Factors of the Revisit Intention of Patients in the Primary Health Care System in Argentina
Abstract
:1. Introduction
2. Theoretical Framework and Hypothesis
2.1. Quality → Satisfaction
2.2. Quality → Trust
2.3. Quality → Revisit (Repurchase)
2.4. Satisfaction → Revisit (Repurchase)
2.5. Satisfaction → Trust
2.6. Trust → Revisit Intention
3. Methodology
3.1. Study Design
3.2. Instrument
3.3. Validity and Analysis
3.4. Ethical Considerations
4. Results
4.1. Demographic Data
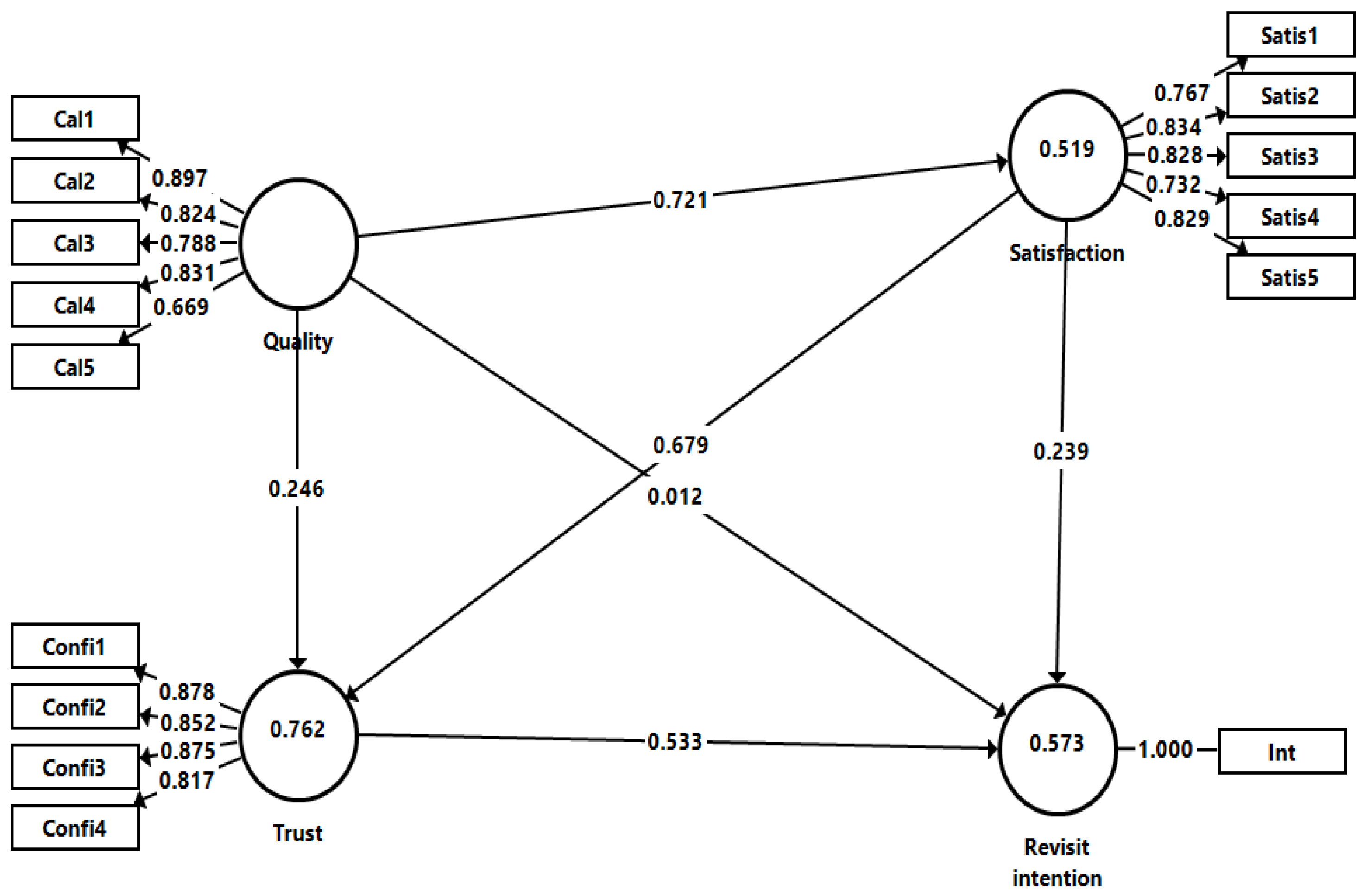
4.2. Discriminant Validity Using SEM-PLS
4.3. Test of Hypothesis
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lozada-Urbano, M.; Huamán, F.; Xirinachs, Y.; Rivera-Lozada, O.; Alvarez-Risco, A.; Yáñez, J.A. Poverty, Household Structure and Consumption of Foods Away from Home in Peru in 2019: A Cross-Sectional Study. Foods 2022, 11, 2547. [Google Scholar] [CrossRef] [PubMed]
- Leclercq-Machado, L.; Alvarez-Risco, A.; Gómez-Prado, R.; Cuya-Velásquez, B.B.; Esquerre-Botton, S.; Morales-Ríos, F.; Almanza-Cruz, C.; Castillo-Benancio, S.; de las Mercedes Anderson-Seminario, M.; Del-Aguila-Arcentales, S.; et al. Sustainable Fashion and Consumption Patterns in Peru: An Environmental-Attitude-Intention-Behavior Analysis. Sustainability 2022, 14, 9965. [Google Scholar] [CrossRef]
- Leclercq-Machado, L.; Alvarez-Risco, A.; Esquerre-Botton, S.; Almanza-Cruz, C.; Anderson-Seminario, M.L.M.; Del-Aguila-Arcentales, S.; Yáñez, J.A. Effect of Corporate Social Responsibility on Consumer Satisfaction and Consumer Loyalty of Private Banking Companies in Peru. Sustainability 2022, 14, 9078. [Google Scholar] [CrossRef]
- Gómez-Prado, R.; Alvarez-Risco, A.; Cuya-Velásquez, B.B.; Anderson-Seminario, M.d.l.M.; Del-Aguila-Arcentales, S.; Yáñez, J.A. Product Innovation, Market Intelligence and Pricing Capability as a Competitive Advantage in the International Performance of Startups: Case of Peru. Sustainability 2022, 14, 10703. [Google Scholar] [CrossRef]
- Biswas, R.K.; Farzana, M.; Bhar, S.; Bhowmik, J. Contraceptive use in South and South-East Asian region: Assessment of sustainable development goal 3.7 through indicator 3.7.1. J. Public Health 2022, fdac105. [Google Scholar] [CrossRef]
- Deng, J. Sustainable Development Research of Green Smart Park in High-End Manufacturing Based on Internet of Things. J. Environ. Public Health 2022, 2022, 3961647. [Google Scholar] [CrossRef]
- Sundewall, J.; Forsberg, B.C. Understanding health spending for SDG 3. Lancet 2020, 396, 650–651. [Google Scholar] [CrossRef]
- Abou, J.; Crutzen, S.; Tromp, V.; Heringa, M.; Van Marum, R.; Elders, P.; Taxis, K.; Denig, P.; Hugtenburg, J. Barriers and Enablers of Healthcare Providers to Deprescribe Cardiometabolic Medication in Older Patients: A Focus Group Study. Drugs Aging 2022, 39, 209–221. [Google Scholar] [CrossRef]
- Zinatsa, F.; Engelbrecht, M.; van Rensburg, A.J.; Kigozi, G. Voices from the frontline: Barriers and strategies to improve tuberculosis infection control in primary health care facilities in South Africa. BMC Health Serv. Res. 2018, 18, 269. [Google Scholar] [CrossRef]
- Trinka, E.; Kwan, P.; Lee, B.; Dash, A. Epilepsy in Asia: Disease burden, management barriers, and challenges. Epilepsia 2019, 60, 7–21. [Google Scholar] [CrossRef]
- Martina, D.; Lin, C.-P.; Kristanti, M.S.; Bramer, W.M.; Mori, M.; Korfage, I.J.; van der Heide, A.; van der Rijt, C.C.D.; Rietjens, J.A.C. Advance Care Planning in Asia: A Systematic Narrative Review of Healthcare Professionals’ Knowledge, Attitude, and Experience. J. Am. Med. Dir. Assoc. 2021, 22, e341–e349. [Google Scholar] [CrossRef] [PubMed]
- Blackwood, D.H.; Walker, D.; Mythen, M.G.; Taylor, R.M.; Vindrola-Padros, C. Barriers to advance care planning with patients as perceived by nurses and other healthcare professionals: A systematic review. J. Clin. Nurs. 2019, 28, 4276–4297. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, S.R.; Connaghan, J.; Maguire, R.; Kotronoulas, G.; Flannagan, C.; Jain, S.; Brady, N.; McCaughan, E. Healthcare professional perceived barriers and facilitators to discussing sexual wellbeing with patients after diagnosis of chronic illness: A mixed-methods evidence synthesis. Patient Educ. Couns. 2019, 102, 850–863. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abdel-Rahman, O. Patient-related barriers to some virtual healthcare services among cancer patients in the USA: A population-based study. J. Comp. Eff. Res. 2021, 10, 119–126. [Google Scholar] [CrossRef]
- Haleem, A.; Javaid, M.; Singh, R.P.; Suman, R. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sens. Int. 2021, 2, 100117. [Google Scholar] [CrossRef]
- Schwarz, D.; Hirschhorn, L.R.; Kim, J.-H.; Ratcliffe, H.L.; Bitton, A. Continuity in primary care: A critical but neglected component for achieving high-quality universal health coverage. BMJ Glob. Health 2019, 4, e001435. [Google Scholar] [CrossRef] [Green Version]
- WHO. 9th Global Conference on Health Promotion: Global Leaders Agree to Promote Health in Order to Achieve Sustainable Development Goals. Available online: https://www.who.int/news/item/21-11-2016-9th-global-conference-on-health-promotion-global-leaders-agree-to-promote-health-in-order-to-achieve-sustainable-development-goals (accessed on 4 April 2022).
- Kirchhoff, S.; Dadaczynski, K.; Pelikan, J.M.; Zelinka-Roitner, I.; Dietscher, C.; Bittlingmayer, U.H.; Okan, O. Organizational Health Literacy in Schools: Concept Development for Health-Literate Schools. Int. J. Environ. Res. Public Health 2022, 19, 8795. [Google Scholar] [CrossRef]
- Yáñez, J.A.; Remsberg, C.M.; Takemoto, J.K.; Vega-Villa, K.R.; Andrews, P.K.; Sayre, C.L.; Martinez, S.E.; Davies, N.M. Polyphenols and Flavonoids: An Overview. In Flavonoid Pharmacokinetics: Methods of Analysis, Preclinical and Clinical Pharmacokinetics, Safety, and Toxicology; Davies, N.M., Yáñez, J.A., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2012; pp. 1–69. [Google Scholar]
- Ramos-Escudero, F.; Santos-Buelga, C.; Pérez-Alonso, J.J.; Yáñez, J.A.; Dueñas, M. HPLC-DAD-ESI/MS identification of anthocyanins in Dioscorea trifida L. yam tubers (purple sachapapa). Eur. Food Res. Technol. 2010, 230, 745–752. [Google Scholar] [CrossRef]
- Lurie, I.; Maree, S.; Mendlovic, S.; Shefet, D. Psychiatrists’ awareness of the cost of medication, rates of social disability pension, and their attitudes regarding knowledge of treatment costs. Isr. J. Health Policy Res. 2022, 11, 35. [Google Scholar] [CrossRef]
- Villena-Tejada, M.; Vera-Ferchau, I.; Cardona-Rivero, A.; Zamalloa-Cornejo, R.; Quispe-Florez, M.; Frisancho-Triveño, Z.; Abarca-Meléndez, R.C.; Alvarez-Sucari, S.G.; Mejia, C.R.; Yañez, J.A. Use of medicinal plants for COVID-19 prevention and respiratory symptom treatment during the pandemic in Cusco, Peru: A cross-sectional survey. PLoS ONE 2021, 16, e0257165. [Google Scholar] [CrossRef]
- Gigli, K.H.; Graaf, G. Changes in Use and Access to Care for Children and Youth With Special Health Care Needs During the COVID-19 Pandemic. J. Pediatr. Health Care 2022. [Google Scholar] [CrossRef]
- Alvarez-Risco, A.; Del-Aguila-Arcentales, S.; Yáñez, J.A.; Rosen, M.A.; Mejia, C.R. Influence of Technostress on Academic Performance of University Medicine Students in Peru during the COVID-19 Pandemic. Sustainability 2021, 13, 8949. [Google Scholar] [CrossRef]
- Alvarez-Risco, A.; Del-Aguila-Arcentales, S.; Yanez, J.A. Telemedicine in Peru as a Result of the COVID-19 Pandemic: Perspective from a Country with Limited Internet Access. Am. J. Trop. Med. Hyg. 2021, 105, 6–11. [Google Scholar] [CrossRef] [PubMed]
- Yáñez, J.A.; Alvarez-Risco, A.; Delgado-Zegarra, J. Covid-19 in Peru: From supervised walks for children to the first case of Kawasaki-like syndrome. BMJ Clin. Res. 2020, 369, m2418. [Google Scholar] [CrossRef] [PubMed]
- Khazanchi, R.; Heard-Garris, N.J.; Winkelman, T.N.A. Health Care Access and Use Among Children & Adolescents Exposed to Parental Incarceration—United States, 2019: Short title: Parental Incarceration and Child/Adolescent Access to Care. Acad. Pediatr. 2022. [Google Scholar] [CrossRef]
- Serchen, J.; Mathew, S.; Hilden, D.; Southworth, M.; Atiq, O. Supporting the Health and Well-Being of Indigenous Communities: A Position Paper From the American College of Physicians. Ann. Intern. Med. 2022. [Google Scholar] [CrossRef]
- Haider, K.A.; Gulam, O.; Adamjee, R.; Balouch, B.; Hoodbhoy, Z. Health workers’ experience of a digital health intervention implemented in peri-urban communities in Karachi, Pakistan. Digit. Health 2022, 8, 20552076221129076. [Google Scholar] [CrossRef]
- Cheng, W.; Zhang, Z.; Hoelzer, S.; Tang, W.; Liang, Y.; Du, Y.; Xue, H.; Zhou, Q.; Yip, W.; Ma, X.; et al. Evaluation of a village-based digital health kiosks program: A protocol for a cluster randomized clinical trial. Digit. Health 2022, 8, 20552076221129100. [Google Scholar] [CrossRef]
- Corscadden, L.; Levesque, J.F.; Lewis, V.; Strumpf, E.; Breton, M.; Russell, G. Factors associated with multiple barriers to access to primary care: An international analysis. Int. J. Equity Health 2018, 17, 28. [Google Scholar] [CrossRef] [Green Version]
- Osae, S.P.; Chastain, D.B.; Young, H.N. Pharmacists role in addressing health disparities—Part 1: Social determinants of health and their intersectionality with medication use, health care utilization, and health outcomes. JACCP J. Am. Coll. Clin. Pharm. 2022, 5, 533–540. [Google Scholar] [CrossRef]
- Bonin, A.M.; Yáñez, J.A.; Fukuda, C.; Teng, X.W.; Dillon, C.T.; Hambley, T.W.; Lay, P.A.; Davies, N.M. Inhibition of experimental colorectal cancer and reduction in renal and gastrointestinal toxicities by copper-indomethacin in rats. Cancer Chemother. Pharmacol. 2010, 66, 755–764. [Google Scholar] [CrossRef]
- Vega-Villa, K.R.; Remsberg, C.M.; Ohgami, Y.; Yanez, J.A.; Takemoto, J.K.; Andrews, P.K.; Davies, N.M. Stereospecific high-performance liquid chromatography of taxifolin, applications in pharmacokinetics, and determination in tu fu ling (Rhizoma smilacis glabrae) and apple (Malus x domestica). Biomed. Chromatogr. 2009, 23, 638–646. [Google Scholar] [CrossRef] [PubMed]
- Yáñez, J.A.; Miranda, N.D.; Remsberg, C.M.; Ohgami, Y.; Davies, N.M. Stereospecific high-performance liquid chromatographic analysis of eriodictyol in urine. J. Pharm. Biomed. Anal. 2007, 43, 255–262. [Google Scholar] [CrossRef]
- Agarwal, S.; Simmonds, I.; Myers, A.K. The Use of Diabetes Technology to Address Inequity in Health Outcomes: Limitations and Opportunities. Curr. Diab. Rep. 2022, 22, 275–281. [Google Scholar] [CrossRef] [PubMed]
- Coles, E.; Anderson, J.; Maxwell, M.; Harris, F.M.; Gray, N.M.; Milner, G.; MacGillivray, S. The influence of contextual factors on healthcare quality improvement initiatives: A realist review. Syst. Rev. 2020, 9, 94. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lázaro Pérez Peña, J.; Jiménez Rodríguez, D. The discreet charm of medicines [El discreto encanto de los medicamentos]. Rev. Cuba. Salud Pública 2014, 40, 349–360. [Google Scholar]
- Jain, R.; Tobey, M. The Indian Health Service can meet its goals for hepatitis C virus treatment through telehealth expansion. J. Rural. Health Off. J. Am. Rural. Health Assoc. Natl. Rural. Health Care Assoc. 2022. [Google Scholar] [CrossRef]
- Soliman, A.A.; Akgün, K.M.; Coffee, J.; Kapo, J.; Morrison, L.J.; Hopkinson, E.; Schulman-Green, D.; Feder, S.L. Quality of Telehealth-Delivered Inpatient Palliative Care During the Early COVID-19 Pandemic. J. Pain Symptom. Manag. 2022. [Google Scholar] [CrossRef]
- Salameh, A.A.; Amin, S.; Danish, M.H.; Asghar, N.; Naveed, R.T.; Munir, M. Socio-economic determinants of subjective wellbeing toward Sustainable Development Goals: An insight from a developing country. Front. Psychol. 2022, 13, 961400. [Google Scholar] [CrossRef]
- Kooshkebaghi, M.; Emamgholipour, S.; Dargahi, H. Explaining specific taxes management and use in the health sector: A qualitative study. BMC Health Serv. Res. 2022, 22, 1220. [Google Scholar] [CrossRef]
- Xu, X.; Yang, H.; Li, C. Theoretical Model and Actual Characteristics of Air Pollution Affecting Health Cost: A Review. Int. J. Environ. Res. Public Health 2022, 19, 3532. [Google Scholar] [CrossRef] [PubMed]
- García Salman, J.D. Considerations on Natural and Traditional Medicine, the scientific method and the Cuban health system [Consideraciones sobre la Medicina Natural y Tradicional, el método científico y el sistema de salud cubano]. Rev. Cuba. Salud Pública 2013, 39, 540–555. [Google Scholar]
- Seliger, C.; Luber, C.; Gerken, M.; Schaertl, J.; Proescholdt, M.; Riemenschneider, M.J.; Meier, C.R.; Bogdahn, U.; Leitzmann, M.F.; Klinkhammer-Schalke, M.; et al. Use of metformin and survival of patients with high-grade glioma. Int. J. Cancer 2019, 144, 273–280. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lapuente, M.; Estruch, R.; Shahbaz, M.; Casas, R. Relation of Fruits and Vegetables with Major Cardiometabolic Risk Factors, Markers of Oxidation, and Inflammation. Nutrients 2019, 11, 2381. [Google Scholar] [CrossRef] [Green Version]
- Salvadó, M.J.; Casanova, E.; Fernández-Iglesias, A.; Arola, L.; Bladé, C. Roles of proanthocyanidin rich extracts in obesity. Food Funct. 2015, 6, 1053–1071. [Google Scholar] [CrossRef] [Green Version]
- Roupe, K.A.; Helms, G.L.; Halls, S.C.; Yanez, J.A.; Davies, N.M. Preparative enzymatic synthesis and HPLC analysis of rhapontigenin: Applications to metabolism, pharmacokinetics and anti-cancer studies. J. Pharm. Pharm. Sci. 2005, 8, 374–386. [Google Scholar]
- Konfino, J.; Linetzky, B.; Ferrante, D. Evolution and current status of non-communicable diseases in Argentina [Evolución y estado actual de las enfermedades no transmisibles en Argentina]. Rev. Argent. Salud Pública 2010, 1, 27–39. [Google Scholar]
- García Milian, A.J.; López Verde, L.; Pría Barros, M.C.; Cabrera, P.L. Drug use and living conditions [Consumo de medicamentos y condiciones de vida]. Rev. Cuba. Salud Pública 2016, 42, 442–450. [Google Scholar]
- İlhan, S.; Yıldız, M.; Tüzün, H.; Dikmen, A.U. Evaluation of irrational drug use of individuals over the age of 18 who applied to a university hospital. Turk. J. Med. Sci. 2022, 52, 484–493. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Yuan, F.; Li, L.; Jin, J.; He, J. Effects of monthly evaluations on the rates of irrational antimicrobial prescription in the outpatient and emergency departments at Ningbo No. 6 Hospital, Ningbo, China. Eur. J. Med. Res. 2022, 27, 98. [Google Scholar] [CrossRef]
- Liu, H.; Li, H.; Teuwen, D.E.; Sylvia, S.; Shi, H.; Rozelle, S.; Yi, H. Irrational Use of Medicine in the Treatment of Presumptive Asthma Among Rural Primary Care Providers in Southwestern China. Front. Pharmacol. 2022, 13, 767917. [Google Scholar] [CrossRef] [PubMed]
- Cañás, M.; Buschiazzo, H.O.; Urtasun, M.A. Therapeutic value and price of new drugs marketed in Argentina: Are they worth what they cost? [Valor terapéutico y precio de los nuevos fármacos comercializados en Argentina: ¿valen lo que cuestan?]. Salud Colect. 2019, 15, e1962. [Google Scholar] [CrossRef] [PubMed]
- Nieto-Blasco, J.; Vicente-Blanco, M.V.; Calvo-Vera, A.B.; Lobato-Benito, L.; Rubio-Gil, F.J.; Mendoza-García, J.L.; Rodríguez-Pérez, M.P. Satisfaction study of patients treated at the CAUSA Rehabilitation Service [Estudio de satisfacción de los pacientes atendidos en el Servicio de Rehabilitación del CAUSA]. Rehabilitación 2018, 52, 28–37. [Google Scholar] [CrossRef]
- Jimeno-Serrano, F.J.; Medina-Mirapeix, F.; Escolar-Reina, P.; DelBaño-Aledo, M.E. Patient satisfaction and experiences in rehabilitation centers associated with their trust in the professionalism of physical therapists [Satisfacción y experiencias de los pacientes en centros de rehabilitación asociados con su confianza en la profesionalidad de los fisioterapeutas]. Rehabilitación 2012, 46, 227–235. [Google Scholar] [CrossRef]
- Osuna Pérez, C. Therapeutic Information, Satisfaction and Confidence in Physiotherapy: Measurement Instruments and Correlational Study in Physiotherapy Centers in Eastern Andalusia [Información Terapéutica, Satisfacción y Confianza en Fisioterapia: Instrumentos de Medida y Estudio Correlacional en Centros de Fisioterapia de Andalucía Oriental]. Ph.D. Thesis, Universidad de Jaén, Japen, Spain, 2012. [Google Scholar]
- Kijima, T.; Matsushita, A.; Akai, K.; Hamano, T.; Takahashi, S.; Fujiwara, K.; Fujiwara, Y.; Sato, M.; Nabika, T.; Sundquist, K.; et al. Patient satisfaction and loyalty in Japanese primary care: A cross-sectional study. BMC Health Serv. Res. 2021, 21, 274. [Google Scholar] [CrossRef] [PubMed]
- Goetz, K.; Jossen, M.; Rosemann, T.; Hess, S.; Brodowski, M.; Bezzola, P. Is patient loyalty associated with quality of care? Results of a patient survey over primary care in Switzerland. Int. J. Qual. Health Care 2019, 31, 199–204. [Google Scholar] [CrossRef]
- Revilla Arias, H.; González Mustelier, D.; Valenzuela Fonseca, L.M. Quality of health care provided in a comprehensive community-based rehabilitation service [Calidad de la atención de salud brindada en un servicio de rehabilitación integral de base comunitaria]. Medisan 2016, 20, 313–319. [Google Scholar]
- Khatoon, S.; Zhengliang, X.; Hussain, H. The Mediating Effect of Customer Satisfaction on the Relationship Between Electronic Banking Service Quality and Customer Purchase Intention: Evidence From the Qatar Banking Sector. SAGE Open 2020, 10, 2158244020935887. [Google Scholar] [CrossRef]
- Nguyen, T.L.H.; Nagase, K. The influence of total quality management on customer satisfaction. Int. J. Healthc. Manag. 2019, 12, 277–285. [Google Scholar] [CrossRef]
- Fatima, T.; Malik, S.A.; Shabbir, A. Hospital healthcare service quality, patient satisfaction and loyalty. Int. J. Qual. Reliab. Manag. 2018, 35, 1195–1214. [Google Scholar] [CrossRef]
- Ng, J.H.Y.; Luk, B.H.K. Patient satisfaction: Concept analysis in the healthcare context. Patient Educ. Couns. 2019, 102, 790–796. [Google Scholar] [CrossRef] [PubMed]
- Javed, S.A.; Liu, S.; Mahmoudi, A.; Nawaz, M. Patients’ satisfaction and public and private sectors’ health care service quality in Pakistan: Application of grey decision analysis approaches. Int. J. Health Plan. Manag. 2019, 34, e168–e182. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suhail, P.; Srinivasulu, Y. Perception of service quality, satisfaction, and behavioral intentions in Ayurveda healthcare. J. Ayurveda Integr. Med. 2021, 12, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Radu, F.; Radu, V.; Turkeș, M.C.; Ivan, O.R.; Tăbîrcă, A.I. A research of service quality perceptions and patient satisfaction: Case study of public hospitals in Romania. Int. J. Health Plan. Manag. 2022, 37, 1018–1048. [Google Scholar] [CrossRef]
- Chen, L.; Li, Y.-Q.; Liu, C.-H. How airline service quality determines the quantity of repurchase intention—Mediate and moderate effects of brand quality and perceived value. J. Air Transp. Manag. 2019, 75, 185–197. [Google Scholar] [CrossRef]
- Nasir, M.; Adil, M.; Dhamija, A. The synergetic effect of after sales service, customer satisfaction, loyalty and repurchase intention on word of mouth. Int. J. Qual. Serv. Sci. 2021, 13, 489–505. [Google Scholar] [CrossRef]
- Antwi, S. “I just like this e-Retailer”: Understanding online consumers repurchase intention from relationship quality perspective. J. Retail. Consum. Serv. 2021, 61, 102568. [Google Scholar] [CrossRef]
- Tandon, A.; Aakash, A.; Aggarwal, A.G. Impact of EWOM, website quality, and product satisfaction on customer satisfaction and repurchase intention: Moderating role of shipping and handling. Int. J. Syst. Assur. Eng. Manag. 2020, 11, 349–356. [Google Scholar] [CrossRef]
- Chang, W.-J.; Liao, S.-H.; Chung, Y.-C.; Chen, H.-P. Service quality, experiential value and repurchase intention for medical cosmetology clinic: Moderating effect of Generation. Total Qual. Manag. Bus. Excell. 2020, 31, 1077–1097. [Google Scholar] [CrossRef]
- Ali, A.; Bhasin, J. Understanding Customer Repurchase Intention in E-commerce: Role of Perceived Price, Delivery Quality, and Perceived Value. Jindal J. Bus. Res. 2019, 8, 142–157. [Google Scholar] [CrossRef]
- Amoako, G.K.; Caesar, L.D.; Dzogbenuku, R.K.; Bonsu, G.A. Service recovery performance and repurchase intentions: The mediation effect of service quality at KFC. J. Hosp. Tour. Insights 2021. ahead-of-print. [Google Scholar] [CrossRef]
- Anderson, E.W.; Sullivan, M.W. The Antecedents and Consequences of Customer Satisfaction for Firms. Mark. Sci. 1993, 12, 125–143. [Google Scholar] [CrossRef]
- Bloemer, J.; de Ruyter, K. On the relationship between store image, store satisfaction and store loyalty. Eur. J. Mark. 1998, 32, 499–513. [Google Scholar] [CrossRef]
- Levesque, T.; McDougall, G.H.G. Determinants of customer satisfaction in retail banking. Int. J. Bank Mark. 1996, 14, 12–20. [Google Scholar] [CrossRef]
- Zeithaml, V.A.; Berry, L.L.; Parasuraman, A. The Behavioral Consequences of Service Quality. J. Mark. 1996, 60, 31–46. [Google Scholar] [CrossRef]
- Chiguvi, D.; Guruwo, P. Impact of Customer Satisfaction on Customer Loyalty in the Banking Sector. Int. J. Sci. Eng. Res. 2017, 5, 55–63. [Google Scholar]
- Oliver, R.L. Whence Consumer Loyalty? J. Mark. 1999, 63, 33–44. [Google Scholar] [CrossRef]
- Lee, M.A.; Yom, Y.-H. A comparative study of patients’ and nurses’ perceptions of the quality of nursing services, satisfaction and intent to revisit the hospital: A questionnaire survey. Int. J. Nurs. Stud. 2007, 44, 545–555. [Google Scholar] [CrossRef]
- Woo, S.; Choi, M. Medical service quality, patient satisfaction and intent to revisit: Case study of public hub hospitals in the Republic of Korea. PLoS ONE 2021, 16, e0252241. [Google Scholar] [CrossRef]
- Park, S.; Kim, H.-K.; Choi, M.; Lee, M. Factors affecting revisit intention for medical services at dental clinics. PLoS ONE 2021, 16, e0250546. [Google Scholar] [CrossRef]
- Assaker, G.; O’Connor, P.; El-Haddad, R. Examining an integrated model of green image, perceived quality, satisfaction, trust, and loyalty in upscale hotels. J. Hosp. Mark. Manag. 2020, 29, 934–955. [Google Scholar] [CrossRef]
- Fauzi, A.A.; Suryani, T. Measuring the effects of service quality by using CARTER model towards customer satisfaction, trust and loyalty in Indonesian Islamic banking. J. Islamic Mark. 2019, 10, 269–289. [Google Scholar] [CrossRef]
- Kalia, P.; Kaushal, R.; Singla, M.; Parkash, J. Determining the role of service quality, trust and commitment to customer loyalty for telecom service users: A PLS-SEM approach. TQM J. 2021, 33, 377–396. [Google Scholar] [CrossRef]
- Martínez-Navalón, J.G.; Gelashvili, V.; Saura, J.R. The impact of environmental social media publications on user satisfaction with and trust in tourism businesses. Int. J. Environ. Res. Public Health 2020, 17, 5417. [Google Scholar] [CrossRef] [PubMed]
- Mohd Isa, S.; Lim, G.S.S.; Chin, P.N. Patients’ intent to revisit with trust as the mediating role: Lessons from Penang Malaysia. Int. J. Pharm. Healthc. Mark. 2019, 13, 140–159. [Google Scholar] [CrossRef]
- Sun, T.; Zhang, J.; Zhang, B.; Ong, Y.; Ito, N. How trust in a destination’s risk regulation navigates outbound travel constraints on revisit intention post-COVID-19: Segmenting insights from experienced Chinese tourists to Japan. J. Destin. Mark. Manag. 2022, 25, 100711. [Google Scholar] [CrossRef]
- Wijaya, R.; Farida, N.; Andriyansah. Determinants of Repurchase Intentions at Online Stores in Indonesia. Int. J. E-Bus. Res. (IJEBR) 2018, 14, 95–111. [Google Scholar] [CrossRef]
- Hassanein, K.; Head, M. Manipulating perceived social presence through the web interface and its impact on attitude towards online shopping. Int. J. Hum.-Comput. Stud. 2007, 65, 689–708. [Google Scholar] [CrossRef]
- Gefen, D.; Karahanna, E.; Straub, D.W. Trust and TAM in Online Shopping: An Integrated Model. MIS Q. 2003, 27, 51–90. [Google Scholar] [CrossRef]
- Pozdnyakova, A.; Laiteerapong, N.; Volerman, A.; Feld, L.D.; Wan, W.; Burnet, D.L.; Lee, W.W. Impact of Medical Scribes on Physician and Patient Satisfaction in Primary Care. J. Gen. Intern. Med. 2018, 33, 1109–1115. [Google Scholar] [CrossRef] [Green Version]
- Villagarcía Trujiilo, E.X.; Delgadillo Guzmán, L.G.; Argüello Zepeda, F.J.; González Villanueva, L. User perception of the quality of the ISSEMyM health services [Percepción usuaria de la calidad en los servicios de salud del ISSEMyM]. Horiz. Sanit. 2017, 16, 46–54. [Google Scholar] [CrossRef] [Green Version]
- Cronin, J.J.; Taylor, S.A. Measuring Service Quality: A Reexamination and Extension. J. Mark. 1992, 56, 55–68. [Google Scholar] [CrossRef]
- Babakus, E.; Mangold, W.G. Adapting the SERVQUAL scale to hospital services: An empirical investigation. Health Serv. Res. 1992, 26, 767–786. [Google Scholar] [PubMed]
- Bolton, R.N.; Drew, J.H. A Multistage Model of Customers’ Assessments of Service Quality and Value. J. Consum. Res. 1991, 17, 375–384. [Google Scholar] [CrossRef]
- Shafei, I.; Walburg, J.; Taher, A. Verifying alternative measures of healthcare service quality. Int. J. Health Care Qual. Assur. 2019, 32, 516–533. [Google Scholar] [CrossRef]
- Boulding, W.; Kalra, A.; Staelin, R.; Zeithaml, V.A. A Dynamic Process Model of Service Quality: From Expectations to Behavioral Intentions. J. Mark. Res. 1993, 30, 7–27. [Google Scholar] [CrossRef]
- Gómez-Besteiro, M.I.; Somoza-Digón, J.; Einöder-Moreno, M.; Jiménez-Fraga, M.N.; Castiñeira-Pereira, S.; Feijoo-Fuentes, M.L. Quality of health care perceived by patients in an urban health center in La Coruña [Calidad de atención en salud percibida por los pacientes en un centro de salud urbano de La Coruña]. Enfermería Clínica 2012, 22, 182–190. [Google Scholar] [CrossRef]
- Bustamante, M.A.; Zerda, E.; Obando, F.; Tello, M. Fundamentals of service quality, the SERVQUAL model [Fundamentos de la calidad de servicio, el modelo SERVQUAL]. Rev. Empresarial 2019, 13, 1–15. [Google Scholar]
- Jain, S.K.; Gupta, G. Measuring Service Quality: Servqual vs. Servperf Scales. Vikalpa 2004, 29, 25–38. [Google Scholar] [CrossRef]
- Torres Navarro, C.; Jélvez Caamaño, A.; Vega-Pinto, F. Quality assessment in an emergency service using the Servperf model [Evaluación de la calidad en un servicio de urgencia utilizando el modelo Servperf]. Univ. Cienc. Tecnol. 2014, 18, 38–49. [Google Scholar]
- Buitron de la Vega, P.; Losi, S.; Sprague Martinez, L.; Bovell-Ammon, A.; Garg, A.; James, T.; Ewen, A.M.; Stack, M.; DeCarvalho, H.; Sandel, M.; et al. Implementing an EHR-based Screening and Referral System to Address Social Determinants of Health in Primary Care. Med. Care 2019, 57, S133–S139. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez Cabrera, A.; Collazo Ramo, M.; Calero Ricard, J.L.; Álvarez Vázquez, L.; Castañeda Abasca, I. Perceptions of older adults and providers about accessibility to health services [Percepciones de adultos mayores y prestadores acerca de la accesibilidad a servicios de salud]. Rev. Cuba. Salud Pública 2017, 43, 1–12. [Google Scholar]
- Olivares, D.E.V.; Chambi, F.R.V.; Chañi, E.M.M.; Craig, W.J.; Pacheco, S.O.S.; Pacheco, F.J. Risk Factors for Chronic Diseases and Multimorbidity in a Primary Care Context of Central Argentina: A Web-Based Interactive and Cross-Sectional Study. Int. J. Environ. Res. Public Health 2017, 14, 251. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Viego, V.N.; Luján Temporelli, T. Socioeconomic and environmental determinants of arterial hypertension in the adult population of Argentina [Determinantes socioeconómicos y ambientales de la hipertensión arterial en población adulta de Argentina]. Rev. Cuba. Salud Pública 2016, 42, 27–36. [Google Scholar]
- Licea Puig, M.E.; González Calero, T.M. Strategies for the prevention of type 1 diabetes mellitus [Estrategias para la prevención de la diabetes mellitus tipo 1]. Rev. Cuba. Salud Pública 2013, 39, 733–751. [Google Scholar]
- Instituto Nacional del Cáncer. Statistics—Incidence [Estadísticas—Incidencia]. Available online: https://www.argentina.gob.ar/salud/instituto-nacional-del-cancer/estadisticas/incidencia (accessed on 21 April 2022).
- López Verde, F.; Esteva, M.; Vela Vallespín, C. The family doctor in cancer patient care [El médico de familia en la atención al paciente con cáncer]. Aten Primaria 2016, 48, 277–278. [Google Scholar] [CrossRef] [Green Version]
- Esposito, K.; Chiodini, P.; Colao, A.; Lenzi, A.; Giugliano, D. Metabolic Syndrome and Risk of Cancer: A systematic review and meta-analysis. Diabetes Care 2012, 35, 2402–2411. [Google Scholar] [CrossRef] [Green Version]
- Abdelwahab Yousef, A.J. Male Breast Cancer: Epidemiology and Risk Factors. Semin. Oncol. 2017, 44, 267–272. [Google Scholar] [CrossRef]
- Theodoratou, E.; Timofeeva, M.; Li, X.; Meng, X.; Ioannidis, J.P.A. Nature, Nurture, and Cancer Risks: Genetic and Nutritional Contributions to Cancer. Annu. Rev. Nutr. 2017, 37, 293–320. [Google Scholar] [CrossRef]
- Willenbrink, T.J.; Ruiz, E.S.; Cornejo, C.M.; Schmults, C.D.; Arron, S.T.; Jambusaria-Pahlajani, A. Field cancerization: Definition, epidemiology, risk factors, and outcomes. J. Am. Acad. Dermatol. 2020, 83, 709–717. [Google Scholar] [CrossRef]
- Elgart, J.; Pfirter, G.; Gonzalez, L.; Caporale, J. Obesity in Argentina: Epidemiology, morbidity and mortality and economic impact [Obesidad en Argentina: Epidemiología, morbimortalidad e impacto económico]. Rev. Argent. Salud Pública 2010, 1, 6–12. [Google Scholar]
- Castronuovo, L.; Tiscornia, M.V.; Gutkowski, P.; Allemandi, L. Obstacles and perceived facilitators for the consumption of fruits and vegetables: A qualitative study [Obstáculos y facilitadores percibidos para el consumo de Frutas y verduras: Estudio cualitativo]. Rev. Arg. Salud Pública 2019, 10, 14–21. [Google Scholar]
- Huang, H.; Yan, Z.; Chen, Y.; Liu, F. A social contagious model of the obesity epidemic. Sci. Rep. 2016, 6, 37961. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Furones Mourelle, J.A.; Cruz Barrios, M.A.; López Aguilera, A.F.; Broche Villarreal, L.; Jova Boulí, A.P.; Pérez Piñer, J. Adverse drug reactions in Cuban elderly (2003–2013) [Reacciones adversas por medicamentos en ancianos cubanos (2003–2013)]. Rev. Cuba. Salud Pública 2016, 42, 510–523. [Google Scholar]
- Xu, X.; Wang, Q.; Li, C. The Impact of Dependency Burden on Urban Household Health Expenditure and Its Regional Heterogeneity in China: Based on Quantile Regression Method. Front. Public Health 2022, 10, 876088. [Google Scholar] [CrossRef]
- Santos Muñoz, L.; Jiménez López, G.; Alfonso Orta, I. Characterization of adverse drug reactions of low frequency of appearance [Caracterización de las reacciones adversas medicamentosas de baja frecuencia de aparición]. Rev. Cuba. Salud Pública 2018, 44, 71–85. [Google Scholar]
- Amarantou, V.; Chatzoudes, D.; Kechagia, V.; Chatzoglou, P.D. The Impact of Service Quality on Patient Satisfaction and Revisiting Intentions: The Case of Public Emergency Departments. Qual. Manag. Healthc. 2019, 28, 200–208. [Google Scholar] [CrossRef]
- Aliman, N.K.; Mohamad, W.N. Linking Service Quality, Patients’ Satisfaction and Behavioral Intentions: An Investigation on Private Healthcare in Malaysia. Procedia—Soc. Behav. Sci. 2016, 224, 141–148. [Google Scholar] [CrossRef]
| Variable | Items | Source |
|---|---|---|
| Quality of use of health programs | The health clinics I usually go to give me detailed information about my illnesses The health clinics I usually go to give me complete information about my illnesses The health clinics that I usually attend always solve my health problems The health clinics that I usually attend give me security regarding my health The health clinics I usually go to have a good infrastructure | Adapted from Rahmad et al. (2018) [90] |
| Patient satisfaction | I enjoy going to the health clinics that I usually go to It is convenient to go to the health clinics that I usually attend It is a good decision to go to the health clinics that I usually attend Seeing me in the health clinics that I usually attend is pleasant. I am satisfied with the entire experience of the health clinics that I usually attend | Adapted from Hassanein and Head (2007) [91] |
| Patient trust | The health offices I usually go to protect their patients. I think the health clinics I usually go to are doing their best I feel safe going to the health clinics I usually go to The health clinics that I usually go to will always be available to attend to my health problems | Adapted from Rahmad et al. (2018) [90] |
| Patient revisit intention | I intend to continue going to the same offices that I usually visit | Adapted from Gefen et al. (2003) [92] |
| Healthcare Facilities | |
|---|---|
| Health Center No. 17 “Cáritas Guadalupe” | 14.3% |
| Northwest District Municipal Health Center “Olga and Leticia Cossettini” | 24.6% |
| Health Center “Dr. Roque Coullin” | 12.8% |
| Health Center No. 5 “Dr. Pedro Fiorina” | 10.3% |
| C.I.C. “La Cerámica” | 11.8% |
| Health Center “Dr. Luis Pasteur” | 11.1% |
| Center No. 13 “FONAVI” | 15.1% |
| Sex | |
| Female | 62.9% (n = 256) |
| Male | 37.1% (n = 151) |
| Age | |
| Between 18 and 35 years old | 22.9% (n = 93) |
| Between 36 and 50 years old | 37.8% (n = 154) |
| Between 51 and 65 years old | 30.5% (n = 124) |
| More than 65 years old | 8.8% (n = 36) |
| Average age | 45.64 |
| Marital status | |
| Single | 55.0% (n = 224) |
| Married | 37.3% (n = 152) |
| Divorced | 4.4% (n = 18) |
| Widowed | 3.2% (n = 13) |
| Educational level | |
| None | 19.4% (n = 79) |
| Primary | 49.1% (n = 200) |
| Secondary | 23.8% (n = 97) |
| Tertiary | 5.7% (n = 23) |
| University | 2.0% (n = 8) |
| Occupation | |
| Housewife | 25.1% (n = 102) |
| Unemployed | 25.6% (n = 104) |
| Commercial employee | 9.8% (n = 40) |
| Domestic worker | 10.3% (n = 42) |
| Bricklayer | 6.9% (n = 28) |
| Cook | 3.2% (n = 13) |
| Metallurgical employee | 2.2% (n = 9) |
| Retired | 3.2% (n = 13) |
| Teacher | 2.2% (n = 9) |
| Other | 11.3% (n = 46) |
| Chronic Non-Communicable Diseases | N |
|---|---|
| Hypertension | 102 |
| Diabetes | 61 |
| Hypothyroidism | 24 |
| Chronic lung diseases | 12 |
| Hypercholesterolemia | 9 |
| H.I.V. | 9 |
| Other (Chagas disease, rheumatoid arthritis, asthma…) | 26 |
| Variables | Factor Loading | Cronbach’s Alpha | rho_A | Composite Reliability | AVE |
|---|---|---|---|---|---|
| Quality | Q1: 0.897 | 0.862 | 0.871 | 0.901 | 0.649 |
| Q2: 0.824 | |||||
| Q3: 0.788 | |||||
| Q4: 0.831 | |||||
| Q5: 0.669 | |||||
| Trust | T1: 0.878 | 0.878 | 0.880 | 0.916 | 0.639 |
| T2: 0.852 | |||||
| T3: 0.875 | |||||
| T4: 0.817 | |||||
| Satisfaction | RIN1: 0.767 | 0.859 | 0.872 | 0.898 | 0.733 |
| RIN2: 0.834 | |||||
| RIN3: 0.828 | |||||
| RIN4: 0.732 | |||||
| RIN5: 0.829 | |||||
| Revisit Intention | S: 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Variables | Quality | Revisit Intention | Satisfaction | Trust |
|---|---|---|---|---|
| Quality | 0.805 | |||
| Revisit intention | 0.576 | 1.000 | ||
| Satisfaction | 0.721 | 0.704 | 0.856 | |
| Trust | 0.736 | 0.746 | 0.675 | 0.799 |
| Saturated Model | Estimated Model | |
|---|---|---|
| SRMR | 0.077 | 0.077 |
| d_ULS | 0.716 | 0.716 |
| d_G | 0.386 | 0.386 |
| Chi-Square | 853.148 | 853.148 |
| NFI | 0.912 | 0.912 |
| Original | Sample | Standard | T | p-Value | Hypothesis | |
|---|---|---|---|---|---|---|
| H1: Quality → Satisfaction | 0.721 | 0.722 | 0.01 | 23.117 | 0.000 | Accepted |
| H2: Quality → Trust | 0.246 | 0.248 | 0.040 | 6.121 | 0.000 | Accepted |
| H3: Quality → Revisit intention | 0.012 | 0.012 | 0.054 | 0.226 | 0.821 | No Accepted |
| H4: Satisfaction → Revisit intention | 0.239 | 0.0237 | 0.074 | 3.233 | 0.001 | Accepted |
| H5: Satisfaction → Trust | 0.679 | 0.678 | 0.040 | 17.092 | 0.000 | Accepted |
| H6: Trust → Revisit intention | 0.533 | 0.534 | 0.080 | 6.643 | 0.000 | Accepted |
| Original | Sample | Standard | T | p-Value | |
|---|---|---|---|---|---|
| Quality → Trust → Revisit intention | 0.131 | 0.132 | 0.030 | 4.412 | 0.000 |
| Calidad → Satisfaction → Trust | 0.489 | 0.489 | 0.033 | 14.912 | 0.000 |
| Quality → Satisfaction → Revisit intention | 0.172 | 0.172 | 0.055 | 3.130 | 0.002 |
| Satisfaction → Trust → Revisit intention | 0.362 | 0.362 | 0.058 | 6.211 | 0.000 |
| Quality → Satisfaction → Trust → Revisit intention | 0.261 | 0.261 | 0.042 | 6.136 | 0.000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pighin, M.; Alvarez-Risco, A.; Del-Aguila-Arcentales, S.; Rojas-Osorio, M.; Yáñez, J.A. Factors of the Revisit Intention of Patients in the Primary Health Care System in Argentina. Sustainability 2022, 14, 13021. https://doi.org/10.3390/su142013021
Pighin M, Alvarez-Risco A, Del-Aguila-Arcentales S, Rojas-Osorio M, Yáñez JA. Factors of the Revisit Intention of Patients in the Primary Health Care System in Argentina. Sustainability. 2022; 14(20):13021. https://doi.org/10.3390/su142013021
Chicago/Turabian StylePighin, Massimo, Aldo Alvarez-Risco, Shyla Del-Aguila-Arcentales, Mercedes Rojas-Osorio, and Jaime A. Yáñez. 2022. "Factors of the Revisit Intention of Patients in the Primary Health Care System in Argentina" Sustainability 14, no. 20: 13021. https://doi.org/10.3390/su142013021
APA StylePighin, M., Alvarez-Risco, A., Del-Aguila-Arcentales, S., Rojas-Osorio, M., & Yáñez, J. A. (2022). Factors of the Revisit Intention of Patients in the Primary Health Care System in Argentina. Sustainability, 14(20), 13021. https://doi.org/10.3390/su142013021









