Impact of COVID-19 on Health Emergency and Disaster Risk Management System: A Scoping Review of Healthcare Workforce Management in COVID-19
Abstract
:1. Introduction
2. Materials and Methods
- Identifying the research question;
- Identifying relevant studies;
- Selecting studies;
- Presenting data;
- Collating results.
2.1. Identifying the Research Question
- What responses were made by countries against shortages in the healthcare workforce?
- What were the advantages/best practices of the responses taken?
- What were the disadvantages/lessons learnt of the responses taken?
2.2. Identifying Relevant Studies
2.3. Selecting Studies
2.4. Presenting Data
2.5. Collating Results
3. Results
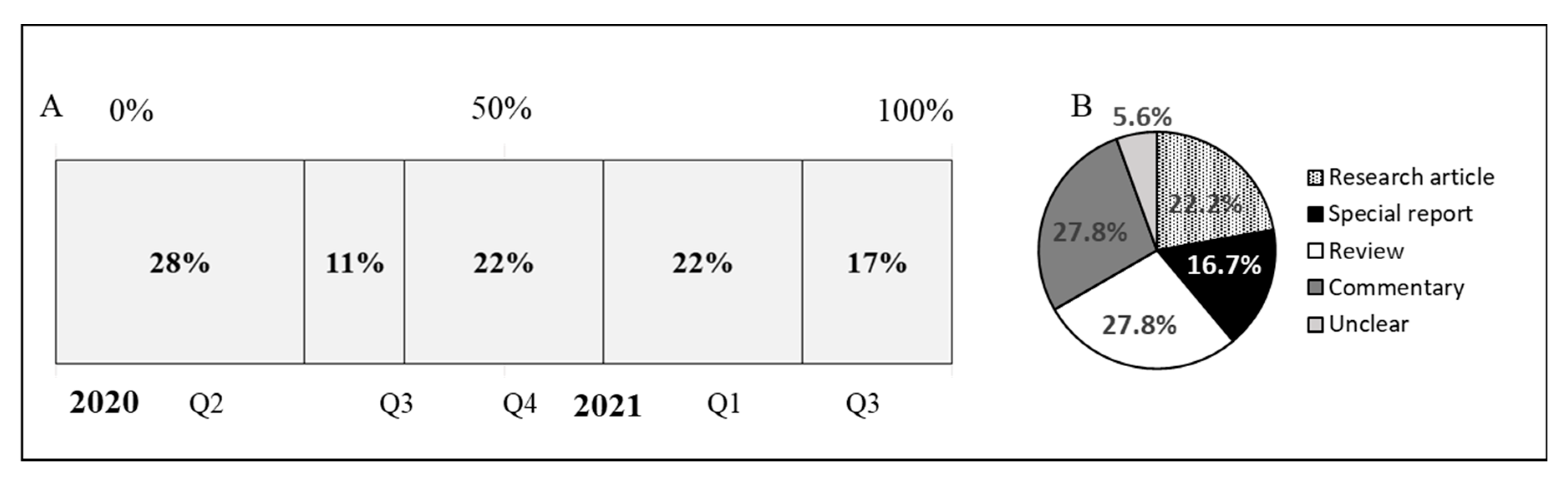
3.1. General Description of Reviewed Articles
3.2. Financial Coordination Mechanisms
3.3. Relaxation of Standards and Rules
3.4. Staff Redeployment, Task Shifting, and Skill Mixing
3.5. Recruiting Volunteers/Fast-Tracking Medical Students
3.6. Using Other Workforce Resources
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhou, P.; Yang, X.-L.; Wang, X.-G.; Hu, B.; Zhang, L.; Zhang, W.; Si, H.-R.; Zhu, Y.; Li, B.; Huang, C.-L.; et al. A Pneumonia Outbreak Associated with a New Coronavirus of Probable Bat Origin. Nature 2020, 579, 270–273. [Google Scholar] [CrossRef] [Green Version]
- WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 10 September 2022).
- Centre for Research on the Epidemiology of Disasters EM-DAT Glossary. Available online: https://www.emdat.be/Glossary#letter_d (accessed on 30 September 2022).
- Campbell, J.; Dussault, G.; Buchan, J.; Pozo-Martin, F.; Guerra Arias, M.; Leone, C.; Siyam, A.; Cometto, G. A Universal Truth: No Health without a Workforce; Global Health Workforce Alliance and World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Burau, V.; Falkenbach, M.; Neri, S.; Peckham, S.; Wallenburg, I.; Kuhlmann, E. Health System Resilience and Health Workforce Capacities: Comparing Health System Responses during the COVID-19 Pandemic in Six European Countries. Int. J. Health Plan. Manag. 2022, 37, 2032–2048. [Google Scholar] [CrossRef]
- Gupta, N.; Balcom, S.A.; Gulliver, A.; Witherspoon, R.L. Health Workforce Surge Capacity during the COVID-19 Pandemic and Other Global Respiratory Disease Outbreaks: A Systematic Review of Health System Requirements and Responses. Int. J. Health Plan. Manag. 2021, 36, 26–41. [Google Scholar] [CrossRef]
- Bal, R.; de Graaff, B.; van de Bovenkamp, H.; Wallenburg, I. Wallenburg Practicing Corona—Towards a Research Agenda of Health Policies. Health Policy 2020, 124, 671–673. [Google Scholar] [CrossRef]
- Denis, J.L.; Côté, N.; Fleury, C.; Currie, G.; Spyridonidis, D. Global Health and Innovation: A Panoramic View on Health Human Resources in the COVID-19 Pandemic Context. Int. J. Health Plan. Manag. 2021, 36, 58–70. [Google Scholar] [CrossRef]
- COVID-19 Health System Response Monitor (HSRM). Available online: https://eurohealthobservatory.who.int/monitors/hsrm/ (accessed on 1 September 2022).
- COVID-19 Health System Response Monitor. Available online: https://apo.who.int/publications/covid-19-health-system-response-monitor (accessed on 10 September 2022).
- Köppen, J.; Hartl, K.; Maier, C.B. Health Workforce Response to COVID-19: What Pandemic Preparedness Planning and Action at the Federal and State Levels in Germany? Germany’s Health Workforce Responses to COVID-19. Int. J. Health Plan. Manag. 2021, 36, 71–91. [Google Scholar] [CrossRef]
- Khalil, H.; Peters, M.; Godfrey, C.M.; McInerney, P.; Soares, C.B.; Parker, D. An Evidence-Based Approach to Scoping Reviews. Worldviews Evid. Based. Nurs. 2016, 13, 118–123. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Carroll, W.D.; Strenger, V.; Eber, E.; Porcaro, F.; Cutrera, R.; Fitzgerald, D.A.; Balfour-Lynn, I.M. European and United Kingdom COVID-19 Pandemic Experience: The Same but Different. Paediatr. Respir. Rev. 2020, 35, 50–56. [Google Scholar] [CrossRef]
- Rees, G.H.; Peralta Quispe, F.; Scotter, C. The Implications of COVID-19 for Health Workforce Planning and Policy: The Case of Peru. Int. J. Health Plan. Manag. 2021, 36, 190–197. [Google Scholar] [CrossRef]
- Dinić, M.; Šantrić Milićević, M.; Mandić-Rajčević, S.; Tripković, K. Health Workforce Management in the Context of the COVID-19 Pandemic: A Survey of Physicians in Serbia. Int. J. Health Plan. Manag. 2021, 36, 92–111. [Google Scholar] [CrossRef]
- Said, D.; Brinkwirth, S.; Taylor, A.; Markwart, R.; Eckmanns, T. The Containment Scouts: First Insights into an Initiative to Increase the Public Health Workforce for Contact Tracing during the COVID-19 Pandemic in Germany. Int. J. Environ. Res. Public Health 2021, 18, 9325. [Google Scholar] [CrossRef]
- Waitzberg, R.; Hernández-Quevedo, C.; Bernal-Delgado, E.; Estupiñán-Romero, F.; Angulo-Pueyo, E.; Theodorou, M.; Kantaris, M.; Charalambous, C.; Gabriel, E.; Economou, C.; et al. Early Health System Responses to the COVID-19 Pandemic in Mediterranean Countries: A Tale of Successes and Challenges. Health Policy 2022, 126, 465–475. [Google Scholar] [CrossRef]
- Nittayasoot, N.; Suphanchaimat, R.; Namwat, C.; Dejburum, P.; Tangcharoensathien, V. Public Health Policies and Health-Care Workers’ Response to the COVID-19 Pandemic, Thailand. Bull. World Health Organ. 2021, 99, 312–318. [Google Scholar] [CrossRef]
- Webb, E.; Winkelmann, J.; Scarpetti, G.; Behmane, D.; Habicht, T.; Kahur, K.; Kasekamp, K.; Köhler, K.; Miščikienė, L.; Misins, J.; et al. Lessons Learned from the Baltic Countries’ Response to the First Wave of COVID-19. Health Policy 2022, 126, 438–445. [Google Scholar] [CrossRef]
- Winkelmann, J.; Webb, E.; Williams, G.A.; Hernández-Quevedo, C.; Maier, C.B.; Panteli, D. European Countries’ Responses in Ensuring Sufficient Physical Infrastructure and Workforce Capacity during the First COVID-19 Wave. Health Policy 2022, 126, 362–372. [Google Scholar] [CrossRef]
- Bourgeault, I.L.; Maier, C.B.; Dieleman, M.; Ball, J.; MacKenzie, A.; Nancarrow, S.; Nigenda, G.; Sidat, M. The COVID-19 Pandemic Presents an Opportunity to Develop More Sustainable Health Workforces. Hum. Resour. Health 2020, 18, 83. [Google Scholar] [CrossRef]
- Muhammad Nur Amir, A.R.; Binti Amer Nordin, A.; Lim, Y.C.; Binti Ahmad Shauki, N.I.; Binti Ibrahim, N.H. Workforce Mobilization from the National Institutes of Health for the Ministry of Health Malaysia: A COVID-19 Pandemic Response. Front. Public Health 2021, 9, 574135. [Google Scholar] [CrossRef]
- Divito, M.; Advincula, A.; Burgansky, A.; Westhoff, C.; Williams, S.Z.; Wright, J.D.; McNamara, M.; Fuchs, K.M. Intradepartmental Redeployment of Faculty and Staff. Semin. Perinatol. 2020, 44, 151299. [Google Scholar] [CrossRef]
- Zhu, P.; Liu, X.; Wu, Q.; Loke, J.; Lim, D.; Xu, H. China’s Successful Recruitment of Healthcare Professionals to the Worst-Hit City: A Lesson Learned. Int. J. Environ. Res. Public Health 2021, 18, 8737. [Google Scholar] [CrossRef]
- Collins, G.B.; Ahluwalia, N.; Arrol, L.; Forrest, N.; McGlennan, A.; O’Brien, B.; Proudfoot, A.; Trainer, M.; Schilling, R.; Sullivan, E.; et al. Lessons in Cognitive Unloading, Skills Mixing, Flattened Hierarchy and Organisational Agility from the Nightingale Hospital London during the First Wave of the SARS-CoV-2 Pandemic. BMJ Open Qual. 2021, 10, e001415. [Google Scholar] [CrossRef]
- Vera San Juan, N.; Clark, S.E.; Camilleri, M.; Jeans, J.P.; Monkhouse, A.; Chisnall, G.; Vindrola-Padros, C. Training and Redeployment of Healthcare Workers to Intensive Care Units (ICUs) during the COVID-19 Pandemic: A Systematic Review. BMJ Open 2022, 12, e050038. [Google Scholar] [CrossRef]
- Satterfield, C.A.; Goodman, M.L.; Keiser, P.; Pennel, C.; Elliott, A.; Stalnaker, L.; Cotharn, A.; Kai, R. Rapid Development, Training, and Implementation of a Remote Health Profession’s Student Volunteer Corps during the COVID-19 Pandemic. Public Health Rep. 2021, 136, 658–662. [Google Scholar] [CrossRef] [PubMed]
- Bahethi, R.R.; Liu, B.Y.; Asriel, B.; Blum, J.R.; Huxley-Reicher, Z.; Agathis, A.Z.; Pathak, S.; Sainte Willis, M.; Muller, D. The COVID-19 Student WorkForce at the Icahn School of Medicine at Mount Sinai: A Model for Rapid Response in Emergency Preparedness. Acad. Med. 2021, 96, 859–863. [Google Scholar] [CrossRef] [PubMed]
- Satiani, B.; Zigrang, T.A.; Bailey-Wheaton, J.L. COVID-19 Financial Resources for Physicians. J. Vasc. Surg. 2020, 72, 1161–1165. [Google Scholar] [CrossRef]
- Pueyo, T. Coronavirus: The Hammer and the Dance. Available online: https://tomaspueyo.medium.com/coronavirus-the-hammer-and-the-dance-be9337092b56 (accessed on 2 September 2022).
- Asia Pacific Observatory on Health Systems and Policies India Health System Review. Available online: https://apo.who.int/publications/i/item/india-health-system-review (accessed on 2 September 2022).
- Protecting Nurses from COVID-19 a Top Priority: A Survey of ICN’s National Nursing Associations; International Council of Nurses: Geneva, Switzerland, 2020.
- Cui, M. COVID-19: China Steps in to Help Italy Battle the Viru. Available online: https://www.dw.com/en/covid-19-china-steps-in-to-help-italy-battle-the-virus/a-52901560 (accessed on 1 August 2022).
- Creese, J.; Byrne, J.-P.; Conway, E.; Barrett, E.; Prihodova, L.; Humphries, N. “We All Really Need to Just Take a Breath”: Composite Narratives of Hospital Doctors’ Well-Being during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 2051. [Google Scholar] [CrossRef]
- Lasater, K.B.; Aiken, L.H.; Sloane, D.M.; French, R.; Martin, B.; Reneau, K.; Alexander, M.; McHugh, M.D. Chronic Hospital Nurse Understaffing Meets COVID-19: An Observational Study. BMJ Qual. Saf. 2021, 30, 639–647. [Google Scholar] [CrossRef] [PubMed]
- Good Neighbor Protocol to Be Signed. Available online: https://novascotia.ca/news/release/?id=20091027005#:~:text=The%20Good%20Neighbor%20Protocol%20confirms%20how%20health%20human,the%20province%2C%20from%20other%20jurisdictions%20and%20to%20volunteers (accessed on 1 August 2022).
- Zhang, X.; Jiang, Y.; Yu, H.; Jiang, Y.; Guan, Q.; Zhao, W.; Mao, Y.; Huang, D.; Hong, W.; Li, D. Psychological and Occupational Impact on Healthcare Workers and Its Associated Factors during the COVID-19 Outbreak in China. Int. Arch. Occup. Environ. Health 2021, 94, 1441–1453. [Google Scholar] [CrossRef]
- Welsh, M. Team of Toronto Doctors and Nurses Fill in for Personal Support Staff at Nursing Homes Hit by COVID-19 Outbreak. Available online: https://www.thestar.com/news/canada/2020/04/18/team-of-toronto-doctors-and-nurses-fill-in-for-personal-support-staff-at-nursing-homes-hit-by-covid-19-outbreak.html (accessed on 6 September 2022).
- Hail the Warriors in White Gowns. Available online: https://www.bangkokpost.com/thailand/general/2042723/hail-the-warriors-in-white-gowns (accessed on 11 August 2022).
- Meng, M.; Zhang, S.; Zhai, C.-J.; Chen, D.-C. Rapidly Organize Redeployed Medical Staff in Coronavirus Disease 2019 Pandemic: What We Should Do. Chin. Med. J. 2020, 133, 2143–2145. [Google Scholar] [CrossRef]
- Li, L.; Gong, S.; Yan, J. COVID-19 in China: Ten Critical Issues for Intensive Care Medicine. Crit. Care 2020, 24, 124. [Google Scholar]
- Panda, N.; Sinyard, R.D.; Henrich, N.; Cauley, C.E.; Hannenberg, A.A.; Sonnay, Y.; Bitton, A.; Brindle, M.; Molina, G. Redeployment of Health Care Workers in the COVID-19 Pandemic: A Qualitative Study of Health System Leaders’ Strategies. J. Patient Saf. 2021, 17, 256–263. [Google Scholar] [CrossRef]
- Doyle, J.; Smith, E.M.; Gough, C., Jr.; Haq, A.; Willis, C.; Stevenson, T.; Reljic, M. Mobilising a Workforce to Combat COVID-19: An Account, Reflections, and Lessons Learned. Pediatr. Crit. Care Med. 2022, 23, 177–182. [Google Scholar] [CrossRef]
- Wells, C.M.; Zhang, Z.; Spano-Szekely, L.; Siller, J.; Brannon, H.; Schulz, K.; Scott, C.; Dolphy, M.; Hughes, E.; Kohli-Seth, R. Tiered Model of Nurse Staffing for Critical Care and Emergency Departments in the Wake of a Pandemic. J. Nurs. Adm. 2021, 51, E1–E5. [Google Scholar] [CrossRef]
- Ellis, R.; Hay-David, A.G.C.; Brennan, P.A. Operating during the COVID-19 Pandemic: How to Reduce Medical Error. Br. J. Oral Maxillofac. Surg. 2020, 58, 577–580. [Google Scholar] [CrossRef]
- Bauchner, H.; Sharfstein, J. A Bold Response to the COVID-19 Pandemic: Medical Students, National Service, and Public Health. JAMA 2020, 323, 1790–1791. [Google Scholar] [CrossRef] [Green Version]
- Kinder, F.; Harvey, A. COVID-19: The Medical Students Responding to the Pandemic. BMJ 2020, 369, m2160. [Google Scholar] [CrossRef]
- Rupley, D.; Grilo, S.A.; Kondragunta, S.; Amiel, J.; Matseoane-Peterssen, D.; Catallozzi, M.; Westhoff, C.L. Mobilization of Health Professions Students during the COVID-19 Pandemic. Semin. Perinatol. 2020, 44, 151276. [Google Scholar] [CrossRef]
- Buckland, R. Medical Student Volunteering during COVID-19: Lessons for Future Interprofessional Practice. J. Interprof. Care 2020, 34, 679–681. [Google Scholar] [CrossRef]
- Kaschel, H. Coronavirus: In Germany, Medical Students Step Up to Fight COVID-19. Available online: https://www.dw.com/en/coronavirus-in-germany-medical-students-step-up-to-fight-covid-19/a-53019943 (accessed on 5 September 2022).
- Anandaciva, S. Critical Care Services in the English NHS. Available online: https://www.kingsfund.org.uk/publications/critical-care-services-nhs (accessed on 2 September 2022).
- Kennelly, B.; O’Callaghan, M.; Coughlan, D.; Cullinan, J.; Doherty, E.; Glynn, L.; Moloney, E.; Queally, M. The COVID-19 Pandemic in Ireland: An Overview of the Health Service and Economic Policy Response. Health Policy Technol. 2020, 9, 419–429. [Google Scholar] [CrossRef]
- COVID-19: President of the German Medical Association Calls on Retired Doctors and Medical Students to Help. Germany. 2020. Available online: https://medical-guidance.com/article/covid-19-president-of-the-german-medical-association-calls-on-retired-doctors-and-medical-students-to-help1600285908 (accessed on 5 September 2022).
- Scotia, N. Ventilator Operators Look to Boost Numbers in Wake of COVID-19. Available online: https://www.cbc.ca/news/canada/nova-scotia/respiratory-therapists-covid-19-health-care-1.5509217 (accessed on 5 September 2022).
- Buerhaus, P.I.; Auerbach, D.I.; Staiger, D.O. Older Clinicians and the Surge in Novel Coronavirus Disease 2019 (COVID-19). JAMA 2020, 323, 1777–1778. [Google Scholar] [CrossRef]
- COVID-19 Temporary Registration. Available online: https://www.nmc.org.uk/news/coronavirus/temporary-registration/ (accessed on 5 September 2022).
- Barrera, J. Manitoba Chiefs Organization Wants Cuban Doctor Aid on COVID-19. Available online: https://www.cbc.ca/news/indigenous/coronavirus-manitoba-sco-wants-cuban-doctors-1.5511712 (accessed on 5 September 2022).
- Javed, N. Brampton Councillor Asks Province to Allow More Foreign-Trained Doctors to Help with COVID-19 Crisis. Available online: https://www.thestar.com/news/gta/2020/03/23/brampton-councillor-asks-province-to-allow-more-foreign-trained-doctors-to-help-with-covid-19-crisis.html (accessed on 24 March 2020).
- Montañez-Hernández, J.C.; Alcalde-Rabanal, J.; Reyes-Morales, H. Socioeconomic factors and inequality in the distribution of physicians and nurses in Mexico. Rev. Saude Publica 2020, 54, 58. [Google Scholar] [CrossRef]
- Carlin, M.; Ensign, K.; Person, C.J.; Kittle, A.; Meadows, K. State of the Public Health Workforce: Trends and Challenges Leading Up to the COVID-19 Pandemic. J. Public Health Manag. Pract. 2021, 27, 92–93. [Google Scholar] [CrossRef]
- Health Workforce Policy and Management in the Context of the COVID-19 Pandemic Response. Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-health_workforce-2020.1 (accessed on 10 September 2022).
- Chamberlain, D.; Pollock, W.; Fulbrook, P.; ACCCN Workforce Standards Development Group. ACCCN Workforce Standards for Intensive Care Nursing: Systematic and Evidence Review, Development, and Appraisal. Aust. Crit. Care 2018, 31, 292–302. [Google Scholar] [CrossRef] [Green Version]
- Ridley, E.J.; Freeman-Sanderson, A.; Haines, K.J. Surge Capacity for Critical Care Specialised Allied Health Professionals in Australia during COVID-19. Aust. Crit. Care 2021, 34, 191–193. [Google Scholar] [CrossRef]
- Litton, E.; Bucci, T.; Chavan, S.; Ho, Y.Y.; Holley, A.; Howard, G.; Secombe, P. Surge Capacity of Australian Intensive Care Units Associated with COVID-19 Admissions. Med. J. Aust. 2020, 212, 463–467. [Google Scholar] [CrossRef] [Green Version]
- Marshall, A.P.; Austin, D.E.; Chamberlain, D.; Chapple, L.-A.S.; Cree, M.; Fetterplace, K.; Foster, M.; Freeman-Sanderson, A.; Fyfe, R.; Grealy, B.A.; et al. A Critical Care Pandemic Staffing Framework in Australia. Aust. Crit. Care 2021, 34, 123–131. [Google Scholar] [CrossRef]
- Baumann, A.; Crea-Arsenio, M.; Ross, D.; Blythe, J. Diversifying the Health Workforce: A Mixed Methods Analysis of an Employment Integration Strategy. Hum. Resour. Health 2021, 19, 62. [Google Scholar] [CrossRef]
- Dubois, S. Why Financial Incentives Aren’t Enough to Deal with Health-Care Staffing Shortages. CBC News, 12 August 2022. [Google Scholar]
- Muoio, D. Will Bonuses, Benefits Solve Hospitals’ Labor Shortages? Available online: https://www.fiercehealthcare.com/hospitals/will-bonuses-and-benefits-be-enough-to-tackle-healthcare-s-workforce-shortages (accessed on 7 July 2023).
- Pallares, G. Financial Incentives for Frontline Health Workers. Available online: https://www.devex.com/news/financial-incentives-for-frontline-health-workers-98447 (accessed on 7 July 2023).
- Razu, S.R.; Yasmin, T.; Arif, T.B.; Islam, M.S.; Islam, S.M.S.; Gesesew, H.A.; Ward, P. Challenges Faced by Healthcare Professionals During the COVID-19 Pandemic: A Qualitative Inquiry from Bangladesh. Front. Public Health 2021, 9, 647315. [Google Scholar] [CrossRef]
- COVID-19 Intensifies Home Care Workforce Challenges. Available online: https://aspe.hhs.gov/reports/covid-19-intensifies-home-care-workforce-challenges (accessed on 7 July 2023).
- COVID-19 Intensifies Home Care Workforce Challenges: Agency Perspectives Issue Brief. Available online: https://aspe.hhs.gov/reports/covid-19-intensifies-home-care-workforce-challenges-agency-perspectives-issue-brief (accessed on 7 July 2023).
- Filip, R.; Gheorghita Puscaselu, R.; Anchidin-Norocel, L.; Dimian, M.; Savage, W.K. Global Challenges to Public Health Care Systems during the COVID-19 Pandemic: A Review of Pandemic Measures and Problems. J. Pers. Med. 2022, 12, 1295. [Google Scholar] [CrossRef]
- Ghotbi, N. The COVID-19 Pandemic Response and Its Impact on Post-Corona Health Emergency and Disaster Risk Management in Iran. Sustain. Sci. Pract. Policy 2022, 14, 14858. [Google Scholar] [CrossRef]
- Lamberti-Castronuovo, A.; Parotto, E.; Della Corte, F.; Hubloue, I.; Ragazzoni, L.; Valente, M. The COVID-19 Pandemic Response and Its Impact on Post-Corona Health Emergency and Disaster Risk Management in Italy. Front. Public Health 2022, 10, 1034196. [Google Scholar] [CrossRef] [PubMed]
- Ishimaru, T.; Shimizu, S.; Teshima, A.; Ibayashi, K.; Arikado, M.; Tsurugi, Y.; Tateishi, S.; Okawara, M. The Impact of COVID-19 Outbreak on Health Emergency and Disaster in Japan. Sustain. Sci. Pract. Policy 2022, 14, 15686. [Google Scholar] [CrossRef]
- Park, J.; Min, J.; Song, J.-H.; Park, M.Y.; Yoo, H.; Kwon, O.; Yang, M.; Kim, S.; Lee, J.; Myong, J.-P. The COVID-19 Pandemic Response and Its Impact on Post-Corona Health Emergency and Disaster Risk Management in Republic of Korea. Sustain. Sci. Pract. Policy 2023, 15, 3175. [Google Scholar] [CrossRef]
- Chen, A.P.; Hansoti, B.; Hsu, E.B. The COVID-19 Pandemic Response and Its Impact on Post-Pandemic Health Emergency and Disaster Risk Management in the United States. Sustain. Sci. Pract. Policy 2022, 14, 16301. [Google Scholar] [CrossRef]
- Dahn, B.; Kerr, L.; Nuthulaganti, T.; Massaquoi, M.; Subah, M.; Yaman, A.; Plyler, C.M.; Cancedda, C.; Marshall, R.E.; Marsh, R.H. Liberia’s First Health Workforce Program Strategy: Reflections and Lessons Learned. Ann. Glob. Health 2021, 87, 95. [Google Scholar] [CrossRef] [PubMed]
- Paez, A. Gray Literature: An Important Resource in Systematic Reviews. J. Evid. Based Med. 2017, 10, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Adams, J.; Hillier-Brown, F.C.; Moore, H.J.; Lake, A.A.; Araujo-Soares, V.; White, M.; Summerbell, C. Searching and Synthesising “grey Literature” and “Grey Information” in Public Health: Critical Reflections on Three Case Studies. Syst. Rev. 2016, 5, 164. [Google Scholar] [CrossRef] [Green Version]
- Liu, J.X.; Goryakin, Y.; Maeda, A.; Bruckner, T.; Scheffler, R. Global Health Workforce Labor Market Projections for 2030. Hum. Resour. Health 2017, 15, 11. [Google Scholar] [CrossRef] [Green Version]


| Database | Search Term | Number of Articles |
|---|---|---|
| PubMed * | ((“COVID-19/epidemiology”[MeSH Terms] OR “COVID-19/organization and administration”[MeSH Terms]) AND (“workforce/economics”[MeSH Terms] OR “workforce/organization and administration”[MeSH Terms] OR “workforce/supply and distribution”[MeSH Terms] OR “surge capacity/organization and administration”[MeSH Terms] OR (“personnel management/adverse effects”[MeSH Terms] OR “personnel management/instrumentation”[MeSH Terms] OR “personnel management/methods”[MeSH Terms] OR “personnel management/organization and administration”[MeSH Terms] OR “personnel management/psychology”[MeSH Terms] OR “personnel management/statistics and numerical data”[MeSH Terms] OR “personnel management/supply and distribution”[MeSH Terms]))) Filters: Free full text, English | 251 |
| Web of Science | COVID-19 (Topic) and “health* workforce” OR “human resource” (Topic) and Public Environmental Occupational Health or Health Policy Services or Multidisciplinary Sciences (Web of Science Categories) and English (Languages) | 293 |
| CINAHL |
TX healthcare workforce shortage OR TX human resource management AND TX COVID-19 Limiters—Linked Full Text; Published Date: 20200101–20221231 Expanders—Apply equivalent subjects Narrow by Language:—English Search modes—Boolean/Phrase | 46 |
| TRIP Medical Database | PICO: Population (healthcare workers OR doctors OR nurses) AND Intervention (COVID-19) AND Outcome: (country responses OR intervention OR strategies) | 12 |
| Inclusion Criteria | Exclusion Criteria | |
|---|---|---|
| Population | Healthcare workers (including physicians, nurses, allied health professionals, and support staff) working in any healthcare setting (including hospitals, primary care clinics, and community health centers) during the COVID-19 pandemic | Non-healthcare workers |
| Concept | Any type of responses that were taken to support the shortage of healthcare workforce at any levels including organizational, local, regional, and international | Only highlighting the problems and challenges of healthcare workforce but not addressing the response to these issues |
| Context | COVID-19 pandemic, including any phase of the pandemic (e.g., initial outbreak, subsequent waves, vaccination campaigns) | Non-COVID-19 infection including SARS, MERS |
| Publication type | All types of publications that were related to responses for healthcare workforce shortages during the COVID-19 pandemic and published in peer-reviewed journals | Articles in pre-print server, other publication venues, including books, book chapters and gray literature |
| Publication date | 1 January 2020 to 8 August 2022 | NA |
| Study design | Any study design, including empirical and non-empirical works that answer the research questions | Clinical randomized trials |
| Language | English | Other than English |
| N | Author Information | Article Title | Journal Published | Article Type | Study Covering Period | Publication Year | Country |
|---|---|---|---|---|---|---|---|
| 1 | Burau V, Falkenbach M, Neri S, Peckham S, Wallenburg I, Kuhlmann E. [5] | Health system resilience and health workforce capacities: Comparing health system responses during the COVID-19 pandemic in six European countries. | The International Journal of Health Planning and Management | Research article | June 2020 | 2022 | England, Germany, Denmark, Netherlands, Denmark, Austria |
| 2 | Köppen J, Hartl K, Maier CB. [11] | Health workforce response to COVID-19: What pandemic preparedness planning and action at the federal and state levels in Germany? Germany’s health workforce responses to COVID-19. | The International Journal of Health Planning and Management | Research article | May 2020 | 2021 | Germany |
| 3 | Carroll WD, Strenger V, Eber E, et al. [14] | European and United Kingdom COVID-19 pandemic experience: The same but different. | Paediatric Respiratory Reviews | Review | June 2020 | 2020 | Italy, UK |
| 4 | Rees GH, Peralta Quispe F, Scotter C. [15] | The implications of COVID-19 for health workforce planning and policy: the case of Peru. | The International Journal of Health Planning and Management | Special report | December 2020 | 2021 | Peru |
| 5 | Dinić M, Šantrić Milićević M, Mandić-Rajčević S, Tripković K. [16] | Health workforce management in the context of the COVID-19 pandemic: A survey of physicians in Serbia. | The International Journal of Health Planning and Management | Article | December 2020 | 2021 | Serbia |
| 6 | Said D, Brinkwirth S, Taylor A, Markwart R, Eckmanns T. [17] | The Containment Scouts: First Insights into an Initiative to Increase the Public Health Workforce for Contact Tracing during the COVID-19 Pandemic in Germany. | International Journal of Environmental Research and Public Health | Project report | July 2021 | 2021 | Germany |
| 7 | Waitzberg R, Hernández-Quevedo C, Bernal-Delgado E, et al. [18] | Early health system responses to the COVID-19 pandemic in Mediterranean countries: A tale of successes and challenges [published correction appears in Health Policy]. | Health Policy | Review | October 2021 | 2022 | Cyprus, Greece Israel, Italy, Malta, Portugal, Spain |
| 8 | Nittayasoot N, Suphanchaimat R, Namwat C, Dejburum P, Tangcharoensathien V. [19] | Public health policies and health-care workers’ response to the COVID-19 pandemic, Thailand. | The Bulletin of the World Health Organization | Policy & Practice | August 2020 | 2021 | Thailand |
| 9 | Webb E, Winkelmann J, Scarpetti G, et al. [20] | Lessons learned from the Baltic countries’ response to the first wave of COVID-19. | Health Policy | Summary | March 2021 | 2021 | Latvia, Estonia, Lithuania |
| 10 | Winkelmann J, Webb E, Williams GA, Hernández-Quevedo C, Maier CB, Panteli D. [21] | European countries’ responses in ensuring sufficient physical infrastructure and workforce capacity during the first COVID-19 wave. | Health Policy | Comprehensive review | February 2021 | 2022 | Albania, Armenia, Austria, Belgium, Bosnia and Herzegovina, Bulgaria, Croatia, Cyprus, Denmark, England, Estonia, France, Germany, Hungary, Iceland, Ireland, Italy, Germany, Lithuania, Luxembourg, Malta, Montenegro, Monaco, Netherlands, Norway, North Macedonia, Poland, Portugal, Romania, Russia, San Marino, Romania, Serbia, Slovenia, Spain, Sweden, Switzerland, Portugal, Turkey, Ukraine |
| 11 | Bourgeault IL, Maier CB, Dieleman M, et al. [22] | The COVID-19 pandemic presents an opportunity to develop more sustainable health workforces. | Human Resources for Health | Commentary | December 2020 | 2020 | Netherlands, Germany, Australia, Jamaica, UK, Canada, Mexico, China, USA |
| 12 | Muhammad Nur Amir AR, Binti Amer Nordin A, Lim YC, Binti Ahmad Shauki NI, Binti Ibrahim NH. [23] | Workforce Mobilization From the National Institutes of Health for the Ministry of Health Malaysia: A COVID-19 Pandemic Response. | Frontiers in Public Health | Community case study | June 2020 | 2021 | Malaysia |
| 13 | Divito M, Advincula A, Burgansky A, et al. [24] | Intradepartmental redeployment of faculty and staff. | Seminars in Perinatology | Unclear | July 2020 | 2020 | USA |
| 14 | Zhu P, Liu X, Wu Q, Loke J, Lim D, Xu H. [25] | China’s Successful Recruitment of Healthcare Professionals to the Worst-Hit City: A Lesson Learned. | International Journal of Environmental Research and Public Health | Article | July 2021 | 2021 | China |
| 15 | Collins GB, Ahluwalia N, Arrol L, et al. [26] | Lessons in cognitive unloading, skills mixing, flattened hierarchy and organisational agility from the Nightingale Hospital London during the first wave of the SARS-CoV-2 pandemic. | BMJ Open Quality | Narrative review | February 2021 | 2021 | England |
| 16 | Vera San Juan N, Clark SE, Camilleri M, et al. [27] | Training and redeployment of healthcare workers to intensive care units (ICUs) during the COVID-19 pandemic: a systematic review. | BMJ Open | Review | February 2021 | 2022 | |
| 17 | Satterfield CA, Goodman ML, Keiser P, et al. [28] | Rapid Development, Training, and Implementation of a Remote Health Profession’s Student Volunteer Corps During the COVID-19 Pandemic. | Public Health Reports | Case Reports/Practice | August 2021 | 2021 | USA |
| 18 | Bahethi RR, Liu BY, Asriel B, et al. [29] | The COVID-19 Student WorkForce at the Icahn School of Medicine at Mount Sinai: A Model for Rapid Response in Emergency Preparedness. | Academic Medicine | Innovation Report | December 2020 | 2021 | USA |
| Response Examples | Advantages/Best Practices | Disadvantages/Lessons Learned |
|---|---|---|
| Financial coordination mechanism | ||
|
|
|
| Relaxing standards and rules | ||
|
|
|
| Redeployment/task shifting/skill mixing | ||
International level:
| General/system level:
| General/system level:
|
National level:
| ||
Subnational level:
| ||
Organizational level:
| Organizational level:
| Organization level:
|
Personnel level:
| Personnel level:
| |
| Recruiting volunteer/fast-tracking medical students | ||
| General:
| General:
|
Organizational level:
| Organizational level:
| |
Personnel level:
| Personnel level:
| |
| Using other workforce resources | ||
| General:
| General:
|
Organizational level:
| ||
Personnel level:
| ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/3.0/igo/).
Share and Cite
Chimed-Ochir, O.; Amarsanaa, J.; Ghotbi, N.; Yumiya, Y.; Kayano, R.; Van Trimpont, F.; Murray, V.; Kubo, T. Impact of COVID-19 on Health Emergency and Disaster Risk Management System: A Scoping Review of Healthcare Workforce Management in COVID-19. Sustainability 2023, 15, 11668. https://doi.org/10.3390/su151511668
Chimed-Ochir O, Amarsanaa J, Ghotbi N, Yumiya Y, Kayano R, Van Trimpont F, Murray V, Kubo T. Impact of COVID-19 on Health Emergency and Disaster Risk Management System: A Scoping Review of Healthcare Workforce Management in COVID-19. Sustainability. 2023; 15(15):11668. https://doi.org/10.3390/su151511668
Chicago/Turabian StyleChimed-Ochir, Odgerel, Jargalmaa Amarsanaa, Nader Ghotbi, Yui Yumiya, Ryoma Kayano, Frank Van Trimpont, Virginia Murray, and Tatsuhiko Kubo. 2023. "Impact of COVID-19 on Health Emergency and Disaster Risk Management System: A Scoping Review of Healthcare Workforce Management in COVID-19" Sustainability 15, no. 15: 11668. https://doi.org/10.3390/su151511668
APA StyleChimed-Ochir, O., Amarsanaa, J., Ghotbi, N., Yumiya, Y., Kayano, R., Van Trimpont, F., Murray, V., & Kubo, T. (2023). Impact of COVID-19 on Health Emergency and Disaster Risk Management System: A Scoping Review of Healthcare Workforce Management in COVID-19. Sustainability, 15(15), 11668. https://doi.org/10.3390/su151511668






