The COVID-19 Pandemic Response and Its Impact on Post-Corona Health Emergency and Disaster Risk Management in Republic of Korea
Abstract
:1. Introduction
2. Materials and Methods
2.1. Methods Setting
2.2. Literature Resources
3. Results
3.1. Human Resources
3.1.1. Challenges Experienced during COVID-19 and Responses
Shortage of Medical Staff
Complicated Guideline
3.1.2. High Vulnerability
3.1.3. Lessons Learned from the Current COVID-19 Pandemic to Prepare for the Future Response
3.1.4. Impact of Challenges and Responses on the Present and Post-Corona Health-EDRM System
3.2. Health Service Delivery
3.2.1. Challenges Experienced during COVID-19 and Responses
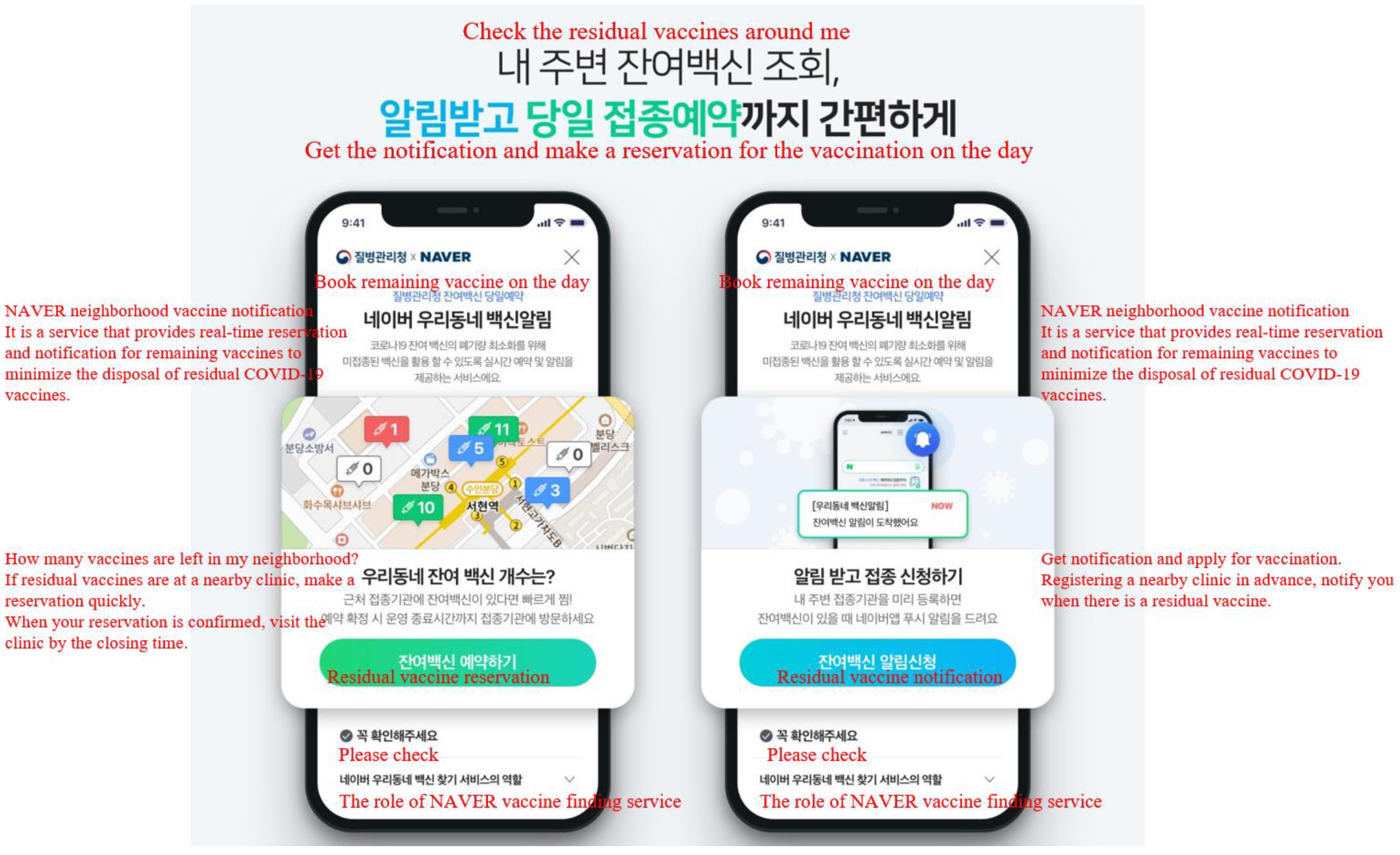
Risk Communication
Shortage of Hospitalization for COVID-19 Patients
Operation of the Emergency Medical Center
Vulnerable Groups in Healthcare
3.2.2. Lessons Learned from the Current COVID-19 Pandemic to Prepare for the Future Response
3.2.3. Impact of Challenges and Responses on the Present and Post-Corona Health-EDRM System
3.3. Logistics
3.3.1. Challenges Experienced during COVID-19 and Responses
Shortage of Personal Protective Equipment
Increasing of Non-Face-to-Face Consumption
3.3.2. Lessons Learned from the Current COVID-19 Pandemic to Prepare for the Future Response
3.3.3. Impact of Challenges and Responses on the Present and Post-Corona Health-EDRM System
4. Discussion
4.1. Human Resources
4.2. Health Service Delivery
4.3. Logistics
4.4. Limitations of Materials and Methods
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Yang, S.; Jang, J.; Park, S.Y.; Ahn, S.H.; Kim, S.S.; Ryu, B. COVID-19 outbreak report from January 20, 2020 to January 19, 2022 in the Republic of Korea. Public Health Wkly. Rep. 2022, 15, 796–805. [Google Scholar]
- Chan, E.Y.Y.; Lam, H.C.Y. Health-Related Emergency Disaster Risk Management (Health-EDRM); MDPI-Multidisciplinary Digital Publishing Institute: Basel, Switzerland, 2020. [Google Scholar]
- Ho, G.W. Where Everyone Plays a Part: Singapore’s Health EDRM Responses in Face of the COVID-19 Crisis. In COVID-19 Pandemic, Crisis Responses and the Changing World; Springer: Berlin/Heidelberg, Germany, 2021; pp. 149–157. [Google Scholar]
- World Health Organization. Health Emergency and Disaster Risk Management Framework; World Health Organization: Geneva, Switzerland, 2019.
- Hung, K.K.C.; Mashino, S.; Chan, E.Y.Y.; MacDermot, M.K.; Balsari, S.; Ciottone, G.R.; Della Corte, F.; Dell’Aringa, M.F.; Egawa, S.; Evio, B.D. Health workforce development in health emergency and disaster risk management: The need for evidence-based recommendations. Int. J. Environ. Res. Public Health 2021, 18, 3382. [Google Scholar] [PubMed]
- Kim, Y.-K.; Poncelet, J.-L.; Min, G.; Lee, J.; Yang, Y. COVID-19: Systemic risk and response management in the Republic of Korea. Prog. Disaster Sci. 2021, 12, 100200. [Google Scholar] [PubMed]
- Sanfelici, M. The Italian response to the COVID-19 crisis: Lessons learned and future direction in social development. Int. J. Community Soc. Dev. 2020, 2, 191–210. [Google Scholar]
- Tashiro, A.; Shaw, R. COVID-19 pandemic response in Japan: What is behind the initial flattening of the curve? Sustainability 2020, 12, 5250. [Google Scholar]
- Túri, G.; Virág, A. Experiences and lessons learned from COVID-19 pandemic management in South Korea and the V4 Countries. Trop. Med. Infect. Dis. 2021, 6, 201. [Google Scholar]
- Chan, E.Y.Y.; Shahzada, T.S.; Sham, T.S.T.; Dubois, C.; Huang, Z.; Liu, S.; Ho, J.Y.-e.; Hung, K.K.C.; Kwok, K.O.; Shaw, R. Narrative review of non-pharmaceutical behavioural measures for the prevention of COVID-19 (SARS-CoV-2) based on the Health-EDRM framework. Br. Med. Bull. 2020, 136, 46. [Google Scholar] [CrossRef]
- Lamberti-Castronuovo, A.; Parotto, E.; Della Corte, F.; Hubloue, I.; Ragazzoni, L.; Valente, M. The COVID-19 pandemic response and its impact on post-corona health emergency and disaster risk management in Italy. Front. Public Health 2022, 10, 1034196. [Google Scholar]
- Chen, A.P.; Hansoti, B.; Hsu, E.B. The COVID-19 Pandemic Response and Its Impact on Post-Pandemic Health Emergency and Disaster Risk Management in the United States. Sustainability 2022, 14, 16301. [Google Scholar] [CrossRef]
- Ishimaru, T.; Shimizu, S.; Teshima, A.; Ibayashi, K.; Arikado, M.; Tsurugi, Y.; Tateishi, S.; Okawara, M. The Impact of COVID-19 Outbreak on Health Emergency and Disaster in Japan. Sustainability 2022, 14, 15686. [Google Scholar] [CrossRef]
- Ghotbi, N. The COVID-19 Pandemic Response and Its Impact on Post-Corona Health Emergency and Disaster Risk Management in Iran. Sustainability 2022, 14, 14858. [Google Scholar] [CrossRef]
- Chung, H.S.; Lee, D.E.; Kim, J.K.; Yeo, I.H.; Kim, C.; Park, J.; Seo, K.S.; Park, S.-Y.; Kim, J.H.; Kim, G. Revised triage and surveillance protocols for temporary emergency department closures in tertiary hospitals as a response to COVID-19 crisis in Daegu Metropolitan City. J. Korean Med. Sci. 2020, 35, e189. [Google Scholar] [PubMed]
- Jeon, Y.; Kim, Y. COVID-19: Protecting Health-Care Workers in South Korea. Disaster Med. Public Health Prep. 2021, 16, 2355–2357. [Google Scholar]
- Shin, H.-S.; Park, H.; Kwon, J.S.; Namgoong, H.; Kim, S.-J.; Kim, J.M.; Peck, K.R.; Lee, K.; Lee, J.-k.; Lee, J. National Academy of Medicine of Korea (NAMOK) key statements on COVID-19. J. Korean Med. Sci. 2021, 36, e287. [Google Scholar] [CrossRef]
- Kim, J.-H.; An, J.A.-R.; Min, P.-k.; Bitton, A.; Gawande, A.A. How South Korea responded to the COVID-19 outbreak in Daegu. NEJM Catal. Innov. Care Deliv. 2020, 1. [Google Scholar] [CrossRef]
- Cheong, H.S.; Kwon, K.T.; Hwang, S.; Kim, S.-W.; Chang, H.-H.; Park, S.Y.; Kim, B.; Lee, S.; Park, J.; Heo, S.T. Workload of healthcare workers during the COVID-19 outbreak in Korea: A nationwide survey. J. Korean Med. Sci. 2022, 37. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y.; Shin, K.R. COVID-19: Korean nurses’ experiences and ongoing tasks for the pandemic’s second wave. Int. Nurs. Rev. 2020, 67, 445–449. [Google Scholar] [PubMed]
- Choi, S. A hidden key to COVID-19 management in Korea: Public health doctors. J. Prev. Med. Public Health 2020, 53, 175. [Google Scholar]
- Extending the Period of Intensive Operation of Cremation Facilities Nationwide (~4.30). Available online: https://ncov.kdca.go.kr/tcmBoardView.do?brdId=&brdGubun=&dataGubun=&ncvContSeq=371038&contSeq=371038&board_id=140&gubun=BDJ (accessed on 30 April 2022). (In Korean).
- Shin, J.; Cheon, M.K. Expansion of Health Care Resources to Respond to COVID-19: Three Axis. Health Welf. Issue Focus 2021, 408, 1–11. [Google Scholar]
- Mistry of Health and Welfare. The Public Health Center Supports 2064 Temporary Workers in Response to COVID-19. Available online: https://www.korea.kr/news/pressReleaseView.do?newsId=156487566. (accessed on 23 January 2023). (In Korean)
- Korea Health Promotion Institution. Korea Health Promotion Development Institute Conducts Job Training in Preparation for the Deployment of COVID-19 Korea Health Webzine. Available online: https://www.khealth.or.kr/webzine/vol_03/cnt_1_2.jsp (accessed on 15 September 2022). (In Korean).
- Sung-geun, K. Estimating the Effects of Social Distancing for COVID-19: Applying Spatially Explicit SEPIR Model. J. Korea Assoc. Policy Stud. 2021, 30, 237–270. [Google Scholar]
- Choi, K. Survey on Mental Health Status of Korean Public Health Doctors Who Dealt with COVID-19 Pandemic; 2021-18; KMA Research Institute for Healthcare Policy: Seoul, Republic of Korea, 2022. [Google Scholar]
- Han, S.; Choi, S.; Cho, S.H.; Lee, J.; Yun, J.-Y. Associations between the working experiences at frontline of COVID-19 pandemic and mental health of Korean public health doctors. BMC Psychiatry 2021, 21, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Hea, Y. A Consignment Study for the Integrated Management of Health and Medical Resources; G000BD2-2021-97; Ajou University Industry-Academic Cooperation Foundation: Suwon, Republic of Korea, 2021. [Google Scholar]
- Lee, J.-Y.; Lee, J.-y.; Lee, S.H.; Kim, J.; Park, H.Y.; Kim, Y.; Kwon, K.T. The experiences of health care workers during the COVID-19 pandemic in Korea: A qualitative study. J. Korean Med. Sci. 2021, 36, e170. [Google Scholar] [CrossRef] [PubMed]
- Development. Beyond Containment: Health Systems Responses to COVID-19 in the OECD; OECD Publishing: Paris, France, 2020. [Google Scholar]
- Minister Kwon Deok-Cheol Visited the Site of Pyeongtaek Park Ae Hospital on the 1st Anniversary of the Designation of a Hospital Dedicated to the COVID-19 Base. Available online: http://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&page=1&CONT_SEQ=368862# (accessed on 23 January 2023). (In Korean).
- Ministry of Health and Welfare. Implementation of Additional Measures to Expand Cremation Capacity and Burial Space in Cremation Facilities Nationwide. Available online: http://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&page=57&CONT_SEQ=370703 (accessed on 23 January 2023). (In Korean)
- Ministry of Health and Welfar. Emergency Room Operation Recommendations in the Event of an Infectious Disease Epidemic. 2021. Available online: https://www.ydp.go.kr/health/downloadBbsFileStr.do?bbsNo=321&atchmnflStr=A5J6ULE42SVOCC5MBLVRFAXSKYFB2AVW3LMFWUHOLR6JTZYUDNVQ_AILO (accessed on 12 December 2022).
- Centers for Disease Control and Prevention. Standard Operating Procedure (SOP) for Triage of Suspected COVID-19 Patients in Non-US Healthcare Settings: Early Identification and Prevention of Transmission during Triage; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2020.
- Han, J.H.; Lee, S.M.; Lee, D.H.; Heo, T. The analysis of the status of emergency department-based screening clinic according to the spread of coronavirus disease 2019: A retrospective single-center study. J. Korean Soc. Emerg. Med. 2022, 33, 19–27. [Google Scholar]
- Mistry of Health and Welfare. Expansion of Infrastructure for Face-to-Face and Inpatient Treatment of COVID-19 Confirmed Patients in Children; Mistry of Health and Welfare: Sejong, Republic of Korea, 2022.
- Kim, T. Improving preparedness for and response to coronavirus disease 19 (COVID-19) in long-term care hospitals in Korea. Infect. Chemother. 2020, 52, 133. [Google Scholar]
- Kwon, S.L.; Oh, J. COVID-19 vaccination program in South Korea: A long journey toward a new normal. Health Policy Technol. 2022, 11, 100601. [Google Scholar]
- Ministry of Health and Welfare. The COVID-19 Oral Antiviral Drug Will Be Introduced Tomorrow (1.13.) for 210,000 People, and Will Be Available as Early as January 14. Available online: http://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&page=32&CONT_SEQ=369685&SEARCHKEY=CONTENT&SEARCHVALUE (accessed on 20 January 2023). (In Korean)
- Yoo, J.-H.; Park, S.-K.; Cheong, I.-K. The Impact of COVID-19 and Korea’s New Southern Policy on Its Global Value Chain. J. Korea Trade 2020, 24, 19–38. [Google Scholar]
- Ministry of Food and Drug Safety. Guidelines for Preparing Anti-Droplet Mask Standards and Test Methods. Available online: https://www.mfds.go.kr/brd/m_578/view.do?seq=41854&srchFr=&srchTo=&srchWord=&srchTp=&itm_seq_1=0&itm_seq_2=0&multi_itm_seq=0&company_cd=&company_nm=&page=1 (accessed on 20 January 2023). (In Korean)
- Min-kyung, J. South Korean Government Takes Full Control of Face Mask Supply, Bans Exports. Available online: https://www.koreaherald.com/view.php?ud=20200305000730 (accessed on 20 January 2023). (In Korean).
- Ministry of Food and Drug Safety. Public-Private Partnerships Accelerate the Diagnosis of the Novel Coronavirus. Available online: https://udiportal.mfds.go.kr/brd/view/P01_01?ntceSn=42 (accessed on 20 January 2023). (In Korean)
- Ministry of SMEs and Startups, and the Korea SMEs and Startups Agency Are Recruiting Additional Companies Participating in the Aviation Maritime Freight Conservation Project. 2021. Available online: https://www.etnews.com/20210830000114 (accessed on 20 January 2023).
- The Korea SMEs and Startups Agency and the Ministry of SMEs and Startups Have Provided Support for Soaring Aviation Logistics Costs Due to COVID-19. 2021. Available online: https://www.mss.go.kr/site/smba/ex/bbs/View.do?cbIdx=86&bcIdx=1028879 (accessed on 20 January 2023).
- Choi, D. The Protection of Workers in the Consumer Logistics Service Industry Development Act, Which Supports the Delivery Ecosystem Suffering from COVID-19, Will Be Implemented Tomorrow Hankookilbo. 2021. Available online: https://www.hankookilbo.com/News/Read/A2021072610040002337 (accessed on 20 January 2023).
- Ministry of Labor. Recommend Improvement of Safety Treatment for Courier Workers in Response to COVID-19; Ministry of Labor: New Taipei, Taiwan, 2020.
- Ministry of the Interior and Safety. All About Korea’s Response to COVID-19. Available online: https://www.mois.go.kr/eng/bbs/type002/commonSelectBoardArticle.do?bbsId=BBSMSTR_000000000022&nttId=80581 (accessed on 23 January 2023). (In Korean)
- Hyeji, C.; Younghee, W. Remaining Season. The Status of Human Rights Security for the Vulnerable in the COVID-19; National Human Rights Commision: Seoul, Republic of Korea, 2021.

| Challenges Experienced during COVID-19 and Responses | Responses during COVID-19 | Lesson Learned from the Current COVID-19 Pandemic to Prepare for the Future Response | Impact of Challenges and Responses on the Present and Post-Corona Health-EDRM System |
|---|---|---|---|
|
|
|
|
| Challenges Experienced during COVID-19 and Responses | Responses during COVID-19 | Lesson Learned from the Current COVID-19 Pandemic to Prepare for the Future Response | Impact of Challenges and Responses on the Present and Post-Corona Health-EDRM System |
|---|---|---|---|
|
|
|
|
| Challenges Experienced during COVID-19 and Responses | Responses during COVID-19 | Lesson Learned from the Current COVID-19 Pandemic to Prepare for the Future Response | Impact of Challenges and Responses on the Present and Post-Corona Health-EDRM System |
|---|---|---|---|
|
|
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, J.; Min, J.; Song, J.-H.; Park, M.Y.; Yoo, H.; Kwon, O.; Yang, M.; Kim, S.; Lee, J.; Myong, J.-P. The COVID-19 Pandemic Response and Its Impact on Post-Corona Health Emergency and Disaster Risk Management in Republic of Korea. Sustainability 2023, 15, 3175. https://doi.org/10.3390/su15043175
Park J, Min J, Song J-H, Park MY, Yoo H, Kwon O, Yang M, Kim S, Lee J, Myong J-P. The COVID-19 Pandemic Response and Its Impact on Post-Corona Health Emergency and Disaster Risk Management in Republic of Korea. Sustainability. 2023; 15(4):3175. https://doi.org/10.3390/su15043175
Chicago/Turabian StylePark, Jaeyoung, Jeehee Min, Ji-Hun Song, Min Young Park, Hyoungseob Yoo, Ohwi Kwon, Munyoung Yang, Seoyoung Kim, Jongin Lee, and Jun-Pyo Myong. 2023. "The COVID-19 Pandemic Response and Its Impact on Post-Corona Health Emergency and Disaster Risk Management in Republic of Korea" Sustainability 15, no. 4: 3175. https://doi.org/10.3390/su15043175
APA StylePark, J., Min, J., Song, J.-H., Park, M. Y., Yoo, H., Kwon, O., Yang, M., Kim, S., Lee, J., & Myong, J.-P. (2023). The COVID-19 Pandemic Response and Its Impact on Post-Corona Health Emergency and Disaster Risk Management in Republic of Korea. Sustainability, 15(4), 3175. https://doi.org/10.3390/su15043175






