Systematic Review of Smart Elderly Care in Digital Environments: Toward Sustainable Wellbeing for Older Adults
Abstract
1. Introduction
- (1)
- What intellectual bases support the field of smart elderly care?
- (2)
- What research fronts have formed within this domain?
- (3)
- What thematic foci dominate current scholarship?
- (4)
- What future research pathways are needed to advance the field?
2. Materials and Methods
2.1. Data Collection
2.2. Data Analysis
2.2.1. Co-Citation Analysis and Its Implementation in CiteSpace
2.2.2. Content Analysis and Its Implementation in Leximancer
3. Results
3.1. Findings of the Bibliometric Analysis
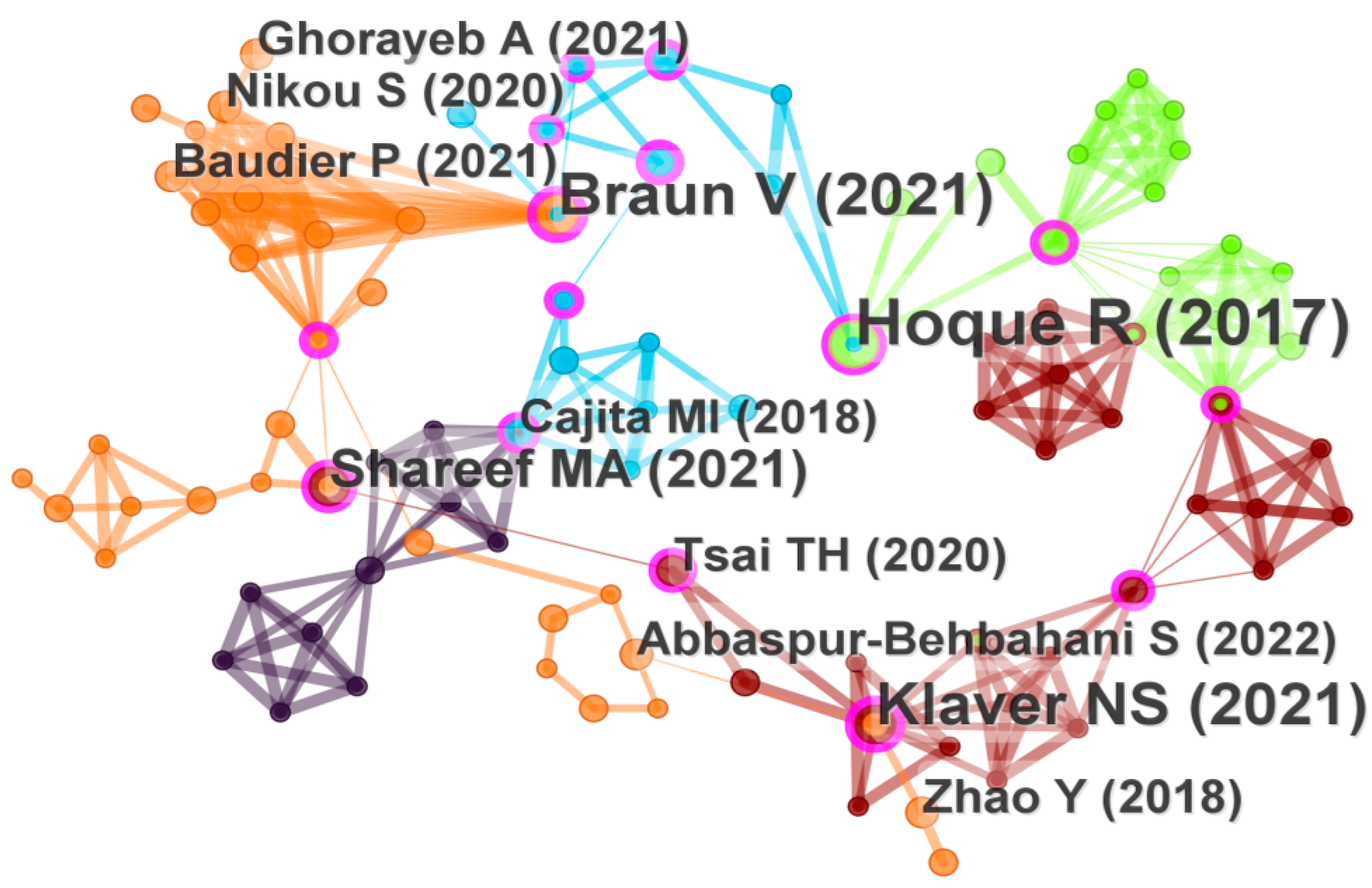
3.1.1. Landmark References as Intellectual Bases
| Rank | Citation Count | Centrality | Authors (Year) | Fields |
|---|---|---|---|---|
| 1 | 6 | 0.21 | Hoque and Sorwar (2017) [37] | Medical Informatics |
| 2 | 5 | 0.30 | Braun and Clarke (2021) [47] | Research method |
| 3 | 5 | 0.20 | Klaver et al. (2021) [38] | Healthcare |
| 4 | 4 | 0.10 | Shareef et al. (2021) [41] | Information Systems |
| 5 | 3 | 0.18 | Cajita et al. (2018) [39] | Medical Informatics |
| 6 | 3 | 0.08 | Baudier et al. (2021) [46] | Information Systems |
| 7 | 3 | 0.08 | Tsai et al. (2020) [43] | Medical Informatics |
| 8 | 3 | 0.05 | Ghorayeb et al. (2021) [42] | Computer Science |
| 9 | 3 | 0.02 | Zhao et al. (2018) [40] | Information Systems |
| 10 | 2 | 0.23 | Kavandi and Jaana (2020) [49] | Healthcare |
| 11 | 2 | 0.22 | Zhang et al. (2017) [48] | Medical Informatics |
| 12 | 2 | 0.21 | Teh et al. (2017) [50] | Information Systems |
3.1.2. Six Knowledge Clusters: Mapping the Research Front Structure
3.2. Key Findings from the Content Analysis
4. Discussion
4.1. Operationalizing of Smart Elderly Care
4.2. Intellectual Base of Smart Elderly Care
4.3. Factors Related to Smart Elderly Care Research Fronts
4.4. Consequences of Smart Elderly Care
4.5. Research Method and Field of Smart Elderly Care
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AAL | Ambient-Assisted Living |
| AI | Artificial Intelligence |
| ATM | Autonomous Trust Model |
| DHPs | Digital Healthcare Platforms |
| eHealth | Electronic Health |
| EHR | Electronic Health Record |
| HBM | Health Belief Model |
| ICT | Information and Communication Technology |
| IRT | Innovation Resistance Theory |
| ISS model/IS success model | Information Systems Success Model |
| mHealth | Mobile Health |
| WHTs | Wearable Health Technologies |
| OHCs | Online Health Communities |
| PMT | Protection Motivation Theory |
| SARs | Socially Assistive Robots |
| SEM | Structural Equation Modeling |
| SMECS | Smart Medical and Elderly Care Systems |
| S–O–R | Stimulus–Organism–Response |
| TAM | Technology Acceptance Model |
| TCM | Traditional Chinese Medicine |
| UTAUT | Unified Theory of Acceptance and Use of Technology |
| UTAUT2 | Extended Unified Theory of Acceptance and Use of Technology |
| VR | Virtual Reality |
Appendix A
| Authors (Year) | Context | Age Range | Research Design | Main Related Concepts |
|---|---|---|---|---|
| Jeng et al. (2020) [89] | Smart bracelets | 60+ | Qualitative | Means–end chain theory, older adults’ perceived value (attribute functions, consequent benefits and value goals) |
| Jaana and Pare (2020) [67] | mHealth | 65+ | Quantitative | Expectation-confirmation theory, initial expectations, perceived ease of use, perceived usefulness, satisfaction, intention to continue |
| Vandemeulebroucke et al. (2020) [88] | Socially assistive robots (SARs) | 70+ | Qualitative | Older adults’ multidimensional perceptions (such as components of a techno-societal evolution, embeddedness in aged-care dynamics, and embodiments of ethical considerations) |
| Hawley et al. (2020) [113] | Telehealth | 65+ | Qualitative | Patient-perceived barriers (interest, access to care, access to technology, and confidence) |
| Askari et al. (2020) [62] | Medical apps | 65+ | Quantitative | TAM, perceived usefulness, perceived ease of use, attitude toward use, subjective norm, sense of control, personal innovativeness, social relationships, self-perceived effectiveness, service availability, facilities, feelings of anxiety, intention to use |
| Verloo et al. (2020) [114] | Gerontechnology | 65+ | Qualitative | Older adults’ perception (preferring technologies related to their mobility and safety and those that would help slow down their cognitive decline) |
| Lin et al. (2020) [90] | mHealth | 58+ | Qualitative | TAM, perceived usefulness, ease of use, compatibility, technology anxiety, financial cost, and self-efficacy |
| Ko and Chou (2020) [70] | eHealth | 51+ | Quantitative | Information systems success model (ISS model), the five dimensions of service quality (tangibles, reliability, responsiveness, assurance, empathy), and satisfaction with service quality |
| Kim and Han (2021) [86] | Health apps | 60+ | Quantitative | Social cognitive theory, healthcare technology self-efficacy, outcome expectations (including physical, social, and self-evaluative dimensions), privacy risk, self-regulatory behavior, and continuance intention |
| Huang et al. (2021) [66] | Gerontechnology | 60+ | Mixed-method | TAM, Health Behavioral Model (HBM), need factors (assessed need, perceived need), resources accessibility (cost, community services, health policy), predictive factors (personal characteristics, health belief), products characteristic (usability, reliability), and adoption intention |
| Wilson et al. (2021) [14] | eHealth | 60+ | Literature review | UTAUT2, barriers (a lack of self-efficacy, knowledge, support, functionality, and information provision about the benefits), and facilitators (active engagement, support for overcoming concerns privacy and enhancing self-efficacy, and integration to accommodate the multi-morbidity with which older adults typically present) |
| Klaver et al. (2021) [38] | mHealth | 65+ | Quantitative | TAM, UTAUT, privacy risk, performance risk, legal concern, trust, intention to use |
| Liu et al. (2021) [115] | Social robots | 60+ | Quantitative | Perceived competence and perceived warmth |
| Wilkowska et al. (2021) [72] | Assistive technology | 60+ | Quantitative | Age (60–69 years vs. 70+ years), health status (healthy vs. chronic illness), gender (male vs. female), acceptance of health-supporting technologies |
| Wang et al. (2021) [74] | Aged-care products | 55+ | Quantitative | ISS model, attachment theory, perceived information quality, perceived system quality, perceived service quality, self-perception of ageing, self-perception of ageing, emotional attachment, willingness to use |
| Johnson et al. (2021) [116] | mHealth | 65+ | Qualitative | Previous experience, care environment, personal values, knowledge, support systems, app usability, life stage, and friend or family history |
| Talukder et al. (2021) [59] | Wearable Health Technologies (WHTs) | 65+ | Quantitative | Theory of consumption values, enabler-inhibitor perspective, functional value (including device quality and convenience value. social value. epistemic value. emotional value, continued use intention |
| Cross et al. (2021) [117] | Patient portals electronic health record (EHR) | 65+ | Quantitative | TAM, expectation-confirmation theory, level of patient portal use (none, moderate, extensive, self-rated health care quality) |
| Ghorayeb et al. (2021) [42] | Smart home | 65+ | Qualitative | Older people’s views and expectations |
| Ali et al. (2021) [58] | eHealth | 65+ | Quantitative | Age, gender, education level, employment status, household income, health status, disability severity, ICT access, eHealth use |
| Shareef et al. (2021) [41] | Autonomous homecare system | —— | Quantitative | Autonomous trust model (ATM), technological uncertainty and Reliability, self-Concept and behavioral attitude, personal benefit and accomplishment, personal ability and control, empathetic cooperation and social interaction, trust, behavioral intention |
| Huang et al. (2022) [73] | Smart senior care | 60+ | Quantitative | Age, number of children, frequency of children visiting parents, perceived adequacy of senior care received, self-reported health, chronic diseases, smartphone use, attitude towards smart senior care, willingness of older adults to choose smart senior care |
| Rój (2022) [82] | eHealth | 60+ | Quantitative | UTAUT, performance expectancy, effort expectancy, social influence, acceptance and use of eHealth |
| Zhou et al. (2022) [118] | Wisdom healthcare | —— | Mixed-method | Knowledge gap theory, digital divide (including digital access gap, digital use gap, and digital knowledge gap), AI and big data, value perception, satisfaction with wisdom healthcare services |
| van Elburg et al. (2022) [63] | mHealth | 65+ | Quantitative | TAM, perceived usefulness, perceived ease of use, attitude toward use, sense of control, personal innovativeness, self-perceived effectiveness, service availability, facilitating circumstances, gender, intention to use |
| Camp et al. (2022) [91] | In-home monitoring technology | 55+ | Qualitative | Older adults’ perceptions (personal hygiene, feeding, and socializing) |
| Jeng et al. (2022) [68] | Smart health wearable devices | 60+ | Quantitative | TAM, technology readiness, technology interactivity, perceived usefulness, perceived ease of use, technology anxiety, attitude, intention to use |
| Alam and Khanam (2022) [69] | mHealth | 46+ | Quantitative | TAM, perceived usefulness, perceived ease of use, perceived reliability, price value, technology anxiety, behavioral intention, actual usage behavior |
| Ma and Zuo (2022) [75] | OHCs | 50+ | Quantitative | Dual-process model, direct informational support, indirect informational support, direct emotional support, indirect emotional support, habit, continued participation |
| Rodríguez-Fernández et al. (2022) [119] | Telemedicine | 65+ | Quantitative | TAM, UTAUT, chronic conditions (e.g., cancer, hypertension, diabetes), mood disorders (depression and anxiety), age, gender, race/ethnicity, education level, marital status, telemedicine readiness |
| Pirzada et al. (2022) [120] | Smart homes | —— | Literature review | Four key criteria of smart elderly care (be personalized toward their needs, protect their dignity and independence, provide user control, and not be isolating) |
| Wang et al. (2023) [76] | Internet + traditional Chinese medicine | 60+ | Mixed-method | Attitude, knowledge cognition, and digital literacy, demand for TCM nursing services |
| Choi et al. (2023) [121] | Smart silver care | 65+ | Quantitative | ADDIE model, emotional support, cognition, physical activity, health data, nutrition, and motivation |
| Tandon et al. (2024) [71] | mHealth | 60+ | Quantitative | Self-determination theory, gamification, usability (including error prevention, completeness, memorability, learnability, and customization), empathetic cooperation and social interaction, engagement, continued use intention |
| Ren and Zhou (2023) [64] | Virtual nursing home | 60+ | Quantitative | UTAUT, TAM, performance expectancy, effort expectancy, social influence, facilitating conditions, conformist mentality, attitude, behavioral intention |
| He et al. (2023) [95] | SARs | 60+ | Quantitative | TAM, perceived usefulness, perceived ease of use, perceived enjoyment, whether to use mobile devices, attitude, intention to use |
| van Elburg et al. (2023) [65] | mHealth | 65+ | Quantitative | TAM, perceived usefulness, perceived ease of use, attitude toward use, subjective norm, sense of control, feelings of anxiety, personal innovativeness, social relationships, self-perceived effectiveness, service availability, facilitating circumstances, intention to use |
| Shareef et al. (2023) [85] | Machine autonomy | 65+ | Quantitative | ATM, expected personal ability and control, expected technological uncertainty, family benefit and accomplishment, expected empathetic cooperation and social interaction, self-concept and personality & image, trust, behavioral intention |
| Wang et al. (2023) [83] | Smart aged-care products | 60+ | Quantitative | UTAUT, performance expectancy, effort expectancy, social influence, facilitating conditions, perceived cost, perceived risk, behavioral intention, use behavior |
| Berridge et al. (2023) [77] | AI companion robots | —— | Quantitative | Age, education level, history of memory problems, number of chronic conditions, computer use confidence, social activity level, perceptions |
| Wang et al. (2023) [122] | mHealth | 60+ | Quantitative | TAM, Protection motivation theory (PMT), Perceived risk theory, perceived ease of use, perceived usefulness, perceived susceptibility, perceived severity, perceived risk, attitude, behavioral intention |
| Frishammar et al. (2023) [92] | Digital healthcare platforms (DHPs) | 65+ | Qualitative | UTAUT2, negative attitudes, technology anxiety, lack of trust |
| Cao et al. (2023) [123] | Smart medical and elderly care systems (SMECS) | 50+ | Quantitative | Stimulus-organism-response (S-O-R), price, operability, personalisation, perceived risk, perceived value, continuous participation |
| Koo et al. (2023) [124] | mHealth | 60+ | Quantitative | UTAUT, performance expectancy, social influence, facilitating conditions, device trust, chronic disease (Y/N), performance expectancy, behavioral intention |
| Yang et al. (2023) [79] | Digital health Technologies | 50+ | Quantitative | Age, gender, education level, marital status, employment status, exercise, medical insurance, income, life satisfaction, history of illness, willingness to use and willingness to pay |
| Zafrani et al. (2023) [80] | SARs named Gymmy | 65+ | Quantitative | Trust (including trust in the robot’s functional capabilities and social aspects) and technophobia (including personal failure, human vs. machine ambiguity, and inconvenience), quality evaluation (including pragmatic quality, hedonic quality, and attractiveness) |
| Chiu et al. (2023) [87] | VR | 65+ | Quantitative | VR training intervention |
| Frishammar et al. (2023) [78] | DHPs | 60+ | Mixed-method | TAM, perceived usefulness, perceived ease of use, digital maturity, trust, usage behavior |
| Afifi et al. (2023) [94] | VR | 54+ | Quantitative | VR improvements (older adults’ affect and stress, relationship with their family member, and overall quality of life) |
| Sancho-Esper et al. (2023) [125] | VR | 70+ | Mixed-method | TAM, perceived ease of use, perceived usefulness, technology anxiety, attitude, intention to use, intention to recommend |
| Sun et al. (2023) [126] | Mobile health services (MHS) | 60+ | Quantitative | PMT, S-O-R, fear appeal, coping appeal, fear Arousal, perceived usefulness, adoption intention |
| Li et al. (2024) [81] | Smart health services | 60+ | Quantitative | TAM, technical trust, security trust, privacy trust, family support, community support, service support. perceived usefulness, perceived ease of use, health expectations, attitude, intention to use |
| Chen et al. (2024) [2] | Smart elderly care | 60+ | Quantitative | Social Support theory, smart elderly care, social support, quality of life |
| Leung et al. (2024) [84] | mHealth | 60+ | Mixed-method | IRT, medical management task support, dietary task support, and exercise task support, perceived usefulness and technology anxiety, adoption intention |
| Zhang et al. (2024) [93] | Cameras | 55+ | Mixed-method | Older adults’ privacy concerns (data privacy, ageing, and their ability to use digital technology) |
References
- World-Health-Organization. Ageing and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 1 May 2025).
- Chen, X.; Wu, M.L.; Wang, D.B.; Zhang, J.; Qu, B.; Zhu, Y.X. Association of smart elderly care and quality of life among older adults: The mediating role of social support. BMC Geriatr. 2024, 24, 8. [Google Scholar] [CrossRef] [PubMed]
- Fang, E.F.; Xie, C.; Schenkel, J.A.; Wu, C.; Long, Q.; Cui, H.; Aman, Y.; Frank, J.; Liao, J.; Zou, H.; et al. A research agenda for ageing in China in the 21st century (2nd edition): Focusing on basic and translational research, long-term care, policy and social networks. Ageing Res. Rev. 2020, 64, 101174. [Google Scholar] [CrossRef]
- Xiao, M.; Liu, H. The Impact Mechanism of Government Regulation on the Operation of Smart Health Senior Care Service Platform: A Perspective from Evolutionary Game Theory. Int. J. Health Policy Manag. 2025, 14, 8646. [Google Scholar] [CrossRef] [PubMed]
- Verified-Market-Reports. Smart Elderly Care System Market Insights; Verified Market Reports: Pune, India, 2025. [Google Scholar]
- Rybenská, K.; Knapová, L.; Janiš, K.; Kühnová, J.; Cimler, R.; Elavsky, S. SMART technologies in older adult care: A scoping review and guide for caregivers. J. Enabling Technol. 2024, 18, 200–222. [Google Scholar] [CrossRef]
- Whittaker, L.; Mulcahy, R.; Letheren, K.; Kietzmann, J.; Russell-Bennett, R. Mapping the deepfake landscape for innovation: A multidisciplinary systematic review and future research agenda. Technovation 2023, 125, 102784. [Google Scholar] [CrossRef]
- Ng, S.W.T.; Zhang, R. Trust in AI chatbots: A systematic review. Telemat. Inform. 2025, 97, 102240. [Google Scholar] [CrossRef]
- Chen, H.L.; Hagedorn, A.; An, N. The development of smart eldercare in China. Lancet Reg. Health-West. Pac. 2023, 35, 7. [Google Scholar] [CrossRef]
- Kachouie, R.; Sedighadeli, S.; Khosla, R.; Chu, M.-T. Socially assistive robots in elderly care: A mixed-method systematic literature review. Int. J. Hum. Comput. Interact. 2014, 30, 369–393. [Google Scholar] [CrossRef]
- Zhu, J.H.; Shi, K.Y.; Yang, C.Y.; Niu, Y.P.; Zeng, Y.C.; Zhang, N.; Liu, T.; Chu, C.H. Ethical issues of smart home-based elderly care: A scoping review. J. Nurs. Manag. 2022, 30, 3686–3699. [Google Scholar] [CrossRef]
- Guo, B.; Shukor, N.S.A.; Ishak, I.S. Systematic literature review of healthcare services for the elderly: Trends, challenges, and application scenarios. Int. J. Public Health 2023, 12, 1637–1646. [Google Scholar] [CrossRef]
- Xie, L.; Zhang, W. Research Progress in Artificial Intelligence-Assisted Smart Elderly Care Service Design: A Bibliometric Analysis. In Proceedings of the 2025 5th International Conference on Artificial Intelligence and Industrial Technology Applications (AIITA), Xi’an, China, 28–30 March 2025; pp. 1280–1284. [Google Scholar]
- Wilson, J.; Heinsch, M.; Betts, D.; Booth, D.; Kay-Lambkin, F. Barriers and facilitators to the use of e-health by older adults: A scoping review. BMC Public Health 2021, 21, 12. [Google Scholar] [CrossRef]
- Liu, X.Y.; Chau, K.Y.; Liu, X.X.; Wan, Y. The progress of smart elderly care research: A scientometric analysis based on CNKI and WOS. Int. J. Environ. Res. Public Health 2023, 20, 21. [Google Scholar] [CrossRef] [PubMed]
- Randhawa, K.; Wilden, R.; Hohberger, J. A bibliometric review of open innovation: Setting a research agenda. J. Prod. Innov. Manag. 2016, 33, 750–772. [Google Scholar] [CrossRef]
- Ellegaard, O.; Wallin, J.A. The bibliometric analysis of scholarly production: How great is the impact? Scientometrics 2015, 105, 1809–1831. [Google Scholar] [CrossRef] [PubMed]
- United-Nations. World Population Ageing 2023: Challenges and Opportunities of Population Ageing in the Least Developed Countries; United Nations: New York City, NY, USA, 2023. [Google Scholar]
- Tajudeen, F.; Bahar, N.; Pin, T.; Saedon, N. Mobile technologies and healthy ageing: A bibliometric analysis on publication trends and knowledge structure of mHealth research for older adults. Int. J. Hum. Comput. Interact. 2022, 38, 118–130. [Google Scholar] [CrossRef]
- Vrontis, D.; Christofi, M. R&D internationalization and innovation: A systematic review, integrative framework and future research directions. J. Bus. Res. 2021, 128, 812–823. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.; Grp, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement (Reprinted from Annals of Internal Medicine). Phys. Ther. 2009, 89, 873–880. [Google Scholar] [CrossRef]
- Yang, Y.; Ngai, E.; Wang, L. Resistance to artificial intelligence in health care: Literature review, conceptual framework, and research agenda. Inf. Manag. 2024, 61, 103961. [Google Scholar] [CrossRef]
- Frizzo-Barker, J.; Chow-White, P.A.; Adams, P.R.; Mentanko, J.; Ha, D.; Green, S. Blockchain as a disruptive technology for business: A systematic review. Int. J. Inf. Manag. 2020, 51, 102029. [Google Scholar] [CrossRef]
- Xiao, Y.; Watson, M. Guidance on conducting a systematic literature review. J. Plan. Educ. Res. 2019, 39, 93–112. [Google Scholar] [CrossRef]
- Guerrero-Bote, V.P.; Moya-Anegón, F. A further step forward in measuring journals’ scientific prestige: The SJR2 indicator. J. Informetr. 2012, 6, 674–688. [Google Scholar] [CrossRef]
- Luo, Y.; Zhang, H. Emerging market MNEs: Qualitative review and theoretical directions. J. Int. Manag. 2016, 22, 333–350. [Google Scholar] [CrossRef]
- Mukherjee, D.; Lim, W.; Kumar, S.; Donthu, N. Guidelines for advancing theory and practice through bibliometric research. J. Bus. Res. 2022, 148, 101–115. [Google Scholar] [CrossRef]
- Donthu, N.; Kumar, S.; Mukherjee, D.; Pandey, N.; Lim, W. How to conduct a bibliometric analysis: An overview and guidelines. J. Bus. Res. 2021, 133, 285–296. [Google Scholar] [CrossRef]
- Chen, C.; Ibekwe-SanJuan, F.; Hou, J. The Structure and Dynamics of Cocitation Clusters: A Multiple-Perspective Cocitation Analysis. J. Am. Soc. Inf. Sci. Technol. 2010, 61, 1386–1409. [Google Scholar] [CrossRef]
- Chen, C. CiteSpace II: Detecting and visualizing emerging trends and transient patterns in scientific literature. J. Am. Soc. Inf. Sci. Technol. 2006, 57, 359–377. [Google Scholar] [CrossRef]
- Sabe, M.; Pillinger, T.; Kaiser, S.; Chen, C.; Taipale, H.; Tanskanen, A.; Tiihonen, J.; Leucht, S.; Correll, C.; Solmi, M. Half a century of research on antipsychotics and schizophrenia: A scientometric study of hotspots, nodes, bursts, and trends. Neurosci. Biobehav. Rev. 2022, 136, 104608. [Google Scholar] [CrossRef]
- Chen, C. CiteSpace: A Practical Guide for Mapping Scientific Literature; Nova Science Publishers: Hauppauge, NY, USA, 2016. [Google Scholar]
- Krippendorff, K. Content Analysis: An Introduction to Its Methodology; Sage Publications: Thousand Oaks, CA, USA, 2018. [Google Scholar]
- Smith, A.; Humphreys, M. Evaluation of unsupervised semantic mapping of natural language with Leximancer concept mapping. Behav. Res. Methods 2006, 38, 262–279. [Google Scholar] [CrossRef]
- Indulska, M.; Hovorka, D.; Recker, J. Quantitative approaches to content analysis: Identifying conceptual drift across publication outlets. Eur. J. Inf. Syst. 2012, 21, 49–69. [Google Scholar] [CrossRef]
- Legendre, T.S.; Ding, A.; Back, K.-J. A bibliometric analysis of the hospitality and tourism environmental, social, and governance (ESG) literature. J. Hosp. Tour. Manag. 2024, 58, 309–321. [Google Scholar] [CrossRef]
- Hoque, R.; Sorwar, G. Understanding factors influencing the adoption of mHealth by the elderly: An extension of the UTAUT model. Int. J. Med. Inf. 2017, 101, 75–84. [Google Scholar] [CrossRef] [PubMed]
- Klaver, N.; van de Klundert, J.; van den Broek, R.; Askari, M. Relationship between perceived risks of using mHealth applications and the intention to use them among older adults in the Netherlands: Cross-sectional study. JMIR mHealth uHealth 2021, 9, e26845. [Google Scholar] [CrossRef] [PubMed]
- Cajita, M.; Hodgson, N.; Lam, K.; Yoo, S.; Han, H. Facilitators of and barriers to mHealth adoption in older adults with heart failure. CIN-Comput. Inform. Nurs. 2018, 36, 376–382. [Google Scholar] [CrossRef]
- Zhao, Y.; Ni, Q.; Zhou, R. What factors influence the mobile health service adoption? A meta-analysis and the moderating role of age. Int. J. Inf. Manag. 2018, 43, 342–350. [Google Scholar] [CrossRef]
- Shareef, M.A.; Kumar, V.; Dwivedi, Y.K.; Kumar, U.; Akram, M.S.; Raman, R. A new health care system enabled by machine intelligence: Elderly people’s trust or losing self control. Technol. Forecast. Soc. Change 2021, 162, 16. [Google Scholar] [CrossRef]
- Ghorayeb, A.; Comber, R.; Gooberman-Hill, R. Older adults’ perspectives of smart home technology: Are we developing the technology that older people want? Int. J. Hum. Comput. Stud. 2021, 147, 13. [Google Scholar] [CrossRef]
- Tsai, T.-H.; Lin, W.-Y.; Chang, Y.-S.; Chang, P.-C.; Lee, M.-Y. Technology anxiety and resistance to change behavioral study of a wearable cardiac warming system using an extended TAM for older adults. PLoS ONE 2020, 15, e0227270. [Google Scholar] [CrossRef]
- Nikou, S.; Agahari, W.; Keijzer-Broers, W.; de Reuver, M. Digital healthcare technology adoption by elderly people: A capability approach model. Telemat. Inform. 2020, 53, 101315. [Google Scholar] [CrossRef]
- Abbaspur-Behbahani, S.; Monaghesh, E.; Hajizadeh, A.; Fehresti, S. Application of mobile health to support the elderly during the covid-19 outbreak: A systematic review. Health Policy Technol. 2022, 11, 100595. [Google Scholar] [CrossRef]
- Baudier, P.; Kondrateva, G.; Ammi, C.; Chang, V.; Schiavone, F. Patients’ perceptions of teleconsultation during COVID-19: A cross-national study. Technol. Forecast. Soc. Change 2021, 163, 120510. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. One size fits all? What counts as quality practice in (reflexive) thematic analysis? Qual. Res. Psychol. 2021, 18, 328–352. [Google Scholar] [CrossRef]
- Zhang, M.; Luo, M.; Nie, R.; Zhang, Y. Technical attributes, health attribute, consumer attributes and their roles in adoption intention of healthcare wearable technology. Int. J. Med. Inf. 2017, 108, 97–109. [Google Scholar] [CrossRef] [PubMed]
- Kavandi, H.; Jaana, M. Factors that affect health information technology adoption by seniors: A systematic review. Health Soc. Care Community 2020, 28, 1827–1842. [Google Scholar] [CrossRef] [PubMed]
- Teh, P.-L.; Lim, W.M.; Ahmed, P.K.; Chan, A.H.; Loo, J.M.; Cheong, S.-N.; Yap, W.-J. Does power posing affect gerontechnology adoption among older adults? Behav. Inf. Technol. 2017, 36, 33–42. [Google Scholar] [CrossRef]
- Davis, F.D.; Bagozzi, R.P.; Warshaw, P.R. User acceptance of computer technology: A comparison of two theoretical models. Manag. Sci. 1989, 35, 982–1003. [Google Scholar] [CrossRef]
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. User acceptance of information technology: Toward a unified view. MIS Q. 2003, 27, 425–478. [Google Scholar] [CrossRef]
- Arthanat, S.; Wilcox, J.; Macuch, M. Profiles and predictors of smart home technology adoption by older adults. OTJR Occup. Particip. Health 2019, 39, 247–256. [Google Scholar] [CrossRef]
- Pywell, J.; Vijaykumar, S.; Dodd, A.; Coventry, L. Barriers to older adults’ uptake of mobile-based mental health interventions. Digit. Health 2020, 6, 15. [Google Scholar] [CrossRef]
- Chung, J.; Demiris, G.; Thompson, H.J.; Chen, K.Y.; Burr, R.; Patel, S.; Fogarty, J. Feasibility testing of a home-based sensor system to monitor mobility and daily activities in korean american older adults. Int. J. Older People Nurs. 2017, 12, e12127. [Google Scholar] [CrossRef]
- Astell, A.J.; McGrath, C.; Dove, E. ‘That’s for old so and so’s!’: Does identity influence older adults’ technology adoption decisions? Ageing Soc. 2020, 40, 1550–1576. [Google Scholar] [CrossRef]
- Cajita, M.I.; Hodgson, N.A.; Budhathoki, C.; Han, H.-R. Intention to use mHealth in older adults with heart failure. J. Cardiovasc. Nurs. 2017, 32, E1–E7. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.A.; Alam, K.; Taylor, B.; Ashraf, M. Examining the determinants of eHealth usage among elderly people with disability: The moderating role of behavioural aspects. Int. J. Med. Inf. 2021, 149, 8. [Google Scholar] [CrossRef] [PubMed]
- Talukder, M.S.; Laato, S.; Islam, A.K.M.N.; Bao, Y. Continued use intention of wearable health technologies among the elderly: An enablers and inhibitors perspective. Internet Res. 2021, 31, 1611–1640. [Google Scholar] [CrossRef]
- Califf, C.B.; Sarker, S.; Sarker, S. The bright and dark sides of technostress: A mixed-methods study involving healthcare IT. MIS Q. 2020, 44, 809–856. [Google Scholar] [CrossRef]
- Khosla, R.; Chu, M.-T.; Khaksar, S.M.S.; Nguyen, K.; Nishida, T. Engagement and experience of older people with socially assistive robots in home care. Assist. Technol. 2021, 33, 57–71. [Google Scholar] [CrossRef]
- Askari, M.; Klaver, N.S.; van Gestel, T.J.; van de Klundert, J. Intention to use medical apps among older adults in the Netherlands: Cross-sectional study. J. Med. Internet Res. 2020, 22, 12. [Google Scholar] [CrossRef]
- van Elburg, F.R.T.; Klaver, N.S.; Nieboer, A.P.; Askari, M. Gender differences regarding intention to use mHealth applications in the Dutch elderly population: A cross-sectional study. BMC Geriatr. 2022, 22, 11. [Google Scholar] [CrossRef]
- Ren, Z.W.; Zhou, G.M. Analysis of driving factors in the intention to use the virtual nursing home for the elderly: A modified UTAUT model in the Chinese context. Healthcare 2023, 11, 22. [Google Scholar] [CrossRef]
- van Elburg, F.R.T.; van de Klundert, J.; Nieboer, A.P.; Askari, M. The intention to use mHealth applications among Dutch older adults prior and during the COVID pandemic. Front. Public Health 2023, 11, 9. [Google Scholar] [CrossRef]
- Huang, H.H.; Chen, Z.Y.; Cao, S.M.; Xiao, M.Z.; Xie, L.L.; Zhao, Q.H. Adoption intention and factors influencing the use of gerontechnology in Chinese community-dwelling older adults: A mixed-methods study. Front. Public Health 2021, 9, 12. [Google Scholar] [CrossRef]
- Jaana, M.; Pare, G. Comparison of mobile health technology use for self-tracking between older adults and the general adult population in Canada: Cross-sectional survey. JMIR mHealth uHealth 2020, 8, 14. [Google Scholar] [CrossRef] [PubMed]
- Jeng, M.Y.; Pai, F.Y.; Yeh, T.M. Antecedents for older adults’ intention to use smart health wearable devices-technology anxiety as a moderator. Behav. Sci. 2022, 12, 16. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.Z.; Khanam, L. Comparison of the young aged and elderly female users’ adoption of mHealth services. Health Care Women Int. 2022, 43, 1259–1283. [Google Scholar] [CrossRef] [PubMed]
- Ko, C.H.; Chou, C.M. Apply the SERVQUAL instrument to measure service quality for the adaptation of ICT technologies: A case study of nursing homes in Taiwan. Healthcare 2020, 8, 16. [Google Scholar] [CrossRef]
- Tandon, U.; Ertz, M.; Shashi. Continued Intention of mHealth Care Applications among the Elderly: An Enabler Inhibitor Perspective. Int. J. Hum. Comput. Interact. 2024, 40, 5026–5041. [Google Scholar] [CrossRef]
- Wilkowska, W.; Offermann-van Heek, J.; Laurentius, T.; Bollheimer, L.C.; Ziefle, M. Insights Into the Older Adults’ World: Concepts of Aging, Care, and Using Assistive Technology in Late Adulthood. Front. Public Health 2021, 9, 14. [Google Scholar] [CrossRef]
- Huang, Q.Y.; Li, Y.; Wu, X.; Ge, S.; Qu, Z.; Wang, A.M.; Tang, X.P. The willingness and influencing factors to choose smart senior care among old adults in China. BMC Geriatr. 2022, 22, 12. [Google Scholar] [CrossRef]
- Wang, B.A.; Zhang, R.; Wang, Y. Mechanism Influencing Older People’s Willingness to Use Intelligent Aged-Care Products. Healthcare 2021, 9, 17. [Google Scholar] [CrossRef]
- Ma, D.; Zuo, M.Y. Unconscious or conscious? The impacts of habit and social support receipt on older adults’ continued participation in online health communities. Aslib J. Inf. Manag. 2022, 74, 688–709. [Google Scholar] [CrossRef]
- Wang, X.H.; Chen, J.Y.; Feng, M.Q.; Zhuang, M.Q.; Wang, J.Y.; Zhang, L.Y.; Liu, Y.; Chen, H.F. Demand and influencing factors of “Internet plus Traditional Chinese Medicine” home nursing service for older adult patients with chronic diseases: A mixed research perspective. Front. Public Health 2023, 11, 10. [Google Scholar] [CrossRef]
- Berridge, C.; Zhou, Y.J.; Robillard, J.M.; Kaye, J. Companion robots to mitigate loneliness among older adults: Perceptions of benefit and possible deception. Front. Psychol. 2023, 14, 9. [Google Scholar] [CrossRef] [PubMed]
- Frishammar, J.; Essen, A.; Simms, C.; Edblad, R.; Hardebro, V. Older individuals and digital healthcare platforms: Usage motivations and the impact of age on postadoption usage patterns. IEEE Trans. Eng. Manag. 2023, 70, 2903–2919. [Google Scholar] [CrossRef]
- Yang, K.; Li, Y.; Qi, H.Y. Determinants of and Willingness to Use and Pay for Digital Health Technologies Among the Urban Elderly in Hangzhou, China. Risk Manag. Healthc. Policy 2023, 16, 463–478. [Google Scholar] [CrossRef] [PubMed]
- Zafrani, O.; Nimrod, G.; Edan, Y. Between fear and trust: Older adults’ evaluation of socially assistive robots. Int. J. Hum. Comput. Stud. 2023, 171, 14. [Google Scholar] [CrossRef]
- Li, Y.M.; Ma, Y.M.; Wang, Y.; Hong, W.J. The Adoption of smart health services by older adults in retirement communities: Analysis with the technology acceptance model (TAM). Univers. Access Inf. Soc. 2024, 24, 1105–1121. [Google Scholar] [CrossRef]
- Rój, J. What determines the acceptance and use of eHealth by older adults in Poland? Int. J. Environ. Res. Public Health 2022, 19, 16. [Google Scholar] [CrossRef]
- Wang, X.; Lee, C.F.; Jiang, J.B.; Zhang, G.L.; Wei, Z. Research on the Factors Affecting the Adoption of Smart Aged-Care Products by the Aged in China: Extension Based on UTAUT Model. Behav. Sci. 2023, 13, 21. [Google Scholar] [CrossRef]
- Leung, W.K.; Law, S.P.; Cheung, M.L.; Chang, M.K.; Lai, C.-Y.; Liu, N. From resistance to acceptance: Developing health task measures to boost mHealth adoption among older adults: Mixed-methods approach and innovation resistance. Internet Res. 2024, 35, 1678–1721. [Google Scholar] [CrossRef]
- Shareef, M.A.; Ahmed, J.U.; Giannakis, M.; Dwivedi, Y.K.; Kumar, V.; Butt, I.; Kumar, U. Machine autonomy for rehabilitation of elderly people: A trade-off between machine intelligence and consumer trust. J. Bus. Res. 2023, 164, 17. [Google Scholar] [CrossRef]
- Kim, E.; Han, S. Determinants of continuance intention to use health apps among users over 60: A test of social cognitive model. Int. J. Environ. Res. Public Health 2021, 18, 19. [Google Scholar] [CrossRef]
- Chiu, H.M.; Hsu, M.C.; Ouyang, W.C. Effects of incorporating virtual reality training intervention into health care on cognitive function and wellbeing in older adults with cognitive impairment: A randomized controlled trial. Int. J. Hum. Comput. Stud. 2023, 170, 12. [Google Scholar] [CrossRef]
- Vandemeulebroucke, T.; de Casterlé, B.D.; Welbergen, L.; Massart, M.; Gastmans, C. The Ethics of Socially Assistive Robots in Aged Care. A Focus Group Study With Older Adults in Flanders, Belgium. J. Gerontol. Ser. B-Psychol. Sci. Soc. Sci. 2020, 75, 1996–2007. [Google Scholar] [CrossRef] [PubMed]
- Jeng, M.Y.; Yeh, T.M.; Pai, F.Y. Analyzing older adults’ perceived values of using smart bracelets by means-end chain. Healthcare 2020, 8, 16. [Google Scholar] [CrossRef] [PubMed]
- Lin, T.T.C.; Bautista, J.R.; Core, R. Seniors and mobiles: A qualitative inquiry of mHealth adoption among Singapore seniors. Inform. Health Soc. Care 2020, 45, 360–373. [Google Scholar] [CrossRef]
- Camp, N.; Johnston, J.; Lewis, M.G.C.; Zecca, M.; Di Nuovo, A.; Hunter, K.; Magistro, D. Perceptions of in-home monitoring technology for activities of daily living: Semistructured interview study with community-dwelling older adults. JMIR Aging 2022, 5, 17. [Google Scholar] [CrossRef]
- Frishammar, J.; Essén, A.; Bergström, F.; Ekman, T. Digital health platforms for the elderly? Key adoption and usage barriers and ways to address them. Technol. Forecast. Soc. Change 2023, 189, 13. [Google Scholar] [CrossRef]
- Zhang, W.; Yin, J.; Chan, K.I.; Sun, T.; Jin, T.; Jeung, J.; Gong, J. Beyond digital privacy: Uncovering deeper attitudes toward privacy in cameras among older adults. Int. J. Hum. Comput. Stud. 2024, 192, 103345. [Google Scholar] [CrossRef]
- Afifi, T.; Collins, N.; Rand, K.; Otmar, C.; Mazur, A.; Dunbar, N.E.; Fujiwara, K.; Harrison, K.; Logsdon, R. Using virtual reality to improve the quality of life of older adults with cognitive impairments and their family members who live at a distance. Health Commun. 2023, 38, 1904–1915. [Google Scholar] [CrossRef]
- He, Q.; He, Y.; Liu, Q.; Ma, C.L. Acceptance of social assistant robots for the older adults living in the community in China. Geriatr. Nurs. 2023, 52, 191–198. [Google Scholar] [CrossRef]
- Bandura, A. Health promotion by social cognitive means. Health Educ. Behav. 2004, 31, 143–164. [Google Scholar] [CrossRef]
- Deci, E.L.; Ryan, R.M. Intrinsic Motivation and Self-Determination in Human Behavior; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2013. [Google Scholar]
- Bowlby, J. Attachment and Loss; Random House: New York City, NY, USA, 1969. [Google Scholar]
- Ram, S. A model of innovation resistance. ACR N. Am. Adv. 1987, 14, 208–212. [Google Scholar]
- Lusch, R.F.; Nambisan, S. Service innovation: A service-dominant logic perspective. MIS Q. 2015, 39, 155–176. [Google Scholar] [CrossRef]
- Park, D.C.; Festini, S.B. Theories of memory and aging: A look at the past and a glimpse of the future. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2017, 72, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Coelho, J.; Duarte, C. A literature survey on older adults’ use of social network services and social applications. Comput. Hum. Behav. 2016, 58, 187–205. [Google Scholar] [CrossRef]
- Sallis, J.F.; Owen, N.; Fisher, E. Ecological models of health behavior. Health Behav. Theory Res. Pract. 2015, 5, 43–64. [Google Scholar]
- Kadushin, C. Understanding Social Networks: Theories, Concepts, and Findings; Oxford University Press: Oxford, UK, 2012. [Google Scholar]
- Curumsing, M.K.; Fernando, N.; Abdelrazek, M.; Vasa, R.; Mouzakis, K.; Grundy, J. Emotion-oriented requirements engineering: A case study in developing a smart home system for the elderly. J. Syst. Softw. 2019, 147, 215–229. [Google Scholar] [CrossRef]
- Shie, A.-J.; Xu, E.-M.; Wang, Y.; Yang, M.; Wu, Y.J. Emotional needs and service process optimization in combined medical and elder care: A TRIZ approach. Technovation 2025, 143, 103224. [Google Scholar] [CrossRef]
- Yuan, Y.-P.; Tan, G.W.-H.; Ooi, K.-B. What shapes mobile fintech consumers’ post-adoption experience? A multi-analytical PLS-ANN-fsQCA perspective. Technol. Forecast. Soc. Change 2025, 217, 124162. [Google Scholar] [CrossRef]
- Yu, Y.; Davis, F.; Walden, E.; Turel, O. Unpacking conflicting evaluations and ambivalence in online hotel booking: The moderating role of perceived enjoyment in user retention. J. Retail. Consum. Serv. 2025, 85, 104266. [Google Scholar] [CrossRef]
- Li, X.; Cai, S.; Fu, X. Platform affordance as job resources: Job crafting and online retention of physicians in online health communities. Inf. Manag. 2025, 62, 104137. [Google Scholar] [CrossRef]
- Richetin, J.; Conner, M.; Perugini, M. Not doing is not the opposite of doing: Implications for attitudinal models of behavioral prediction. Personal. Soc. Psychol. Bull. 2011, 37, 40–54. [Google Scholar] [CrossRef] [PubMed]
- Sestino, A.; D’Angelo, A. Elderly patients’ reactions to gamification-based digital therapeutics (DTx): The relevance of socialization tendency seeking. Technol. Forecast. Soc. Change 2024, 205, 123526. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Hawley, C.E.; Genovese, N.; Owsiany, M.T.; Triantafylidis, L.K.; Moo, L.R.; Linsky, A.M.; Sullivan, J.L.; Paik, J.M. Rapid Integration of Home Telehealth Visits AmidstCOVID-19: What Do Older Adults Need to Succeed? J. Am. Geriatr. Soc. 2020, 68, 2431–2439. [Google Scholar] [CrossRef]
- Verloo, H.; Kampel, T.; Vide, N.; Pereira, F. Perceptions About Technologies That Help Community-Dwelling Older Adults Remain at Home: Qualitative Study. J. Med. Internet Res. 2020, 22, 17. [Google Scholar] [CrossRef]
- Liu, S.X.; Shen, Q.; Hancock, J. Can a social robot be too warm or too competent? Older Chinese adults’ perceptions of social robots and vulnerabilities. Comput. Hum. Behav. 2021, 125, 7. [Google Scholar] [CrossRef]
- Johnson, A.; Shukla, N.; Halley, M.; Nava, V.; Budaraju, J.; Zhang, L.; Linos, E. Barriers and facilitators to mobile health and active surveillance use among older adults with skin disease. Health Expect. 2021, 24, 1582–1592. [Google Scholar] [CrossRef]
- Cross, D.A.; Levin, Z.; Raj, M. Patient Portal Use, Perceptions of Electronic Health Record Value, and Self-Rated Primary Care Quality Among Older Adults: Cross-sectional Survey. J. Med. Internet Res. 2021, 23, 13. [Google Scholar] [CrossRef]
- Zhou, J.; Wang, Z.Y.; Liu, Y.; Yang, J. Research on the influence mechanism and governance mechanism of digital divide for the elderly on wisdom healthcare: The role of artificial intelligence and big data. Front. Public Health 2022, 10, 11. [Google Scholar] [CrossRef]
- Rodríguez-Fernández, J.M.; Danies, E.; Hoertel, N.; Galanter, W.; Saner, H.; Franco, O.H. Telemedicine Readiness Across Medical Conditions in a US National Representative Sample of Older Adults. J. Appl. Gerontol. 2022, 41, 982–992. [Google Scholar] [CrossRef]
- Pirzada, P.; Wilde, A.; Doherty, G.H.; Harris-Birtill, D. Ethics and acceptance of smart homes for older adults. Inform. Health Soc. Care 2022, 47, 10–37. [Google Scholar] [CrossRef]
- Choi, H.K.; Lee, K.; Lee, S.H. Developmental Study on “Smart Silver Care”: A Mobile Application to Alleviate Loneliness in Older Adults within the Community. Healthcare 2023, 11, 16. [Google Scholar] [CrossRef]
- Wang, X.; Lee, C.F.; Jiang, J.B.; Zhu, X.Y. Factors Influencing the Aged in the Use of Mobile Healthcare Applications: An Empirical Study in China. Healthcare 2023, 11, 21. [Google Scholar] [CrossRef]
- Cao, C.; Dai, H.Y.; Li, D. How to promote the healthy development of continuous participation in smart medical and elderly care systems: The dual perspective of perceived value and risk. Digit. Health 2023, 9, 16. [Google Scholar] [CrossRef]
- Koo, J.H.; Park, Y.H.; Kang, D.R. Factors Predicting Older People’s Acceptance of a Personalized Health Care Service App and the Effect of Chronic Disease: Cross-Sectional Questionnaire Study. JMIR Aging 2023, 6, 13. [Google Scholar] [CrossRef]
- Sancho-Esper, F.; Ostrovskaya, L.; Rodriguez-Sanchez, C.; Campayo-Sanchez, F. Virtual reality in retirement communities: Technology acceptance and tourist destination recommendation. J. Vacat. Mark. 2023, 29, 275–290. [Google Scholar] [CrossRef]
- Sun, Y.Q.; Feng, Y.F.; Shen, X.L.; Guo, X.T. Fear appeal, coping appeal and mobile health technology persuasion: A two-stage scenario-based survey of the elderly. Inf. Technol. People 2023, 36, 362–386. [Google Scholar] [CrossRef]




| Cluster | Silhouette Score | Size | Mean Year | Title | Keywords | Fields |
|---|---|---|---|---|---|---|
| #0 | 0.930 | 18 | 2019 | Smart home; ethics; machine intelligence | Assistive technology; ethical aspects; AAL | Medical Informatics; Healthcare; Business |
| #1 | 0.969 | 17 | 2017 | Senior; mobile health; qualitative inquiry | Engagement; multimorbidity; e-mental health | Medical Informatics; Business; Healthcare |
| #2 | 0.973 | 16 | 2019 | Usage motivation; postadoption usage pattern; usage barrier | Interviews; digital health; elderly patients | Management; Engineering; Healthcare |
| #3 | 0.930 | 16 | 2018 | Use; eHealth; acceptance | UTAUT model; nested regression analysis; eHealth | Public Health; Environmental Sciences; Business |
| #4 | 0.988 | 14 | 2021 | Innovation resistance; mixed-methods approach; inhibitor perspective | mHealth application; perceived risk; empathetic cooperation and social interaction | Computer Science; Telecommunications; Public Health |
| #6 | 0.966 | 10 | 2019 | Trust; fear; quality evaluation | Automation; human behavior; socially assistive robots | Psychology; Healthcare; Computer Science |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, J.; Wang, B. Systematic Review of Smart Elderly Care in Digital Environments: Toward Sustainable Wellbeing for Older Adults. Sustainability 2025, 17, 11357. https://doi.org/10.3390/su172411357
Liu J, Wang B. Systematic Review of Smart Elderly Care in Digital Environments: Toward Sustainable Wellbeing for Older Adults. Sustainability. 2025; 17(24):11357. https://doi.org/10.3390/su172411357
Chicago/Turabian StyleLiu, Jiaqi, and Bo Wang. 2025. "Systematic Review of Smart Elderly Care in Digital Environments: Toward Sustainable Wellbeing for Older Adults" Sustainability 17, no. 24: 11357. https://doi.org/10.3390/su172411357
APA StyleLiu, J., & Wang, B. (2025). Systematic Review of Smart Elderly Care in Digital Environments: Toward Sustainable Wellbeing for Older Adults. Sustainability, 17(24), 11357. https://doi.org/10.3390/su172411357








