Abstract
The protracted war in Ukraine, sparked in 2014 and persistently escalating, has significantly impacted the country’s healthcare system. It has amplified existing challenges, such as shortages of medical supplies and personnel, outdated infrastructure, and restricted access to healthcare services. Destruction of medical facilities, non-adherence to prevention and treatment standards, lack of medical personnel and supplies, and logistical disruptions are hampering the provision of timely healthcare to the Ukrainian population. This study employed a rapid review methodology to synthesize available research concerning the healthcare crisis in Ukraine, with an explicit focus on the war’s sustained impact on the healthcare system. Through this review, a series of critical challenges facing Ukraine’s healthcare system were identified. These included the shortage of medical supplies and personnel, insufficient infrastructure, and funding deficits. Additionally, the review brought to light various interventions and strategies aimed at counteracting these challenges. These comprised international aid and support, initiatives enhancing the resilience of the Ukrainian health system, and others. Given the ongoing war, this review highlighted the pressing need for continuous support and investment in the Ukrainian healthcare system. This commitment is essential to guarantee access to quality healthcare for the Ukrainian population during the war and in its aftermath. The findings presented here can serve as a guide for policymakers and healthcare professionals working not only in Ukraine but also in other regions impacted by war. These insights can inform the development and implementation of effective strategies and interventions tailored to such challenging contexts.
1. Introduction
Wars and armed conflicts have wide-ranging and devastating impacts on several aspects of human life. In recent years, the mode of warfare has increasingly targeted civilians [1], leading to the loss of human life, political and socioeconomic disintegration, and destabilization of entire regions [2]. This type of warfare is particularly devastating to vulnerable populations, including women and children, who are disproportionately affected by conflict, with millions of people suffering from starvation, infectious diseases, sexual violence, mental disorders, and forced migration [3,4,5,6].
Armed conflict and subsequent displacement can lead to an increased risk of starvation and malnutrition and a lack of access to basic medical care. Infectious diseases can spread rapidly in overcrowded and unsanitary living conditions, particularly in refugee camps and other temporary settlements. There is also an increasing recognition of the need to consider the gendered impacts of conflict, particularly in terms of reproductive health and gender-based violence. Emerging reports from organizations such as the United Nations highlight the pressing health needs of Ukrainian women and men that may have been overlooked in previous academic research [7].
Sexual violence is another common abuse during the conflict, with women and children being particularly vulnerable to rape and sexual assault [3,4,5,6]. The trauma of such experiences can have long-lasting effects on mental health, including post-traumatic stress disorder (PTSD) and depression [8].
Forced migration, a prominent repercussion of ongoing conflicts such as the one seen in Ukraine, results in the displacement of millions of people from their homes. This compels individuals and families to seek refuge in safer areas. Such displacement often entails the loss of community and social networks, exerting negative impacts on mental health and well-being [8]. Furthermore, it can restrict access to healthcare, education, and employment opportunities, precipitating a cycle of poverty and social exclusion [9].
Since the impact of war and armed conflict on civilians is profound and devastating and the loss of life, displacement, and the resulting physical and mental health consequences have long-lasting effects on individuals, families, and entire communities, it is crucial to address the root causes of conflict and to work towards sustainable peace and stability in affected regions to alleviate the suffering of millions of people [10].
The full-scale invasion of Ukraine exemplifies the major tenets of hybrid warfare. This form of conflict distinctly targets not only civilians but also the crucial infrastructure that sustains them, including energy, healthcare, and finance sectors [2]. Concurrently, a pervasive element of this warfare is the propagation of disinformation and deceptive narratives. These tactics aim to normalize war crimes and obfuscate the true brutality of hybrid warfare [11,12]. Consequently, the current war has caused significant damage to Ukraine’s healthcare system. The destruction of medical infrastructure, the inability to adhere to prevention and treatment standards, the shortage of medical personnel and medicines, and the disruption of logistics prevent timely medical care for the country’s population [13,14]. However, despite extensive destruction and continued indiscriminate shelling, the Ukrainian medical system has survived, reoriented itself, and continues to provide services, although limited, within the Ukrainian-controlled state. The assistance of the international medical community played an important role in its success to date [15,16].
This paper reviews the current status of Ukrainian healthcare amid the ongoing Russian–Ukrainian war, demonstrating the critical impact of public health priorities. It particularly highlights the effects of the Russian invasion on the Ukrainian health system, along with the consequent implications and outcomes on regional and subregional health capacities.
2. Materials and Methods
Considering the critical nature of the current scenario, a rapid review methodology of existing literature was deployed. This technique allows for a fast-paced but intensive exploration of the subject by simplifying or omitting some elements of a traditional systematic review process to meet urgent information requirements [17].
2.1. Search Strategy
An exhaustive online search was independently executed across databases like PubMed, Scopus, and Web of Science. This search combined both MeSH terms and free-text words, using search phrases like ‘Ukraine’, ‘war’, ‘conflict’, ‘healthcare’, ‘health system’, ‘medical services’, ‘humanitarian aid’, and related terms. The focus was on articles published within the duration of the conflict, from 2014 to 2023. The search strategy went through several iterations to ensure a comprehensive coverage of the literature.
2.2. Inclusion and Exclusion Criteria
The scope included original research articles, reviews, reports, and case studies that provided insights into the ramifications of the continuing war on Ukraine’s healthcare system. Exclusions were made for articles not written in English, articles lacking full-text availability, and sources without explicit information concerning the impact of the war on the Ukrainian healthcare system.
2.3. Data Extraction
After elimination of duplicate entries, the titles and abstracts were individually reviewed to judge their relevance. Any discrepancies were settled via discussion and consensus. The chosen articles then underwent a full-text review, and data were extracted, emphasizing study design, objectives, key findings, and conclusions.
2.4. Data Analysis
For data analysis, a thematic content analysis strategy was adopted. This method involves spotting, examining, and reporting patterns (themes) present in the data. These themes were derived inductively, indicating they surfaced from the data and were not pre-defined. Initially, open coding was conducted, where codes were generated by assessing the data line by line. Then, these codes were grouped into potential themes. As the analysis progressed, the codes were constantly compared for similarities and differences, and themes were refined and consolidated. This analysis was carried out manually without the use of any specific software.
2.5. Quality Assessment
Given the expedited nature of this review and the inclusion of varied types of publications, a formal quality appraisal of the sources included was not conducted. Nonetheless, all incorporated sources underwent a critical evaluation to determine their relevance and contribution to the review. This involved considering the reliability and reputability of the source, the rigor and robustness of the study design, and the relevance and applicability of the findings to the Ukrainian context.
As stated, this rapid review methodology permitted a swift synthesis of available evidence to comprehend the effect of the war on Ukraine’s healthcare system and recognize potential strategies to address these challenges [17]. The potential limitations of the rapid review process are discussed later in the text.
3. Results
A total of 25 studies met the inclusion criteria and were incorporated into the review (Figure 1).
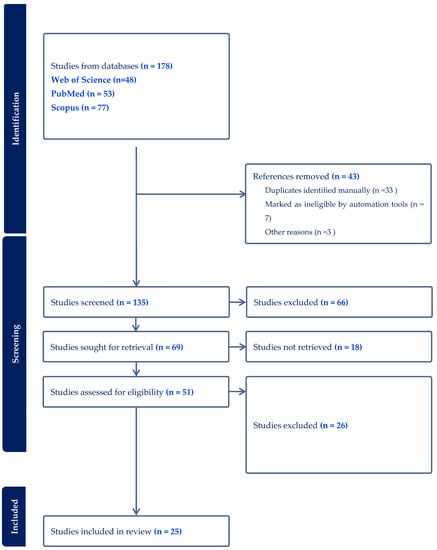
Figure 1.
Flow Diagram of Literature Selection Process [18].
These studies were individually categorized and underwent qualitative evaluation. Upon performing a systematic content analysis, key themes emerged, which are discussed in the sections that follow.
3.1. Medical Facilities and Healthcare Services
The start of the conflict in eastern Ukraine in 2014 wrought havoc on the region’s medical infrastructure. Reports indicate that around 1200 medical facilities were damaged, with more than 160 completely destroyed. The conflict also resulted in more than 400 medical facilities falling into temporarily occupied areas, leading to limited access and reduced operational capabilities [19]. According to World Bank estimates, these damages led to losses exceeding USD 1 billion for the state’s health sector [19]. This substantial financial burden posed serious challenges for Ukraine, already grappling with the direct human cost of the conflict.
Since the onset of the conflict in 2014, the Ministry of Health of Ukraine prioritized the restoration of medical services for the population, particularly emphasizing internally displaced persons and ensuring employment for health professionals. Despite the immense challenges, over 122 medical facilities have fully resumed operation, and an additional 260 have been partially renewed, according to data from the Ministry of Health of Ukraine as of January 2023 [11,20,21].
Efforts have also been undertaken to expand the network of mobile outpatient clinics, a strategy found to be essential especially in the Vinnytsia and Khmelnytskyi regions, which host the largest number of internally displaced persons. However, as of the current date, almost a third (30%) of the population continues to experience difficulties accessing healthcare [22].
The Ukrainian health service also faces significant staff shortages. More than 30,000 medical professionals have either joined the Ukrainian Armed Forces or become volunteers, while over 2500 have left the country and 4500 have been internally displaced [23]. This displacement of healthcare professionals has further exacerbated the staffing crisis in the health sector. A particular concern is the lack of accurate, up-to-date information on the exact number of medical professionals currently working in the country [24,25,26].
However, some progress has been made in addressing this issue. As of January 2023, about 45,000 internally displaced medics have found employment in other medical facilities across the country, including more than 2000 physicians, 1500 mid-level medical professionals (nurses, midwives, paramedics, pharmacy assistants), and approximately 800 technical staff. These healthcare professionals are predominantly found in the Cherkasy, Kharkiv, and Poltava regions [11,27]. Interestingly, in certain parts of Ukraine, such as the Zaporizhia, Poltava, and Dnipropetrovsk regions, physicians who left these areas have been ‘replaced’ by specialists coming from the temporarily occupied areas.
Regrettably, it is currently impossible to fully estimate the losses among civilian medical workers who have died due to shelling and shell explosions [28]. This loss further underscores the grave impact of the war on Ukraine’s healthcare system and its dedicated professionals.
3.2. Humanitarian Support
Due to the systematic destruction of Ukraine’s medical infrastructure and logistical problems, hospitals have been facing shortages of medicines and equipment since the beginning of the Russian invasion [8,22]. According to data from the Ministry of Health of Ukraine, as of January 2023, during the period of martial law (November to December 2022), Ukraine received 10,500 tonnes of medical humanitarian aid worth approximately USD 350 million, consisting of, among other things, medicines, medical devices, especially medical apparatus, both new and used, together with consumables, sanitary transport, medical furniture, mobile hospitals, and power generators. In addition, Ukraine’s foreign partners co-organized approximately 2100 training courses on tactical and emergency medicine and other healthcare issues for Ukrainian medics in 2022 [20,21].
The Ukrainian medical sector also receives direct financial assistance. By 30 January 2023, the Ministry of Health of Ukraine account via the fundraising platform received approximately USD 30 million. More than 9000 pieces of medical and other equipment and means of transport were purchased with the raised funds [20,21].
Additional financial resources have been utilized to bolster other areas of healthcare as well. Notably, a significant portion of these funds went towards investing in mental health resources and support systems to cope with the psychological aftermath of the war. In response to increasing reports of post-traumatic stress disorder and other mental health issues among displaced persons and those living in conflict-affected regions, new initiatives have been launched to expand mental health services. This includes setting up mobile mental health clinics, recruiting and training of additional mental health professionals, and partnering with international agencies to implement evidence-based trauma response programs [20,21].
Furthermore, these funds have also been used to address the concerning rise in reproductive health issues and gender-based violence, as highlighted by several reports from international organizations. Investments have been made in enhancing obstetric and gynecological care facilities, providing access to birth control and safe abortion services, and setting up helplines and safe spaces for survivors of gender-based violence. These services are crucial in addressing the gendered impacts of the war and ensuring the health and safety of women and children in Ukraine [20,21].
Lastly, the financial aid also supported the long-term care needs of individuals with disabilities and those requiring prosthetics due to conflict-related injuries. Realizing the ongoing requirement of these individuals, efforts have been made to provide not just immediate care but also necessary follow-up surgeries, physical rehabilitation services, and periodic replacement of prosthetics and mobility aids [21].
Thus, the financial assistance received has been strategically used to address various healthcare challenges emerging from the conflict, demonstrating the resilience and adaptability of Ukraine’s healthcare system in these testing times.
3.3. Medical Evacuation and Cooperation
According to the International Organization for Migration (IOM), as of 14 June 2022, approximately 7.13 million people have been internally displaced, and there are 7.3 million refugees [8,21]. Another important area of international medical assistance to Ukraine since the beginning of the war has been the organization of medical evacuation and treatment of Ukrainians abroad. Essential life-saving support and necessary evacuation assistance were provided to those who were not able or willing to leave their homes, including those living in care institutions.
As of 14 June 2022, at least 641 patients (78% of the requests) have been evacuated for medical reasons from Poland, the Republic of Moldova, Slovakia, and Ukraine via the EU Civil Protection Mechanism to 13 European countries (Belgium, Denmark, France, Germany, Ireland, Italy, Luxembourg, the Netherlands, Norway, Portugal, Romania, Spain, and Sweden) [11,20,21].
During the war, medical evacuations were carried out for 2354 patients with complicated combined wounds or from mines, burns, or with serious illnesses (including more than 500 children with cancer), whose treatment in Ukraine is now difficult or impossible due to damaged or destroyed medical infrastructure [20,21].
In addition, as part of the collaboration between the Ministry of Health of Ukraine and the West Ukrainian Children’s Specialised Medical Centre from Lviv and the global initiative of St. Jude’s pediatric oncologists, the Ministry of Health of Ukraine will be working with the St. Jude Children’s Specialised Medical Centre.
While there is a focus on the immediate medical needs and evacuations, it is also important to acknowledge the lasting psychological trauma, specifically with regard to the impact on mental health. Programs have been initiated to provide mental health support for evacuees, with a specific emphasis on children and those directly impacted by violence. Collaborations with international mental health organizations and institutions facilitated this process [11,20,21].
Additionally, steps have been taken to facilitate the medical evacuation and treatment of women facing complications in reproductive health due to the crisis. Several women, especially from conflict zones, have been evacuated to safer locations where they can receive necessary obstetric and gynecological care. This is particularly critical in situations where access to such healthcare is hampered in their current location due to the ongoing war [21].
Efforts have also been made to evacuate and provide care for survivors of domestic and sexual violence, a growing concern in conflict zones. This includes setting up secure pathways for evacuation, providing immediate medical care, and establishing support services to assist with the trauma associated with such experiences.
Similarly, special attention has been paid to individuals with disabilities, ensuring their safe evacuation and addressing their specific health needs. This includes persons who have become disabled as a direct result of the war, requiring specialized medical care and support.
According to a survey conducted by the St Jude Children’s Hospital (USA) and the international community of pediatric oncologists, approximately 1000 children with cancer have been evacuated for further treatment at leading cancer centres in the USA, Canada, and the EU, particularly Poland [11,29,30].
3.4. Mental Health Impact of War in Ukraine
The ongoing war in Ukraine has had a significant impact on the mental health of the population, including both civilians and military personnel. One of the mental health effects of war in Ukraine includes post-traumatic stress disorder. The experience of war, including exposure to violence and trauma, can lead to the development of PTSD, a mental health disorder that can cause symptoms such as intrusive thoughts, hyperarousal, and avoidance behavior. The stress and trauma of war can also lead to the development of depression and anxiety, which can be debilitating and make it difficult to function in daily life. Some individuals may turn to drugs or alcohol as a way to cope with the stress and trauma of war. The stress and trauma of war can increase the risk of suicide, particularly among military personnel. The experience of war can disrupt family relationships and lead to increased conflict and tension. Individuals with mental health issues related to the conflict may be stigmatized and experience social isolation [31,32,33,34].
The psychosocial impact of the war has been broad and devastating, affecting individuals of all ages and backgrounds. The elderly population, for example, has had to grapple with the dual burden of war-related stressors and age-related health challenges, exacerbating mental health issues like anxiety and depression [32].
Children and adolescents have been significantly impacted as well, with many experiencing traumatic stress, behavioral changes, and academic difficulties. Schools and community spaces, traditionally regarded as safe environments, have been disrupted or destroyed. This displacement, coupled with exposure to violence and loss, has had severe implications for the mental health and overall development of young people [33].
Many healthcare workers and first responders, constantly exposed to high levels of trauma and stress, also reported feeling overwhelmed and experiencing burnout, which can increase the risk of mental health disorders [34].
The mental health impact of the war in Ukraine has been significant, and addressing the mental health needs of the population will be an important part of the country’s recovery process. It is important to provide access to mental health services and support for those who have been affected by the conflict.
3.5. Other Healthcare Problems in Ukraine
Numerous victims in Ukraine need prosthetics for their upper and lower extremities due to war injuries. The real number of civilians and military staff in need of different types of prosthetics was not officially announced due to government limitations on such information. The Ministry of Health of Ukraine, the Ministry of Social Policy, the Ministry of Veterans, and the Command of the Medical Forces of the Armed Forces of Ukraine are looking for funding opportunities to ensure the provision of prosthetics for patients who lost limbs during the war in Ukraine, and not abroad [35,36].
Addressing the prosthetics needs of victims is a complex process that requires not only the provision of the prosthesis itself but also a comprehensive approach that includes medical rehabilitation and psychosocial support to help individuals adjust to their new circumstances. The availability of such comprehensive care varies across the country, depending largely on available resources and local capacity.
Currently, Ukrainian facilities are working with international partners to supply enough training prostheses to Ukrainian hospitals that provide primary inpatient rehabilitation. This will allow a patient with a leg amputation to stand up and learn to walk as soon as possible with the help of a multidisciplinary rehabilitation team. At the same time, the stump-forming process takes place and the patient, together with the rehabilitation team, determines the type of his primary prosthesis [21].
Unfortunately, even when prosthetics are available, access to them can be challenging. They are often expensive, and not all individuals who need prosthetics can afford them. Also, prosthetics need to be replaced periodically, which increases the overall costs. There is a need for more funding and resources to ensure the accessibility and affordability of prosthetics.
For example, Parashar Industries, a company specializing in prosthetics and rehabilitation, donated 350 functional iGrip prostheses to the military and civilians who suffered from Russian aggression [34]. Leading British manufacturer Open Bionics provided three state-of-the-art bionic prosthetics of the upper limbs called Hero Arms. This was realized by a strategic partnership between Mastercard and Superhumans. The partners also organized training for three Ukrainian prosthetics engineers based on Open Bionics [36].
The partnership and training initiatives mentioned above are crucial steps towards improving the prosthetics sector in Ukraine. Strengthening local capacity by training Ukrainian prosthetists, along with the provision of high-quality prosthetics, can greatly enhance the quality of care for individuals needing prosthetics. However, this effort needs to be sustained and expanded, with more international collaboration and funding, to meet the demand adequately [36].
Another significant healthcare issue is the treatment and management of serious war-related injuries. The nature of these injuries is often complex and severe, involving multiple organ systems and requiring specialized care. Common war-related injuries include gunshot wounds, injuries from explosions, burns, and traumatic amputations. These injuries require immediate and ongoing treatment, often involving surgery, hospitalization, and long-term rehabilitation. However, the damaged healthcare infrastructure in Ukraine made the treatment of these injuries incredibly challenging. Many hospitals have been damaged or destroyed, medical supplies are limited, and many healthcare professionals have either been displaced or are working in extremely difficult conditions. In addition, the long-term implications of these injuries are significant. Many of those injured will require ongoing medical care and rehabilitation, and may face permanent disability. This adds to the already significant burden on the healthcare system and underscores the urgent need for more resources and support.
The war in Ukraine significantly affected the healthcare sector, resulting in substantial damage to medical infrastructure, displacement of medical professionals, and restricted access to necessary healthcare for many civilians. The availability of medical and humanitarian aid, despite being substantial, struggled to address the multitude of emerging needs, one of which is a rising demand for prosthetics due to war injuries.
Medical evacuation and cooperation have become essential tools in managing severe medical cases that can no longer be adequately treated within the country. Mental health implications due to the stress and trauma of the conflict are pervasive and extend to both civilian and military populations. The conflict has also notably impacted the management of chronic illnesses, such as rheumatic diseases. Patients experience relapses triggered by stress and disruption of continuous treatment due to drug shortages. Furthermore, an increase in cases of spondylarthritis among soldiers was noted, which is attributed to the excessive load on the spine during long-term use of heavy body armours.
The response to these various healthcare challenges has been significant but remains inadequate in fully addressing the magnitude of the problems. As such, continuous and enhanced support, both national and international, is crucial for mitigating the health implications of the ongoing war and paving the way towards recovery.
4. Discussion
The healthcare system in Ukraine found itself in a precarious situation as the full-scale war ensued. It was a situation the system was not prepared for, with constant massive shelling, problems with supplies, and shortages of medicines all exacerbating the pre-existing challenges. However, despite the considerable damage to its infrastructure, the Ukrainian healthcare system demonstrated remarkable resilience and adaptability, transforming itself according to its new needs and demands [8].
The ability of the healthcare system to navigate these challenges was greatly facilitated by the rapid humanitarian, financial, and educational assistance it received from Ukraine’s foreign partners and the international medical community [28,34]. This international collaboration extended beyond immediate aid, providing opportunities for specialized treatment and rehabilitation of Ukrainians abroad, which was an essential element in alleviating some of the burdens on the domestic healthcare system [36].
The impact of war on healthcare systems extends beyond immediate trauma care. One such consequence was the increased demand for prosthetics due to war injuries. This urgent need exposed the limited capacity of the government to fully address the repercussions of the conflict and highlighted the importance of international collaboration. Manufacturing companies such as Parashar Industries and Open Bionics played a significant role in mitigating this demand, emphasizing the need for coordination and collaboration in providing essential health services.
The study by Malysh and Grytsyk [37] highlighted the significance of the assistance received from foreign partners and the international medical community in addressing the challenges of the conflict. The authors shed light on the provision of medical equipment, supplies, and expertise, but also importantly on the opportunities that have been created for specialized treatment and rehabilitation of Ukrainians abroad. Their work supports the notion that international humanitarian aid and medical assistance are fundamental in addressing the complex and multifaceted challenges of modern armed conflicts.
Population displacement due to the war led to significant transformations in the demand for medical services. Simultaneously, the capacity of the health system decreased, particularly in areas of active warfare, leading to an imbalance of resources and personnel in the health sector. This highlights the importance of seeking alternative sources of funding for the sector and creating conditions that attract private capital to invest in the reconstruction and development of medical facilities in Ukraine, especially in the areas most affected by the war [38,39].
Furthermore, the war influenced the incidence and management of various diseases. For example, an increase in rheumatic diseases due to stress and disruption of continuity of care and spondylarthritis among soldiers due to the long-term use of heavy body armor were observed. Therefore, it is crucial to devise targeted health initiatives that not only respond to immediate health needs but also prevent the escalation of long-term health issues, contributing to a sustainable health sector in Ukraine.
The ongoing war has had profound impacts on the country’s healthcare system. Before the conflict, the system was already grappling with several challenges such as underfunding and outdated infrastructure. The outbreak of war exacerbated these issues [8]. Despite these adversities, the Ukrainian health system demonstrated resilience, managing to survive and adapt to the new reality of the conflict. However, the constant shelling and damage to infrastructure have made it challenging to provide adequate medical care, with shortages of critical supplies and medicines adding to the burden.
Equally important is the impact of the war on mental health among both civilians and military personnel. The escalation in conditions such as PTSD, depression, and anxiety, combined with the disruption of familial relationships and an increase in social stigmatization and isolation, underscores the pressing need for comprehensive mental health services. Ongoing international support, along with the development of robust local mental health services, are crucial to tackle this challenge [8].
The study by Hou and colleagues [40] provided valuable insights into this reality, sharing the experiences of healthcare professionals who provided medical care in a combat zone during the conflict. Despite facing challenges such as limited resources and high patient volumes, the healthcare professionals interviewed described their commitment to providing care to their patients as unwavering. They saw their work as essential to preserving the health and wellbeing of the civilian population and demonstrated a strong sense of duty to their patients and the entire health system.
The rapid and substantial assistance from foreign partners and the international medical community played a crucial role in helping Ukraine tackle the challenges posed by the war [41,42,43]. This assistance included financial aid, humanitarian aid, and educational support. Borysova and Gubar [41] also noted the humanitarian aspect of this aid, recognizing that it helped alleviate the suffering of civilians affected by the war. Additionally, the international community provided opportunities for Ukrainians to receive specialized medical treatment and rehabilitation abroad, significantly contributing to improved health outcomes for those affected by the conflict [40,42,43].
The large-scale displacement of populations to other areas of the country and beyond had a significant impact on the healthcare system in Ukraine. The demand for medical services shifted, while the health system’s capacity decreased. This led to an imbalance of resources and personnel in the health sector, particularly in areas of active warfare. Bowers and colleagues [44] described the impact of the conflict in Ukraine on the healthcare system, with a focus on the challenges of health system capacity building in the post-conflict period. They noted that the displacement of large populations led to a significant imbalance in resources and personnel in the health sector, especially in areas of active warfare. The authors highlighted the challenges of providing adequate medical care in these regions, given the limited resources and the need to balance the competing demands of military and civilian healthcare. Furthermore, the authors emphasized the role of international aid in addressing these challenges and building the capacity of the health system.
The non-governmental organization Doctors Without Borders also underscored the impact of the war on the healthcare system, including the destruction of medical infrastructure, displacement of populations, and a lack of medical supplies and personnel [45]. They described their efforts to provide medical care in these areas, including the deployment of mobile clinics and mental health services for those affected by the conflict. They emphasized the need for sustained international support and the importance of upholding the neutrality of medical workers and facilities in conflict zones.
To effectively address these multifaceted challenges, it is imperative to seek alternative sources of funding and resources for the healthcare sector. Creating conditions that encourage private capital to invest in the reconstruction and development of medical facilities in Ukraine is one such approach, along with facilitating the use of community resources [41]. Gogolashvili and Morozova [46] suggested that the healthcare system in Ukraine, which has historically been underfunded, could greatly benefit from alternative sources of funding. They proposed private investment and public–private partnerships as potential avenues to address these challenges. The authors also highlighted the importance of improving the efficiency of healthcare spending and implementing health financing reforms. This approach is particularly important for areas most affected by the war, as they require significant resources and attention to rebuild and develop [47,48,49,50,51,52].
Furthermore, it is crucial to critically evaluate the role and impact of international aid in this context. While assistance from foreign partners and the international medical community has been substantial and vital, there is a need to ensure that these resources are effectively and efficiently utilized. This necessitates robust coordination mechanisms, transparency, and accountability. The role of local communities and stakeholders in decision-making and implementation also needs to be emphasized to ensure that the aid and interventions are contextually appropriate and sustainable [39,53,54].
The conflict in Ukraine significantly impacted the healthcare system, exacerbating pre-existing challenges and creating new ones. However, the resilience and adaptability of the healthcare system, along with international support, have been instrumental in navigating these challenges. As the war continues, the need for sustained and coordinated efforts to strengthen the health system remains critical, with a focus on alternative funding sources, infrastructure development, and capacity building.
5. Limitations
The limitations of this study primarily originate from the nature of the rapid review process, which mandates a trade-off between thoroughness and timeliness. The expedited review process may inadvertently miss some relevant studies due to time constraints, thereby potentially affecting the overall quality, breadth, and depth of the review. Consequently, the rigor of the “Identify” and “Evaluate” stages might be compromised.
Furthermore, there is potential bias in the selection of studies for review due to our research question and the scope of the review that produced a finite pool of pertinent studies. This limitation may impact the comprehensiveness and generalizability of our findings, potentially yielding an incomplete representation of the current research landscape on this topic.
Another limitation was that the rapid review methodology employed, while appropriate for the research question, may not offer the same depth and granularity found in more exhaustive systematic review methodologies. The swift pace of the review process inherently impacts the depth of data extraction and the extent of data synthesis, which might limit the understanding of complex phenomena.
Notably, the absence of a detailed quality analysis of the included studies was a limitation, as it prevented us from assessing the level of evidence and the risk of bias in individual studies. This lack of assessment could influence the interpretation and applicability of our findings.
Lastly, while data collection was extensive, the use of only open source, non-confidential data might not fully capture the extent of the healthcare crisis in Ukraine, as some critical information may be undisclosed due to governmental restrictions or security concerns. This limitation might lead to an underestimation of the real impact of the war on healthcare in Ukraine.
Future research could benefit from implementing more nuanced search strategies, utilizing advanced search techniques, and engaging a team of reviewers with diverse expertise to mitigate these limitations. A thorough quality assessment of the included studies is also recommended to enhance the validity and reliability of the review findings.
Despite these limitations, the rapid review methodology offers a timely synthesis of available evidence, providing valuable insights into the effects of the war in Ukraine on its healthcare system.
6. Conclusions and Recommendations
The escalating war in Ukraine and its far-reaching implications on the nation’s healthcare system underscore the indispensable role of sustained international support. This backing is vital not only in terms of financial aid but also humanitarian and emergency medical assistance. It is essential to accurately document and report war-related morbidity and mortality. This information will help strategize responses to both immediate and long-term health consequences of the war and serve as a powerful deterrent to further acts of aggression.
The challenges confronting Ukraine’s healthcare system are manifold and complex. Amid the ongoing war, particularly in the eastern region of the country, these challenges have unearthed unique hurdles. Understanding these hurdles can guide multi-agency assessments and inform strategies for managing similar crises in the future. In light of these challenges, the following potential solutions are proposed:
- The destruction of healthcare infrastructure, often resulting from intentional attacks, severely hampers medical care delivery. Mitigation strategies should include incorporating potential care facilities into all contingency plans.
- The disruption of supply chains, a common fallout of modern warfare, leads to shortages of crucial medical supplies and equipment. Governments and aid organizations should collaborate to establish alternative supply chains and distribution channels.
- Armed conflicts often cause healthcare workers to flee, resulting in professional shortages in affected areas. Flexible community education programs could impart knowledge of first-aid management to civilians, and supportive measures should be implemented to train and deploy new healthcare workers.
- The mental health toll on populations affected by conflicts necessitates a greater emphasis on mental health services. Investments should be made in mental health programs, such as professional training, mental health clinics and hotlines, and improved access to medications and treatments.
- Overcrowding and inadequate sanitation often trigger infectious disease outbreaks. Measures such as improving sanitation and hygiene, providing clean water, implementing vaccination programs, and establishing disease-surveillance and -response systems should be adopted.
- Stress and disrupted treatment due to drug shortages can exacerbate chronic diseases. Healthcare providers should prioritize early identification and treatment of these conditions and provide continuous treatment with alternative drugs when necessary.
- The provision of prosthetics for limb injuries during conflict can be facilitated through dedicated funding and resources for the development and distribution of prosthetic devices.
- To ensure access to healthcare services for vulnerable populations during and after a conflict, outreach programs, mobile clinics, and transportation assistance should be established, accompanied by policies for accessible healthcare facilities.
Furthermore, in light of our findings highlighting several pressing health issues, we propose the following additional recommendations:
- On Sexual and Reproductive Health: Enhanced programs focusing on sexual and reproductive health education, access to contraceptives, and safe maternity services should be prioritized. It is crucial to ensure that sexual and reproductive health services are integrated into the broader healthcare response to the conflict, given the significant impact conflict has on these areas.
- On Working with Victims of Conflict-Related Sexual Violence: Establishment of comprehensive and sensitive care pathways for victims of conflict-related sexual violence is of utmost importance. This involves not only immediate medical care but also long-term psychological support and social rehabilitation. The healthcare workforce should be provided with specialized training to appropriately and empathetically handle these cases.
- On Domestic Violence: The escalating instances of domestic violence amidst conflict situations demand urgent attention. Initiatives should include increasing awareness about domestic violence, implementing safe reporting mechanisms, and integrating domestic violence interventions into broader healthcare and social services. Providing support and protection for victims, alongside legal measures to address the issue, is vital.
These challenges, while significant, offer a roadmap for a concerted and collaborative approach towards rebuilding Ukraine’s healthcare system. Addressing these obstacles and implementing proposed recommendations demand robust partnerships, financial support, and flexible contingency plans. Success is contingent upon the collective efforts of governments and local and international aid organizations working together to pool resources for the reconstruction of the entire infrastructure, including the healthcare system. This collaborative and systematic approach can provide a pathway to alleviate the health crises triggered by the ongoing war and improve the resilience of Ukraine’s healthcare system against future adversities.
Author Contributions
K.G. provided the main framework, identified primary materials, and collaborated on the writing of the paper; A.K.-M. organized research materials, identified appropriate references, and collaborated on the writing of the paper. The rest of the authors collaborated on the writing and editing of the paper. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- United Nations. Report of the Secretary-General on the Work of the Organization, Supplement No. 1 (A/77/1). 2022. Available online: https://www.un.org/sexualviolenceinconflict/wp-content/uploads/2022/09/report/auto-draft/SG-Annual-Report-on-the-work-of-the-Organization.pdf (accessed on 14 July 2023).
- Khorram-Manesh, A.; Burkle, F.M., Jr. Civilian Population Victimization: A Systematic Review Comparing Humanitarian and Health Outcomes in Conventional and Hybrid Warfare. Disaster Med. Public Health Prep. 2022, 17, e192. [Google Scholar] [CrossRef] [PubMed]
- Khorram-Manesh, A. The Impacts of Armed Conflicts and Civilian Uprisings on Children’s Health. Children 2022, 9, 1913. [Google Scholar] [CrossRef]
- Khorram-Manesh, A.; Burkle, F.M.; Goniewicz, K.; Robinson, Y. Estimating the Number of Civilian Casualties in Modern Armed Conflicts-A Systematic Review. Front. Public Health 2021, 9, 765261. [Google Scholar] [CrossRef]
- Murthy, R.S.; Lakshminarayana, R. Mental health consequences of war: A brief review of research findings. World Psychiatry 2006, 5, 25–30. [Google Scholar] [PubMed]
- Goniewicz, K.; Burkle, F.M.; Horne, S.; Borowska-Stefańska, M.; Wiśniewski, S.; Khorram-Manesh, A. The Influence of War and Conflict on Infectious Disease: A Rapid Review of Historical Lessons We Have Yet to Learn. Sustainability 2021, 13, 10783. [Google Scholar] [CrossRef]
- Rapid Gender Analysis of Ukraine. Available online: https://www.unwomen.org/sites/default/files/2022-05/Rapid-Gender-Analysis-of-Ukraine-en.pdf (accessed on 14 July 2023).
- Dzhus, M.; Golovach, I. Impact of Ukrainian-Russian war on healthcare and humanitarian crisis. Disaster Med. Public Health Prep. 2022, 17, e340. [Google Scholar] [CrossRef] [PubMed]
- Shkodina, A.D.; Chopra, H.; Singh, I.; Ahmad, S.; Boiko, D.I. Healthcare system amidst the war in Ukraine. Ann. Med. Surg. 2022, 80, 104271. [Google Scholar]
- Kashdan, T.B.; Morina, N.; Priebe, S. Post-traumatic stress disorder, social anxiety disorder, and depression in survivors of the Kosovo War: Experiential avoidance as a contributor to distress and quality of life. J. Anxiety Disord. 2009, 23, 185–196. [Google Scholar]
- Bazhenova, H. System Opieki Zdrowotnej Ukrainy w Warunkach Wojny. Komentarze IES nr 754 (2/2023). The Central Europe Institute. Available online: https://ies.lublin.pl/komentarze/system-opieki-zdrowotnej-ukrainy-w-warunkach-wojny/ (accessed on 8 February 2023).
- Patel, S.S.; Erickson, T.B. The new humanitarian crisis in Ukraine: Coping with the public health impact of hybrid warfare, mass migration, and mental health trauma. Disaster Med. Public Health Prep. 2022, 16, 2231–2232. [Google Scholar]
- Burnett, A.; Peel, M. Asylum seekers and refugees in Britain: Health needs of asylum seekers and refugees. BMJ Br. Med. J. 2001, 322, 544. [Google Scholar]
- Plümper, T.; Neumayer, E. The unequal burden of war: The effect of armed conflict on the gender gap in life expectancy. Int. Organ. 2006, 60, 723–754. [Google Scholar]
- Watling, J.; Danylyuk, O.V.; Reynolds, N. Preliminary Lessons from Russia’s Unconventional Operations During the Russo-Ukrainian War, February 2022–February 2023; Royal United Services Institute: London, UK, 2023. [Google Scholar]
- Leasure, D.R.; Kashyap, R.; Rampazzo, F.; Elbers, B.; Dooley, C.; Weber, I.; Fatehkia, M.; Verhagen, M.D.; Frey, A.; Yan, J.; et al. Ukraine Crisis: Monitoring Population Displacement through Social Media Activity; University of Oxford: Oxford, UK, 2022. [Google Scholar]
- Ganann, R.; Ciliska, D.; Thomas, H. Expediting systematic reviews: Methods and implications of rapid reviews. Implement Sci. 2010, 5, 56. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar]
- Ukraine Rapid Damage and Needs Assessment, August 2022 World Bank. 2019. Available online: https://openknowledge.worldbank.org/handle/10986/37988 (accessed on 2 July 2023).
- Emergency in Ukraine: External Situation Reports #15, Published 16 June 2022: Reporting Period: 2–15 June 2022. Available online: https://www.who.int/publications/i/item/WHO-EURO-2022-5152-44915-65074 (accessed on 2 July 2023).
- Khorram-Manesh, A.; Goniewicz, K.; Burkle, F.M. Social and Healthcare Impacts of the Russian-Led Hybrid War in Ukraine—A Conflict With Unique Global Consequences. Disaster Med. Public Health Prep. 2023, 17, e432. [Google Scholar] [CrossRef]
- Haque, U.; Naeem, A.; Wang, S.; Espinoza, J.; Holovanova, I.; Gutor, T.; Bazyka, D.; Galindo, R.; Sharma, S.; Kaidashev, I.P.; et al. The human toll and humanitarian crisis of the Russia-Ukraine war: The first 162 days. BMJ Glob. Health 2022, 7, e009550. [Google Scholar]
- Tsagkaris, C.; Ozturk, N.; Matiashova, L. Missile attacks in Ukraine are torpedoing global health. QJM Int. J. Med. 2022, 116, hcac269. [Google Scholar] [CrossRef]
- Jargin, S.V. The Conflict in Ukraine: Medical and Psychological Aspects. Curr. Res. Med. Sci. 2023, 2, 26–36. [Google Scholar]
- Tin, D.; Barten, D.G.; Granholm, F.; Kovtonyuk, P.; Burkle, F.M.; Ciottone, G.R. Hybrid warfare and counter-terrorism medicine. Eur. J. Trauma Emerg. Surg. 2023, 49, 589–593. [Google Scholar]
- Fontanarosa, P.B.; Flanagin, A.; Golub, R.M. Catastrophic health consequences of the war in Ukraine. JAMA 2022, 327, 1549–1550. [Google Scholar] [CrossRef]
- Novakivskyy, V.; Shurduk, R.; Grin, I.; Tkachenko, T.; Pavlenko, N.; Hrynevych, A.; Hymes, J.L.; Maddux, F.W.; Stuard, S. War in Ukraine and dialysis treatment: Human suffering and organizational challenges. Clin. Kidney J. 2023, 16, 676–683. [Google Scholar]
- Rubin, R. Physicians in Ukraine: Caring for patients in the middle of a war. JAMA 2022, 327, 1318–1320. [Google Scholar]
- Khanyk, N.; Hromovyk, B.; Levytska, O.; Agh, T.; Wettermark, B.; Kardas, P. The impact of the war on the maintenance of long-term therapies in Ukraine. Front. Pharmacol. 2022, 13, 1024046. [Google Scholar]
- Uğurluer, G.; Özyar, E.; Corapcioglu, F.; Miller, R.C. Psychosocial impact of the war in Ukraine on pediatric cancer patients and their families receiving oncological care outside their country at the onset of hostilities. Adv. Radiat. Oncol. 2022, 7, 100957. [Google Scholar]
- Bryant, R.A.; Schnurr, P.P.; Pedlar, D. Addressing the mental health needs of civilian combatants in Ukraine. Lancet Psychiatry 2022, 9, 346–347. [Google Scholar] [CrossRef]
- Haydabrus, A.; Santana-Santana, M.; Lazarenko, Y.; Giménez-Llort, L. Current War in Ukraine: Lessons from the Impact of War on Combatants’ Mental Health during the Last Decade. Int. J. Environ. Res. Public Health 2022, 19, 10536. [Google Scholar]
- Osokina, O.; Silwal, S.; Bohdanova, T.; Hodes, M.; Sourander, A.; Skokauskas, N. Impact of the Russian invasion on the mental health of adolescents in Ukraine. J. Am. Acad. Child Adolesc. Psychiatry 2022, 62, 335–343. [Google Scholar]
- Bouchard, J.P.; Stiegler, N.; Padmanabhanunni, A.; Pretorius, T.B. Psychotraumatology of the war in Ukraine: The question of the psychological care of victims who are refugees or who remain in Ukraine. In Annales Médico-Psychologiques, Revue Psychiatrique; Elsevier Masson: Amsterdam, The Netherlands, 2023; Volume 181, pp. 12–15. [Google Scholar]
- Ministry of Social Policy of Ukraine. Available online: https://www.msp.gov.ua/content/zabezpechennya-tehnichnimi-ta-inshimi-zasobami-reabilitacii-specavtotransportom.html (accessed on 11 June 2023).
- Ministry of Health of Ukraine. Available online: https://moz.gov.ua/article/news/dvom-ukrainskim-zahisnikam-vstanovljat-suchasni-bionichni-protezi-ruk-hero-arms (accessed on 20 June 2023).
- Malysh, O.; Grytsyk, Y. International humanitarian aid and medical assistance in armed conflicts. Ann. Acad. Med. Ukr. 2020, 20, 292–298. [Google Scholar]
- Chumachenko, D.; Meniailov, I.; Bazilevych, K.; Chumachenko, T.; Yakovlev, S. On intelligent agent-based simulation of COVID-19 epidemic process in Ukraine. Procedia Comput. Sci. 2022, 198, 706–711. [Google Scholar]
- Khorram-Manesh, A. Flexible surge capacity—Public health, public education, and disaster management. Health Promot. Perspect. 2020, 10, 175–179. [Google Scholar] [CrossRef]
- Hou, X.Y.; Regenbogen, S.E.; Chen, C.; Lee, J.S. Medical care in a wartime setting: A qualitative study. J. Surg. Res. 2019, 244, 169–174. [Google Scholar]
- Borysova, T.; Gubar, O. International medical aid in the conflict zone in Ukraine: A humanitarian aspect. J. Int. Med. Res. 2018, 46, 4435–4443. [Google Scholar]
- Ministry of Foreign Affairs of Ukraine. Ukraine’s Cooperation with the United Nations. 2021. Available online: https://mfa.gov.ua/ (accessed on 17 May 2023).
- European Union External Action Service. EU-Ukraine Relations. 2021. Available online: https://eeas.europa.eu/ (accessed on 16 April 2023).
- Bowers, L.; Mamchur, Y.; Zdanevych, L. Health system capacity building in post-conflict states: Ukraine as a case study. Glob. Health 2017, 13, 44. [Google Scholar]
- Doctors without Borders. Ukraine: Medical Care Severely Disrupted in War-Torn Areas. Available online: https://www.doctorswithoutborders.org/latest/ukraine-medical-care-severely-disrupted-war-torn-areas (accessed on 1 July 2023).
- Gogolashvili, K.; Morozova, O. Financing the Health Care System in Ukraine: Challenges and Opportunities. J. Public Budg. Account. Financ. Manag. 2019, 31, 214–241. [Google Scholar]
- Geneva Call Strategy. Protecting Civilians in Armed Conflict through Humanitarian Engagement with Armed Non-State Actors. Available online: https://genevacall.org/wp-content/uploads/dlm_uploads/2014/06/GC-2014-2016-strategy.pdf (accessed on 19 May 2023).
- Collier, P.; Hoeffler, A. Greed and Grievance in Civil War. Oxf. Econ. Pap. 2004, 56, 563–595. [Google Scholar] [CrossRef]
- Spiegel, P.; Checchi, F.; Colombo, S.; Paik, E. Health-care needs of people affected by conflict: Future trends and changing frameworks. Lancet 2010, 375, 341–345. [Google Scholar]
- Kalt, A.; Hossain, M.; Kiss, L.; Zimmerman, C. Asylum seekers, violence and health: A systematic review of research in high-income host countries. Am. J. Public Health 2013, 103, e30–e42. [Google Scholar]
- Patel, P.; Roberts, B.; Guy, S.; Lee-Jones, L.; Conteh, L. Tracking official development assistance for reproductive health in conflict-affected countries. PLoS Med. 2009, 6, e1000090. [Google Scholar]
- Hynes, M.; Sheik, M.; Wilson, C.; Spiegel, P. Reproductive health indicators and outcomes among refugee and internally displaced persons in postemergency phase camps. J. Am. Med. Assoc. 2002, 288, 595–603. [Google Scholar]
- Phattharapornjaroen, P.; Carlström, E.; Khorram-Manesh, A. Developing a conceptual framework for flexible surge capacity based on complexity and collaborative theoretical frameworks. Public Health 2022, 208, 46–51. [Google Scholar] [CrossRef]
- Goniewicz, K.; Carlström, E.; Hertelendy, A.J.; Burkle, F.M.; Goniewicz, M.; Lasota, D.; Richmond, J.G.; Khorram-Manesh, A. Integrated Healthcare and the Dilemma of Public Health Emergencies. Sustainability 2021, 13, 4517. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).