Sustainability in the Management of the Private Medical Sector in Romania: A European, USA and Japan Comparison
Abstract
1. Introduction
- Assess environmental, social and economic sustainability practices in Romania’s private healthcare sector, with a focus on prominent providers such as Medlife, Regina Maria, Medicover and Sanador.
- Analyze health expenditure indicators and financing schemes in Romania relative to global benchmarks, identifying key correlations and sustainability challenges.
- Explore the role of technology—including telemedicine, digital health records and AI in driving sustainability in healthcare.
- Provide actionable recommendations for improving sustainability in Romania’s private healthcare sector by drawing on successful strategies from other countries.
2. Materials and Methods
2.1. Bibliographic Review on Sustainability in Healthcare Management
- Climate change and healthcare (e.g., carbon footprint and green hospitals).
- Healthcare innovations (e.g., AI, telemedicine and electronic health records).
- Public–private partnerships in healthcare.
- Health equity and sustainability in healthcare systems.
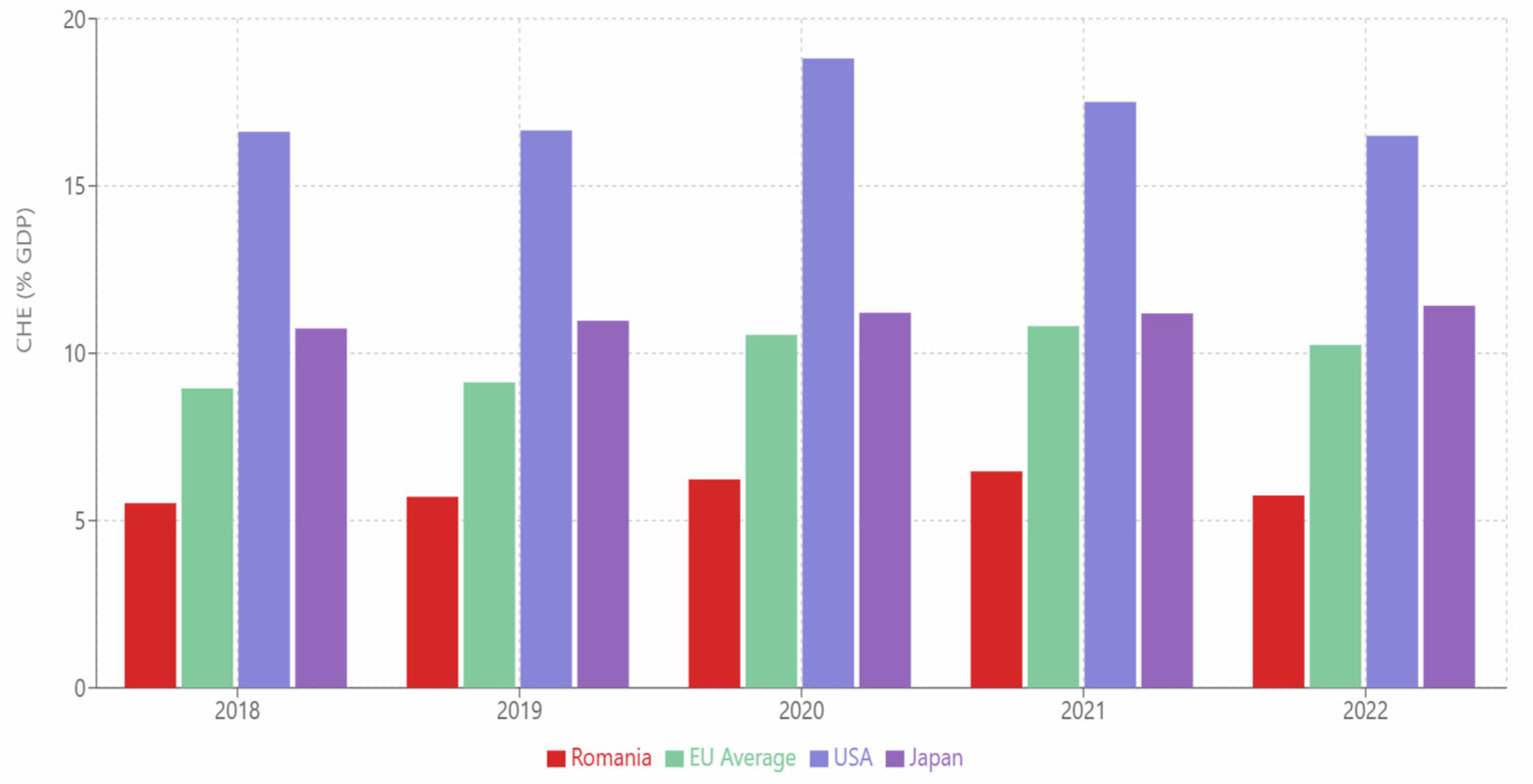
2.2. Statistical Analysis of Health Expenditure Indicators, Financing Schemes and Administrative Data for All EU Countries, USA and Japan for the Period 2018–2023
- Current Health Expenditure (CHE) as % of GDP: Measures the share of healthcare spending relative to the country’s economic output.
- Compulsory Health Insurance (CHI) as % of CHE: Indicates the reliance on mandatory health insurance schemes to finance health expenditures.
- General Government Expenditure (GGE) as % of GDP: Reflects the overall government spending relative to the economy.
- Governance, Health System and Financing Administration (in million USD): Represents the administrative costs associated with governance and health financing.
- Capital Health Expenditure: Divided into domestic public and domestic private expenditure.
- Population (in thousands): Provides context for per capita calculations and comparisons.
2.3. A Benchmarking Analysis of Sustainability Practices Across Romania, EU Countries, the USA, and Japan
3. Results
3.1. Results of Bibliographic Review on Sustainability in Healthcare Management
- Germany’s Green Hospital Program: Achieved a 25% emission reduction and significant cost savings through energy-efficient infrastructure.
- Sweden’s Renewable Energy Adoption: Integrated renewable energy into 80% of healthcare facilities, reducing emissions and energy costs.
- Identification Phase
- Screening Phase
- Eligibility Phase
- Inclusion Phase
- Language Restrictions: Primarily English sources were considered, potentially excluding relevant studies in other languages.
- Timeframe: The focus on recent literature (2013–2024) may have overlooked older foundational studies.
- Database Access: Some sources may have been inaccessible due to subscription restrictions.
3.1.1. Environmental Sustainability in Healthcare Management
- Environmental sustainability focuses on reducing the ecological footprint of healthcare facilities through energy efficiency, waste management and sustainable infrastructure. The World Health Organization (WHO) emphasizes that hospitals are among the most energy-intensive buildings, accounting for a significant share of global energy consumption [1,5,6,7,8,9]. Green hospitals are critical in reducing healthcare’s environmental footprint, with renewable energy adoption reducing emissions by 25% in participating facilities [10,11,12,13]. Developed countries such as Germany, Sweden and the Netherlands have pioneered green healthcare initiatives [12,14]. For instance, Germany’s “Green Hospital Program” incentivizes private and public hospitals to adopt energy-efficient technologies and renewable energy sources, contributing to a 25% reduction in emissions in participating hospitals between 2015 and 2022 [12,15,16,17].
- Similarly, Sweden’s healthcare sector has integrated renewable energy into 80% of its facilities, significantly reducing its carbon footprint [12,14,18]. The Netherlands has adopted circular economy principles in healthcare, with hospitals recycling up to 70% of their medical waste and reusing medical devices where feasible [19]. However, in low- and middle-income countries (LMICs), limited financial resources hinder the implementation of green practices [5,20]. Despite these challenges, global initiatives like Healthcare Without Harm and the Global Green and Healthy Hospitals Network promote environmentally sustainable practices worldwide, offering frameworks for reducing waste, energy use and carbon emissions [10,12,21].
3.1.2. Social Sustainability and Healthcare Equity
- Social sustainability in healthcare involves ensuring equitable access to services for all population groups, addressing disparities in care delivery and supporting workforce well-being. Research by Marmot (2020) [6] highlights that inequities in healthcare access are exacerbated in privatized systems, where higher-income groups benefit disproportionately [22,23,24,25]. Countries like Canada and Sweden have successfully integrated private providers into public healthcare systems, ensuring universal access through robust public–private collaboration [23,26,27,28].
- Telemedicine has emerged as a vital tool for addressing healthcare inequities, particularly in underserved rural areas. Telemedicine reduces geographical barriers, enabling patients in remote regions to access specialized care [3,29,30,31,32]. During the COVID-19 pandemic, telemedicine adoption accelerated globally, improving healthcare access in both high- and low-income countries. However, challenges remain, including the digital divide and the need for infrastructure investment to expand telehealth services. Studies also highlight the importance of addressing digital equity in telemedicine adoption, especially in low-income regions.
3.1.3. Economic Sustainability in Healthcare Management
- Economic sustainability in healthcare focuses on achieving financial viability while maintaining affordability for patients [24,33,34]. In countries like the United States and Switzerland, private providers have implemented value-based care models that prioritize patient outcomes while reducing costs [34,35,36,37]. Public–private partnerships (PPPs) have proven effective in reducing the financial burden on private providers while expanding access to care. For example, Germany’s PPPs [12,17] have facilitated the modernization of healthcare infrastructure, enabling private hospitals to access public funding for technology upgrades and facility expansions [22,38].
- In low- and middle-income countries (LMICs), economic sustainability remains a challenge due to high operational costs and limited revenue streams. Research by the Organisation for Economic Co-operation and Development (OECD) indicates that governments in these countries must strengthen collaboration with private providers to improve healthcare access and sustainability [22,39]. The adoption of cost-optimization tools, such as AI-driven predictive analytics, has shown promise in reducing operational inefficiencies and improving resource allocation in hospitals worldwide [4,40,41,42]. Advanced waste management technologies, such as autoclaves and waste-to-energy systems, also provide dual benefits of environmental and economic sustainability [43,44,45,46,47,48].
3.1.4. The Role of Technology in Driving Sustainability
- Technology is a cornerstone of sustainability in healthcare, enabling providers to address environmental, social and economic challenges effectively. Innovations such as artificial intelligence (AI), the Internet of Things (IoT) and telemedicine have transformed healthcare delivery globally [2,4,49,50]. For instance, AI-powered tools are being used in the United Kingdom to predict patient demand, optimize staffing and reduce energy consumption in hospitals [51]. The adoption of electronic health records (EHRs) has streamlined patient management and reduced paper waste in countries like Germany, Sweden and the United States [35,52].
- Moreover, telemedicine has enhanced access to care while reducing healthcare’s environmental impact by minimizing patient travel [53]. Studies show that telemedicine adoption in the United States has reduced carbon emissions associated with patient transportation by 18% annually. Blockchain technology is also emerging as a tool to enhance administrative efficiency and support data security in healthcare systems. These technologies not only improve efficiency but also support the long-term sustainability goals of healthcare providers [54].
3.2. Results of the Statistical Analysis of Health Expenditure Indicators, Financing Schemes and Administrative Data for All EU Countries, the USA and Japan for the Period 2018–2023
- IBM SPSS Statistics (Version 28.0), used for calculating correlation coefficients (Pearson and Spearman) and performed descriptive statistics and regression analyses.
- Microsoft Excel, used for data cleaning, preparation and preliminary visualization (e.g., trend analysis and bar charts), calculated basic descriptive statistics (e.g., means, medians and standard deviations).
- R (Version 4.2.2), conducted advanced statistical tests, including multivariate analysis and visualizations, used libraries such as ggplot2 for data visualization and correlation for correlation matrices.
- Python 3.11.3 (with Pandas, NumPy and SciPy libraries), utilized for exploratory data analysis (EDA) to identify outliers and trends, supported additional statistical validation for robustness.
- Correlation analysis was used with the purpose of assessing relationships between key health expenditure indicators. Pearson correlation coefficients were used for linear relationships between two continuous variables: CHE as % of GDP vs. CHI as % of CHE. Spearman’s rank correlation was used for non-linear relationships or ordinal data: CHE as % of GDP vs. governance costs. A significance level (p-value) of 0.05 was used to determine statistical significance. Correlation values (r) were interpreted as follows:
- Regression Analysis was used with the purpose of exploring the predictive power of one variable over another. For example, CHE as % of GDP predicting governance costs. The method employed was Linear Regression with the dependent variable governance costs (in million USD). The independent variable was CHE as % of GDP.
- Multivariate analysis was used for the purpose of assessing the combined impact of multiple indicators on sustainability metrics. The method employed was Principal Component Analysis (PCA), used to reduce dimensionality and identify key factors explaining variance in the dataset. The indicators included the following: CHE, CHI, GGE and governance costs.
- Descriptive statistics were used to compute the mean, median, standard deviation and interquartile range for all indicators to summarize the data.
- Trend analysis was used to evaluate how sustainability metrics evolved over time (e.g., CHE as % of GDP). Time-series analysis tracked changes in indicators from 2018 to 2023.
- Current Health Expenditure (CHE) as % of GDP—Measures the share of healthcare spending relative to economic output.
- Compulsory Health Insurance (CHI) as % of CHE—Indicates reliance on mandatory health insurance schemes for financing.
- General Government Expenditure (GGE) as % of GDP—Reflects overall government spending relative to GDP.
- Governance Costs (in million USD)—Represents administrative costs associated with health financing.
- Capital Health Expenditure (public vs. private)—Split into domestic public and private expenditures.
- Population (in thousands)—Provided context for per capita calculations.
- Correlation Analysis: CHE as % of GDP vs. CHI as % of CHE:
- Regression Analysis
- Multivariate Analysis (PCA)
- Time-Series Analysis
- Data Gaps: Missing 2023 data for some countries (e.g., Romania’s capital health expenditure).
- Assumptions: Linear relationships were assumed for regression models, which may not fully capture non-linear dynamics.
- Sample Size: Limited to EU countries, the USA and Japan, which may restrict generalizability.
- Significance Threshold: A strict p-value cutoff (0.05) may overlook smaller but meaningful effects.
- The statistical analysis aligns with key findings in the bibliographic review.
- Correlation between CHE and governance costs.
- The findings highlight that higher CHE (e.g., USA and Germany) leads to higher governance costs, confirming the correlation analysis.
- Time-Series Trends: The rising CHE in Romania and the USA, supported by the time-series analysis.
- PCA Findings: The identification of governance costs and CHI as key contributors to sustainability aligns with the recommendations for optimizing administrative efficiency and financing models.
- Policy Implications: Statistical findings support this article’s call for Romania to adopt hybrid financing models and reduce governance inefficiencies.
3.2.1. Key Observations in the Indicators Included in the Dataset
- Current Health Expenditure (CHE) as % of GDP vs. Compulsory Health Insurance (CHI) as % of CHE:
- CHE as % of GDP vs. General Government Expenditure (GGE) as % of GDP:
- CHE as % of GDP vs. Governance and Administration Costs:
3.2.2. Regional and Country-Level Observations
- USA:
- EU Countries:
- Japan:
3.2.3. Capital Health Expenditure (Public vs. Private)
- Countries with higher public capital health expenditure (e.g., Germany and Denmark) tend to have lower private contributions, indicating a robust public financing system.
- Countries with significant private capital health expenditure (e.g., USA and Latvia) may risk inequities in access to healthcare services.
3.2.4. Management Sustainability
- Financing Models:
- Administrative Costs:
- Population Trends:
3.2.5. Relevance to Romania
3.3. Key Players in Romania’s Private Medical Sector and European Benchmarking
3.3.1. Major Private Players in Romania
- Medlife: Romania’s largest healthcare provider with over 230 clinics, 14 hospitals and 33 laboratories. Medlife is known for its technological innovation and is expanding its network to underserved areas.
- Regina Maria: Operating 70 clinics and 19 hospitals, Regina Maria emphasizes digital transformation and telemedicine, serving over 3 million patients annually.
- Medicover: A multinational company with 37 facilities in Romania, Medicover specializes in corporate health programs and preventative care.
- Sanador: Focused on tertiary care, Sanador operates the largest private hospital in Bucharest, offering advanced diagnostic and surgical services.
3.3.2. Sustainability Practices in Romania vs. EU Countries
- Romania: While providers like Medlife and Regina Maria have piloted renewable energy projects, only 15% of private healthcare facilities in Romania have adopted green building standards. Waste management programs remain underdeveloped, with limited recycling and energy recovery initiatives. The financial benefits of green practices are underutilized in the Romanian private healthcare sector. For instance, Medlife could adopt waste-to-energy initiatives, like those in Sweden, to reduce waste disposal costs while generating energy.
- Germany: Hospitals participating in Germany’s Green Hospital Program report significant cost savings. For example, a medium-sized private hospital in Bavaria installed energy-efficient Heating, Ventilation and Air Conditioning (HVAC) systems and reported annual savings of EUR 350,000 in operational costs within five years of implementation [15].
- Sweden: Swedish hospitals have achieved long-term economic benefits from renewable energy adoption. A case study from Karolinska University Hospital showed that switching to geothermal heating and cooling reduced energy costs by EUR 500,000 annually, with an ROI achieved in just four years. Sweden’s geothermal and solar energy systems serve as benchmarks for Romania.
- Romania: Access to private healthcare is limited by cost, with services unaffordable for 40% of the population. Providers like Medicover have expanded telemedicine but struggle to reach rural areas. Workforce retention is another challenge, with high migration rates among healthcare professionals [59,60,61].
- Germany: Private healthcare is well-integrated with public insurance, making services more accessible. Workforce shortages are less acute due to strong retention programs and competitive salaries.
- Sweden: Sweden’s private healthcare sector prioritizes equity, with government subsidies ensuring access for low-income patients. Strong workforce development initiatives reduce turnover.
- Poland: Similarly to Romania, Poland faces significant disparities in access to private healthcare. However, providers like Medicover Poland have introduced subsidized care programs to address inequities.
- Romania: Rising operational costs, such as energy expenses and regulatory compliance, strain profitability. Limited integration with public insurance further restricts revenue streams.
- Germany: Private providers benefit from robust public–private partnerships, reducing financial burdens through shared infrastructure and resources.
- Sweden: Government incentives for green investments and integrated insurance systems contribute to the financial stability of private providers.
- Poland: Like Romania, Poland’s private healthcare sector faces high operational costs, but increasing partnerships with public insurance providers are improving financial sustainability.
3.4. The Role of Technology in Achieving Sustainability
3.4.1. Telemedicine
- Impact: In 2023, Regina Maria reported a 30% increase in telemedicine usage, with significant uptake in rural areas. Similar models in Sweden have demonstrated how telemedicine can reduce carbon emissions by minimizing patient travel.
3.4.2. Digital Health Records
- Romania: Medlife and Medicover have implemented electronic health record (EHR) systems across their networks, improving efficiency and reducing administrative costs.
- Comparison: Germany and Sweden have achieved nearly universal adoption of electronic health records (EHRs), resulting in significant reductions in operational waste and enhanced patient care coordination.
3.4.3. Operational Optimization
- Romania: Medlife has piloted AI tools to predict patient demand, ensuring better staffing and resource management.
- Comparison: In Germany, AI-driven tools have reduced hospital energy consumption by up to 15%, showcasing the potential for technology to enhance environmental sustainability.
3.4.4. Advanced Medical Technologies
- Impact: While these technologies are resource-intensive initially, they reduce long-term costs and improve patient outcomes.
3.4.5. Energy Efficiency Technologies
- ROI Example: A study in the United Kingdom found that hospitals implementing IoT-based energy monitoring systems reduced energy expenses by 20–30%, with an ROI achieved in less than three years.
- Romania’s Potential: Romanian providers like Medicover and Sanador could implement similar IoT solutions to optimize energy use and reduce operational costs.
3.4.6. Waste Management Innovations
- Romania’s Opportunity: Implementing waste-to-energy systems could help Romanian providers address waste disposal challenges while reducing energy bills.
3.4.7. Renewable Energy Investments
- Sweden: Hospitals using solar energy report annual savings of EUR 200,000–EUR 500,000, depending on facility size, with ROI achieved in 4–6 years.
- Romania: Providers like Medlife and Regina Maria could benefit from government subsidies and European Uion funding for renewable energy projects, which would significantly reduce upfront costs and improve ROI.
3.4.8. ROI Comparison of Renewable Energy Sources in Romanian Hospitals
- Global Data: Hospitals in Sweden have reported annual electricity cost savings of up to 30% after adopting solar panels, with an ROI achieved in 4–6 years.
- Romania’s Context: Romania receives an average of 210 sunny days per year, making solar energy a viable option for hospitals. The estimated installation cost for a medium-sized hospital is EUR 300,000–EUR 400,000, depending on the size of the solar array.
- ROI Estimates:
- Global Data: Karolinska University Hospital in Sweden reported savings of EUR 500,000 annually by switching to geothermal heating and cooling, with an ROI achieved in 6–8 years.
- Romania’s Context: Romania has significant geothermal potential, particularly in areas like Oradea, Bucharest and the western region. However, the upfront costs for drilling and installing geothermal systems are higher than solar energy.
- ROI Estimates:
- Global Data: Hospitals in the Netherlands that installed small-scale wind turbines reported annual savings of EUR 60,000–EUR 80,000, with an ROI achieved in 8–10 years.
- Romania’s Context: Wind energy is viable in regions like Dobrogea, which has some of the highest wind potential in Europe. However, space constraints and regulatory challenges may limit adoption in urban areas where most hospitals are located.
- ROI Estimates:
3.5. Strategies for Sustainable Healthcare Management
- Environmental Strategies
- Social Strategies
- Economic Strategies
- Cost-Effective Green Solutions for Romania
4. Discussion
- Limited availability of healthcare facilities and specialists in rural areas.
- High transportation costs and long travel times for rural residents to access urban healthcare centers.
- Telemedicine platforms can connect rural patients with urban specialists for consultations, reducing the need for travel.
- Examples of telemedicine adoption in Romania, such as the expansion of telehealth services by Regina Maria and Medlife, which have shown promising results in increasing access to care for underserved communities.
- Evidence from similar initiatives in other countries (e.g., India and Brazil) demonstrating significant improvements in healthcare equity through telemedicine.
- Mobile health (mHealth) applications can provide rural patients with access to health education, appointment scheduling and medication reminders.
- AI-enabled diagnostic tools that empower general practitioners in remote areas to make more accurate diagnoses without requiring specialist referrals [70].
- Subsidized telemedicine programs for rural residents.
- Investment in digital infrastructure, such as high-speed internet, to support telemedicine platforms.
- Training programs for rural healthcare providers to effectively use digital health tools.
- Optimize Administrative Costs:
- Balance Public and Private Financing:
- Address Aging Populations:
- Enhance Equity in Access:
4.1. Results and Interpretation
4.1.1. Environmental Sustainability—Key Findings
4.1.2. Social Sustainability and Equity—Key Findings
4.1.3. Economic Sustainability—Key Findings
4.1.4. Role of Technology—Key Findings
4.2. Broad Context and Future Research Directions
Future Research Directions
- Assess the financial and operational feasibility of green initiatives (e.g., solar panels and waste-to-energy systems) in Romania.
- Explore the role of government incentives in accelerating renewable energy adoption.
- Study the impact of telemedicine on healthcare access in rural and underserved areas.
- Investigate strategies to integrate private providers into public insurance systems.
- Evaluate the effectiveness of public–private partnerships in the Romanian healthcare sector.
- Examine the long-term financial impact of adopting AI-driven tools and other advanced technologies.
- Conduct longitudinal studies on the ROI of digital health technologies in Romanian hospitals.
- Explore the potential of blockchain technology in streamlining administrative processes and enhancing data security [54].
5. Conclusions
- Environmental Sustainability
- Social Equity
- Economic Sustainability
- Germany: Robust Compulsory Health Insurance Integration
- Sweden: Environmental Leadership
- USA: Innovation with Challenges
- Japan: Balanced Access and Efficiency
- Green Investments: Accelerate renewable energy adoption (e.g., solar panels and geothermal systems) using EU funding.
- Waste-to-Energy Systems: Implement systems to reduce disposal costs and generate energy
- Green Infrastructure: Encourage compliance with green building standards through government incentives.
- Expand Telemedicine: Improve rural access by leveraging telehealth platforms, as seen in Sweden.
- Subsidized Care: Introduce affordability programs inspired by Germany’s Compulsory Health Insurance (CHI) integration.
- Public–Private Partnerships: Strengthen collaboration with public insurers to expand revenue streams.
- Hybrid Financing Models: Combine CHI and public funds to reduce governance inefficiencies.
- Operational Optimization: Adopt AI-driven tools to predict patient demand and reduce inefficiencies.
Supplementary Materials
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| CHE | Current Health Expenditure (as % of GDP) |
| CHI | Compulsory Health Insurance (as % of Current Health Expenditure) |
| GGE | General Government Expenditure (as % of GDP) |
| LMICs | Low- and Middle-Income Countries |
| ROI | Return on Investment |
| AI | Artificial Intelligence |
| IoT | Internet of Things |
| EU | European Union |
| HVAC | Heating, Ventilation and Air Conditioning |
| HERs | Electronic Health Records |
| USA | United States of America |
| PPPs | Public–Private Partnerships |
References
- Healthcare Without Harm. Health Care’s Climate Footprint Report. 2019. Available online: https://global.noharm.org/sites/default/files/documents-files/5961/HealthCaresClimateFootprint_092319.pdf (accessed on 27 March 2025).
- Topol, E.J. Deep Medicine: How Artificial Intelligence Can Make Healthcare Human Again; Basic Books: New York, NY, USA, 2019. [Google Scholar]
- Purohit, A.; Smith, J.; Hibble, A. Does telemedicine reduce the carbon footprint of healthcare? A systematic review. Future Healthc. J. 2021, 8, e85–e91. [Google Scholar] [CrossRef] [PubMed]
- Topol, E.J. High-performance medicine: The convergence of human and artificial intelligence. Nat. Med. 2019, 25, 44–56. [Google Scholar] [CrossRef]
- Karliner, J.; Slotterback, S.; Boyd, R.; Ashby, B.; Steele, K.; Wang, J. Health care’s climate footprint: The health sector contribution and opportunities for action. Eur. J. Public Health 2020, 30, ckaa165. [Google Scholar] [CrossRef]
- Marmot, M. The Health Gap: The Challenge of an Unequal World; Bloomsbury: London, UK, 2020. [Google Scholar]
- Rodler, S.; Ramacciotti, L.S.; Maas, M.; Mokhtar, D.; Hershenhouse, J.; De Castro Abreu, A.L.; Fuchs, G.; Stief, C.G.; Gill, I.S.; Cacciamani, G.E. The Impact of Telemedicine in Reducing the Carbon Footprint in Health Care: A Systematic Review and Cumulative Analysis of 68 million Clinical Consultations. Eur. Urol. Focus 2023, 9, 873–887. [Google Scholar] [CrossRef]
- García-Sanz-Calcedo, J.; Al-Kassir, A.; Yusaf, T. Economic and Environmental Impact of Energy Saving in Healthcare Buildings. Appl. Sci. 2018, 8, 440. [Google Scholar] [CrossRef]
- Fischel, E.; Dalaison, W.; González-Mahecha, E.; Astorga, I.; Carvalho Metanias Hallack, M.; Snyder, V. Green Buildings for The Health Care Sector: Cost-effective Measures for Sustainable Design; IDB: Washington, DC, USA, 2020. [Google Scholar] [CrossRef]
- Healthcare Without Harm. Global Green and Healthy Hospitals Initiative. 2022. Available online: https://global.noharm.org/act/join-our-networks/gghh (accessed on 27 March 2025).
- Karliner, J.; Manogaran, S. Climate-smart healthcare: What does it entail? In Climate Change and the Health Sector; Routledge India: London, UK, 2021. [Google Scholar] [CrossRef]
- German Health Alliance. Green Hospital Study. 2023. Available online: https://gha.health/positionen-expertise/green-hospital. (accessed on 28 March 2025).
- Naveed, A.; Iqbal, S.; Munir, S.; Rehman, A.; Eslami, M.; Kamel, S. Renewable energy integration in healthcare systems: A case study of a hospital in Azad Jammu and Kashmir. IET Renew. Power Gener. 2024, 18, 796–809. [Google Scholar] [CrossRef]
- Alotaiby, R.; Krenyacz, E. Energy efficiency in healthcare institutions. Soc. Econ. 2023, 45, 494–511. [Google Scholar] [CrossRef]
- González, A.; García-Sanz-Calcedo, J.; Rodríguez Salgado, D. Evaluation of Energy Consumption in German Hospitals: Benchmarking in the Public Sector. Energies 2018, 11, 2279. [Google Scholar] [CrossRef]
- Available online: https://www.beckershospitalreview.com/hospital-management-administration/a-new-green-standard-how-hospitals-can-utilize-geothermal-energy-to-save-the-environment-and-money/ (accessed on 24 April 2025).
- Hengel, P.; Achstetter, K.; Blümel, M.; Schwarzbach, V.; Busse, R. Health system efficiency in Germany: Results of a pilot study to assess health system performance. Eur. J. Public Health 2022, 32, ckac131.024. [Google Scholar] [CrossRef]
- Angelino, D.; Olsson, H.B.; Eriksson, D. Sustainability in healthcare: The Nordic experience, TEM Foundation. 2022. Available online: https://www.openaccessgovernment.org/sustainability-in-healthcare-the-nordic-experience/140627/ (accessed on 24 April 2025).
- Grand View Research. Medical Waste Management Market Size, Share & Trends Analysis Report by Treatment Site (Onsite, Offsite), by Treatment (Incineration, Autoclaving, Chemical Treatment), by Region and Segment Forecasts, 2024–2030. Available online: https://www.grandviewresearch.com/industry-analysis/medical-waste-management-market (accessed on 24 April 2025).
- Organization for Economic Co-Operation and Development (OECD). Public-Private Partnerships in Healthcare: Best Practices and Challenges. 2020. Available online: https://www.weforum.org/publications/public-private-partnerships-for-health-access-best-practices/ (accessed on 18 April 2025).
- Gomez-Trujillo, A.M.; Velez-Ocampo, J.; Gonzalez-Perez, M.A. A literature review on the causality between sustainability and corporate reputation: What goes first? Manag. Environ. Qual. 2020, 31, 406–430. [Google Scholar] [CrossRef]
- International Finance Corporation. The Role of the Private Sector in Expanding Health Access to the Base of the Pyramid. 2021. Available online: https://documents1.worldbank.org/curated/en/442501492766874363/pdf/114449-WP-IFC-HealthReport-PUBLIC.pdf (accessed on 18 April 2025).
- Scholz, N. Addressing Health Inequalities in the European Union; European Parliament Think Tank: Brussels, Belgium, 2020; ISBN 978-92-846-6343-9. [Google Scholar] [CrossRef]
- Romaniuk, P.; Szromek, A.R. The evolution of the health system outcomes in Central and Eastern Europe and their association with social, economic and political factors: An analysis of 25 years of transition. BMC Health Serv. Res. 2016, 16, 95. [Google Scholar] [CrossRef] [PubMed]
- Zallman, L.; Nardin, R.; Malowney, M.; Sayah, A.; McCormick, D. Affordability of health care under publicly subsidized insurance after Massachusetts health care reform: A qualitative study of safety net patients. Int. J. Equity Health 2015, 14, 112. [Google Scholar] [CrossRef] [PubMed]
- Case Study: The Largest Geothermal System in Canadian Healthcare. 2023. Available online: https://www.smithandandersen.com/news/insight/case-study-largest-geothermal-system-canadian-healthcare (accessed on 9 May 2025).
- Hussein, D. Public-Private Partnerships: A Pathway to Health Equity in Developing Countries. Barw Med. J. 2025, 3. [Google Scholar] [CrossRef]
- Joudyian, N.; Doshmangir, L.; Mahdavi, M.; Tabrizi, J.S.; Gordeev, V.S. Public-private partnerships in primary health care: A scoping review. BMC Health Serv. Res. 2021, 21, 1–18. [Google Scholar] [CrossRef]
- Combi, C.; Pozzani, G.; Pozzi, G. Telemedicine for Developing Countries. A Survey and Some Design Issues. Appl. Clin. Inform. 2016, 7, 1025–1050. [Google Scholar] [CrossRef]
- Rizos, F.; Karanikas, H.; Katsapi, A.; Tsana, M.; Tsoukas, V.; Koukoulas, G.; Drakopoulos, D.; Katsiroumpa, A.; Galanis, P. The Role of Sustainability in Telemedicine Services: The Case of the Greek National Telemedicine Network. Healthcare 2025, 13, 1046. [Google Scholar] [CrossRef]
- Lyles, C.R.; Sharma, A.E.; Fields, J.D.; Getachew, Y.; Sarkar, U.; Zephyrin, L. Centering Health Equity in Telemedicine. Ann Fam Med. 2022, 20, 362–367. [Google Scholar] [CrossRef]
- Luke, M.J.; Craig, S.; Pak-Gorstein, S.; Arellano, M.; Zhang, J.; Wright, S.M.; Chuo, J.; Scribano, P.V. Narrowing the Digital Divide: Framework for Creating Telehealth Equity Dashboards. Interact. J. Med. Res. 2024, 13, e57435. [Google Scholar] [CrossRef]
- Al Meslamani, A.Z. Challenges in health economics research: Insights from real-world examples. J. Med. Econ. 2024, 27, 215–218. [Google Scholar] [CrossRef]
- Bulatnikov, V.; Constantin, C.P. Systematic Analysis of Literature on the Healthcare Financial Models to Follow in Russia and Romania. Healthcare 2022, 10, 1086. [Google Scholar] [CrossRef]
- U.S. Department of HHS. EHR Integration in U.S. Hospitals. 2022. Available online: https://www.hhs.gov/sites/default/files/electronic-health-record-systems.pdf. (accessed on 24 April 2025).
- Patil, R.; Roy, S.; Juvekar, S. Public-Private Partnership for Providing Quality Health-Care Services in India-Vadu Rural Health Program Experience. Asian Man Int. J. 2016, 10, 216–221. [Google Scholar] [CrossRef]
- Geropoulos, N.; Voultsos, P.; Geropoulos, M.; Tsolaki, F.; Tagarakis, G. Hybrid model: A promising type of public procurement in the healthcare sector of the European Union. Front. Public Health 2024, 12, 1359155. [Google Scholar] [CrossRef] [PubMed]
- De Matteis, F.; Notaristefano, G.; Striani, F.; Borgonovi, E. Public-Private Partnerships and Public Healthcare Sustainability: The Contribution of Governance and Digitalization, A Sustainable Green Future; Springer: Cham, Switzerland, 2023. [Google Scholar] [CrossRef]
- Marx, A. Public-Private Partnerships for Sustainable Development: Exploring Their Design and Its Impact on Effectiveness. Sustainability 2019, 11, 1087. [Google Scholar] [CrossRef]
- Zdęba-Mozoła, A.; Rybarczyk-Szwajkowska, A.; Czapla, T.; Marczak, M.; Kozłowski, R. Implementation of Lean Management in a Multi-Specialist Hospital in Poland and the Analysis of Waste. Int. J. Environ. Res. Public Health 2022, 19, 800. [Google Scholar] [CrossRef] [PubMed]
- Maleki Varnosfaderani, S.; Forouzanfar, M. The Role of AI in Hospitals and Clinics: Transforming Healthcare in the 21st Century. Bioengineering 2024, 11, 337. [Google Scholar] [CrossRef]
- Stoumpos, A.I.; Kitsios, F.; Talias, M.A. Digital Transformation in Healthcare: Technology Acceptance and Its Applications. Int. J. Environ. Res. Public Health 2023, 20, 3407. [Google Scholar] [CrossRef]
- Dixit, A.; Dutta, P. Critical success factors for the adoption of circular economy in sustainable healthcare waste management. Clean Technol. Environ. Policy 2024, 26, 2181–2201. [Google Scholar] [CrossRef]
- de Aquino, A.C.T.; Gonçalves, M.F.S.; Mol, M.P.G. Healthcare waste and circular economy principles: It is time to improve! Waste Manag. Res. 2024, 42, 857–859. [Google Scholar] [CrossRef]
- Amitha, A.J.; Manoj, V. Sustainable Waste Management: Policies and Case Studies; 7th Icon SWM—ISWMAW; Ghosh, S.K., Ed.; Springer: Berlin/Heidelberg, Germany, 2017; Volume 1, pp. 167–181. [Google Scholar] [CrossRef]
- Williams, M.; Kookana, R.S. Chapter 3—Fate and Behavior of Environmental Contaminants Arising from Health-Care Provision. In Health Care and Environmental Contamination; Boxall, A.B.A., Ed.; Elsevier: Amsterdam, The Netherlands, 2018; pp. 21–40. [Google Scholar] [CrossRef]
- Arup for the European Bank for Reconstruction and Development. Energy and Resource Efficiency in Hospitals and Healthcare Facilities. 2021. Available online: https://e5p.eu/public/upload/media/Healthcare.pdf (accessed on 9 May 2025).
- Giakoumakis, G.; Politi, D.; Sidiras, D. Medical Waste Treatment Technologies for Energy, Fuels and Materials Production: A Review. Energies 2021, 14, 8065. [Google Scholar] [CrossRef]
- Wachter, R.M. The Digital Doctor: Hope, Hype and Harm at the Dawn of Medicine’s Computer Age, 1st ed.; McGraw Hill: New York, NY, USA, 2017. [Google Scholar]
- Rehman, A.; Saba, T.; Haseeb, K.; Alam, T.; Lloret, J. Sustainability Model for the Internet of Health Things (IoHT) Using Reinforcement Learning with Mobile Edge Secured Services. Sustainability 2022, 14, 12185. [Google Scholar] [CrossRef]
- Keil, M.; Frehse, L.; Hagemeister, M.; Knieß, M.; Lange, O.; Kronenberg, T.; Rogowski, W. Carbon footprint of healthcare systems: A systematic review of evidence and methods. BMJ Open 2024, 14, e078464. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services. Adoption of Electronic Health Records in U.S. Hospitals. 2022. Available online: https://www.hhs.gov/sites/default/files/fy2022-performance-plan.pdf (accessed on 9 May 2025).
- World Health Organization. Green Hospitals for a Healthier Future. 2022. Available online: https://www.who.int/indonesia/news/detail/15-08-2022-green-hospitals-for-a-healthier-future (accessed on 9 May 2025).
- Hölbl, M.; Kompara, M.; Kamišalić, A.; Nemec Zlatolas, L. A Systematic Review of the Use of Blockchain in Healthcare. Symmetry 2018, 10, 470. [Google Scholar] [CrossRef]
- Hastie, T.J.; Tibshirani, R.; Friedman, J.H. The Elements of Statistical Learning: Data Mining, Inference and Prediction. Math. Intell. 2005, 27, 83–85. [Google Scholar] [CrossRef]
- Hair, J.F.; Anderson, R.E.; Tatham, R.L.; Black, W.C. Multivariate Data Analysis: A Global Perspective; Pearson: New York, NY, USA, 2010; ISBN 0135153093. [Google Scholar]
- Komp-Leukkunen, K.; Sarasma, J. Social Sustainability in Aging Populations: A Systematic Literature Review. Gerontologist 2024, 64, gnad097. [Google Scholar] [CrossRef]
- Cygańska, M.; Kludacz-Alessandri, M. Energy Consumption Trends and Determinants in Polish Hospitals: Implications for Energy Efficiency Strategies. Sustainability 2024, 16, 9153. [Google Scholar] [CrossRef]
- Costache, C.; Dumitrascu, D.-D.; Maniu, I. Facilitators of and Barriers to Sustainable Development in Small and Medium-Sized Enterprises: A Descriptive Exploratory Study in Romania. Sustainability 2021, 13, 3213. [Google Scholar] [CrossRef]
- Matei, F.B.; Boboc, C.; Ghiță, S. The relationship corporate social responsibility and financial performances in Romanian companies. Econ. Comput. Econ. Cybern. Stud. Res. 2021, 55, 297–314. [Google Scholar]
- De Vries, N.; Lavreysen, O.; Boone, A.; Bouman, J.; Szemik, S.; Baranski, K.; Godderis, L.; De Winter, P. Retaining Healthcare Workers: A Systematic Review of Strategies for Sustaining Power in the Workplace. Healthcare 2023, 11, 1887. [Google Scholar] [CrossRef]
- Saeed, S.A.; Masters, R.M. Disparities in Health Care and the Digital Divide. Curr. Psychiatry Rep. 2021, 23, 1–6. [Google Scholar] [CrossRef]
- Coman, E.; Coman, C.; Repanovici, A.; Baritz, M.; Kovacs, A.; Tomozeiu, A.M.; Barbu, S.; Toderici, O. Does Sustainable Consumption Matter? The Influence of the COVID-19 Pandemic on Medication Use in Brasov, Romania. Sustainability 2022, 14, 8017. [Google Scholar] [CrossRef]
- Molero, A.; Calabrò, M.; Vignes, M.; Gouget, B.; Gruson, D. Sustainability in Healthcare: Perspectives and Reflections Regarding Laboratory Medicine. Ann. Lab. Med. 2021, 41, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Quttainah, M.A.; Singh, P. Barriers to Sustainable Healthcare Waste Management: A Grey Method Approach for Barrier Ranking. Sustainability 2024, 16, 11285. [Google Scholar] [CrossRef]
- Ba-Swaimi, S.; Verayiah, R.; Ramachandaramurthy, V.K.; Alahmad, A.K. An integrated and optimized framework for hybrid renewable and hydrogen energy systems in the healthcare sector: Economic, technical and environmental assessment. Int. J. Hydrog. Energy 2025, 115, 361–378. [Google Scholar] [CrossRef]
- Romero-Lankao, P.; Gnatz, D.M.; Wilhelmi, O.; Hayden, M. Urban Sustainability and Resilience: From Theory to Practice. Sustainability 2016, 8, 1224. [Google Scholar] [CrossRef]
- Porter, M.E.; van der Linde, C. Toward a new conception of the environment competitiveness relationship. J. Econ. Perspect. 1995, 9, 97–118. [Google Scholar] [CrossRef]
- Crespo-Gonzalez, C.; Benrimoj, S.I.; Scerri, M.; Garcia-Cardenas, V. Sustainability of innovations in healthcare: A systematic review and conceptual framework for professional pharmacy services. Res. Soc. Adm. Pharm. 2020, 16, 1331–1343. [Google Scholar] [CrossRef]
- Wolff, J.; Pauling, J.; Keck, A.; Baumbach, J. The Economic Impact of Artificial Intelligence in Health Care: Systematic Review. J. Med. Internet Res. 2020, 22, e16866. [Google Scholar] [CrossRef]
- Porter, M.E.; Lee, T.H. The strategy that will fix healthcare. Harv. Bus. Rev. 2013, 91, 50–70. [Google Scholar]
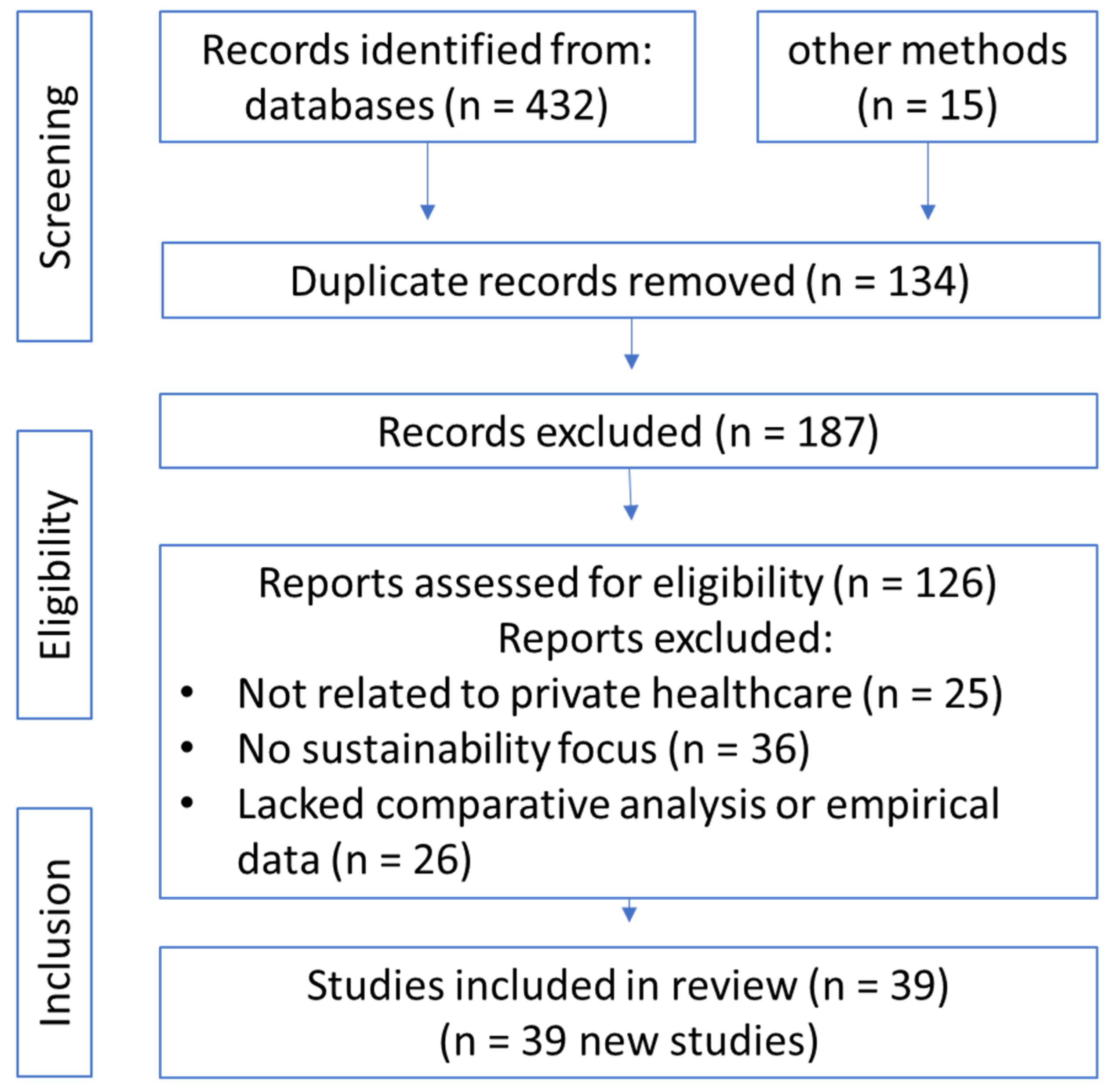


| Phase | Number of Articles |
|---|---|
| Articles Identified | 447 |
| Duplicates Removed | 134 |
| Excluded (Title/Abstract Screening) | 187 |
| Full-Text Articles Excluded | 87 |
| Articles Included | 39 |
| Indicator | Romania | Germany | Sweden | USA | Japan |
|---|---|---|---|---|---|
| CHE as % of GDP | 5.7% (2022) | 12.6% (2022) | 10.5% (2022) | 16.5% (2022) | 11.4% (2022) |
| CHI as % of CHE | Limited (~62%) | 77% | 0% (tax-funded) | 53% | 75% |
| GGE as % of GDP | 40% (2022) | 49.5% | 47.5% | 36.8% | 41.9% |
| Governance Costs (USD) | USD 433 M (2022) | USD 21 B (2022) | USD 1.7 B | USD 295 B | USD 8.3 B |
| Environmental Practices | Limited adoption of green initiatives. | Green Hospital Program; 25% emission reduction. | 80% renewable energy adoption. | High inefficiencies due to fragmented systems. | Moderate renewable energy use. |
| Social Equity | Low affordability; rural gaps. | Universal access via CHI. | Subsidized equity programs. | High disparities in access. | Strong access and affordability. |
| Renewable Energy Source | Estimated Installation Cost | Annual Savings | ROI Period | Carbon Reduction |
|---|---|---|---|---|
| Solar Energy | EUR 300,000–EUR 400,000 | EUR 80,000–EUR 120,000 | 4–6 years | 200–300 tons/year |
| Geothermal Energy | EUR 1.5–EUR 2 million | EUR 150,000–EUR 200,000 | 6–8 years | 50% reduction in heating emissions |
| Wind Energy | EUR 500,000–EUR 1 million | EUR 50,000–EUR 100,000 | 8–10 years | 100–150 tons/year |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mesteru, E.G. Sustainability in the Management of the Private Medical Sector in Romania: A European, USA and Japan Comparison. Sustainability 2025, 17, 5360. https://doi.org/10.3390/su17125360
Mesteru EG. Sustainability in the Management of the Private Medical Sector in Romania: A European, USA and Japan Comparison. Sustainability. 2025; 17(12):5360. https://doi.org/10.3390/su17125360
Chicago/Turabian StyleMesteru, Emanuel George. 2025. "Sustainability in the Management of the Private Medical Sector in Romania: A European, USA and Japan Comparison" Sustainability 17, no. 12: 5360. https://doi.org/10.3390/su17125360
APA StyleMesteru, E. G. (2025). Sustainability in the Management of the Private Medical Sector in Romania: A European, USA and Japan Comparison. Sustainability, 17(12), 5360. https://doi.org/10.3390/su17125360






