Best Practices for Environmental Sustainability in Healthcare Simulation Education: A Scoping Review
Abstract
1. Introduction
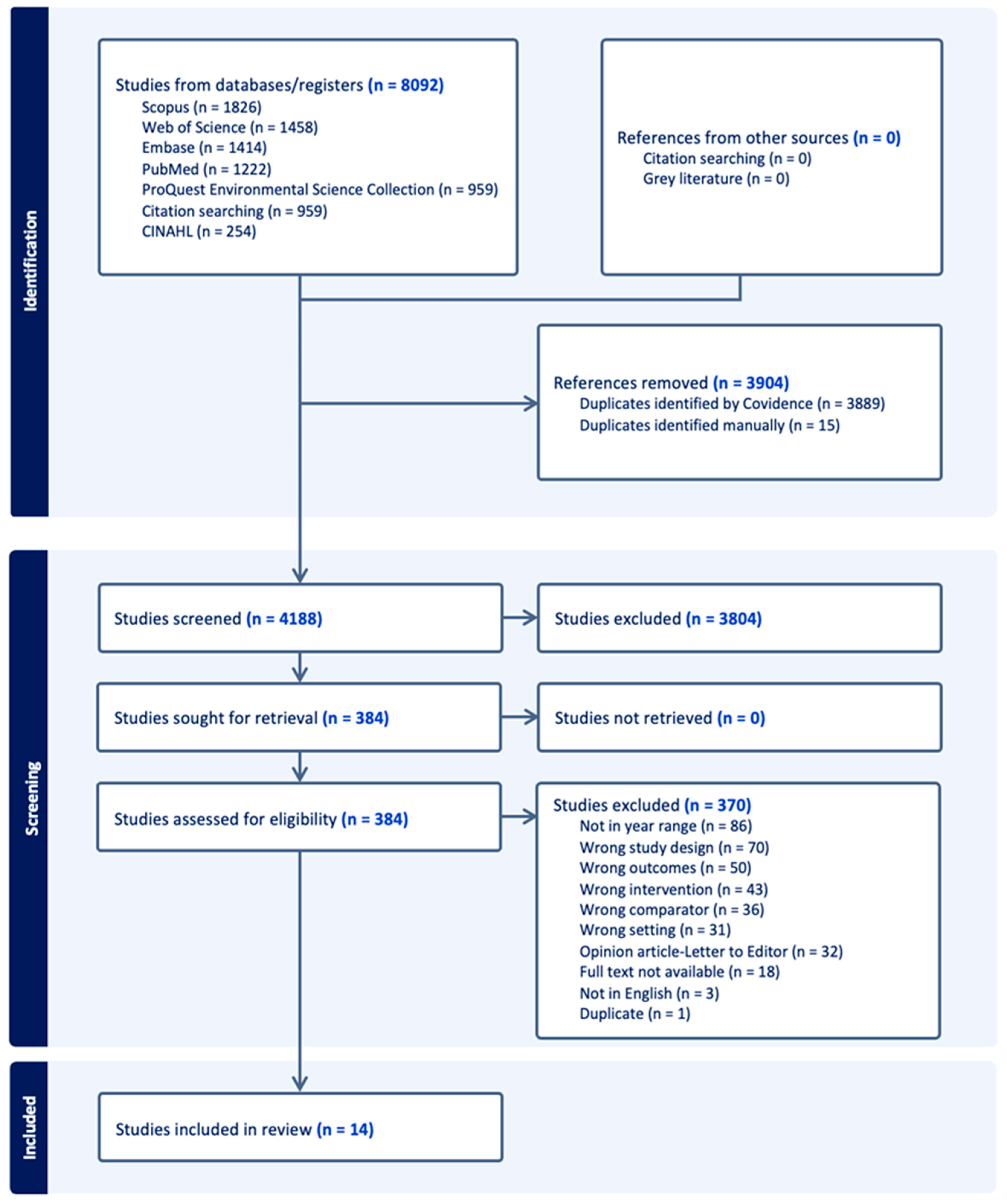
2. Materials and Methods
2.1. Search Strategy and Selection Criteria
2.2. Extraction, Critical Appraisal, and Data Synthesis
3. Results
3.1. Summary of Studies
3.1.1. Theme 1: The 5 R’s
Reduce, Reuse, and Recycle
Research and Rethink
3.1.2. Theme 2: Getting People Motivated
Education and Acceptance
Setting Clear Standards of Practice
Emphasizing Cost Savings
Internal Collaborative Efforts
3.1.3. Theme 3: Larger External Collaboration
Interdisciplinary Partnerships and External Engagement
Technological Solutions
Regulatory Frameworks and Compliance
National Policies and Strategic Initiatives
4. Discussion
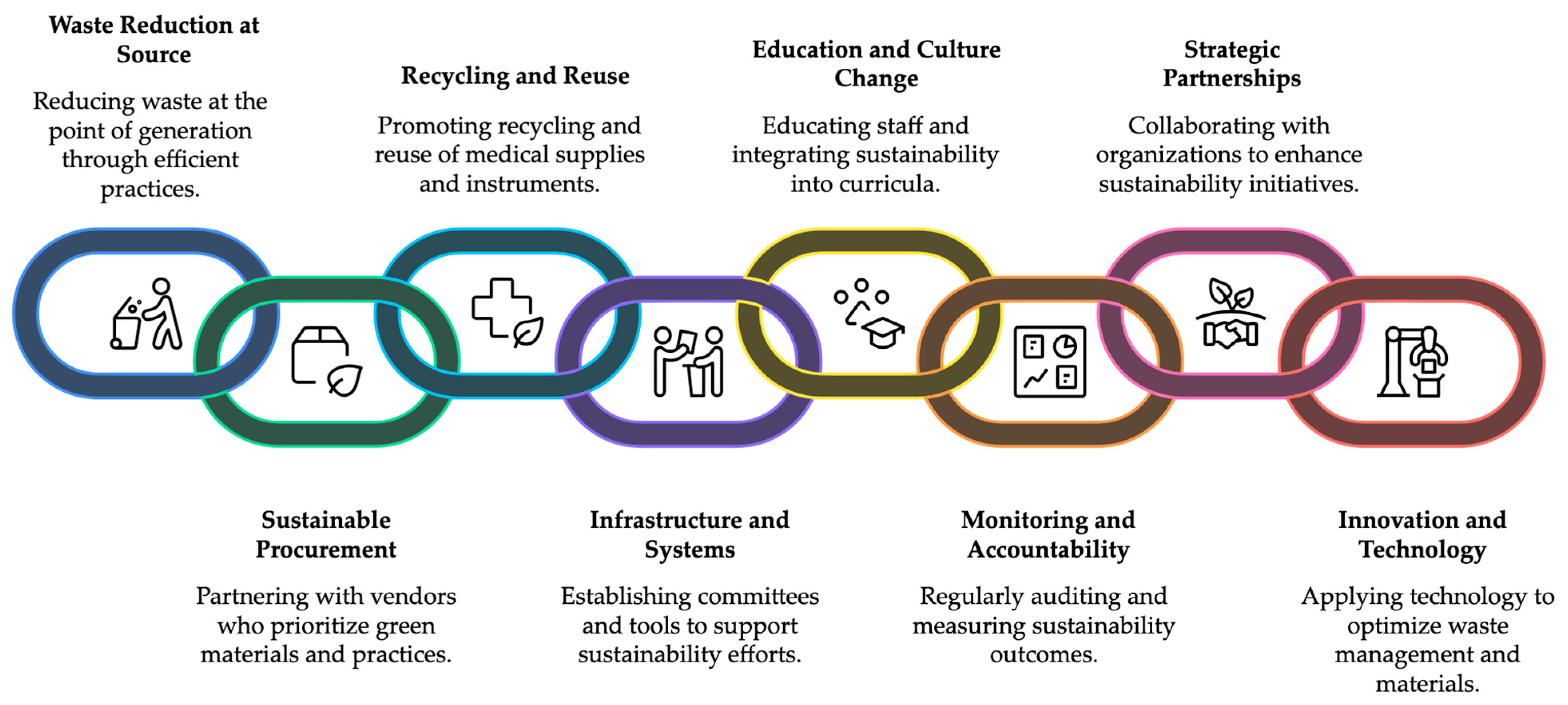
4.1. Implications for Practice
4.2. Action Items—What Simulation Centers Can Do Now
4.3. Future Directions
4.4. Cost Implications
4.5. Additional Sustainability Initiatives
4.6. Limitations
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| PICO | Population, Intervention, Comparison, and Outcome |
| PRISMA-SCR | The Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews |
| INACSL | International Nursing Association for Clinical Simulation and Learning |
| SIG | Special Interest Group |
Appendix A. Database Search Strategies
Appendix A.1. PubMed
- (“Plastics”[Mesh] OR plastic[tiab] OR plastics[tiab]) AND (“Waste Products”[Mesh:NoExp] OR “Environmental Monitoring”[Mesh] OR “Waste Management”[Mesh] OR “Conservation of Natural Resources”[Mesh] OR “Recycling”[Mesh] OR “Equipment Reuse”[Mesh] OR “carbon footprint”[tiab] OR “carbon neutral*”[tiab] OR “climate change”[tiab] OR “climate crisis”[tiab] OR “zero waste”[tiab] OR conservation[tiab] OR eco-friend*[tiab] OR ecofriend*[tiab] OR re-use[tiab] OR recycle*[tiab] OR recycling[tiab] OR reuse[tiab] OR sustainability[tiab] OR sustainable[tiab] OR waste[tiab] OR upcycle[tiab] OR upcycling[tiab] OR “up cycle”[tiab] OR “up cycling”[tiab])
- 20,530 results
- “Patient Simulation”[Mesh] OR “Simulation Training”[Mesh] OR “Augmented Reality”[Mesh] OR “Disposable Equipment”[Mesh] OR “Catheters”[Mesh] OR “Personal Protective Equipment”[Mesh:NoExp] OR “Masks”[Mesh:NoExp] OR “Gloves, Protective”[Mesh] OR “Syringes”[Mesh] OR “Tourniquets”[Mesh] OR “Health Facilities”[Mesh] OR “Schools, Health Occupations”[Mesh] OR “Schools, Health Occupations”[Mesh] OR “Students, Health Occupations”[Mesh] OR “Education, Professional”[Mesh] OR “clinical education”[tiab] OR “dental education”[tiab] OR “health care student*”[tiab] OR “health care”[tiab] OR “health student*”[tiab] OR “healthcare education”[tiab] OR “healthcare student*”[tiab] OR “medical education”[tiab] OR “medical student*”[tiab] OR “nursing education”[tiab] OR “nursing student*”[tiab] OR “patient care”[tiab] OR “pharmacy student*”[tiab] OR healthcare[tiab] OR hospital[tiab] OR hospitals[tiab] OR medical[tiab] OR medicine[tiab] OR nurse*[tiab] OR nursing[tiab] OR Glove[tiab] OR gloves[tiab] OR Syringe*[tiab] OR Tourniquet*[tiab] OR Catheter*[tiab] OR mask[tiab] OR masks[tiab] OR gloves[tiab] OR “augmented reality”[tiab] OR “clinical simulation”[tiab] OR “health care simulation”[tiab] OR “healthcare simulation”[tiab] OR “mixed reality”[tiab] OR “patient simulation”[tiab] OR “simulated patient*”[tiab]
- 4,745,384 results
Appendix A.2. Embase
- (‘plastic’/de OR ‘plastic waste’/de OR plastic:ti,ab OR plastics:ti,ab) AND (‘waste management’/exp OR ‘waste disposal facility’/exp OR ‘waste’/de OR ‘hospital waste’/exp OR ‘packaging waste’/exp OR ‘environmental protection’/de OR ‘environmental sustainability’/de OR ‘carbon footprint’/de OR ‘ecological footprint’/de OR (“carbon footprint” OR “carbon neutral*” OR “climate change” OR “climate crisis” OR “zero waste” OR conservation OR eco-friend* OR ecofriend* OR re-use OR recycle* OR recycling OR reuse OR sustainability OR sustainable OR waste OR upcycle OR upcycling OR “up cycle” OR “up cycling”):ti,ab)
- 12,073 results
- ‘patient simulation’/exp OR ‘simulation training’/exp OR ‘augmented reality’/exp OR ‘disposable equipment’/exp OR ‘catheters and tubes’/exp OR ‘protective equipment’/de OR ‘protective glove’/de OR ‘surgical mask’/de OR ‘syringe’/de OR ‘hypodermic syringe’/de OR ‘insulin syringe’/de OR ‘Luer lock syringe’/de OR ‘tourniquet’/exp OR ‘health care facility’/exp OR ‘medical school’/exp OR ‘pharmacy school’/exp OR ‘health student’/exp OR ‘nursing student’/exp OR ‘paramedical education’/exp OR ‘medical education’/exp OR (“clinical education” OR “dental education” OR “health care student*” OR “health care” OR “health student*” OR “healthcare education” OR “healthcare student*” OR “medical education” OR “medical student*” OR “nursing education” OR “nursing student*” OR “patient care” OR “pharmacy student*” OR healthcare OR hospital OR hospitals OR medical OR medicine OR nurse* OR nursing OR Glove OR gloves OR Syringe* OR Tourniquet* OR Catheter* OR mask OR masks OR gloves OR “augmented reality” OR “clinical simulation” OR “health care simulation” OR “healthcare simulation” OR “mixed reality” OR “patient simulation” OR “simulated patient*”):ti,ab
- 7,337,159 results
Appendix A.3. CINAHL
- (MH “Plastics” OR MH “Plasticizers” OR MH “Polyethylenes” OR MH “Polyurethanes” OR MH “Polyvinyls+” OR MH “Resins, Synthetic+” OR plastic OR plastics) AND (MH “Conservation of Natural Resources” OR MH “Refuse Disposal” OR MH “Recycling” OR MH “Medical Waste Disposal” OR MH “Sharps Disposal” OR MH “Dental Waste” OR MH “Environmental Sustainability” OR MH “Carbon Footprint” OR MH “Equipment Reuse” OR MH “Climate Change” OR “carbon footprint” OR “carbon neutral*” OR “climate change” OR “climate crisis” OR “zero waste” OR conservation OR eco-friend* OR ecofriend* OR re-use OR recycle* OR recycling OR reuse OR sustainability OR sustainable OR waste OR upcycle OR upcycling OR “up cycle” OR “up cycling”)
- 621 results
- MH “Patient Care+” OR MH “Simulations” OR MH “Patient Simulation” OR MH “Augmented Reality” OR MH “Computerized Clinical Simulation Testing” OR MH “Disposable Equipment” OR MH “Catheters and Tubes+” OR MH “Masks” OR MH “Personal Protective Equipment+” OR MH “Gloves” OR MH “Syringes” OR MH “Tourniquets” OR MH “Health Facilities+” OR MH “Schools, Allied Health” OR MH “Schools, Dental” OR MH “Schools, Medical” OR MH “Schools, Nursing” OR MH “Schools, Podiatry” OR MH “Students, Health Occupations+” OR MH “Students, Allied Health+” OR MH “Students, Medical+” OR MH “Students, Nursing+” OR MH “Students, Pharmacy” OR MH “Students, Podiatry” OR MH “Education, Health Sciences+” OR MH “Education, Nursing”OR “clinical education” OR “dental education” OR “health care student*” OR “health care” OR “health student*” OR “healthcare education” OR “healthcare student*” OR “medical education” OR “medical student*” OR “nursing education” OR “nursing student*” OR “patient care” OR “pharmacy student*” OR healthcare OR hospital OR hospitals OR medical OR medicine OR nurse* OR nursing OR Glove OR gloves OR Syringe* OR Tourniquet* OR Catheter* OR mask OR masks OR gloves OR “augmented reality” OR “clinical simulation” OR “health care simulation” OR “healthcare simulation” OR “mixed reality” OR “patient simulation” OR “simulated patient*”
- 3,233,545 results
Appendix A.4. ProQuest (Environmental Science Collection)
- MAINSUBJECT.EXACT(“Plastic pollution”) OR OR MAINSUBJECT.EXACT(“Plastic debris”) OR (MAINSUBJECT.EXACT(“Plastics”) AND (MAINSUBJECT.EXACT(“Sustainability management”) OR MAINSUBJECT.EXACT(“Sustainability reporting”) OR MAINSUBJECT.EXACT(“Sustainability”) OR MAINSUBJECT.EXACT(“Sustainability science”) OR MAINSUBJECT.EXACT(“Nature conservation”) OR MAINSUBJECT.EXACT(“Recycling”) OR MAINSUBJECT.EXACT(“Resource conservation”) OR MAINSUBJECT.EXACT(“Conservation”) OR MAINSUBJECT.EXACT(“Climate change”) OR MAINSUBJECT.EXACT(“Global warming”) OR MAINSUBJECT.EXACT(“Sustainable practices”) OR MAINSUBJECT.EXACT(“Sustainable use”) OR MAINSUBJECT.EXACT(“Carbon footprint”) OR MAINSUBJECT.EXACT(“Sustainable materials”))) OR NOFT (plastic OR plastics) AND NOFT(“carbon footprint” OR “carbon neutral*” OR “climate change” OR “climate crisis” OR “zero waste” OR conservation OR eco-friend* OR ecofriend* OR re-use OR recycle* OR recycling OR reuse OR sustainability OR sustainable OR waste OR upcycle OR upcycling OR “up cycle” OR “up cycling”)
- 9996 results
- MAINSUBJECT.EXACT(“Hospitals”) OR MAINSUBJECT.EXACT(“Gloves”) OR MAINSUBJECT.EXACT(“Hypodermic needles”) OR MAINSUBJECT.EXACT(“Health care”) OR MAINSUBJECT.EXACT(“Intravenous administration”) OR MAINSUBJECT.EXACT(“Medical equipment”) OR MAINSUBJECT.EXACT(“Medical wastes”) OR MAINSUBJECT.EXACT(“Medicine”) OR MAINSUBJECT.EXACT(“Medical instruments”) OR MAINSUBJECT.EXACT(“Syringes”) OR MAINSUBJECT.EXACT(“Medical personnel”) OR MAINSUBJECT.EXACT(“Hospital wastes”) OR MAINSUBJECT.EXACT(“Nursing”) OR NOFT(“clinical education” OR “dental education” OR “health care student*” OR “health care” OR “health student*” OR “healthcare education” OR “healthcare student*” OR “medical education” OR “medical student*” OR “nursing education” OR “nursing student*” OR “patient care” OR “pharmacy student*” OR healthcare OR hospital OR hospitals OR medical OR medicine OR nurse* OR nursing OR Glove OR gloves OR Syringe* OR Tourniquet* OR Catheter* OR mask OR masks OR gloves) OR NOFT(“augmented reality” OR “clinical simulation” OR “health care simulation” OR “healthcare simulation” OR “mixed reality” OR “patient simulation” OR “simulated patient*”)
- 8,289,281 results
Appendix A.5. Web of Science
- TITLE OR KEYWORDS Plus: ((plastic OR plastics) AND (“carbon footprint” OR “carbon neutral” OR”carbon neutrality” OR “climate change” OR “climate crisis” OR “zero waste” OR conservation OR eco-friend* OR ecofriend* OR re-use OR recycle* OR recycling OR reuse OR sustainability OR sustainable OR waste OR upcycle OR upcycling OR “up cycle” OR “up cycling”) AND (“clinical education” OR “dental education” OR “health care student” OR “health care students” OR “health care” OR “health student” OR “health students”OR “healthcare education” OR “healthcare student” OR “healthcare students” OR “medical education” OR “medical student” OR “medical students” OR “nursing education” OR “nursing student” OR “nursing students” OR”patient care” OR “pharmacy student” OR “pharmacy students” OR healthcare OR hospital OR hospitals OR medical OR medicine OR nurse* OR nursing OR Glove OR gloves OR Syringe* OR Tourniquet* OR Catheter* OR mask OR masks OR gloves OR “augmented reality” OR “clinical simulation” OR “health care simulation” OR “healthcare simulation” OR “mixed reality” OR “patient simulation” OR “simulated patient” OR “simulated patients”))
Appendix A.6. Scopus
- (TITLE (plastic OR plastics AND “carbon footprint” OR “carbon neutral” OR “carbon neutrality” OR “climate change” OR “climate crisis” OR “zero waste” OR conservation OR eco-friend* OR ecofriend* OR re-use OR recycle* OR recycling OR reuse OR sustainability OR sustainable OR waste OR upcycle OR upcycling OR “up cycle” OR “up cycling” AND “clinical education” OR “dental education” OR “health care student” OR “health care students” OR “health care” OR “health student” OR “health students” OR “healthcare education” OR “healthcare student” OR “healthcare students” OR “medical education” OR “medical student” OR “medical students” OR “nursing education” OR “nursing student” OR “nursing students” OR “patient care” OR “pharmacy student” OR “pharmacy students” OR healthcare OR hospital OR hospitals OR medical OR medicine OR nurse* OR nursing OR glove OR gloves OR syringe* OR tourniquet* OR catheter* OR mask OR masks OR gloves OR “augmented reality” OR “clinical simulation” OR “health care simulation” OR “healthcare simulation” OR “mixed reality” OR “patient simulation” OR “simulated patient” OR “simulated patients”) OR KEY (plastic OR plastics AND “carbon footprint” OR “carbon neutral” OR “carbon neutrality” OR “climate change” OR “climate crisis” OR “zero waste” OR conservation OR eco-friend* OR ecofriend* OR re-use OR recycle* OR recycling OR reuse OR sustainability OR sustainable OR waste OR upcycle OR upcycling OR “up cycle” OR “up cycling” AND “clinical education” OR “dental education” OR “health care student” OR “health care students” OR “health care” OR “health student” OR “health students” OR “healthcare education” OR “healthcare student” OR “healthcare students” OR “medical education” OR “medical student” OR “medical students” OR “nursing education” OR “nursing student” OR “nursing students” OR “patient care” OR “pharmacy student” OR “pharmacy students” OR healthcare OR hospital OR hospitals OR medical OR medicine OR nurse* OR nursing OR glove OR gloves OR syringe* OR tourniquet* OR catheter* OR mask OR masks OR gloves OR “augmented reality” OR “clinical simulation” OR “health care simulation” OR “healthcare simulation” OR “mixed reality” OR “patient simulation” OR “simulated patient” OR “simulated patients”))
References
- Practice Greenhealth. Defining Waste and Material Streams; Practice Greenhealth: Reston, VA, USA, 2015; Available online: https://practicegreenhealth.org/sites/default/files/2019-03/defining_waste_and_material_streams.pdf (accessed on 28 April 2025).
- Sims, R.R. Kolb’s experiential learning theory: A framework for assessing person-job interaction. Acad. Manag. Rev. 1983, 8, 501. [Google Scholar] [CrossRef]
- Bathish, M.A.; Lee, D.R.; Czerwinski, M.A.; Marsack, J.E. A survey of sustainability efforts in healthcare simulation and clinical learning. Clin. Simul. Nurs. 2022, 69, 1–6. [Google Scholar] [CrossRef]
- National Council of State Boards of Nursing (NCSBN). The 2025 NCSBN environmental scan: Going beyond. J. Nurs. Regul. 2025, 15, S1–S48. [Google Scholar] [CrossRef]
- AAMC. Enrollment up at U.S. Medical Schools. 2020. Available online: https://www.aamc.org/news/press-releases/enrollment-us-medical-schools (accessed on 30 April 2025).
- Sousa, A.C.; Veiga, A.; Maurício, A.C.; Lopes, M.A.; Santos, J.D.; Neto, B. Assessment of the environmental impacts of medical devices: A review. Environ. Dev. Sustain. 2021, 23, 9641–9666. [Google Scholar] [CrossRef]
- Kamp, E.; Musbahi, E.; Gupta, P. Topical treatment samples: Plastic, recycling and sustainability. Clin. Exp. Dermatol. 2022, 47, 186. [Google Scholar] [CrossRef] [PubMed]
- Vogt, J.; Nunes, K.R. Recycling behaviour in healthcare: Waste handling at work. Ergonomics 2014, 57, 525–535. [Google Scholar] [CrossRef] [PubMed]
- Faraca, G.; Astrup, T. Plastic waste from recycling centres: Characterisation and evaluation of plastic recyclability. Waste Manag. 2019, 95, 388–398. [Google Scholar] [CrossRef] [PubMed]
- Martin, N.; Sheppard, M.; Gorasia, G.; Arora, P.; Cooper, M.; Mulligan, S. Awareness and barriers to sustainability in dentistry: A scoping review. J. Dent. 2021, 112, 103735. [Google Scholar] [CrossRef] [PubMed]
- Wyssusek, K.H.; Keys, M.T.; van Zundert, A.A. Operating room greening initiatives—The old, the new, and the way forward: A narrative review. Waste Manag. Res. 2019, 37, 3–19. [Google Scholar] [CrossRef] [PubMed]
- Kheirabadi, S.; Sheikhi, A. Recent advances and challenges in recycling and reusing biomedical materials. Curr. Opin. Green Sustain. Chem. 2022, 38, 100695. [Google Scholar] [CrossRef] [PubMed]
- Mewaldt, C.; Armand, W.; Slutzman, J.; Eisen, J. The plastic pandemic: Quantification of waste on an inpatient medicine unit. J. Clim. Chang. Health 2023, 11, 100230. [Google Scholar] [CrossRef]
- Rasheed, F.N.; Walraven, G. Cleaning up plastics in healthcare waste: The transformative potential of leadership. BMJ Innov. 2023, 9, 103–108. [Google Scholar] [CrossRef]
- Williams, A.T.; Rangel-Buitrago, N. The past, present, and future of plastic pollution. Mar. Pollut. Bull. 2022, 176, 113429. [Google Scholar] [CrossRef] [PubMed]
- Kanwar, T.; Asad, H. The need for environmental sustainability in our curriculum. Med. Teach. 2019, 41, 1328. [Google Scholar] [CrossRef] [PubMed]
- Schwerdtle, P.N.; Maxwell, J.; Horton, G.; Bonnamy, J. 12 tips for teaching environmental sustainability to health professionals. Med. Teach. 2020, 42, 150–155. [Google Scholar] [CrossRef] [PubMed]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Covidence. Veritas Health Innovation, Melbourne, Australia. Available online: https://www.covidence.org/ (accessed on 28 April 2025).
- Xiao, M.Z.; Abbass, S.A.; Bahrey, L.; Rubinstein, E.; Chan, V.W. A roadmap for environmental sustainability of plastic use in anesthesia and the perioperative arena. Anesthesiology 2021, 135, 729–737. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Han, S. Carbon neutral hand surgery: Simple changes to reduce carbon footprint. Plast. Surg. 2024, 32, 108–112. [Google Scholar] [CrossRef] [PubMed]
- Linstadt, H.; Collins, A.; Slutzman, J.E.; Kimball, E.; Lemery, J.; Sorensen, C.; Winstead-Derlega, C.; Evans, K.; Auerbach, P.S. The climate-smart emergency department: A primer. Ann. Emerg. Med. 2020, 76, 155–167. [Google Scholar] [CrossRef] [PubMed]
- Joseph, B.; James, J.; Kalarikkal, N.; Thomas, S. Recycling of medical plastics. Adv. Ind. Eng. Polym. Res. 2021, 4, 199–208. [Google Scholar] [CrossRef]
- Kleber, J.; Cohen, B. Reducing Waste and Increasing Sustainability in Health Care Settings. Am. J. Nurs. 2020, 120, 45–48. [Google Scholar] [CrossRef] [PubMed]
- Harding, C.; Van Loon, J.; Moons, I.; De Win, G.; Du Bois, E. Design opportunities to reduce waste in operating rooms. Sustainability 2021, 13, 2207. [Google Scholar] [CrossRef]
- Azouz, S.; Boyll, P.; Swanson, M.; Castel, N.; Maffi, T.; Rebecca, A.M. Managing barriers to recycling in the operating room. Am. J. Surg. 2019, 217, 634–638. [Google Scholar] [CrossRef] [PubMed]
- Mallick, P.K.; Salling, K.B.; Pigosso, D.C.; McAloone, T.C. Designing take-back for single use medical devices: The case of ReturpenTM. J. Diabetes Sci. Technol. 2022, 16, 1363–1369. [Google Scholar] [CrossRef] [PubMed]
- Choi, E.-H.; Lee, H.; Kang, M.-J.; Nam, I.; Moon, H.-K.; Sung, J.-W.; Eu, J.-Y.; Lee, H.-B. Factors affecting zero-waste behaviours of college students. Int. J. Environ. Res. Public. Health 2022, 19, 9697. [Google Scholar] [CrossRef] [PubMed]
- Robert, N. How artificial intelligence is changing nursing. Nurs. Manag. 2019, 50, 30–39. [Google Scholar] [CrossRef] [PubMed]
- Redazione SIMZINE. Can Simulation Be Sustainable? 2023. Available online: https://simzine.news/focus-en/sim-debate-en/can-simulation-be-sustainable/ (accessed on 28 April 2025).
- Shaban, M.M.; Alanazi, M.A.; Mohammed, H.H.; Mohamed Amer, F.G.; Elsayed, H.H.; Zaky, M.E.; Ramadan, O.M.; Abdelgawad, M.E.; Shaban, M. Advancing sustainable healthcare: A concept analysis of eco-conscious nursing practices. BMC Nurs. 2024, 23, 660. [Google Scholar] [CrossRef] [PubMed]
- Marsack, J.E.; Bathish, M.A.; Lee, D.R. Sustainability efforts in healthcare simulation and clinical learning: An international survey. Nurse Educ. Today 2024, 132, 105990. [Google Scholar] [CrossRef] [PubMed]
- American Association of Colleges of Nursing (AACN). Domain 3: Population Health. Available online: https://www.aacnnursing.org/essentials/tool-kit/domains-concepts/population-health (accessed on 28 April 2025).
- Álvarez-Nieto, C.; Parra-Anguita, L.; Álvarez-García, C.; Montoro Ramirez, E.M.; López-Franco, M.D.; Sanz-Martos, S.; López Medina, I.M. Sustainability education in nursing degree for climate-smart healthcare: A quasi-experimental study. Int. J. Sustain. High. Educ. 2024, 25, 278–292. [Google Scholar] [CrossRef]
- Mayo Clinic. Mayo Clinic Green Initiative. Available online: https://www.communityengagement.mayoclinic.org/environmental-stewardship/ (accessed on 28 April 2025).
- University of Minnesota. Resources. Available online: https://environment.umn.edu/leadership/susted/resources/ (accessed on 28 April 2025).
- University of Michigan. How to Be a Green Wolverine: 2012–2013 Student Sustainability Guide. Available online: https://graham.umich.edu/product/how-be-green-wolverine-2012-2013-student-sustainability-guide (accessed on 28 April 2025).
- NHS. Greener NHS. Available online: https://www.england.nhs.uk/greenernhs/ (accessed on 28 April 2025).
- Anderson, K. Environment and healthcare: Why changing the way we consume healthcare is critical. Aust. Nurs. Midwifery J. 2023, 28, 28. Available online: https://search.informit.org/doi/10.3316/informit.177896255819477 (accessed on 14 July 2025).
- The Joint Commission. The Joint Commission Announces Sustainable Healthcare Certification for U.S. Hospitals. 2023. Available online: https://www.jointcommission.org/resources/news-and-multimedia/news/2023/09/sustainable-healthcare-certification-for-us-hospitals/ (accessed on 28 April 2025).
- Chanchlani, A.; Martin, K.; Dunne, B. Environmental sustainability in simulation education in healthcare. Int. J. Healthc. Simul. 2024, 10, 1–5. [Google Scholar] [CrossRef]
- Lamba, P.; Kaur, D.P.; Raj, S.; Sorout, J. Recycling/reuse of plastic waste as construction material for sustainable development: A review. Environ. Sci. Pollut. Res. Int. 2022, 29, 86156–86179. [Google Scholar] [CrossRef] [PubMed]
- Mohan, H.T.; Jayanarayanan, K.; Mini, K.M. A sustainable approach for the utilization of PPE biomedical waste in the construction sector. Jestech 2022, 32, 101060. [Google Scholar] [CrossRef]
- Ran, T.; Pang, J.; Zou, J. An emerging solution for medical waste: Reuse of COVID-19 protective suit in concrete. Sustainability 2022, 14, 10045. [Google Scholar] [CrossRef]
- Sorensen, R.M.; Kanwar, R.S.; Jovanovi, B. Past, present, and possible future policies on plastic use in the United States, particularly microplastics and nanoplastics: A review. Integr. Environ. Assess. Manag. 2023, 19, 474–488. [Google Scholar] [CrossRef] [PubMed]
| Authors | Country | Design | Aim(s) | Setting | Population/ Sample |
|---|---|---|---|---|---|
| Bathish et al., 2022 [3] | United States | Cross sectional | Identify current sustainability practices of clinical simulation education centers in the United States. | Education | 77 respondents from 75 unique healthcare simulation education institutions, representing 31 states and four countries (USA, India, Dominican Republic, and Canada) |
| Vogt & Nunes, 2014 [8] | Germany | Case control study | Review factors influencing recycling behavior. | Hospital (non-OR) | 616 nurses, ward managers, medical doctors, civil servants, and others who worked in six selected hospitals chosen based on size and recycling systems |
| Martin et al., 2021 [10] | United Kingdom | Scoping review | (1) Answer the research question “What is the current state of environmental sustainability in general dental practice?”; (2) Provide baseline data for general awareness, barriers, and challenges for the implementation of sustainable practices. | Dentistry | 128 articles total consisting of original research (n = 60), literature reviews (n = 25), reports on policy and/or legislation (n = 4), and expert opinion articles (n = 39) |
| Wyssusek, Keys, & van Zundert, 2018 [11] | Australia | Systematic review | (1) Quantify and qualify current OR waste; (2) Understand existing practices of waste segregation in ORs in Australia, and how these compare with international practices; (3) Investigate best practices in waste management; (4) Understand the financial implication of these initiatives; (5) Determine potential barriers to greening initiatives and how these can be improved. | Operating room (OR) | 84 articles total consisting of original research (n = 45), review articles (n = 30), editorials/ personal reflections (n = 7), and letters to the editor (n = 2) |
| Kheirabadi & Sheikhi 2022 [12] | United States | Expert opinion | Review the recent advances in recycling and reusing biomedical materials, discuss challenges associated with each practice, and outline prospects for future research. | Education | Healthcare |
| Xiao et al., 2021 [21] | Canada | Literature review, unspecified type | (1) Survey the current landscape of plastic use and disposal in the perioperative setting; (2) Outline evidence-based “reduce, reuse, recycle, rethink, and research” recommendations toward building environmental sustainability for plastics in the OR. | OR | Not described |
| Ma & Han, 2024 [22] | United Kingdom | Literature review, unspecified type | Identify and suggest changes that can be made in hand surgery for more sustainable practices. | OR | Not described |
| Linstadt et al., 2020 [23] | United States | Expert opinion | Educate and motivate emergency providers to action by providing a guide to sustainable healthcare and an approach to creating a climate-smart emergency department. | Hospital (non-OR) | N/A |
| Joseph et al., 2021 [24] | India | Expert opinion | Detail the need for recycling medical plastics, current recycling techniques, and their limitations within the framework of available data. | Hospital (non-OR) | Healthcare facilities producing plastic medical waste |
| Kleber & Cohen, 2020 [25] | United States | Expert opinion | Focus on the health effects of plastic medical waste and how nurses can be leaders in changing the way these products are used and disposed of. | Hospital (non-OR) | Nursing (inpatient or outpatient) |
| Harding et al., 2021 [26] | Belgium | Mixed Method— Observation | Investigate waste creation in the operative room to identify design opportunities to promote waste reduction according to the circular economy. | OR | 8 surgical observations and 5 expert witnesses |
| Azouz et al., 2019 [27] | United States | Educational intervention | Identify barriers to recycling, implement a recycling improvement educational program, and examine the personnel attitudes toward recycling in the OR. | OR | 524 OR personnel from four Mayo Clinic campuses (Phoenix, Rochester, Eau Claire, and Florida) |
| Mallick et al., 2022 [28] | Denmark | Non- randomized experiment | Describe how to design and implement a take-back system for single-use or disposable medical devices, specifically the ReturpenTM insulin pen. | Pharmacy | 66 of the 73 pharmacies in the three participating municipalities (37 in Copenhagen, 21 in Aarhus, and 8 in Kolding) |
| Choi et al., 2022 [29] | Republic of Korea | Cross sectional | (1) Determine how the recognition and attitude of zero waste affected student behavior; (2) Understand the change in plastic use caused by the pandemic; (3) Lay the foundation for the development of programs that promote zero-waste behaviors. | Education | 196 university students recruited via social networking sites |
| Authors | Transferable Concept(s)/Recommendation(s) Relevant to Sustainability |
|---|---|
| Bathish et al., 2022 [3] | -Advancing sustainability efforts in simulation centers will likely benefit from more formal planning, resource support, and partnership with other institutions. -Partnerships must be formed with vendors and industry partners to collectively create and encourage the use of carbon-neutral packaging and products. -Innovation is needed throughout the lifecycle of simulation supplies, from purchasing to reuse, recycling, and disposal, to make further waste reduction feasible and convenient. -Reuse may be the most feasible implementation strategy to combat supply chain shortages. -Recycling, environmentally preferable purchasing, and sustainable disposal are not immediately cost saving and may require investment without a guarantee of financial return. -Supply chain and waste stream assessment can potentially decrease costs; simulation centers may identify additional opportunities for waste reduction within the current infrastructure that only require further education and uptake. -Students should be taught to be environmentally conscious, resourceful, and judicious with supplies, as well as why these actions are important. |
| Vogt & Nunes, 2014 [8] | -The European Eco-Management and Audit Scheme (EMAS) is a voluntary instrument of the European Union that can be used by businesses and organizations to improve their environmental performance. -EMAS-certified hospital employees were significantly more satisfied with waste handling compared to those at non-certified hospitals. -Older employees self-reported more pro-environmental behavior at home, which correlated with fewer problems with waste handling observed on the wards -Modifiable changes can focus on improvement of waste handling. -Management should provide staff with information about the waste, the recycling process, and its outcomes. -Recycling bins should be solid, closed, and cleaned mechanically to reduce the risk of injury, with designated and sufficient space for bins on the wards. -People are motivated to separate waste if it is made easy, with clear labeling and feedback given on the outcome. -Cost-benefit analysis data may increase employers’ interest in ecological issues through feedback on the outcome. |
| Martin et al., 2021 [10] | -The Centre for Sustainable Healthcare in the UK has produced a guide for dental practices that highlights travel, supplies, energy waste management, biodiversity and green space, cost, return on investment, environmental benefit, and ease of implementation of each suggestion as factors to consider. -High knowledge, a positive attitude, and effective infrastructure are key to implementing effective waste management, but these are often lacking due to a lack of education, financial support, and appropriate supportive legislation. -Broad sustainability aims and guidance are beginning to be introduced into healthcare contracts, but these are neither sufficiently pervasive nor enforceable by the employer or law, and should be strengthened.-The disposal of plastic waste contributes a small percentage to the overall impact on pollution and CO2 emissions that arise from plastic usage in healthcare, so focus should be on the major contribution coming upstream in the supply chain from manufacturing, processing, distribution, and logistics. -Coordinating the procurement of products that use plastic as a container or packaging with waste management that can recover and recycle this waste can create significant financial gains by mapping procured plastic (at all levels of packaging) to sustainable recovery and recycling technologies, and a focus on sustainable purchasing leads to lower costs and environmental and health benefits. -There is a growing need to educate staff and students on sustainability using a range of media and resources. -Effective life cycle analyses can provide baseline data for key restorative materials and subsequently identify ways to minimize their use and facilitate recovery. |
| Wyssuse, Keys, & van Zundert, 2018 [11] | -Ensure waste is labeled and segregated into different waste containers to ensure that each type of waste is disposed of appropriately. -Segregation at the source of generation reduces the volume of clinical waste requiring special treatment. -Reducing paper towel waste can be achievable using hand dryers or hand sanitizers. -Teams can use a “just-in-time” model to prevent overage. -A redesign of standard kits to include only the necessary equipment to avoid waste and save money. -Do not automatically open all packages as some may not be used. -By physically documenting overage, staff were more inclined to reduce overage, thus reducing waste and associated costs. -Non-hazardous waste can be donated to schools for art projects, medical or veterinary schools for teaching purposes, or to developing countries -Legislation for healthcare waste management can provide a framework for prioritizing waste management to achieve the best environmental outcome. -Best practice is to limit waste altogether, followed by recycling, then diversion to landfill. -Regular education and mentorship to team leaders is recommended to help mitigate the barrier of staff attitudes. -Greening interventions should occur in small steps because acceptance by staff members is more likely to occur when changes take place gradually. -Greening efforts are intricate and require multidisciplinary collaboration between all healthcare personnel and hospital management, adequate leadership and guidance, implementation of an environmental greening team, staff education, and a predilection for new and novel environmentally friendly technologies. -Every small step counts toward reducing the ecological footprint. |
| Kheirabadi & Sheikhi 2022 [12] | -Reprocessing multiuse devices and recycling plastics is encouraged, with consideration to the specific material compatibilities and the potential risks of various sterilization methods (thermal, radiation, and chemical). -Both mechanical and chemical recycling can be useful to recover valuable materials from medical waste. -Machine learning for waste classification and public awareness campaigns can address the lack of standardized waste sorting. -Economically viable recycling processes, bio-based plastics to reduce environmental impact, and strict adherence to established protocols can ensure safety and efficiency in recycling practices. |
| Xiao et al., 2021 [21] | -The Sustainability Roadmap and the HospiCycle toolkit are valuable, vendor-neutral resources that can help institutions set up recycling programs. -Implementing a consistent color scheme for waste bins helps reduce ambiguity and prevents the mixing of waste streams. -Consider donating open-but-unused supplies to developing nations through reputable programs such as the REMEDY program or Not Just Tourists. -Reformulate standardized kits and remove items that are routinely left unused. -Sharps containers should only hold items capable of puncturing the skin, not empty syringes themselves, to limit overfilling with waste that could be recycled in some jurisdictions; for safe sharp disposal, consider reusable sharp containers with a needle adaptor that can lock the needle and automatically twists it off the syringe, allowing the disposal of only the needle instead of the entire syringe and needle unit. -Preferentially purchase supplies and equipment from companies that align with the hospital’s sustainability goals. -When optimizing their supply chain decisions, end users should pressure manufacturers for more environmentally conserving packaging and extended producer responsibility, where manufacturers of the product are responsible for the take-back, remanufacturing, recycling, and end-of-life management of the product. -Before starting recycling operations, conduct a prospective waste audit (internally or with third-party auditors) to benchmark the waste stream and determine what portions can be targeted by a recycling program. -Institutions can create a “Waste Wizard” sorting tool that guides proper recycling and disposal practices. -Measure program performance through periodic audits and provide measurable results, such as disseminating waste reduction outcomes regularly (e.g., in hospital newsletters) to energize and engage staff members. -Sustainability committees should comprise the following: (1) senior leadership (authority to approve capital investment and equipment purchases); (2) representatives from support services such as facilities, environmental services, and procurement to manage operational infrastructure for sustainability practices; (3) a sustainability officer whose primary responsibilities are to lead environmental initiatives and collect statistics; and (4) multidisciplinary clinical champions (e.g., front-line healthcare providers, surgeons, anesthesiologists, and nurses) to liaise communication efforts between environmental services and departments and coordinate staff education and action plans. |
| Ma & Han, 2024 [22] | -The 5 R’s help to positively impact our carbon footprint—Reduce, Reuse, Recycle, Research, and Rethink. -End users should collaborate with vendors who focus on producing greener materials and creating kits that reduce waste of unnecessary equipment. -A just-in-time model can be used to prepare only the necessary equipment and supplies to reduce waste. -Staff education on recycling practices promotes recycling of materials. -Teamwork promotes a common culture committed to working toward a carbon-neutral environment. |
| Linstadt et al., 2020 [23] | -Minimizing the amount of waste produced is the primary goal, which can be accomplished through more sustainable procurement practices. -Improving purchasing patterns includes working with suppliers to request and support development of environmentally preferred products and redesigning products to minimize waste. -Staff education is critical to waste reduction programs. -Decreasing disposable single-use devices in favor of reusable medical equipment can decrease waste and reduce the need for additional procurement. -Although recycling is an element of climate-smart healthcare and helps minimize the total volume of landfill waste produced, its overall contribution is minor. |
| Joseph et al., 2021 [24] | -Medical professionals should be educated on the value of recycling. -Programs should ensure that recyclers understand not all the materials being sent are contaminated or hazardous. -Materials must be segregated and categorized at the source, with the preparation of the internal collection system at each source. -Correct separation of medical plastics is important for efficient recycling. -Staff must be properly trained in handling and sorting recyclable materials. -Reuse products after sterilization whenever possible. -Unused medical supplies can be donated to non-profit organizations. |
| Kleber & Cohen, 2020 [25] | -Nurses can lead sustainability efforts by example through actions such as informing colleagues, friends, and family about sustainability efforts and supporting legislation to incentivize recycling and reduce emissions. -Information about sustainability efforts should be shared with other departments, administrators, and at conferences. -Nurses should advocate for green purchasing, recycling, and waste diversion. -Personal actions to promote sustainability efforts include communicating using electronic devices, printing double-sided, and using only necessary supplies. -Creating green initiatives, green teams, recycling workflows, and visual reminders can boost sustainability efforts. -Nursing-led interventions can result in reduction of wasted supplies. -Healthcare organizations should have a financial incentive to facilitate and encourage proper waste sorting, wherein local, state, and/or federal fines may be imposed if materials are not separated correctly. -Health Care Without Harm provides resources, including sample policies, to help clinicians jumpstart environmentally preferable purchasing programs. -Recycling bins should be readily available. -Demonstrating institutional cost savings is advantageous when engaging nursing and hospital leadership in waste reduction. -Supplies that can no longer be used can be donated to organizations that sort and distribute the supplies to healthcare systems in need around the world. -Purchasing single-use emesis basins, urinals, and bedpans made from 100% recycled molded pulp allows sewer disposal, reducing plastic waste, fossil fuel use, and hospital solid waste costs. |
| Harding et al., 2021 [26] | -Extending the lifetime and/or reuse of materials has higher value than recycling, but both interventions should be combined, as reuse is not always possible. -Clear labeling assists with communication of cleanliness of reusable instruments for future use. -The composition of supply sets should be reconsidered to reduce waste. -Availability of different recycling receptacles should be convenient and varied. |
| Azouz et al., 2019 [27] | -Most participants were concerned about the amount of garbage produced at their hospital, had a positive attitude toward recycling, and were active recyclers in their homes/community -Many respondents stated that proper training and labeling of recyclable materials would be most effective in improving operating room waste management. -Signs describing proper disposal of sharps were created and placed on each sharp container in the operating room to improve waste management. -A cost savings of 10.3% was achieved in sharp waste disposal expenditure, savings that could offset monetary intervention costs such as printing recycling signs. |
| Mallick et al., 2022 [28] | -Industries should take proactive measures to contribute to a more circular economy for disposable medical devices. -Companies can envision internal and/or reputational value to be recognized as a “green leader” or see financial value from reusing post-consumer recycled materials in the company’s own production; establishing a reverse value chain can contribute to envisioned value. -Collaborative partners and stakeholders are important contributors to a project’s success and may include state and local government, distributors and wholesalers, and relevant associations. -Designing a user-centric, workstream-based approach can provide a practical framework for the development and implementation of take-back programs. -Workstreams should identify recycling solutions in terms of recycling technology and infrastructure, in line with the broader take-back strategy, and find end markets for the recycled materials. -Logistics solutions need to be lean and utilize the existing setup to the greatest extent possible. -Additional workstreams on program management, business modeling, and Life Cycle Assessment may be needed. -Cultural norms matter; if the target group is already accustomed to the idea of sorting other wastes at home and the benefits of recycling are already anchored, incentivizing is not required (in Denmark, there is innate trust in authorities, and thus also in waste sorting obligations). -Communication and marketing plans can increase engagement by identifying where users want to learn about take-back, which tools and media to use, and where users would like to hand in their devices. -A visual identity image can explain the life cycle of the product. |
| Choi et al., 2022 [29] | -Recognition of the adverse link between microplastics and health was a major factor promoting zero-waste awareness and behavior, but participants showed low recognition regarding the health effects of microplastics; students must be offered more education to help them acquire reliable information, promote zero-waste behaviors such as segregation of disposables, and foster thinking on minimizing environmental pollution or microplastic usage. -Collaborative systems with universities should be built and operated to provide zero-waste-related education programs and campaigns for students. -More promotions and exciting public relations campaigns are required to encourage people to change their habits and inculcate zero-waste behaviors. -Companies should develop various alternative products that customers can use conveniently. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marsack, J.E.; Lee, D.; DiClemente, L.M.; Bodi, M.; Clarke, K.; Robison, E.S.; Turnau, S.; Van Horn, L.; Bathish, M.A. Best Practices for Environmental Sustainability in Healthcare Simulation Education: A Scoping Review. Sustainability 2025, 17, 6624. https://doi.org/10.3390/su17146624
Marsack JE, Lee D, DiClemente LM, Bodi M, Clarke K, Robison ES, Turnau S, Van Horn L, Bathish MA. Best Practices for Environmental Sustainability in Healthcare Simulation Education: A Scoping Review. Sustainability. 2025; 17(14):6624. https://doi.org/10.3390/su17146624
Chicago/Turabian StyleMarsack, Jessica E., Deborah Lee, Linda M. DiClemente, Melissa Bodi, Kimberley Clarke, Elizabeth S. Robison, Sandra Turnau, Laura Van Horn, and Melissa A. Bathish. 2025. "Best Practices for Environmental Sustainability in Healthcare Simulation Education: A Scoping Review" Sustainability 17, no. 14: 6624. https://doi.org/10.3390/su17146624
APA StyleMarsack, J. E., Lee, D., DiClemente, L. M., Bodi, M., Clarke, K., Robison, E. S., Turnau, S., Van Horn, L., & Bathish, M. A. (2025). Best Practices for Environmental Sustainability in Healthcare Simulation Education: A Scoping Review. Sustainability, 17(14), 6624. https://doi.org/10.3390/su17146624








