lumpur; convenience sampling for a multicenter study | Cross-sectional | Quantitative FFQ | Yes | Mean (kcal/day), % RDA | Mean (g/day), % RDA | --- | --- | Carbohydrate, protein |
| Source | Energy Consumption Level | Macronutrient Consumption Level | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Protein | Fat | Carbohydrate | ||||||||||
| Met RNI | Below RNI | Above RNI | Met RNI | Below RNI | Above RNI | Met RNI | Below RNI | Above RNI | Met RNI | Below RNI | Above RNI | |
| FAO food balance sheet (2013) [5] | †† | †† | 127% adequacy for 2014–2016 | †† | †† | Available protein supply in 2013 = 81.58 g/capita/day | Per capita fat supply was 28% of energy | †† | †† | Per capita CHO supply was 63% of energy | †† | †† |
| Nationwide studies | ||||||||||||
| Mahmud et al. (2015) [6] | --- | 66.5% of adults had energy intakes below the RNI | --- | --- | --- | 50.7% of adults had protein intake exceeding the RNI | --- | --- | 94.9% of adults exceeded the RNI for fat | --- | 53.5% of adults had CHO intake below RNI | --- |
| Asma (2014) analysis of MANS 2003 data [8] | †† | †† | Mean energy intake was 101% RNI for men and 100.8% RNI for women | †† | †† | Protein intake was 180.4% RNI for men and 171.2% RNI for women | †† | †† | Fat intake was 120% RNI for men and 111.8% for women | †† | †† | CHO intake was 74.4% TEI for men and 74.9% TEI for women |
| Mirnalini et al. (2008) [9] | †† | Energy intake ranged from 66.6% to 75.1% RNI for men and 62.4% to 76% RNI for women | †† | Protein intake ranged from 98.4% to 108.1% RNI for men and 92.7% to 103.6% RNI for women | †† | †† | ** | ** | ** | ** | ** | ** |
| MANS 2014 (2014) [7] | †† | Energy intake for both sexes was 64.4% of RNI | †† | Protein intake was 97.7% RNI (both sexes) | †† | Protein intake among men was 101.3% RNI | Fat intake was 29% TEI | †† | †† | CHO intake was 55% TEI | †† | †† |
| Small studies | ||||||||||||
| All ages | ||||||||||||
| Kaur et al. (2016) [10] | ** | ** | ** | ** | ** | ** | †† | †† | Fat intake was 30.3% TEI | CHO intake was 54.6% TEI | †† | †† |
| Young adults | ||||||||||||
| Shahril et al. (2013) [14] | ** | ** | ** | ** | ** | ** | †† | †† | Fat intake was 34.0% TEI in intervention group and 34.4% TEI in control group | CHO intake was 51.9% TEI in intervention group and 51.6% TEI in control group | †† | †† |
| Karupaiah et al. (2013) [13] | Energy intake was 93% RNI for age 19 to 29 year and 84% RNI for age 30 to 50 year | †† | †† | †† | †† | Protein intake was 129% RNI for age 19 to 50 year | ** | ** | ** | ** | ** | ** |
| Abdull Hakim et al. (2012) [16] | --- | 90.9% of males and 72.2% of females had energy intake below RNI | --- | --- | 68% of females had protein intake below RNI | 56.4% of males had protein intake above RNI | 21.1% of males and 14.6% of females met RNI for fat | --- | 56.5% of females and 41.5% of males exceeded RNI for fat | †† | †† | †† |
| Ismail et al. (2012) [17] | ** | ** | ** | ** | ** | ** | †† | †† | Fat intake ranged from 31.9% to 33.7% RNI | CHO intake ranged from 50.5% to 53.1% TEI | †† | †† |
| Gan et al. (2011) [19] | --- | 73% of males and 80.5% of females had energy intake below RNI | --- | --- | --- | 74.7% of males and 54.4% of females had protein intake above RNI | 42.6% of males and 45.5% of females had fat intake between 20 to 30% TEI | --- | 35.9% of males and 27.7% of females had fat intake >30% TEI | --- | 64.6% of men and 60.6% of women had CHO intake <55% TEI | --- |
| Older adults | ||||||||||||
| Shyam et al. (2015) [12] | ** | ** | ** | ** | ** | ** | Baseline fat intake was 29% TEI in LGI group and 30% TEI in CHDR group | †† | †† | CHO intake ranged from 53% to 55% TEI | †† | †† |
| Norsham et al. (2015) [11] | 51% of women met RNI for energy | ---- | --- | --- | --- | 64.4% of normal women and 70.9% of women with breast adiposity had protein intake above RNI | --- | --- | Fat intake was >35% TEI in 87% of normal women and 79% of women with breast adiposity | --- | --- | CHO intake was >75% TEI in 82% of normal women and 83.5% of women with breast adiposity |
| Yee et al. (2013) [15] | †† | Mean energy intake fell below the RNI | †† | †† | †† | Mean protein intake exceeded the RNI | †† | †† | Mean fat intake was 36% TEI | ** | ** | ** |
| Karupaiah et al. (2013) [13] | †† | Energy intake was 78% RNI for age 51 to 59 year | †† | †† | †† | Protein intake was 129% RNI for age 51 to 59 year | ** | ** | ** | ** | ** | ** |
| Shahar et al. (2011) [20] | ** | ** | ** | ** | ** | ** | Fat intake was 25.1% energy | †† | †† | CHO intake was 58.8% TEI | --- | --- |
| Eng & Moy (2011) [18] | ** | ** | ** | ** | ** | ** | †† | †† | Fat intake was 32.8% TEI | ** | ** | ** |
| Sulaiman et al. (2011) [21] | Energy intake was 90.15% RNI among food secure rural respondents | Energy intake ranged from 53.99% to 77.44% RNI among food secure urban and food insecure urban and rural respondents | †† | †† | †† | Protein intake ranged from 100.06% to 154.42% RNI for food secure and food-insecure women in urban and rural areas | Fat intake of food insecure (rural & urban) and food secure urban women ranged from 23.55% to 29.62% TEI | †† | Fat intake of food secure rural respondents was 32.38% TEI | CHO intake in food secure and insecure women in rural and urban areas ranged from 50% TEI to 59% TEI | --- | --- |
| Lee et al. (2010) [23] | ** | ** | ** | ** | ** | ** | †† | †† | Fat intake ranged from 31.0% to 33.5% TEI | CHO intake ranged from 54.4% TEI to 55.9% TEI | --- | --- |
| Asma et al. (2010) [22] | ** | ** | ** | ** | ** | ** | Fat intake was 28.6% TEI for men and 29.7% TEI for women | †† | †† | ** | ** | ** |
| Pon et al. (2006) [24] | Energy intake was 88.5% RDA | †† | †† | †† | †† | Protein intake was 144% of RDA | ** | ** | ** | ** | ** | ** |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shahar, S.; Jan Bin Jan Mohamed, H.; De los Reyes, F.; Amarra, M.S. Adherence of Malaysian Adults’ Energy and Macronutrient Intakes to National Recommendations: A Review and Meta-Analysis. Nutrients 2018, 10, 1584. https://doi.org/10.3390/nu10111584
Shahar S, Jan Bin Jan Mohamed H, De los Reyes F, Amarra MS. Adherence of Malaysian Adults’ Energy and Macronutrient Intakes to National Recommendations: A Review and Meta-Analysis. Nutrients. 2018; 10(11):1584. https://doi.org/10.3390/nu10111584
Chicago/Turabian StyleShahar, Suzana, Hamid Jan Bin Jan Mohamed, Francisco De los Reyes, and Maria Sofia Amarra. 2018. "Adherence of Malaysian Adults’ Energy and Macronutrient Intakes to National Recommendations: A Review and Meta-Analysis" Nutrients 10, no. 11: 1584. https://doi.org/10.3390/nu10111584
APA StyleShahar, S., Jan Bin Jan Mohamed, H., De los Reyes, F., & Amarra, M. S. (2018). Adherence of Malaysian Adults’ Energy and Macronutrient Intakes to National Recommendations: A Review and Meta-Analysis. Nutrients, 10(11), 1584. https://doi.org/10.3390/nu10111584





