The Effect of Plant-Based Nutrition Diets on Plasma Lipids Profile—A Study Case in Romania
Abstract
:1. Introduction
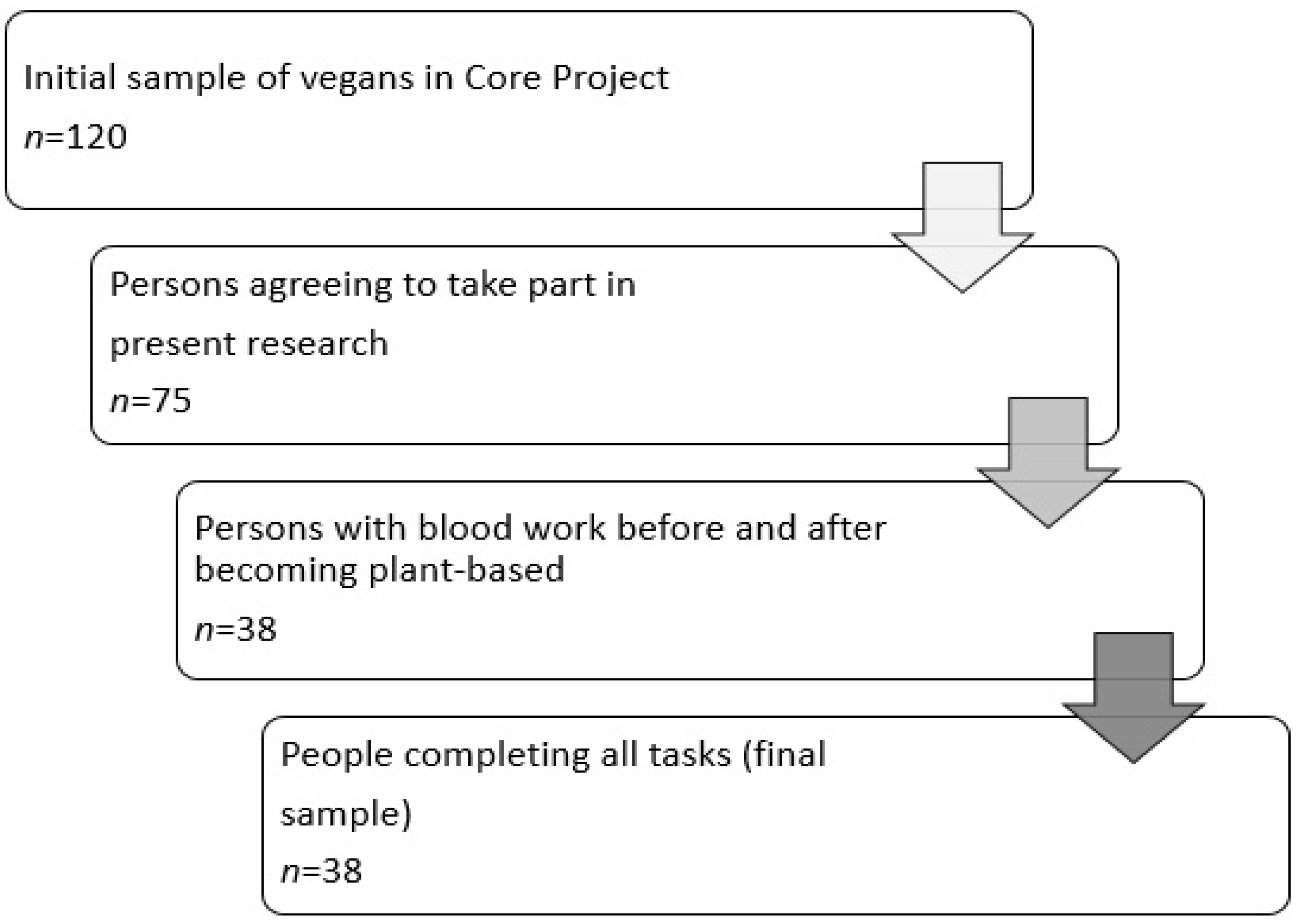
2. Materials and Methods
- 1.
- Lipid profile was defined based on the serum lipoproteins, considering the following as reference values:
- -
- TGs: optimal < 150 mg/dL (0); borderline elevated 150–199 mg/dL (1), elevated 200–499 mg/dL (2), very elevated ≥ 500 mg/dL (3)
- -
- TC: optimal < 200 mg/dL (0), borderline elevated 200–240 mg/dL (1), elevated ≥ 240 mg/dL (2)
- -
- HDL-C: low ≤ 40 mg/dL (2), normal > 40 mg/dL (1), protective > 60 mg/dL (0)
- -
- LDL-C: optimal < 100 mg/dL (0), optimal at the limit = 100–129 mg/dL (1), borderline elevated = 130–159 mg/dL (2), elevated = 160–189 mg/dL (3), very high ≥ 190 mg/dL (4)
- 2.
- The BMI was analyzed as a categorical variable, using four categories: Underweight (0) if BMI < 18.5, normal weight (1) if BMI = 18.5–24.9, overweight (pre-obese) (2) if BMI = 25–29.9, and obese (3) if BMI ≥ 30.
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nordestgaard, B.G. Triglyceride-Rich Lipoproteins and Atherosclerotic Cardiovascular Disease. Circ. Res. 2016, 118, 547–563. [Google Scholar] [CrossRef]
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W.; et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 140, e596–e646. [Google Scholar] [CrossRef] [PubMed]
- Bohîlțea, R.E.; Zugravu, C.A.; Neacsu, A.; Navolan, D.; Berceanu, C.; Nemescu, D.; Bodean, O.; Turcan, N.; Baros, A.; Cîrstoiu, M.M. The prevalence of Vitamin D deficiency and its obstetrical effects. A prospective study on Romanian patients. Rev. Chim. 2019, 70, 1228–1233. [Google Scholar] [CrossRef]
- Bohiltea, R.E.; Zugravu, C.A.; Nemescu, D.; Turcan, N.; Paulet, F.; Gherghiceanu, F.; Ducu, I.; Cirstoiu, M.M. Impact of obesity on the prognosis of hypertensive disorders in pregnancy. Exp. Ther. Med. 2020, 20, 2423–2428. [Google Scholar] [CrossRef] [PubMed]
- Grigoriu, C.; Furtunescu, F.; Gaman, L.E.; Balaceanu, A.L.; Buzatu, R.; Grigoriu, M.A. Biochemical Marker of Preeclampsia—Hypertriglyceridemia—And the Impact of Secondary Prevention Therapy. Rev. Chim. 2018, 69, 2740–2743. [Google Scholar] [CrossRef]
- Iordachescu, A.C.; Cirstoiu, M.M.; Zugravu, C.A.; Teodor, O.M.; Turcan, N.; Ducu, I.; Bohiltea, R.E. Dietary Behavior during Pregnancy. Exp. Ther. Med. 2020, 20, 2460–2464. [Google Scholar] [CrossRef] [PubMed]
- Key, T.; Davey, G. Prevalence of obesity is low in people who do not eat meat. BMJ 1996, 313, 816–817. [Google Scholar] [CrossRef] [Green Version]
- Pettersen, B.J.; Anousheh, R.; Fan, J.; Jaceldo-Siegl, K.; Fraser, G.E. Vegetarian diets and blood pressure among white subjects: Results from the Adventist Health Study-2 (AHS-2). Public Health Nutr. 2012, 15, 1909–1916. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sandu, C.; Bica, C.; Salmen, T.; Stoica, R.; Bohiltea, R.; Gherghiceanu, F.; Pacu, I.; Stefan, S.; Serafinceanu, C.; Stoian, A.P. Gestational diabetes-modern management and therapeutic approach (Review). Exp. Ther. Med. 2021, 21, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Tricopoulou, A.; Vasipoulou, E. Mediterran diet and longevity. Br. J. Nutr. 2000, 84, 205–209. [Google Scholar] [CrossRef]
- Patti, A.M.; Carruba, G.; Cicero, A.F.G.; Banach, M.; Nikolic, D.; Giglio, R.V.; Terranova, A.; Soresi, M.; Giannitrapani, L.; Montalto, G.; et al. Daily Use of Extra Virgin Olive Oil with High Oleocanthal Concentration Reduced Body Weight, Waist Circumference, Alanine Transaminase, Inflammatory Cytokines and Hepatic Steatosis in Subjects with the Metabolic Syndrome: A 2-Month Intervention Study. Metabolites 2020, 10, 392. [Google Scholar] [CrossRef] [PubMed]
- Barnard, N.D.; Scialli, A.R.; Bertron, P.; Hurlock, D.; Edmonds, K.; Talev, L. Effectiveness of a low-fat vegetarian diet in altering serum lipids in healthy premenopausal woman. Am. J. Cardiol 2000, 85, 969–972. [Google Scholar] [CrossRef]
- Cooper, R.S.; Goldberg, R.B.; Trevisan, M.; Tsong, Y.; Liu, K.; Stamler, J.; Rubenstein, A.; Scanu, A.M. The selective lipid-lowering effect of vegetarianism on low-density lipoproteins in a crossover experiment. Atherosclerosis 1982, 44, 293–305. [Google Scholar] [CrossRef]
- Dinu, M.; Pagliai, G.; Angelino, D.; Rosi, A.; Dall’Asta, M.; Bresciani, L.; Ferraris, C.; Guglielmetti, M.; Godos, J.; Del Bo’, C.; et al. Effects of Popular Diets on Anthropometric and Cardiometabolic Parameters: An Umbrella Review of Meta-Analyses of Randomized Controlled Trials. Adv. Nutr. 2020, 11, 815–833. [Google Scholar] [CrossRef] [PubMed]
- Harman, S.K.; Parnell, W.R. The nutritional health of New Zealand vegetarian and non-vegetarian Seventh-day Adventists: Selected vitamin, mineral and lipid levels. N. Z. Med. J. 1998, 111, 91–94. [Google Scholar] [PubMed]
- Key, T.J.; Davey, G.K.; Appleby, P.N. Health benefits of a vegetarian diet. Proc. Nutr. Soc. 1999, 58, 271–275. [Google Scholar] [CrossRef] [Green Version]
- Freeman, A.; Morris, P.; Barnard, N.; Esselstyn, C.; Ros, E.; Agatston, A.; Devries, S.; O’Keefe, J.; Miller, M.; Ornish, D.; et al. Trending Cardiovascular Nutrition Controversies. J. Am. Coll. Cardiol. 2017, 69, 1172–1187. [Google Scholar] [CrossRef] [PubMed]
- Cicero, A.F.G.; Fogacci, F.; Stoian, A.P.; Vrablik, M.; Al Rasadi, K.; Banach, M.; Toth, P.P.; Rizzo, M. Nutraceuticals in the Management of Dyslipidemia: Which, When, and for Whom? Could Nutraceuticals Help Low-Risk Individuals with Non-optimal Lipid Levels? Curr. Atheroscler. Rep. 2021, 23, 57. [Google Scholar] [CrossRef]
- Crismaru, I.; Stoian, A.P.; Bratu, O.G.; Gaman, M.A.; Stanescu, A.M.A.; Bacalbasa, N.; Diaconu, C.C. Low-density lipoprotein cholesterol lowering treatment: The current approach. Lipids Health Dis. 2020, 19, 85. [Google Scholar] [CrossRef]
- Gheorghe, G.; Toth, P.P.; Bungau, S.; Behl, T.; Ilie, M.; Pantea Stoian, A.; Bratu, O.G.; Bacalbasa, N.; Rus, M.; Diaconu, C.C. Cardiovascular Risk and Statin Therapy Considerations in Women. Diagnostics 2020, 10, 483. [Google Scholar] [CrossRef]
- Giglio, R.V.; Carruba, G.; Cicero, A.F.G.; Banach, M.; Patti, A.M.; Nikolic, D.; Cocciadiferro, L.; Zarcone, M.; Montalto, G.; Stoian, A.P.; et al. Pasta Supplemented with Opuntia ficus-indica Extract Improves Metabolic Parameters and Reduces Atherogenic Small Dense Low-Density Lipoproteins in Patients with Risk Factors for the Metabolic Syndrome: A Four-Week Intervention Study. Metabolites 2020, 10, 428. [Google Scholar] [CrossRef]
- Grigore-Gurgu, L. Genomics Era in the Nutrition Field. In The Annals of the University Dunarea De Jos of Galati. Fascicle VI—Food Technology; Galati University Press: Galati, Romania, 2018; Volume 42, pp. 168–174. [Google Scholar]
- Chang, S.L.; Lee, K.J.; Nfor, O.N.; Chen, P.H.; Lu, W.Y.; Ho, C.C.; Lung, C.C.; Chou, M.C.; Liaw, Y.P. Vegetarian Diets along with Regular Exercise: Impact on High-Density Lipoprotein Cholesterol Levels among Taiwanese Adults. Medicina 2020, 56, 74. [Google Scholar] [CrossRef] [Green Version]
- Allard-Ratick, P.; Sandesara, P.; Quyyumi, A.; Sperling, L. Everything in Moderation: Investigating the U-Shaped Link Between HDL Cholesterol and Adverse Outcomes. US Cardiol. Rev. 2019, 13, 49–53. [Google Scholar] [CrossRef]
- Keene, D.; Price, C.; Shun-Shin, M.J.; Francis, D.P. Effect on cardiovascular risk of high-density lipoprotein targeted drug treatments niacin, fibrates, and CETP inhibitors: Meta-analysis of randomized controlled trials including 117,411 patients. BMJ 2014, 349, 4379. [Google Scholar] [CrossRef] [Green Version]
- Hafiane, A.l.; Genest, J. High density lipoproteins: Measurement techniques and potential biomarkers of cardiovascular risk. BBA Clin. 2015, 3, 175–188. [Google Scholar] [CrossRef] [Green Version]
- Ebtehaj, S.; Gruppen, E.G.; Bakker, S.J.L.; Dullaart, R.P.F.; Tietge, U.J.F. HDL (High-Density Lipoprotein) Cholesterol Efflux Capacity Is Associated with Incident Cardiovascular Disease in the General Population. Arterioscler. Thromb. Vasc. 2019, 39, 1874–1883. [Google Scholar] [CrossRef]
- Turner-McGrievy, G.M.; Davidson, C.R.; Wingard, E.E.; Wilcox, S.; Frongillo, E.A. Comparative effectiveness of plant-based diets for weight loss: A randomized controlled trial of five different diets. Nutrition 2015, 31, 350–358. [Google Scholar] [CrossRef] [PubMed]
- Tran, E.; Dale, H.F.; Jensen, C.; Lied, G.A. Effects of Plant-Based Diets on Weight Status: A Systematic Review. Diabetes Metab. Syndr. Obes. 2020, 13, 3433–3448. [Google Scholar] [CrossRef]
- Pedersen, L.R.; Olsen, R.H.; Anholm, C.; Walzem, R.L.; Fenger, M.; Eugen-Olsen, J.; Haugaard, S.B.; Prescott, E. Weight loss is superior to exercise in improving the atherogenic lipid profile in a sedentary, overweight population with stable coronary artery disease: A randomized trial. Atherosclerosis 2016, 246, 221–228. [Google Scholar] [CrossRef]
- Koeth, R.A.; Wang, Z.; Levison, B.S.; Buffa, J.A.; Org, E.; Sheehy, B.T.; Britt, E.B.; Fu, X.; Wu, Y.; Li, L.; et al. Intestinal microbiota metabolism of L-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat. Med. 2013, 19, 576–585. [Google Scholar] [CrossRef] [Green Version]
- Nordestgaard, B.G.; Tybjaerg-Hansen, A.; Lewis, B. Influx in vivo of low density, intermediate density, and very low-density lipoproteins into aortic intimas of genetically hyperlipidemic rabbits. Roles of plasma concentrations, extent of aortic lesion, and lipoprotein particle size as determinants. Arterioscler. Thromb. 1992, 12, 6–18. [Google Scholar] [CrossRef] [Green Version]
- Yokoyama, Y.; Levin, S.M.; Barnard, N.D. Association between plant-based diets and plasma lipids: A systematic review and meta-analysis. Nutr. Rev. 2017, 75, 683–698. [Google Scholar] [CrossRef] [PubMed]
- Storz, M.A. Is There a Lack of Support for Whole-Food, Plant-Based Diets in the Medical Community? Perm J. 2018, 23, 18–068. [Google Scholar] [CrossRef] [PubMed]
- Fraser, G.E. Vegetarian diets: What do we know of their effects on common chronic diseases? Am. J. Clin. Nutr. 2009, 89, 1607S–1612S. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matsumoto, S.; Beeson, W.L.; Shavlik, D.J.; Siapco, G.; Jalcedo-Siegl, K.; Fraser, G.; Knutsen, S. Association between vegetarian diets and cardiovascular risk factors in non-Hispanic white participants of the Adventist Health Study-2. J. Nutr. Sci. 2019, 8, e6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Glenn Andrea, J.; Viguiliouk, E.; Seider, M.; Boucher, B.A.; Khan Tauseef, A.; Blanco, M.S.; Jenkins, D.J.A.; Kahleová, H.; Rahelić, D.; Salas-Salvadó, J.; et al. Relation of Vegetarian Dietary Patterns with Major Cardiovascular Outcomes: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. Front. Nutr. 2019, 6, 80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Campbell, E.K.; Fidahusain, M.; Campbell, T.M. Evaluation of an Eight-Week Whole-Food Plant-Based Lifestyle Modification Program. Nutrients 2019, 11, 2068. [Google Scholar] [CrossRef] [Green Version]
- Jingxuan, Q.; Grace, L.; Hui, L.M.; Han, N.; Zheng, S.W.; Jonathan, T. The Association of Plant-Based Diet with Cardiovascular Disease and Mortality: A Meta-Analysis and Systematic Review of Prospect Cohort Studies. Front. Cardiovasc. Med. 2021, 8, 1389. [Google Scholar]
- Benatar, J.R.; Stewart, R.A.H. Cardiometabolic risk factors in vegans; A meta-analysis of observational studies. PLoS ONE 2018, 13, e0209086. [Google Scholar]
- Zugravu, C.; Macri, A.; Belc, N.; Bohiltea, R. Efficacy of supplementation with methylcobalamin and cyancobalamin in maintaining the level of serum holotranscobalamin in a group of plant-based diet (vegan) adults. Exp. Ther. Med. 2021, 22, 993. [Google Scholar] [CrossRef]
| Variable | Men (Mean Value) | Women (Mean Value) |
|---|---|---|
| BMI 1 (kg/m2) | 22.3 | 23.0 |
| BMI 2 (kg/m2) | 21.2 | 22.2 |
| p | 0.001 | 0.006 |
| TG 1 (mg/dL) | 117.6 | 117.9 |
| TG 2 (mg/dL) | 104.3 | 102.6 |
| p | 0.003 | 0.005 |
| TC 1(mg/dL) | 0.186.5 | 203.4 |
| TC 2 (mg/dL) | 152.9 | 168.3 |
| p | 0.000 | 0.000 |
| HDL-C 1(mg/dL) | 45.0 | 48.2 |
| HDL-C 2(mg/dL) | 43.7 | 47.4 |
| 0.338 | 0.530 | |
| LDL-C 1 (mg/dL) | 133.3 | 143.5 |
| LDL-C 2 (mg/dL) | 99.0 | 108.9 |
| p | 0.000 | 0.000 |
| TC/HDL-C 1 | 4.1 | 4.2 |
| TC/HDL-C 2 | 3.5 | 3.5 |
| p | 0.000 | 0.000 |
| HDL-C 2 Category | ||||
|---|---|---|---|---|
| Normal | Low | Protective | ||
| HDL-C 1 category | normal | 17.6% | 82.4% | - |
| low | 93.8% | 6.2% | - | |
| protective | 50.0% | - | 50.0% | |
| TG 2 Category | |||
|---|---|---|---|
| Normal | Borderline Elevated | ||
| TG 1 category | normal | 100% | - |
| borderline elevated | 75% | 25% | |
| TC 2 Category | ||||
|---|---|---|---|---|
| Optimal | Borderline Elevated | Elevated | ||
| TC 1 category | optimal | 100% | - | - |
| borderline elevated | 100% | - | - | |
| elevated | 30% | 40% | 30% | |
| LDL-C 2 Category | ||||||
|---|---|---|---|---|---|---|
| Optimal | Borderline Optimal | Borderline Elevated | Elevated | Very Elevated | ||
| LDL-C 1 category | optimal | 100% | - | - | - | - |
| borderline optimal | 83.8% | 16.2% | - | - | - | |
| borderline elevated | 72.7% | 18.2% | - | 9.1% | - | |
| elevated | - | 66.7% | 33.3% | - | - | |
| very elevated | - | - | 66.7% | 11.1% | 22.2% | |
| TC/HDL-C 2 | ||||
|---|---|---|---|---|
| Ideal | Optimum | Increased | ||
| TC/HDL-C 1 | Ideal | 100% | - | - |
| Optimum | 62.5% | 25.0% | 12.5% | |
| increased | 7.1% | 78.6% | 14.3% | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zugravu, C.A.; Otelea, M.R.; Vladareanu, R.; Grigoriu, C.; Salmen, T.; Manolache, F.A.; Bohiltea, R.E. The Effect of Plant-Based Nutrition Diets on Plasma Lipids Profile—A Study Case in Romania. Sustainability 2022, 14, 1008. https://doi.org/10.3390/su14021008
Zugravu CA, Otelea MR, Vladareanu R, Grigoriu C, Salmen T, Manolache FA, Bohiltea RE. The Effect of Plant-Based Nutrition Diets on Plasma Lipids Profile—A Study Case in Romania. Sustainability. 2022; 14(2):1008. https://doi.org/10.3390/su14021008
Chicago/Turabian StyleZugravu, Corina Aurelia, Marina Ruxandra Otelea, Radu Vladareanu, Corina Grigoriu, Teodor Salmen, Fulvia Ancuta Manolache, and Roxana Elena Bohiltea. 2022. "The Effect of Plant-Based Nutrition Diets on Plasma Lipids Profile—A Study Case in Romania" Sustainability 14, no. 2: 1008. https://doi.org/10.3390/su14021008
APA StyleZugravu, C. A., Otelea, M. R., Vladareanu, R., Grigoriu, C., Salmen, T., Manolache, F. A., & Bohiltea, R. E. (2022). The Effect of Plant-Based Nutrition Diets on Plasma Lipids Profile—A Study Case in Romania. Sustainability, 14(2), 1008. https://doi.org/10.3390/su14021008








