Abstract
Worldwide, the growing digitalization process and increase in smartphone usage have contributed to promoting mobile health (mHealth) services. This study provides an overview of the research targeting the effectiveness of mHealth interventions among children and adolescents in the school environment. A systematic literature review was performed following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) in the PubMed, Web of Science, and Scopus databases. The results show that physical activity and nutrition are the main intervention topics. Health literacy, mental health, productive health, vaccination rates, and social interaction were also considered in mHealth interventions. Of the 13 studies that remained for analysis, 12 described positive outcomes in at least one health variable after using an mHealth tool. Overall, interventions ranged between four and 24 weeks. Only seven studies managed to have at least 80% of the participants from the baseline until completion. Adding personal information, user interaction, and self-reference comparisons of performance seems crucial for designing successful health digital tools for school-aged children and adolescents.
1. Introduction
The growing digitalization process in health care and the increase in smartphone usage have contributed to the development of digital health [1]. Digital health is described as the integration of technologies into healthcare [2], which comprises mobile health (mHealth) services [1]. This includes simple apps and complex technologies designed for patient monitoring and education, improving access to health care services and treatment adherence, and chronic disease management [3,4]. Overall, mHealth has evolved over the past decade with regard to the capacity and usability of mobile devices employed, addressed health conditions, and its overall purpose [5]. However, most of the solutions available are conceived for adult usage [5,6,7], and details are lacking on the use and effectiveness of these solutions among youth populations. Moreover, in the overall existing models, there is still the need to adapt digital solutions to different areas considering specific contexts and to narrow the gap between health authorities, users, and mHealth developers [8].
Integrating digital technologies into daily living environments such as schools and healthcare facilities has attracted empirical research [9,10,11]. Interventions based on promoting healthy lifestyles, such as diet advice and monitoring physical activity (PA) levels, have been continuously growing. Although behavior change is frequently mentioned, the literature has described the need for an adequate description of the interventions and an integration of behavior change techniques as a critical aspect of effective mHealth interventions [12].
According to the literature, addressing children’s and adolescents’ health literacy is crucial for sustainable development and healthy lifestyle promotion throughout life [13,14]. Children and adolescents spend more time in schools than in any other place except at home [15]. Therefore, schools are a vast platform for enhancing health literacy among pupils and educators [16,17]. Despite the potential of apps for pediatric health change behavior, this is still a largely unexplored topic. Previous research on mHealth services has focused chiefly on privileged adults or the general population, particularly regarding PA self-monitoring and goal setting [18,19,20]. Thus, the novel aim of this review was to provide an overview of the research targeting the effectiveness of mHealth interventions among children and adolescents in the school environment.
2. Materials and Methods
2.1. Study Design
The current systematic review was undertaken following the Preferred Items for Systematic Reviews and Meta-Analyses (PRISMA) statement on the transparent reporting of systematic reviews [21]. The study protocol was registered with PROSPERO (CRD42022349149).
2.2. Search Strategy
In May 2022, the lead author systematically reviewed three electronic databases (PubMed, Web of Science, and Scopus) to find articles that investigated digital health promotion in the school environment among children and adolescents. Primary source articles published in peer-reviewed scientific journals in the past 10 years and up to 31 May were considered eligible. The search terms used for this review were constructed using the PICOS framework: (1) population were children and adolescents of both genders, aged between 12 to 19 years old, (2) interventions that used digital platforms to monitor any type of health condition or to promote health in schools, (3) any type of comparison pre- and post-intervention, (4) healthy lifestyles outcomes, (5) observational and experimental studies, and (6) articles written in English, Spanish or Portuguese. The terms presented in Table 1 were searched in the title/abstract level, in the three databases selected, and combined with the Boolean operators “OR” and “AND”.

Table 1.
Search terms and keywords used in the search strategy.
2.3. Screening Strategy and Study Selection
All returning studies were aggregated and exported into a reference manager (EndNote X20, Thomson Reuters, Philadelphia, PA, USA) for additional assessment once the search was completed. After deleting duplicate entries from the database search, three authors independently reviewed the title and abstract for eligibility (CF, FS, FM). The same authors read all eligible records before determining what studies should be included, and the inclusion and exclusion decisions were made by consensus.
2.4. Data Extraction and Harmonization
Data extraction and harmonization were carried out by three authors (CF, FS, FM) using a standardized approach with a consensus including six items: (1) general information (authors name and year of study publication), (2) sample characteristics, (3) study purpose, (4) procedures, (5) measures and instruments, and (6) results.
2.5. Study Quality and Risk of Bias
The Effective Public Health Practice Project (EPHPP) was used to assess study quality [22]. The six elements of this instrument that examine selection bias include study design, confounding variables, data collecting methods/instruments, whether the evaluators and participants were “blinded,” reports of withdrawals, and dropouts. Based on the predetermined criteria, each category was given a poor, moderate, or high score (Table 2). Three authors performed this process separately (CF, FS, FM). The differences were discussed and resolved by consensus.

Table 2.
Studies methodological quality assessment using the EPHPP.
3. Results
3.1. Study Selection
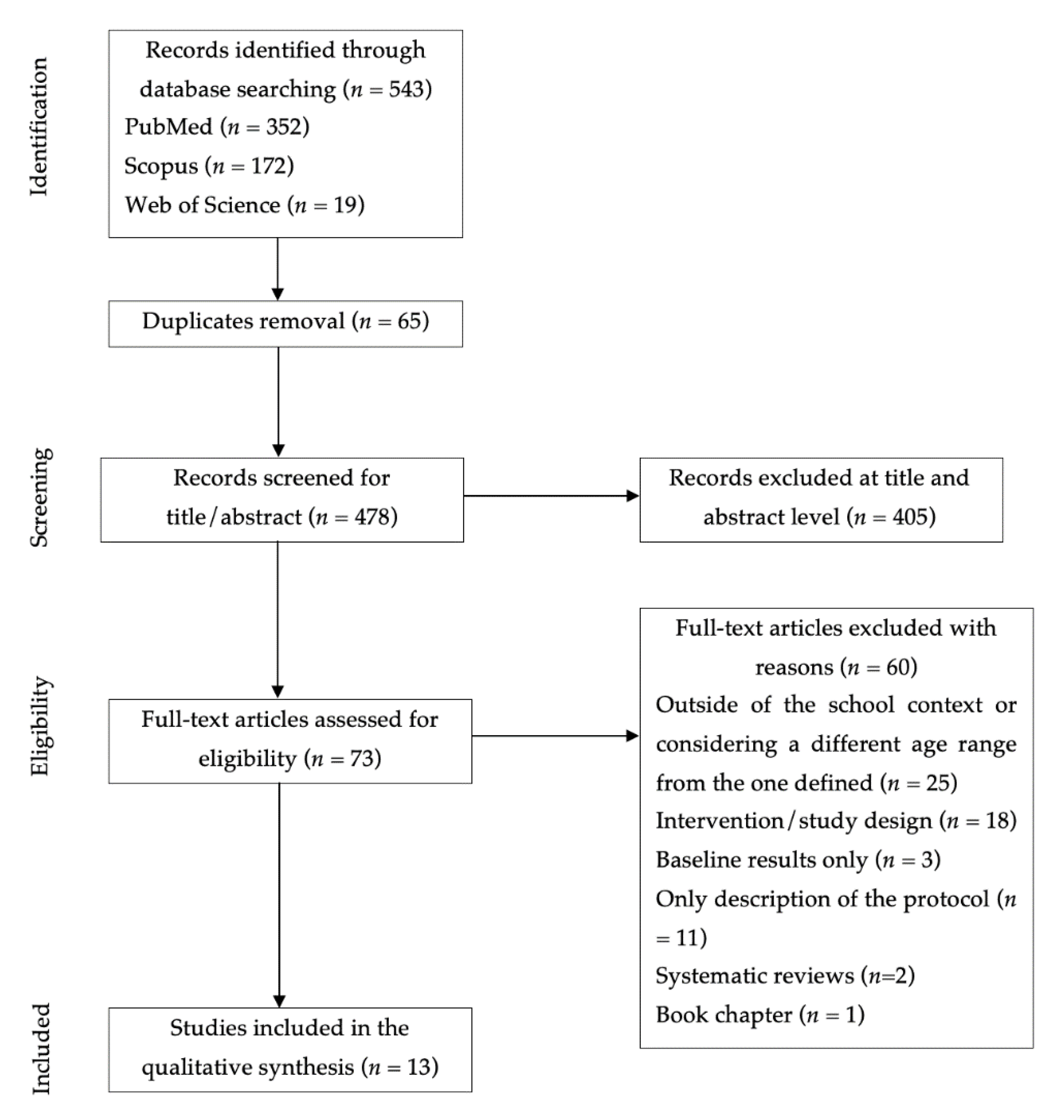
Figure 1 shows the flowchart of the study selection procedure. A total of 543 articles were identified through the search carried out in the aforementioned databases. Of those, 65 articles were duplicates, and 478 remained for eligibility after their removal. In the next step, the title and abstract screening phase, 405 articles were eliminated. Finally, 73 articles were fully assessed, and 13 were chosen as pertinent for inclusion.
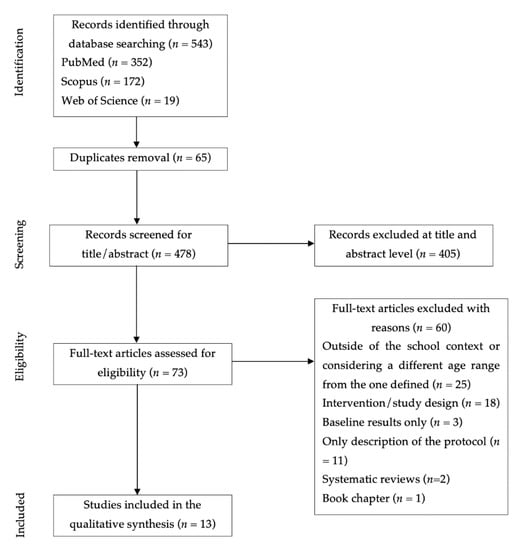
Figure 1.
Flowchart of the study selection process.
3.2. Study Quality and Risk of Bias
The study quality assessment is presented in Table 2. Concerning methodological quality, none of the articles included was classified as strong, five obtained moderate classification [23,25,27,29,30], and eight were poor quality [24,26,31,32,33,34,35]. Considering the instruments categories, it was verified that: (1) only one study was classified as strong in the selection of bias parameter [23], since the rate of participants exceed the 80%, which may be representative of the target population; (2) the randomized controlled trials or controlled clinical trials were classified as strong study design (n = 5) [27,29,33,34,35], while other type of design was classified as moderate (n = 8) [23,24,25,26,28,30,31,32]; (3) seven studies revealed no baseline differences between groups in the confounders’ section or accounted for at least 80% of significant confounders [24,25,27,29,30,33,35], whereas the studies performed with only one group were not evaluated at this point (n = 5) [23,26,28,31,32]; (4) only one study blinded the assessors and participants, being classified as strong [27]; (5) all studies presented valid and reliable data collection instruments; and (6) in the withdrawals and dropouts parameter, studies were classified as strong if the dropout rate did not overcome 20% of the participants (n = 7) [23,24,25,26,28,30,31], as moderate if the dropout rate was between 60 and 79% (n = 1) [29], and as week of the dropout rate was greater than 60% (n = 4) [27,33,34,35].
3.3. Intervention Characteristics
The characteristics of each study included in our review are summarized in Table 3. The interventions involved a total of 2757 students. The students’ age ranged from 9 to 18 years. Six studies included participants over 15 years [23,25,27,31,32,34,35], and five studies included children below 13 years [24,26,28,29,30,35]. One investigation has also included a sample of 23 teachers [33].

Table 3.
Summary of the study description and variables considered.
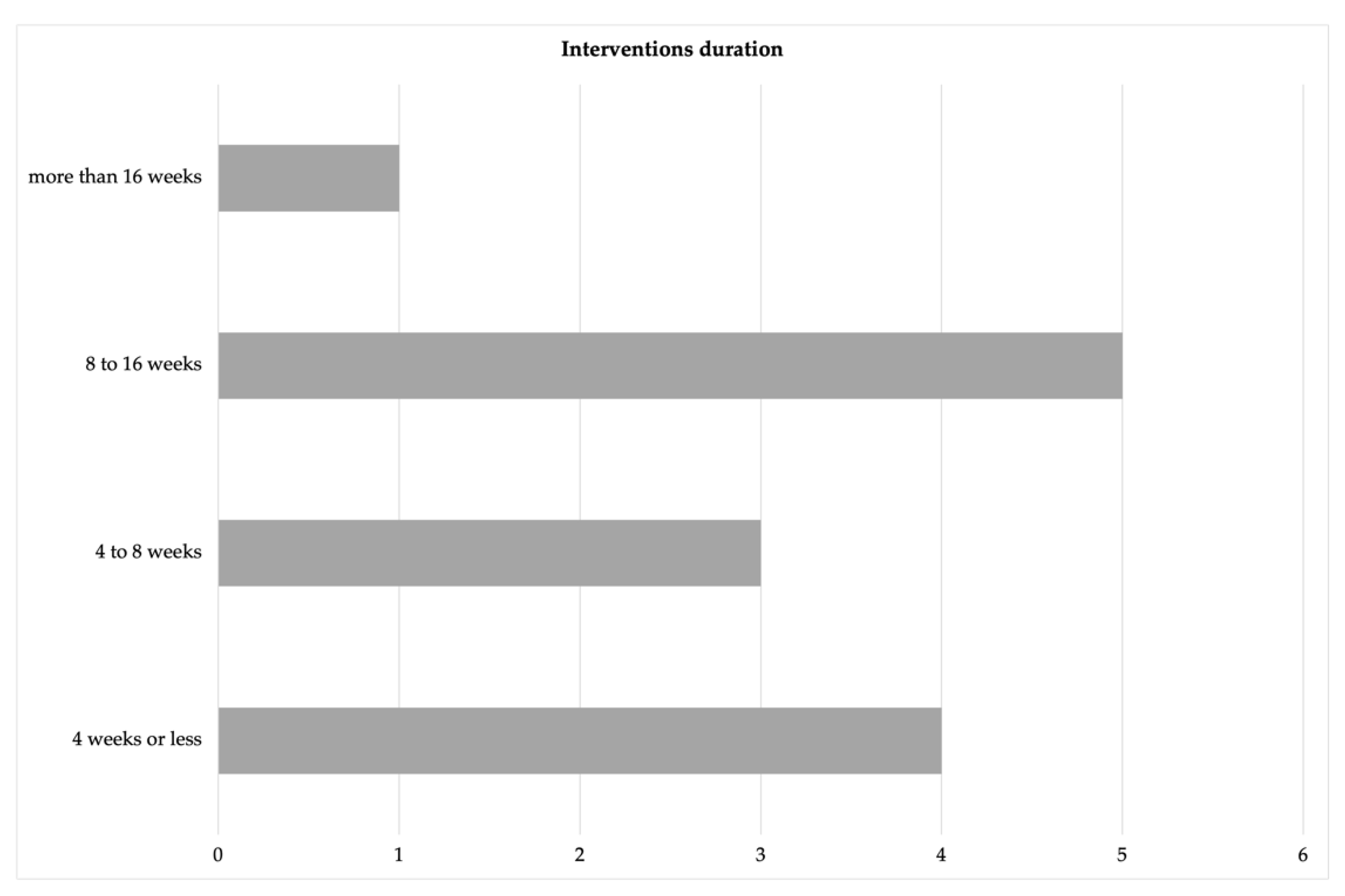
The study’s duration is displayed in Figure 2. Four studies evaluated a digital tool for four weeks or less [25,26,28,32], three studies lasted between four and eight weeks [23,27,30], while the majority varied from eight to 16 weeks [24,29,31,33,34]. The longest intervention was performed for 24 weeks [35].
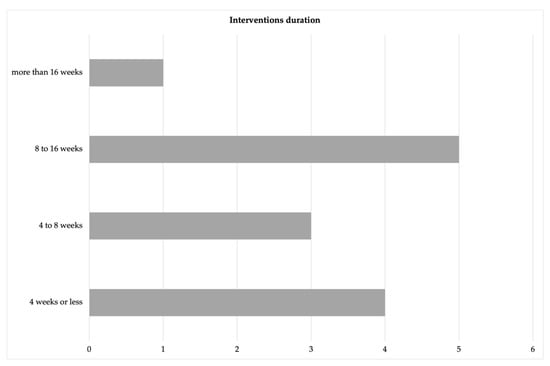
Figure 2.
Summary of the results regarding intervention duration.
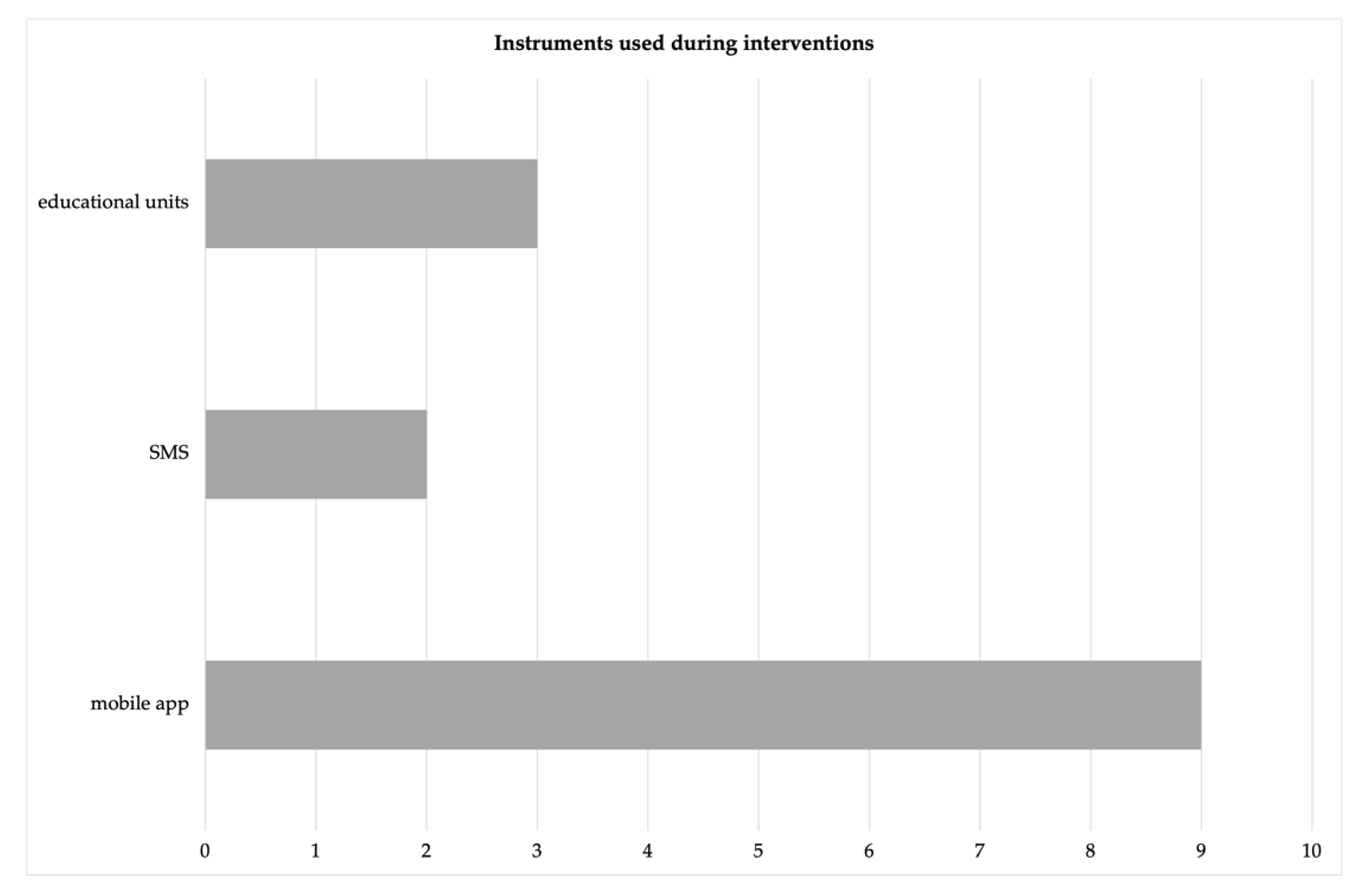
The instruments used during interventions are presented in Figure 3. Most interventions were performed through a mobile app [24,26,27,28,31,32,33,34,35]. Two programs used short message services (SMS) [23,29], and another three primarily relied on educational units during school time [25,29,30].
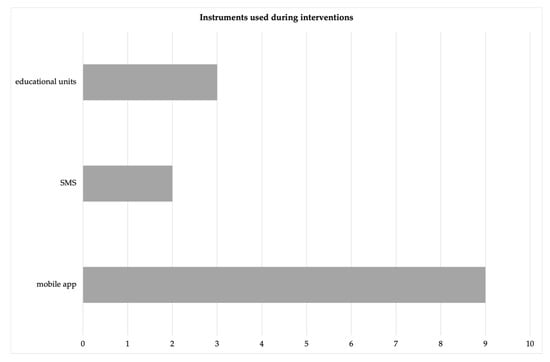
Figure 3.
Summary of the mHealth instruments used in interventions.
3.4. Main Results
Table 3 shows the study description and the variables considered.
The post-intervention assessment dropped significantly (IG = 53 and CG = 151 students). Although the considerable dropout rate, mHealth intervention (TeenPower) significantly affects nutrition, positive life perspective, and global lifestyle outcomes.
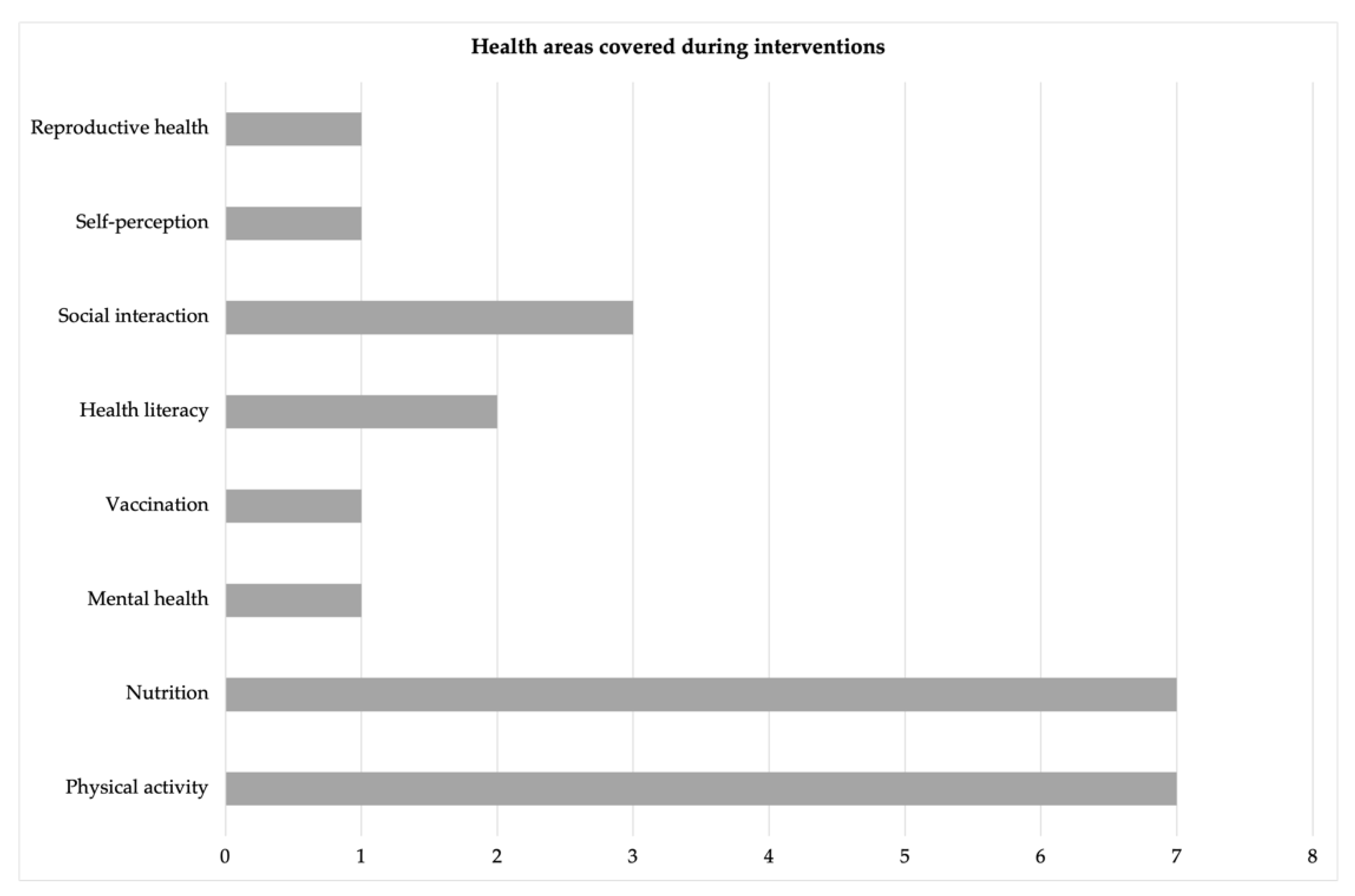
Different health areas were covered (Figure 4), particularly PA and nutrition [24,26,27,28,29,30,31,34]. Besides, mental health [27], reproductive health [23], vaccination [23], social interaction [29,30,33], overall health literacy [30,35], and self-perception [32], were topics covered in the articles retained for analysis.
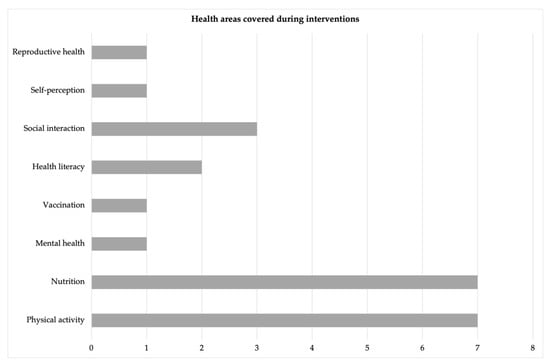
Figure 4.
Summary of the health areas covered in the studies analyzed.
Regarding PA, the positive effects of mHealth were reported in four studies [27,28,29,30], while one investigation did not describe a positive impact of a gamified approach on increasing adolescents’ PA levels [34]. Regarding nutrition, six interventions pointed out positive outcomes [24,26,27,28,30,31]. One of the previous studies combined PA and nutrition interventions, reporting positive outcomes in nutrition but not in PA levels [24].
On the other hand, five studies reported a positive impact of mHealth interventions focused on social interaction, mental health, and self-perception [27,29,30,32,33]. Another four studies described mHealth usage as beneficial to improve reproductive health, vaccination rates, and overall health literacy [23,25,30,35]. Besides students, one study also involved teachers in evaluating how social comparison drives preadolescents’ engagement with an mHealth app, concluding that the involvement of a role model (e.g., a teacher) can influence the average number of activities that preadolescents perform in an intergroup setting [33].
4. Discussion
This study aimed to perform a systematic review of the literature targeting the effectiveness of mHealth interventions among children and adolescents in the school environment. Overall, interventions targeted students’ PA levels, nutrition, and general health components. Of the 13 studies that remained for analysis, 12 described positive outcomes in at least one of the previous components mentioned after using an mHealth tool [23,24,25,26,27,28,29,30,31,32,33,35]. In contrast, one intervention did not successfully increase PA in high school students aged between 16 and 18 years [34].
PA was the focus of most interventions, although most combined it with nutrition [24,26,27,28]. Indeed, overweight and obesity prevalence rates among children and adolescents are an alarming and increasing problem [36], which could be changed by avoiding sedentary behavior and promoting a healthy diet. Most of the interventions focused on this topic were promoted through apps targeting PA-related skills, gamified health-related situations, and nutritional guidelines [24,27,28]. Positive outcomes were reported regarding the number of steps per day [28], time spent in daily PA [27], and BMI assessment [24]. In a study conducted for six weeks among adolescents aged 15.6 ± 0.3 years, the daily reported PA levels increased nearly 20% in the IG, dropping by 26% in the CG. However, a significant decrease was observed in average exercises performed between the first week and the subsequent intervention [27]. Another four-week investigation concluded an improvement of nearly 27% in PA behaviors over the program, particularly for adolescents who were least active at the baseline. Interestingly, these adolescents more often met the international recommendations for daily steps and PA intensity by the end of the program than their more active peers [28].
On the contrary, in a sample of adolescents aged 16 to 18 years, a 12-week gamified intervention that allowed students to get game rewards through their PA levels was unsuccessful. The IG did not present more steps or active minutes than the CG (assessed using Fitbit). Moreover, 50% of the students participated for fewer than 10 days, and only 21 individuals out of the 105 initial sample played at least one game [34]. The authors reported using Fitbit as a constraint since most participants did not use it during the intervention. Another study using Fitbits for eight weeks also described the lack of consistency in wearing these devices and the decreased motivation for PA in an adolescent population [37]. One possible explanation for these outcomes was that participants felt less competent when they did not reach the 10,000 steps/day goal and because they felt like competing with their friends [37]. Therefore, it is recommended to encourage self-referenced comparisons of performance instead of engaging in normative comparisons with peers or established recommendations.
Research among school-age children indicates that they may be significantly influenced by their friends’ PA levels and obesity-related behaviors [38,39]. Literature has mentioned that physically active children positively impact their peers’ PA [40,41,42]. The investigation conducted on 125 students between 9 and 13 years concluded that PA and BMI affected friendship formation and dissolution. In summary, children became more likely to stop being friends with children with different BMI or PA levels and more likely to relate with others with an affinity for PA or BMI [29]. Indeed, shared common interests should be one of the most decisive factors for friendship and choosing to spend time with others during recess.
Meanwhile, eating habits were significantly improved after 14 weeks of mHealth app usage in 139 children aged between 11 and 15 years [24]. Another study aimed to monitor dietary intake through an app in 33 students aged between 16 and 18 years, reporting a significant decrease in sodium and calcium intake between pre-and post-intervention analyses [31]. However, more than 70% of the participants reported trouble remembering to record their food intake [31]. Although some real advantages emerge from mHealth tools over paper diaries, various challenges and obstacles in food intake monitoring still exist, particularly concerning its accuracy [43]. A critical finding in the study of Lee et al. [31] was that nearly 48% of the participants liked getting personal information about their dietary intake from the app, which may underline the value of individualized approaches while using mHealth solutions.
In this review, only one study has considered teachers in the sample to assess social engagement with an mHealth app [33]. The results showed that the active involvement of a role model (i.e., a teacher) could impact the number and type of activities that preadolescents perform. Additionally, the authors observed that students monitored the intergroup competition more closely than the intragroup competition since they checked the app more often when involved in team-based comparisons [33]. Understanding the students’ motivations is crucial to establish the requisites of an mHealth solution focused on promoting healthy lifestyles. Otherwise, the use of the digital tool may be restricted at the beginning of the intervention when it is still a novelty. In fact, in this review, only seven studies managed to get 80–100% of the participants from the baseline to the intervention completion. In contrast, six studies presented a dropout rate of at least 20%. The highest dropout rate corresponded to nearly 62% in the IG and 30% in the CG among students aged between 12 and 16 years [35].
Digital health tools were also used in the school context to improve vaccination rates and knowledge regarding reproductive health among participants aged between 14 and 19 years [23,25]. In both studies, educational support given by interactive classroom content or SMS proved to be an easy and effective approach to enhance students’ awareness and literacy concerning these topics. However, the literature has identified gamified situations as more attractive among children [44,45]. Rewards, feedback, and socialization aspects are frequently employed through gamified mHealth [45]. Therefore, stakeholders should consider the users’ age range during the deployment of digital solutions to provide a successful tool.
Although the number of studies included in this review is limited, it underlines an important gap in the literature concerning the use of mHealth designed in the school environment. Childhood and adolescence are crucial for developing healthy lifestyles, such as regular engagement in PA and a healthy diet, and increasing health literacy [38]. Since youngsters are a significant part of their day-involved schools, this can be a privileged context to implement strategies focused on promoting health. Overall, mHealth tools have effectively changed short-term behaviors and increased network cohesion. However, shared challenges have emerged concerning dropout rates or the continuous decrease in users’ interaction with the respective tools during interventions. On the other hand, although the growing increase in smartphone usage, it is still important considering youngers with fewer opportunities for technology access.
Our results bring critical practical implications for the future design of mHealth solutions, such as considering the target audience age range, allowing the possibility of user interaction, and including self-referenced performance comparisons instead of focusing exclusively on group comparisons. Furthermore, it could be beneficial to gradually introduce new and appealing content in future digital solutions to avoid app usage decline over time. Future research is still needed to investigate which contents and strategies might be more effective in maintaining youngsters’ engagement in mHealth solutions, particularly considering different age ranges and gender.
5. Conclusions
Results from this systematic review suggest that mHealth tools are effective for short-term behavior change and developing knowledge towards health. Intervention duration ranged between four and 24 weeks, and only one study did not report positive outcomes from a 12-week pilot study based on a gamified situation. Overall, only seven studies managed to have at least 80% of the participants from the baseline to the intervention completion, and app usage tended to decline post-intervention. Adding personal information, user interaction, and self-reference comparisons of performance seems crucial for designing a successful digital tool for behavior change in school-aged children and adolescents.
Author Contributions
Conceptualization, C.F., F.S., F.M., and É.R.G.; methodology, C.F., F.G., and F.M.; software, C.F., F.S., and F.M.; validation, B.G., H.L., F.G., P.C., A.M., T.G., A.I., and É.R.G.; formal analysis, C.F., F.S., and F.M; investigation, C.F., F.S., and F.M.; resources, F.G., P.C., B.G., H.L., T.G., and É.R.G.; data curation, C.F., F.S. and F.M.; writing—original draft preparation, C.F., F.S., and F.M.; writing—review and editing, H.L., B.G., F.G., P.C., A.M., T.G., A.I., and É.R.G.; visualization, A.M., A.I., and É.R.G.; supervision, B.G., A.M., H.L., and É.R.G.; project administration, É.R.G.; funding acquisition, P.C., F.G., H.L., B.G., and É.R.G. All authors have read and agreed to the published version of the manuscript.
Funding
É.R.G., C.F., F.M., F.G., P.C., and B.G. acknowledge support from LARSyS—the Portuguese national funding agency for science, research, and technology (FCT) pluriannual funding 2020–2023 (Reference: UIDB/50009/2020). This study is framed in the Saúde Escolas: Projeto de Monitorização em Saúde (SEE_App). The project received funding under application no. M1420-01-0247-FEDER-000042 in the System of Incentives for the Production of Scientific and Technological Knowledge in the Autonomous Region of Madeira—PROCiência 2020.
Institutional Review Board Statement
Ethical review and approval were waived for this study since this study comprises a systematic review of digital health in schools. The study protocol was registered with PROSPERO (CRD42022349149).
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Marcolino, M.S.; Oliveira, J.A.Q.; D’Agostino, M.; Ribeiro, A.L.; Alkmim, M.B.M.; Novillo-Ortiz, D. The impact of mHealth interventions: Systematic review of systematic reviews. JMIR MHealth UHealth 2018, 6, e8873. [Google Scholar] [CrossRef]
- Blandford, A.; Gibbs, J.; Newhouse, N.; Perski, O.; Singh, A.; Murray, E. Seven lessons for interdisciplinary research on interactive digital health interventions. Digit. Health 2018, 4, 2055207618770325. [Google Scholar] [CrossRef]
- Gurman, T.A.; Rubin, S.E.; Roess, A.A. Effectiveness of mHealth behavior change communication interventions in developing countries: A systematic review of the literature. J. Health Commun. 2012, 17, 82–104. [Google Scholar] [CrossRef] [PubMed]
- Nglazi, M.D.; Bekker, L.-G.; Wood, R.; Hussey, G.D.; Wiysonge, C.S. Mobile phone text messaging for promoting adherence to anti-tuberculosis treatment: A systematic review. BMC Infect. Dis. 2013, 13, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Ali, E.E.; Chew, L.; Yap, K.Y.L. Evolution and current status of mhealth research: A systematic review. BMJ Innov. 2016, 2, 33–40. [Google Scholar] [CrossRef]
- Matthew-Maich, N.; Harris, L.; Ploeg, J.; Markle-Reid, M.; Valaitis, R.; Ibrahim, S.; Gafni, A.; Isaacs, S. Designing, implementing, and evaluating mobile health technologies for managing chronic conditions in older adults: A scoping review. JMIR MHealth UHealth 2016, 4, e5127. [Google Scholar] [CrossRef]
- Chiarini, G.; Ray, P.; Akter, S.; Masella, C.; Ganz, A. mHealth technologies for chronic diseases and elders: A systematic review. IEEE J. Sel. Areas Commun. 2013, 31, 6–18. [Google Scholar] [CrossRef]
- Bradway, M.; Carrion, C.; Vallespin, B.; Saadatfard, O.; Puigdomènech, E.; Espallargues, M.; Kotzeva, A. mHealth assessment: Conceptualization of a global framework. JMIR MHealth UHealth 2017, 5, e7291. [Google Scholar] [CrossRef]
- Stark, A.L.; Geukes, C.; Dockweiler, C. Digital Health Promotion and Prevention in Settings: Scoping Review. J. Med. Internet Res. 2022, 24, e21063. [Google Scholar] [CrossRef]
- Bendtsen, M.; Seiterö, A.; Bendtsen, P.; Henriksson, H.; Henriksson, P.; Thomas, K.; Löf, M.; Müssener, U. mHealth intervention for multiple lifestyle behaviour change among high school students in Sweden (LIFE4YOUth): Protocol for a randomised controlled trial. BMC Public Health 2021, 21, 1–12. [Google Scholar] [CrossRef]
- Tryfona, C.; Oatley, G.; Calderon, A.; Thorne, S. M-Health solutions to support the national health service in the diagnosis and monitoring of autism spectrum disorders in young children. In Proceedings of the International Conference on Universal Access in Human-Computer Interaction, Toronto, Canada, 17–22 July 2016; pp. 249–256. [Google Scholar]
- Michie, S.; Richardson, M.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W.; Eccles, M.P.; Cane, J.; Wood, C.E. The behavior change technique taxonomy of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Ann. Behav. Med. 2013, 46, 81–95. [Google Scholar] [CrossRef] [PubMed]
- Paakkari, L.; Paakkari, O. Health literacy as a learning outcome in schools. Health Educ. 2012, 112, 133–152. [Google Scholar] [CrossRef]
- Peralta, L.; Rowling, L.; Samdal, O.; Hipkins, R.; Dudley, D. Conceptualising a new approach to adolescent health literacy. Health Educ. J. 2017, 76, 787–801. [Google Scholar] [CrossRef]
- Geller, R.J.; Rubin, I.L.; Nodvin, J.T.; Teague, W.G.; Frumkin, H. Safe and healthy school environments. Pediatr. Clin. N. Am. 2007, 54, 351–373. [Google Scholar] [CrossRef] [PubMed]
- Hagell, A.; Rigby, E.; Perrow, F. Promoting health literacy in secondary schools: A review. Br. J. Sch. Nurs. 2015, 10, 82–87. [Google Scholar] [CrossRef]
- Nash, R.; Patterson, K.; Flittner, A.; Elmer, S.; Osborne, R. School-Based Health Literacy Programs for Children (2–16 Years): An International Review. J. Sch. Health 2021, 91, 632–649. [Google Scholar] [CrossRef]
- Middelweerd, A.; Mollee, J.S.; van der Wal, C.N.; Brug, J.; Velde, S.J.T. Apps to promote physical activity among adults: A review and content analysis. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 1–9. [Google Scholar] [CrossRef]
- Conroy, D.E.; Yang, C.-H.; Maher, J.P. Behavior change techniques in top-ranked mobile apps for physical activity. Am. J. Prev. Med. 2014, 46, 649–652. [Google Scholar] [CrossRef]
- Lyons, E.J.; Lewis, Z.H.; Mayrsohn, B.G.; Rowland, J.L. Behavior change techniques implemented in electronic lifestyle activity monitors: A systematic content analysis. J. Med. Internet Res. 2014, 16, e3469. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 1–11. [Google Scholar] [CrossRef]
- Thomas, B.; Ciliska, D.; Dobbins, M.; Micucci, S. Quality Assessment Tool for Quantitative Studies Dictionary: The Effective Public Health Practice Project (EPHPP); McMaster University: Hamilton, Canada, 2008. [Google Scholar]
- Ahmed, T. Effect of mHealth tool on knowledge regarding reproductive health of school going adolescent girls: A before-after quasi-experimental study. BMJ Open 2020, 10, e036656. [Google Scholar] [CrossRef]
- Benítez-Andrades, J.A.; Arias, N.; García-Ordás, M.T.; Martínez-Martínez, M.; García-Rodríguez, I. Feasibility of Social-Network-Based eHealth Intervention on the Improvement of Healthy Habits among Children. Sensors 2020, 20, 1404. [Google Scholar] [CrossRef]
- Bethke, N.; Gellert, P.; Knoll, N.; Weber, N.; Seybold, J. A school-based educational on-site vaccination intervention for adolescents in an urban area in Germany: Feasibility and psychometric properties of instruments in a pilot study. BMC Public Health 2022, 22, 60. [Google Scholar] [CrossRef]
- Brown, J.M.; Savaglio, R.; Watson, G.; Kaplansky, A.; LeSage, A.; Hughes, J.; Kapralos, B.; Arcand, J. Optimizing child nutrition education with the foodbot factory mobile health app: Formative evaluation and analysis. JMIR Form. Res. 2020, 4, e15534. [Google Scholar] [CrossRef]
- Egilsson, E.; Bjarnason, R.; Njardvik, U. Usage and Weekly Attrition in a Smartphone-Based Health Behavior Intervention for Adolescents: Pilot Randomized Controlled Trial. JMIR Form. Res. 2021, 5, e21432. [Google Scholar] [CrossRef] [PubMed]
- Galy, O.; Yacef, K.; Caillaud, C. Improving Pacific Adolescents’ Physical Activity Toward International Recommendations: Exploratory Study of a Digital Education App Coupled With Activity Trackers. JMIR Mhealth Uhealth 2019, 7, e14854. [Google Scholar] [CrossRef] [PubMed]
- Guerra, A.M.; Montes, F.; Useche, A.F.; Jaramillo, A.M.; González, S.A.; Meisel, J.D.; Obando, C.; Cardozo, V.; Hunter, R.F.; Sarmiento, O.L. Effects of a Physical Activity Program Potentiated with ICTs on the Formation and Dissolution of Friendship Networks of Children in a Middle-Income Country. Int. J. Environ. Res. Public Health 2020, 17, 5796. [Google Scholar] [CrossRef]
- Hyman, A.; Stewart, K.; Jamin, A.M.; Lauscher, H.N.; Stacy, E.; Kasten, G.; Ho, K. Testing a school-based program to promote digital health literacy and healthy lifestyle behaviours in intermediate elementary students: The Learning for Life program. Prev. Med. Rep. 2020, 19, 101149. [Google Scholar] [CrossRef]
- Lee, J.E.; Song, S.; Ahn, J.S.; Kim, Y.; Lee, J.E. Use of a Mobile Application for Self-Monitoring Dietary Intake: Feasibility Test and an Intervention Study. Nutrients 2017, 9, 748. [Google Scholar] [CrossRef] [PubMed]
- Lyles, A.A.; Amresh, A.; Huberty, J.; Todd, M.; Lee, R.E. A Mobile, Avatar-Based App for Improving Body Perceptions Among Adolescents: A Pilot Test. JMIR Serious Games 2017, 5, e4. [Google Scholar] [CrossRef] [PubMed]
- Nuijten, R.C.Y.; Gorp, P.V.; Borghouts, T.; Blanc, P.L.; den Berg, P.V.; Kemperman, A.; Hadian, E.; Simons, M. Preadolescent Students’ Engagement With an mHealth Intervention Fostering Social Comparison for Health Behavior Change: Crossover Experimental Study. J. Med. Internet Res. 2021, 23, e21202. [Google Scholar] [CrossRef] [PubMed]
- Pope, L.; Garnett, B.; Dibble, M. Lessons Learned Through the Implementation of an eHealth Physical Activity Gaming Intervention with High School Youth. Games Health J. 2018, 7, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Sousa, P.; Martinho, R.; Reis, C.I.; Dias, S.S.; Gaspar, P.J.S.; Dixe, M.D.A.; Luis, L.S.; Ferreira, R. Controlled trial of an mHealth intervention to promote healthy behaviours in adolescence (TeenPower): Effectiveness analysis. J. Adv. Nurs. 2020, 76, 1057–1068. [Google Scholar] [CrossRef] [PubMed]
- Verjans-Janssen, S.R.; van de Kolk, I.; Kann, D.H.V.; Kremers, S.P.; Gerards, S.M. Effectiveness of school-based physical activity and nutrition interventions with direct parental involvement on children’s BMI and energy balance-related behaviors–A systematic review. PLoS ONE 2018, 13, e0204560. [Google Scholar] [CrossRef] [PubMed]
- Kerner, C.; Goodyear, V.A. The motivational impact of wearable healthy lifestyle technologies: A self-determination perspective on Fitbits with adolescents. Am. J. Health Educ. 2017, 48, 287–297. [Google Scholar] [CrossRef]
- la Haye, K.D.; Robins, G.; Mohr, P.; Wilson, C. Obesity-related behaviors in adolescent friendship networks. Soc. Netw. 2010, 32, 161–167. [Google Scholar] [CrossRef]
- Macdonald-Wallis, K.; Jago, R.; Page, A.S.; Brockman, R.; Thompson, J.L. School-based friendship networks and children’s physical activity: A spatial analytical approach. Soc. Sci. Med. 2011, 73, 6–12. [Google Scholar] [CrossRef]
- Garcia, J.M.; Agaronov, A.; Sirard, J.R.; Whaley, D.; Rice, D.J.; Weltman, A. Psychosocial and Friend Influences on Objective Sedentary Behavior and Screen Time: A Mixed Methods Analysis. J. Phys. Act. Health 2017, 14, 213–221. [Google Scholar] [CrossRef]
- Draper, C.; Grobler, L.; Micklesfield, L.; Norris, S. Impact of social norms and social support on diet, physical activity and sedentary behaviour of adolescents: A scoping review. Child. Care Health Dev. 2015, 41, 654–667. [Google Scholar] [CrossRef]
- Fitzgerald, A.; Fitzgerald, N.; Aherne, C. Do peers matter? A review of peer and/or friends’ influence on physical activity among American adolescents. J. Adolesc. 2012, 35, 941–958. [Google Scholar] [CrossRef]
- Vu, T.; Lin, F.; Alshurafa, N.; Xu, W. Wearable food intake monitoring technologies: A comprehensive review. Computers 2017, 6, 4. [Google Scholar] [CrossRef]
- Khamzina, M.; Parab, K.V.; An, R.; Bullard, T.; Grigsby-Toussaint, D.S. Impact of Pokémon Go on physical activity: A systematic review and meta-analysis. Am. J. Prev. Med. 2020, 58, 270–282. [Google Scholar] [CrossRef] [PubMed]
- Sardi, L.; Idri, A.; Fernández-Alemán, J.L. A systematic review of gamification in e-Health. J. Biomed. Inform. 2017, 71, 31–48. [Google Scholar] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).