Disaster Preparedness in Saudi Arabia’s Primary Healthcare Workers for Human Well-Being and Sustainability
Abstract
1. Introduction
- To assess the technical knowledge and disaster response skills of primary healthcare professionals.
- To evaluate psychosocial readiness, including emotional intelligence, teamwork, and stress management.
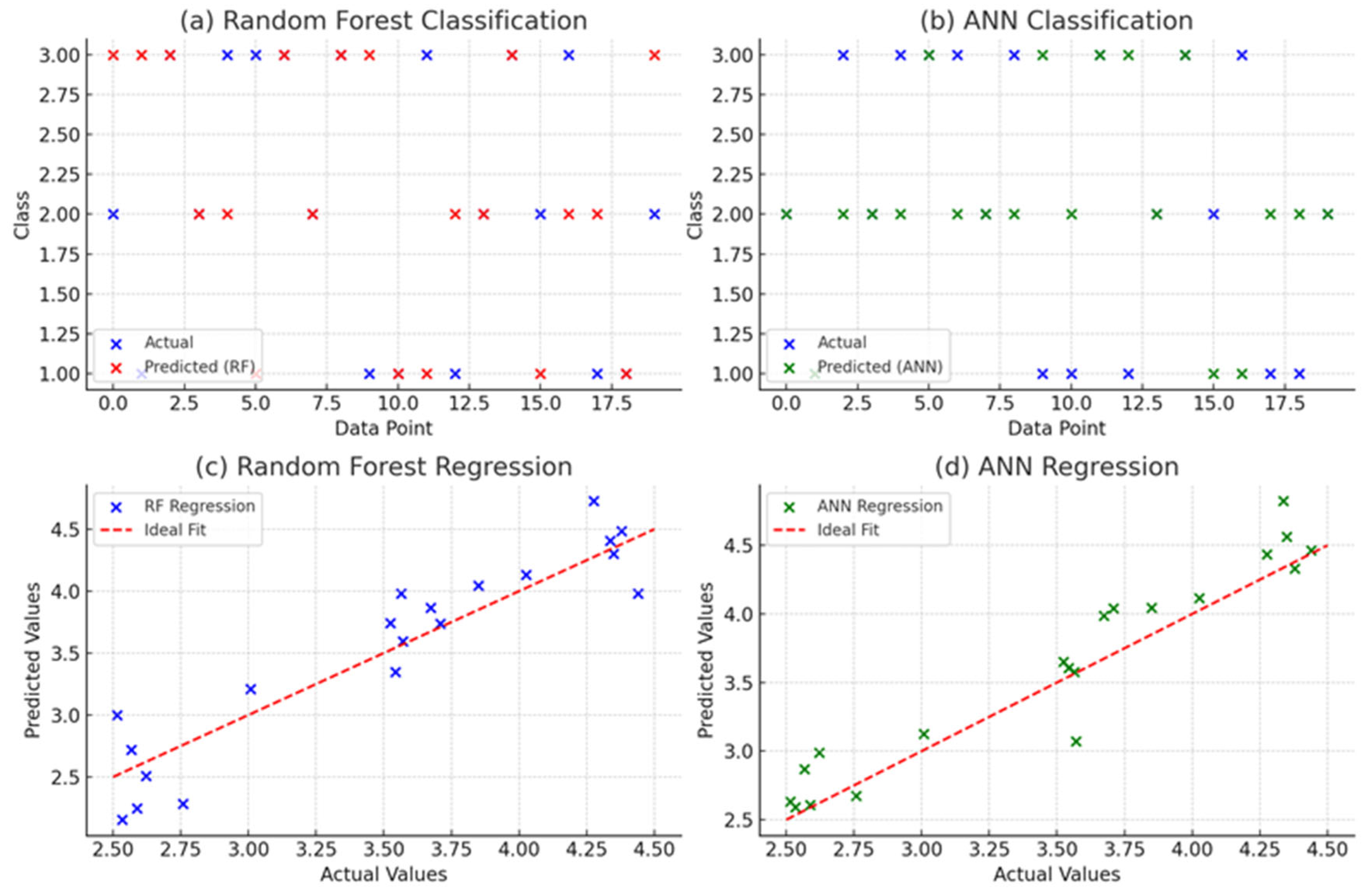
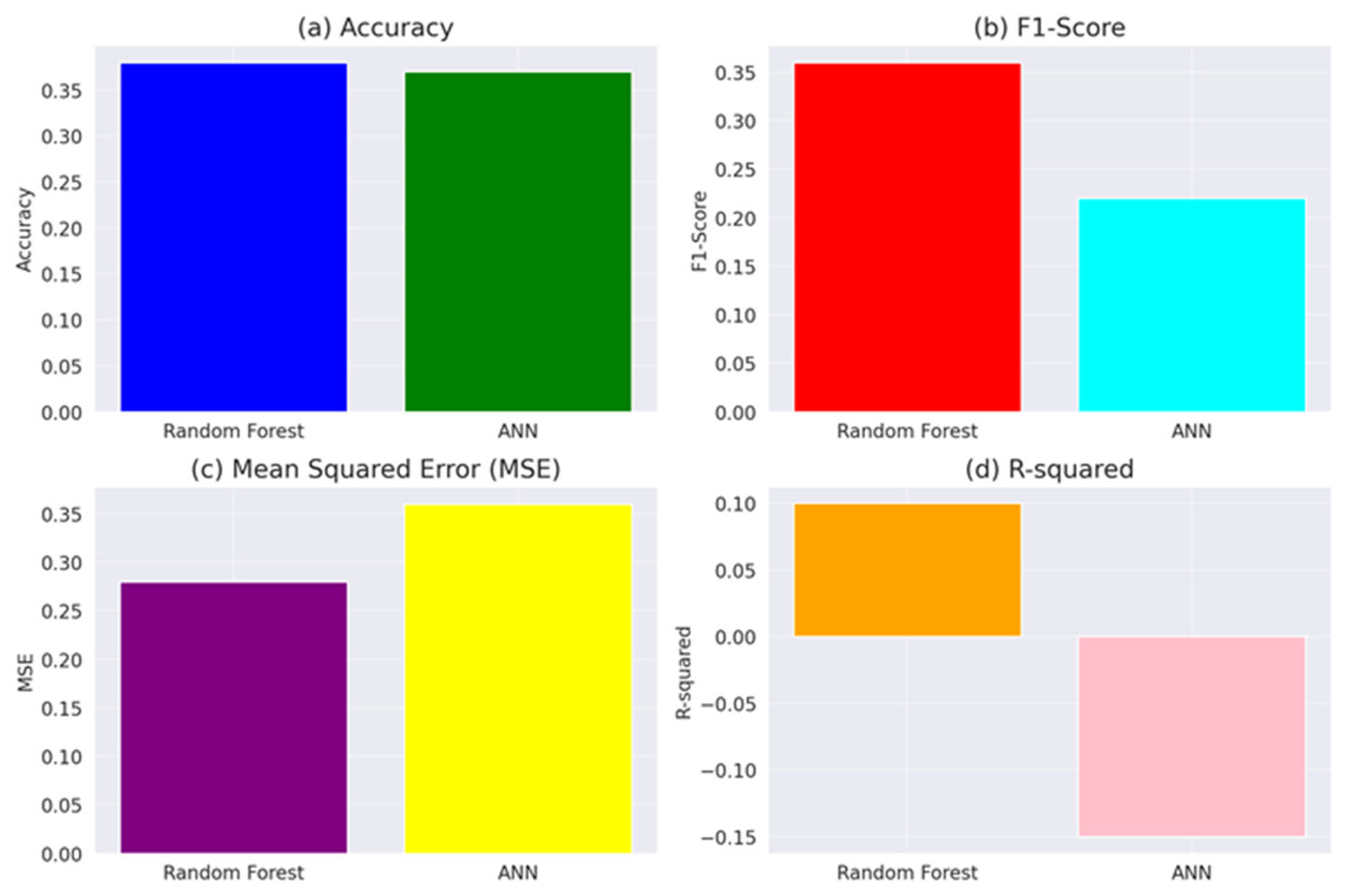
- To use machine learning models (Random Forest and Artificial Neural Networks) to predict preparedness levels.
- To identify key themes and sentiments from qualitative data related to disaster preparedness.
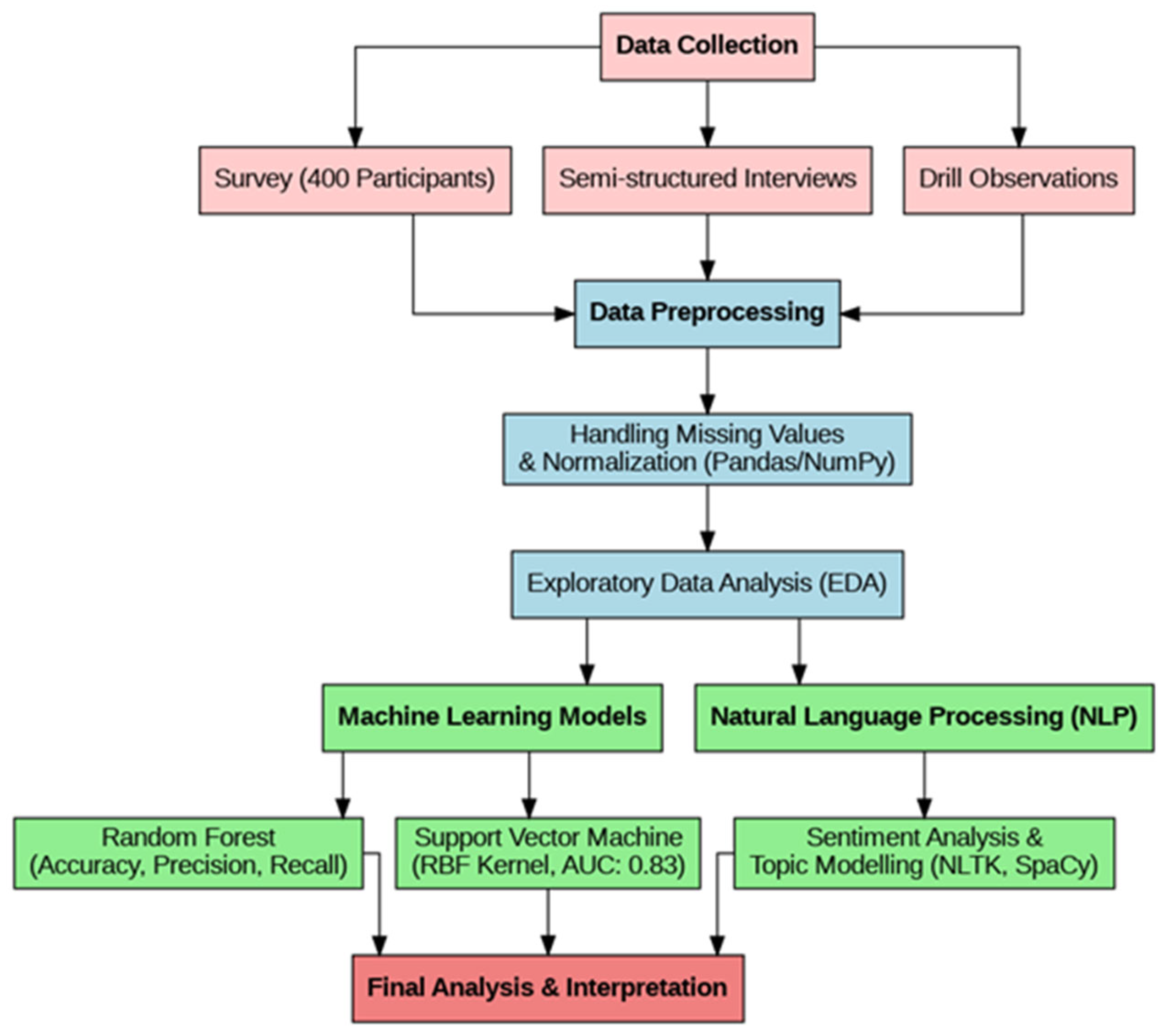
2. Materials and Methods
2.1. Data Collection
2.2. Analytical Framework
3. Results
3.1. Quantitative Findings: Technical and Psychosocial Preparedness
3.2. Psychosocial Readiness and Team Dynamics
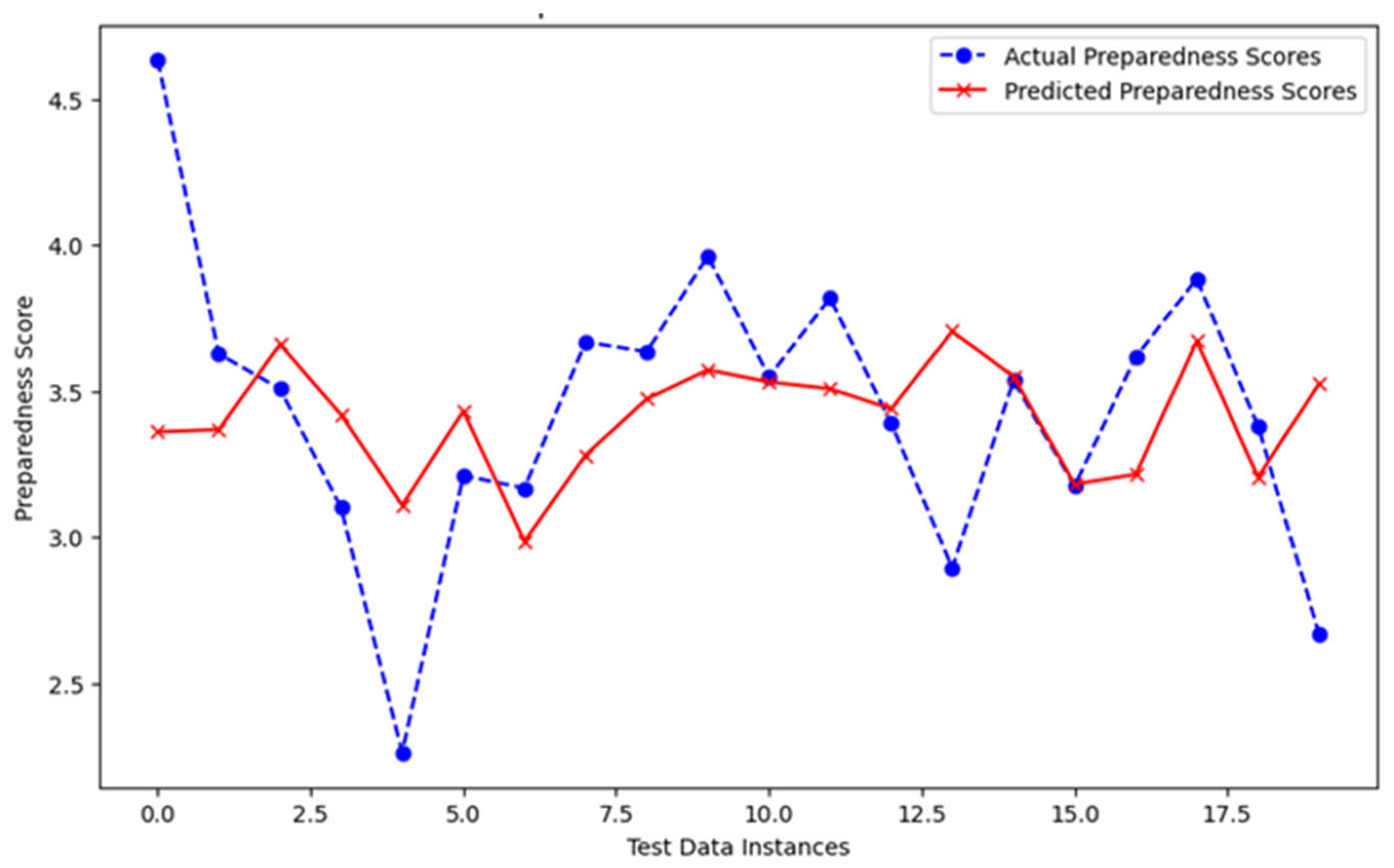
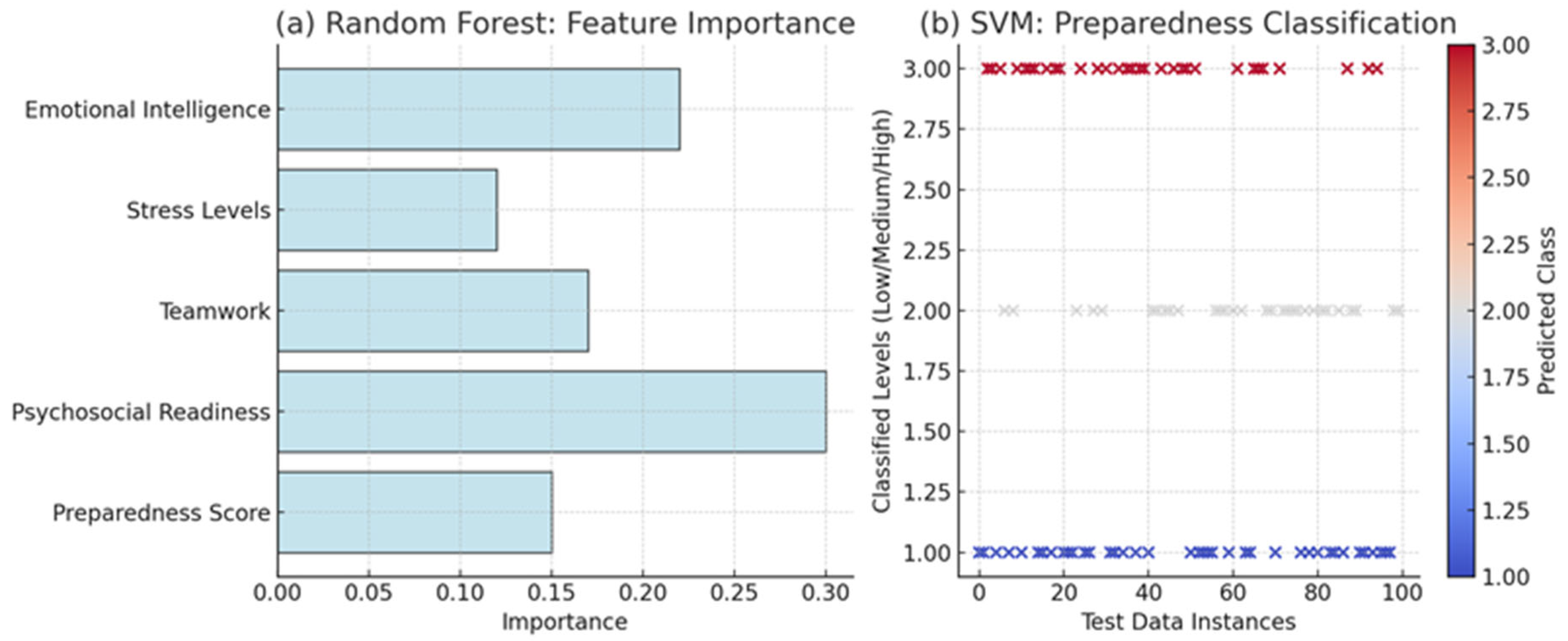
3.3. Machine-Learning Predictions of Preparedness
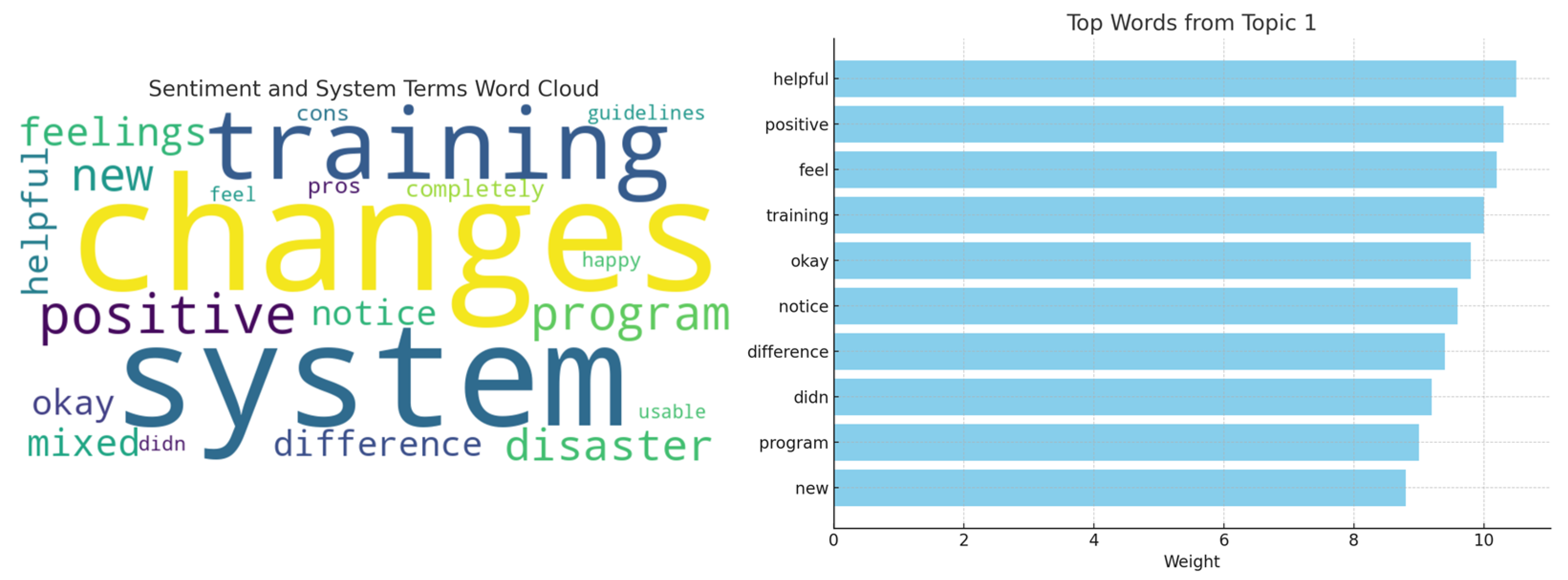
3.4. Sentiment and Topic Analysis of Qualitative Responses
3.5. Theoretical Implications
3.6. Managerial Implications
4. Discussion
4.1. Age-Related Preparedness Patterns
4.2. Occupational Differences Among Healthcare Professionals
4.3. Psychosocial Drivers of Readiness
4.4. Machine-Learning Contribution
4.5. Qualitative Sentiment and Topic Insights
4.6. Regional and Global Benchmarking
4.7. Practical Contributions and Policy Relevance
4.8. Limitations and Future Directions
- Apply the model across multiple Saudi regions and neighboring Gulf states;
- Introduce longitudinal measurement to track skill decay and psychosocial change;
- Incorporate hard performance metrics (e.g., drill completion times) and IoT-based real-time data to refine predictive accuracy.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Salam, A.; Wireko, A.A.; Jiffry, R.; Ng, J.C.; Patel, H.; Zahid, M.J.; Mehta, A.; Huang, H.; Abdul-Rahman, T.; Isik, A. The Impact of Natural Disasters on Healthcare and Surgical Services in Low- and Middle-Income Countries. Ann. Med. Surg. 2023, 85, 3774–3777. [Google Scholar] [CrossRef] [PubMed]
- Susila, I.M.D.P.; Januraga, P.P.; Utami, N.W.A. Perception of disaster preparedness and participation in training are associated with disaster preparedness among health workers. Public Health Prev. Med. Arch. 2019, 7, 8–13. [Google Scholar] [CrossRef]
- Khirekar, J.; Badge, A.; Bandre, G.R.; Shahu, S. Disaster Preparedness in Hospitals. Cureus 2023, 15, e50073. [Google Scholar] [CrossRef] [PubMed]
- Ortiz-Barrios, M.; Gul, M.; López-Meza, P.; Yucesan, M.; Navarro-Jiménez, E. Evaluation of Hospital Disaster Preparedness Using a Multi-Criteria Decision-Making Approach: The Case of Turkish Hospitals. Int. J. Disaster Risk Reduct. 2020, 49, 101748. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.S. Public Health Preparedness and Response in the USA Since 9/11: A National Health Security Imperative. Lancet 2011, 378, 953–956. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.M.; Shafi, I.; Butt, W.H.; Diez, I.D.L.T.; Flores, M.A.L.; Galán, J.C.; Ashraf, I. A Systematic Review of Disaster Management Systems: Approaches, Challenges, and Future Directions. Land 2023, 12, 1514. [Google Scholar] [CrossRef]
- Chegini, Z.; Arab-Zozani, M.; Kakemam, E.; Lotfi, M.; Nobakht, A.; Aziz Karkan, H. Disaster Preparedness and Core Competencies among Emergency Nurses: A Cross-Sectional Study. Nurs. Open 2022, 9, 1294–1302. [Google Scholar] [CrossRef] [PubMed]
- Su, Z.; McDonnell, D.; Ahmad, J.; Cheshmehzangi, A. Disaster Preparedness in Healthcare Professionals Amid COVID-19 and Beyond: A Systematic Review of Randomized Controlled Trials. Nurse Educ. Pract. 2023, 69, 103583. [Google Scholar] [CrossRef] [PubMed]
- Gillani, A.H.; Mohamed Ibrahim, M.I.; Akbar, J.; Fang, Y. Evaluation of Disaster Medicine Preparedness among Healthcare Professional Students: A Cross-Sectional Study in Pakistan. Int. J. Environ. Res. Public Health 2020, 17, 2027. [Google Scholar] [CrossRef]
- Balut, M.D.; Der-Martirosian, C.; Dobalian, A. Disaster Preparedness Training Needs of Healthcare Workers at the US Department of Veterans Affairs. South. Med. J. 2022, 115, 158–163. [Google Scholar] [CrossRef] [PubMed]
- Patel, R.K.; Pamidimukkala, A.; Kermanshachi, S.; Etminani-Ghasrodashti, R. Disaster Preparedness and Awareness among University Students: A Structural Equation Analysis. Int. J. Environ. Res. Public Health 2023, 20, 4447. [Google Scholar] [CrossRef] [PubMed]
- Wu, A.; Roemer, E.C.; Kent, K.B.; Ballard, D.W.; Goetzel, R.Z. Organizational Best Practices Supporting Mental Health in the Workplace. J. Occup. Environ. Med. 2021, 63, e925–e931. [Google Scholar] [CrossRef] [PubMed]
- Fallah Shayan, N.; Mohabbati-Kalejahi, N.; Alavi, S.; Zahed, M.A. Sustainable Development Goals (SDGs) as a Corporate Social Responsibility (CSR) Framework. Sustainability 2022, 14, 1222. [Google Scholar] [CrossRef]
- Kioupi, V.; Voulvoulis, N. Education for Sustainable Development: A Systemic Framework for Connecting the SDGs to Educational Outcomes. Sustainability 2019, 11, 6104. [Google Scholar] [CrossRef]
- Baraldo, M.; Di Franco, P.D.G. Place-Centered Emerging Technologies for Disaster Management: A Scoping Review. Int. J. Disaster Risk Reduct. 2024, 112, 104782. [Google Scholar] [CrossRef]
- Farokhzadian, J.; Mangolian Shahrbabaki, P.; Farahmandnia, H.; Eskici, G.T.; Goki, F.S. Nurses’ Challenges in Disaster Response: A Qualitative Study. BMC Emerg. Med. 2024, 24, 1. [Google Scholar] [CrossRef] [PubMed]
- Al Harthi, M.; Al Thobaity, A.; Al Ahmari, W.; Almalki, M. Challenges for Nurses in Disaster Management: A Scoping Review. Health Policy 2020, 13, 2627–2634. [Google Scholar] [CrossRef] [PubMed]
- Lamberti-Castronuovo, A.; Lamine, H.; Valente, M.; Hubloue, I.; Barone-Adesi, F.; Ragazzoni, L. Assessing Primary Healthcare Disaster Preparedness: A Study in Northern Italy. Prim. Health Care Res. Dev. 2024, 25, e16. [Google Scholar] [CrossRef] [PubMed]
- Jose, A.; Tortorella, G.L.; Vassolo, R.; Kumar, M.; Mac Cawley, A.F. Professional Competence and Its Effect on Implementing Healthcare 4.0 Technologies: Scoping Review and Future Research Directions. Int. J. Environ. Res. Public Health 2022, 20, 478. [Google Scholar] [CrossRef] [PubMed]
- Zhai, L.; Lee, J.E. Exploring and Enhancing Community Disaster Resilience: Perspectives from Different Types of Communities. Water 2024, 16, 881. [Google Scholar] [CrossRef]
- Mogård, E.V.; Rørstad, O.B.; Bang, H. The Relationship between Psychological Safety and Management Team Effectiveness: The Mediating Role of Behavioral Integration. Int. J. Environ. Res. Public Health 2023, 20, 406. [Google Scholar] [CrossRef] [PubMed]
- Ma, C.; Qirui, C.; Lv, Y. “One Community at a Time”: Promoting Community Resilience in the Face of Natural Hazards and Public Health Challenges. BMC Public Health 2023, 23, 2510. [Google Scholar] [CrossRef] [PubMed]
- Nateri, R.; Robazza, C.; Tolvanen, A.; Bortoli, L.; Hatzigeorgiadis, A.; Ruiz, M.C. Emotional Intelligence and Psychobiosocial States: Mediating Effects of Intra-Team Communication and Role Ambiguity. Sustainability 2020, 12, 9019. [Google Scholar] [CrossRef]
- Guerrero-Barona, E.; Guerrero-Molina, M.; García-Gómez, A.; Moreno-Manso, J.M.; García-Baamonde, M.E. Quality of Working Life, Psychosocial Factors, Burnout Syndrome and Emotional Intelligence. Int. J. Environ. Res. Public Health 2020, 17, 9550. [Google Scholar] [CrossRef] [PubMed]
- Guido, R.; Ferris, S.; Lofaro, D.; Conforti, D. An Overview of the Advancements in Support Vector Machine Models for Healthcare Applications: A Review. Information 2024, 15, 235. [Google Scholar] [CrossRef]
- Georgescu, I.; Bocean, C.G.; Vărzaru, A.; Rotea, C.; Mangra, M.; Mangra, G. Enhancing Organizational Resilience: The Transformative Influence of Strategic Human Resource Management Practices and Organizational Culture. Sustainability 2024, 16, 4315. [Google Scholar] [CrossRef]
- Lepelaar, M.; Wahby, A.; Rossouw, M.; Nikitin, L.; Tibble, K.; Ryan, P.J.; Watson, R.B. Sentiment Analysis of Social Survey Data for Local City Councils. J. Sens. Actuator Netw. 2022, 11, 7. [Google Scholar] [CrossRef]
- Watanabe, S.; Liu, K.; Nakamura, K.; Kozu, R.; Horibe, T.; Ishii, K.; Yasumura, D.; Takahashi, Y.; Nanba, T.; Morita, Y.; et al. Association between early mobilization in the ICU and psychiatric symptoms after surviving a critical illness: A multi-center prospective cohort study. J. Clin. Med. 2022, 11, 2587. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.J.; Eom, H.E.; Ko, J.; Park, D.H. A study on influencing factor of patient leaning phenomenon in tertiary hospitals through qualitative research: From the perspective of tertiary hospital users and managers. Korea J. Hosp. Manag. 2021, 26, 55–70. [Google Scholar]
- Ayaslıer, A.A.; Albayrak, B.; Çelik, E.; Özdemir, Ö.; Özgür, Ö.; Kırımlı, E.; Kayı, İ.; Sakarya, S. Burnout in primary healthcare physicians and nurses in Turkey during COVID-19 pandemic. Prim. Health Care Res. Dev. 2023, 24, e4. [Google Scholar] [CrossRef] [PubMed]

| Category | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Population | Healthcare providers (doctors, nurses, paramedics) working in primary healthcare centers | Non-healthcare workers |
| Experience | Healthcare providers with at least one year of experience in primary care or emergency settings | Less than one year of professional experience |
| Geographic Area | Participants working in primary health centers located in disaster-prone areas or with past disaster experience | Healthcare providers working outside disaster-prone areas. |
| Language | Healthcare providers proficient in the official language of the survey or interview | Healthcare providers not fluent in the survey/interview language |
| Preparedness | Involvement in any disaster management training, drill, or simulation within the last five years | No participation in disaster management drills or simulations |
| Willingness | Healthcare providers who voluntarily consent to participate in the study | Healthcare providers who decline or withdraw consent |
| Age | Healthcare providers aged 18–65 years | Individuals younger than 18 or older than 65 |
| Availability | Healthcare providers are available to complete surveys and conduct follow-up interviews as needed | Individuals unavailable for follow-up interviews or unable to complete the survey |
| Variable | Type | Cronbach’s Alpha (α) | KMO | Bartlett’s Test (p) | VIF | Role in ML Model |
|---|---|---|---|---|---|---|
| Stress Levels | Psychosocial Factor | 0.84 | 0.68 | 0.001 | 1.3 | Independent Variable (Input) |
| Emotional Intelligence (EI) | Psychosocial Factor | 0.87 | 0.71 | 0.000 | 1.1 | Independent Variable (Input) |
| Teamwork | Team Competency | 0.82 | 0.66 | 0.003 | 1.05 | Independent Variable (Input) |
| Psychosocial Readiness | Composite Readiness | 0.86 | 0.70 | 0.001 | 1.4 | Independent Variable (Input) |
| Employee Engagement (EE) | Organizational Factor | 0.79 | 0.64 | 0.002 | 1.2 | Independent Variable (Input) |
| Psychological Safety | Organizational Factor | 0.81 | 0.67 | 0.001 | 1.1 | Independent Variable (Input) |
| Preparedness Score | Overall Readiness Score | — | — | — | 1.2 | Target Variable (Output) |
| Variable | <20 | 20–30 | 30–40 | 40–50 | 50–60 |
|---|---|---|---|---|---|
| Sample Size (Age) | 10 | 100 | 150 | 80 | 40 |
| Experience (Years) | 20 | 100 | 150 | 80 | 40 |
| Knowledge Level | 10 | 40 | 100 | 80 | 30 |
| Skills Level | 20 | 50 | 90 | 70 | 30 |
| Drill Participation | 20 | 50 | 100 | 150 | 250 |
| Preparedness Score | 50 | 120 | 150 | 80 | 0 |
| Stress Levels | High | Moderate | Moderate | Low | Low |
| Emotional Intelligence (EI) | Low | Moderate | High | High | Moderate |
| Teamwork | Moderate | High | High | Moderate | Low |
| Psychosocial Readiness | Low | Moderate | High | High | Moderate |
| Employee Engagement (EE) | Low | High | High | Moderate | Low |
| Psychological Safety (Psy.Sfty) | Low | Moderate | High | Moderate | High |
| Variable | Doctor | Nurse | Administrative |
|---|---|---|---|
| Minimum Preparedness Score | 2.0 | 2.5 | 2.5 |
| 25th Percentile (Q1) | 3.0 | 2.8 | 3.0 |
| Median (50th Percentile) | 3.5 | 3.2 | 3.5 |
| 75th Percentile (Q3) | 4.0 | 3.5 | 4.0 |
| Maximum Preparedness Score | 4.5 | 4.0 | 4.5 |
| Stress Levels | Moderate | High | Moderate |
| Emotional Intelligence (EI) | High | Moderate | High |
| Teamwork | High | High | Moderate |
| Psychosocial Readiness | Moderate | High | Moderate |
| Employee Engagement (EE) | High | Moderate | Low |
| Psychological Safety (Psy.Sfty) | High | Moderate | Low |
| Outliers Present | Yes | Yes | Yes |
| Variable | Factor 1 (Stress and Readiness) | Factor 2 (Teamwork and Psychosocial Readiness) | |
|---|---|---|---|
| Emotional Intelligence | −0.086 | −0.400 | |
| Stress Levels | 0.981 | −0.110 | |
| Teamwork | −0.038 | −0.697 | |
| Psychosocial Readiness | 0.003 | 0.260 | |
| Preparedness Score | 0.154 | 0.439 | |
| Psychological Safety | −0.076 | 0.285 | |
| Path | From | To | Path Coefficient |
| Factor 1 (Stress and Readiness) → Stress Levels | Factor 1 (Stress and Readiness) | Stress Levels | 0.981 |
| Factor 1 (Stress and Readiness) → Preparedness Score | Factor 1 (Stress and Readiness) | Preparedness Score | 0.154 |
| Factor 2 (Teamwork and Psychosocial Readiness) → Teamwork | Factor 2 (Teamwork and Psychosocial Readiness) | Teamwork | −0.697 |
| Factor 2 (Teamwork and Psychosocial Readiness) → Psychosocial Readiness | Factor 2 (Teamwork and Psychosocial Readiness) | Psychosocial Readiness | 0.260 |
| Factor 2 (Teamwork and Psychosocial Readiness) → Psychological Safety | Factor 2 (Teamwork and Psychosocial Readiness) | Psychological Safety | 0.285 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alrowili, M.R.; Almoajel, A.M.; Alneam, F.M.; Alhazmi, R.A. Disaster Preparedness in Saudi Arabia’s Primary Healthcare Workers for Human Well-Being and Sustainability. Sustainability 2025, 17, 6562. https://doi.org/10.3390/su17146562
Alrowili MR, Almoajel AM, Alneam FM, Alhazmi RA. Disaster Preparedness in Saudi Arabia’s Primary Healthcare Workers for Human Well-Being and Sustainability. Sustainability. 2025; 17(14):6562. https://doi.org/10.3390/su17146562
Chicago/Turabian StyleAlrowili, Mona Raif, Alia Mohammed Almoajel, Fahad Magbol Alneam, and Riyadh A. Alhazmi. 2025. "Disaster Preparedness in Saudi Arabia’s Primary Healthcare Workers for Human Well-Being and Sustainability" Sustainability 17, no. 14: 6562. https://doi.org/10.3390/su17146562
APA StyleAlrowili, M. R., Almoajel, A. M., Alneam, F. M., & Alhazmi, R. A. (2025). Disaster Preparedness in Saudi Arabia’s Primary Healthcare Workers for Human Well-Being and Sustainability. Sustainability, 17(14), 6562. https://doi.org/10.3390/su17146562






