Romanian Dentists’ Perception of Legal Liability Related to COVID-19 Infection during Dental Treatments in Times of the Pandemic Outbreak
Abstract
:1. Introduction
1.1. Urgent and Routine Dental Care
1.2. Legal Provisions and Immunity
1.3. Research Focus
2. Materials and Methods
2.1. Survey Instrument
- To explore dentists’ and managers’ knowledge about dental liability related to the COVID-19 pandemic (first dimension, A1–A5 in Table 1);
- To inquire about the respondents’ perceptions of immunity to prejudices resulting from non-urgent dental procedures during the COVID-19 pandemic (second dimension, B1 in Table 1);
- To assess respondents’ “good faith” in handling challenges in the pandemic context (third dimension, C1 and C2 in Table 1).
2.2. Study Setting and Participants
2.3. Data Analysis
3. Results
3.1. Respondents’ Profile
3.2. Knowledge about Dental Liability Related to COVID-19 Pandemic
3.3. Perception of Immunity
3.4. “Good Faith” in Handling COVID-19 Challenges
4. Discussion
4.1. Dental Liability Related to the COVID-19 Pandemic
4.2. COVID-19 Pandemic and Immunity
- (a)
- working conditions, insufficient diagnostic and treatment equipment, nosocomial infections, adverse effects, complications, and generally accepted risks of methods of investigation and treatment, hidden defects in sanitary ware, in medical equipment and devices, in medical substances and sanitary ware they used.
- (b)
- when they act in good faith in emergencies, respecting their competencies.
4.3. “Good Faith” in Handling COVID-19 Challenges
4.4. Study’s Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| % | percentage |
| CI | confidence interval |
| COVID-19 | coronavirus disease 2019 |
| e.g. | example |
| n | absolute frequency |
| no. | number |
| Q | quartile (Q1 is the first quartile, Q3 is the third quartile) |
| SD | standard deviation |
| U.K. | United Kingdom |
| U.S.A. | United States of America |
| WHO | World Health Organization |
References
- Peng, X.; Xu, X.; Li, Y.; Cheng, L.; Zhou, X.; Ren, B. Transmission routes of 2019-nCoV and controls in dental practice. Int. J. Oral Sci. 2020, 12, 9. [Google Scholar] [CrossRef] [PubMed]
- Wax, R.S.; Christian, M.D. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can. J. Anesth. 2020, 67, 568–576. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guo, Y.-R.; Cao, Q.-D.; Hong, Z.-S.; Tan, Y.-Y.; Chen, S.-D.; Jin, H.-J.; Tan, K.-S.; Wang, D.-Y.; Yan, Y. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak—An update on the status. Mil. Med. Res. 2020, 7, 11. [Google Scholar] [CrossRef] [Green Version]
- Military Ordinance 1 from March 17, 2020, on First Aid Measures Concerning Overcrowding and the Cross-Border Movement of Goods] [In Romanian]. Official Monitor 219/18 March 2020. Available online: https://legislatie.just.ro/Public/DetaliiDocument/223888 (accessed on 15 March 2022).
- Ministry of Health Order no. 828/May 15, 2020, on Measures to Organize and Carry out the Activity at Dental Offices and Non-COVID Health Units, during the Alert State] [in Romanian]. Official Monitor no. 437/25 May 2020. Available online: https://legislatie.just.ro/Public/DetaliiDocument/225830 (accessed on 15 March 2022).
- World Health Organization (WHO). Considerations for the Provision of Essential Oral Health Services in the Context of COVID-19. Interim Guidance. 3 August 2020. Available online: https://www.who.int/publications/i/item/who-2019-nCoV-oral-health-2020.1 (accessed on 15 February 2022).
- Elzein, R.; Bader, B.; Rammal, A.; Husseini, H.; Jassar, H.; Al-Haidary, M.; Saadeh, M.; Ayoub, F. Legal liability facing COVID-19 in dentistry: Between malpractice and preventive recommendations. J. Forensic Leg. Med. 2021, 78, 102123. [Google Scholar] [CrossRef]
- American Dental Association (ADA). What Constitutes a Dental Emergency? Available online: https://www.fachc.org/assets/ADA_COVID19_Dental_Emergency_DDS.pdf (accessed on 15 February 2022).
- Lo Giudice, R. The Severe Acute Respiratory Syndrome Coronavirus-2 (SARS CoV-2) in Dentistry. Management of Biological Risk in Dental Practice. Int. J. Environ. Res. Public Health 2020, 17, 3067. [Google Scholar] [CrossRef]
- Jiang, C.M.; Duangthip, D.; Auychai, P.; Chiba, M.; Folayan, M.O.; Hamama, H.H.H.; Kamnoedboon, P.; Lyons, K.; Matangkasombut, O.; Mathu-Muju, K.R.; et al. Changes in Oral Health Policies and Guidelines During the COVID-19 Pandemic. Front. Oral. Health 2021, 2, 668444. [Google Scholar] [CrossRef]
- Deana, N.F.; Seiffert, A.; Aravena-Rivas, Y.; Alonso-Coello, P.; Muñoz-Millán, P.; Espinoza-Espinoza, G.; Pineda, P.; Zaror, C. Recommendations for Safe Dental Care: A Systematic Review of Clinical Practice Guidelines in the First Year of the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 10059. [Google Scholar] [CrossRef] [PubMed]
- Benahmed, A.G.; Gasmi, A.; Anzar, W.; Arshad, M.; Bjørklund, G. Improving safety in dental practices during the COVID-19 pandemic. Health Technol. 2022, 12, 205–214. [Google Scholar] [CrossRef] [PubMed]
- Madathil, S.; Siqueira, W.L.; Marin, L.M.; Sanaulla, F.B.; Faraj, N.; Quiñonez, C.R.; McNally, M.; Glogauer, M.; Allison, P. The incidence of COVID-19 among dentists practicing in the community in Canada. A prospective cohort study over a 6-month period. J. Am. Dent. Assoc. 2022, 153, 450–459.e1. [Google Scholar] [CrossRef]
- Araujo, M.W.; Estrich, C.G.; Mikkelsen, M.; Morrissey, R.; Harrison, B.; Geisinger, M.L.; Ioannidou, E.; Vujicic, M. COVID-2019 among dentists in the United States: A 6-month longitudinal report of accumulative prevalence and incidence. J. Am. Dent. Assoc. 2021, 152, 425–433. [Google Scholar] [CrossRef]
- Jungo, S.; Moreau, N.; Mazevet, M.E.; Ejeil, A.-L.; Biosse Duplan, M.; Salmon, B.; Smail-Faugeron, V. Prevalence and risk indicators of first-wave COVID-19 among oral health-care workers: A French epidemiological survey. PLoS ONE 2021, 16, e0246586. [Google Scholar] [CrossRef] [PubMed]
- Gholami, M.; Fawad, I.; Shadan, S.; Rowaiee, R.; Ghanem, H.; Hassan Khamis, A.; Ho, S.B. COVID-19 and healthcare workers: A systematic review and meta-analysis. Int. J. Infect. Dis. 2021, 104, 335–346. [Google Scholar] [CrossRef] [PubMed]
- Sabetian, G.; Moghadami, M.; Hashemizadeh Fard Haghighi, L.; Shahriarirad, R.; Fallahi, M.J.; Asmarian, N.; Moeini, Y.S. COVID-19 infection among healthcare workers: A cross-sectional study in southwest Iran. Virol. J. 2021, 18, 58. [Google Scholar] [CrossRef]
- Law no. 95/2006 on Health Reform] [in Romanian] First Version Published in the Official Monitor no. 372/2006. Available online: https://legislatie.just.ro/Public/DetaliiDocument/80870 (accessed on 5 March 2022).
- Merriam-Webster’s Dictionary of Law ©1996. Merriam-Webster, Incorporated. Published under License with Merriam-Webster, Incorporated. Available online: https://dictionary.findlaw.com/definition/good-faith.html (accessed on 15 March 2022).
- Zolynski, C. La bonne foi en droit d’auteur. Cah. Droit. Sci. Technol. 2015, 5, 307–309. [Google Scholar] [CrossRef]
- Law NO. 287/2009—Civil Law Act. First Version Published in the Official Monitor NO. 511/2009. Available online: https://legislatie.just.ro/Public/DetaliiDocument/162242 (accessed on 15 March 2022).
- American Medical Association. Liability Protections for Health Care Professionals during COVID-19 (2020). Available online: https://www.ama-assn.org/practice-management/sustainability/liability-protections-health-care-professionals-during-covid-19 (accessed on 20 March 2022).
- Duignan, K.; Bradbury, C. COVID-19 and medical negligence litigation: Immunity for healthcare professionals? Med. Leg. J. 2020, 88 (Suppl. 1), 31–34. [Google Scholar] [CrossRef] [PubMed]
- Malla, C.; Anderson, A. Indemnity for Healthcare Professionals in Respect of COVID-19 Claims: A Global Perspective. Available online: https://kennedyslaw.com/thought-leadership/article/indemnity-for-healthcare-professionals-in-respect-of-covid-19-claims-a-global-perspective/ (accessed on 15 March 2022).
- Choctaw, W.T. Avoiding Medical Malpractice: A Physician’s Guide to the Law; Springer: New York, NY, USA, 2008; pp. 63–73. [Google Scholar]
- Tanaka, H.; Kurita, H.; Shibuya, Y.; Chikazu, D.; Iino, M.; Hoshi, K.; Kobayashi, W.; Yokoo, S.; Kawano, K.; Mitsudo, K.; et al. COVID-19 transmission in dental and oral/maxillofacial surgical practice during pandemic: Questionnaire survey in 51 university hospitals in Japan. J. Hosp. Infect. 2022, 125, 21–27. [Google Scholar] [CrossRef]
- Nardone, M.; Cordone, A.; Petti, S. Occupational COVID-19 risk to dental staff working in a public dental unit in the outbreak epicenter. Oral Dis. 2022, 28 (Suppl. 1), 878–890. [Google Scholar] [CrossRef]
- Kathree, B.A.; Khan, S.B.; Ahmed, R.; Maart, R.; Layloo, N.; Asia-Michaels, W. COVID-19 and its impact in the dental setting: A scoping review. PLoS ONE 2020, 15, e0244352. [Google Scholar] [CrossRef]
- Estrich, C.G.; Gurenlian, J.R.; Battrell, A.; Lynch, A.; Mikkelsenm, M.; Morrissey, R.W.; Vujicic, M.; Araujo, M.W.B. Infection Prevention and Control Practices of Dental Hygienists in the United States During the COVID-19 Pandemic: A longitudinal study. J. Dent. Hyg. 2022, 96, 17–26. [Google Scholar]
- Basheer, S.N.; Vinothkumar, T.S.; Albar, N.H.M.; Karobari, M.I.; Renugalakshmi, A.; Bokhari, A.; Peeran, S.W.; Peeran, S.A.; Alhadri, L.M.; Tadakamadla, S.K. Knowledge of COVID-19 Infection Guidelines among the Dental Health Care Professionals of Jazan Region, Saudi Arabia. Int. J. Environ. Res. Public Health 2022, 19, 2034. [Google Scholar] [CrossRef]
- Thurzo, A.; Urbanová, W.; Waczulíková, I.; Kurilová, V.; Mriňáková, B.; Kosnáčová, H.; Gális, B.; Varga, I.; Matajs, M.; Novák, B. Dental Care and Education Facing Highly Transmissible SARS-CoV-2 Variants: Prospective Biosafety Setting: Prospective, Single-Arm, Single-Center Study. Int. J. Environ. Res. Public Health 2022, 19, 7693. [Google Scholar] [CrossRef] [PubMed]
- Centers for Diseases Control and Prevention. Available online: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/how-covid-spreads.html (accessed on 15 March 2022).
- Banakar, M.; Bagheri Lankarani, K.; Jafarpour, D.; Moayedi, S.; Banakar, M.H.; MohammadSadeghi, A. COVID-19 transmission risk and protective protocols in dentistry: A systematic review. BMC Oral Health 2020, 20, 275. [Google Scholar] [CrossRef] [PubMed]
- Spagnuolo, G.; De Vito, D.; Rengo, S.; Tatullo, M. COVID-19 Outbreak: An Overview on Dentistry. Int. J. Environ. Res. Public Health 2020, 17, 2094. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kampf, G.; Todt, D.; Pfaender, S.; Steinmann, E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J. Hosp. Infect. 2020, 104, 246–251. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gonçalves, J.; da Silva, P.G.; Reis, L.; Nascimento, M.S.J.; Koritnik, T.; Paragi, M.; Mesquita, J.R. Surface contamination with SARS-CoV-2: A systematic review. Sci. Total Environ. 2021, 798, 149231. [Google Scholar] [CrossRef]
- Glinert, I.; Ben-Shmuel, A.; Szwartcwort-Cohen, M.; Beth-din, A.; Laskar, O.; Barlev-Gross, M.; Melamed, S.; Arbell, N.; Levy, H.; Horowitz, N.A.; et al. Revisiting SARS-CoV-2 environmental contamination by patients with COVID-19: The Omicron variant does not differ from previous strains. J. Infect. Dis. Med. 2022, 118, 211–213. [Google Scholar] [CrossRef]
- Statute of the International Court of Justice. Available online: https://legal.un.org/avl/pdf/ha/sicj/icj_statute_e.pdf (accessed on 15 March 2022).
- Romanian High Court of Cassation and Justice. Civil Section. Decision 1927/2014. Available online: https://www.iccj.ro/ (accessed on 15 March 2022).
- Law no. 134/2010 revised [Civil Procedure Code] [in Romanian]. Official Monitor no. 247/2015. Available online: https://legislatie.just.ro/Public/DetaliiDocumentAfis/140265 (accessed on 27 February 2022).
- Deery, C. The legal position of delivering dental care in a time of COVID-19. Evid. -Based Dent. 2021, 22, 84. [Google Scholar] [CrossRef]
- Klitzman, R.L. Legal Immunity for Physicians During the COVID-19 Pandemic: Needs to Address Legal and Ethical Challenges. Chest 2020, 158, 1343–1345. [Google Scholar] [CrossRef]
- Teo, W.; Brenner, L.H.; Bal, B.S. Medicolegal Sidebar: Legal Immunity for Healthcare Workers During COVID-19. Clin. Orthop. Relat. Res. 2020, 478, 2218–2220. [Google Scholar] [CrossRef]
- Tomkins, C.; Purshouse, C.; Heywood, R.; Miola, J.; Cave, E.; Devaney, S. Should doctors tackling COVID-19 be immune from negligence liability claims? BMJ 2020, 370, m2487. [Google Scholar] [CrossRef]
- Griffith, R. Duty, indemnity and immunity during the COVID-19 pandemic. Br. J. Nurs. 2020, 29, 537–538. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Infection Prevention & Control in Dental Settings. Available online: https://www.cdc.gov/oralhealth/infectioncontrol/index.html (accessed on 10 June 2022).
- European Center for Disease Prevention and Control. COVID-19 Infection Prevention and Control Measures for Primary Care, Including General Practitioner Practices, Dental Clinics and Pharmacy Settings: First Update. Available online: https://www.ecdc.europa.eu/en/publications-data/covid-19-infection-prevention-and-control-primary-care (accessed on 8 June 2022).
- COVID-19: Infection Prevention and Control Dental Appendix (Guidance Withdrawn on 27 May 2022). Available online: https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control/covid-19-infection-prevention-and-control-dental-appendix (accessed on 10 June 2022).
- Infection Prevention and Control & Oral Health Care during the COVID-19 Pandemic. Available online: https://www.cdsbc.org/Documents/covid-19/COVID-19-IPAC-Oral-Health-Care-Dec-2021.pdf (accessed on 10 June 2022).
- Amato, A.; Caggiano, M.; Amato, M.; Moccia, G.; Capunzo, M.; De Caro, F. Infection Control in Dental Practice During the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 4769. [Google Scholar] [CrossRef] [PubMed]
- Chance, I.R.; Strange, M. What to do When Dentist Thinks COVID is a ‘Joke’. Available online: https://www.dentistryiq.com/dentistry/article/14187100/what-to-do-when-dentist-thinks-covid-is-a-joke (accessed on 27 February 2022).
- Royal College of Dental Surgeons of Ontario, COVID-19: Managing Infection Risks during in-Person Dental Care, Updated September 2021. Available online: https://www.rcdso.org/en-ca/rcdso-members/2019-novel-coronavirus/covid-19--managing-infection-risks-during-in-person-care (accessed on 8 June 2022).
- California Dental Association, Patient Communication and Management, March 2022. Available online: https://www.cda.org/Home/Resource-Library/Resources/category/patients/patient-communication-and-management (accessed on 8 June 2022).
| Dimension | Questions |
|---|---|
| A1.* In the last two years, have you ever thought that patients might complain about being infected with COVID-19 during their visits for dental treatment? Yes/No A2.** To whom should a person address a complaint regarding a possible COVID-19 infection in a dental office/clinic? (a) College of Dentistry, (b) Public Health Authority, (c) Courts, (d) Dental office/clinic where they have been treated, (e) I do not know, (f) Other institution (specify) A3.** Against whom do you consider they should complain? (a) Against dentists, (b) Against the clinic/office management, (c) Against sanitary and pharmaceutical products providers, (d) I do not know, (e) Other institution (specify) A4.** Who is the most susceptible to be responsible for COVID-19 infection of patients in dentistry? (a) The dentist who performed the dental care, (b) Clinic/Office Administration, (c) Dentist/Office/Clinic Malpractice Insurance, (d) I do not know, (e) Other institution (specify) A5.* Who should prove that COVID-19 infection is caused at the dental clinic/office visits? (a) The dentist/dental clinic/office management, (b) Medical Malpractice experts, (c) Patients, (d) I do not know, (e) Other institution (specify) |
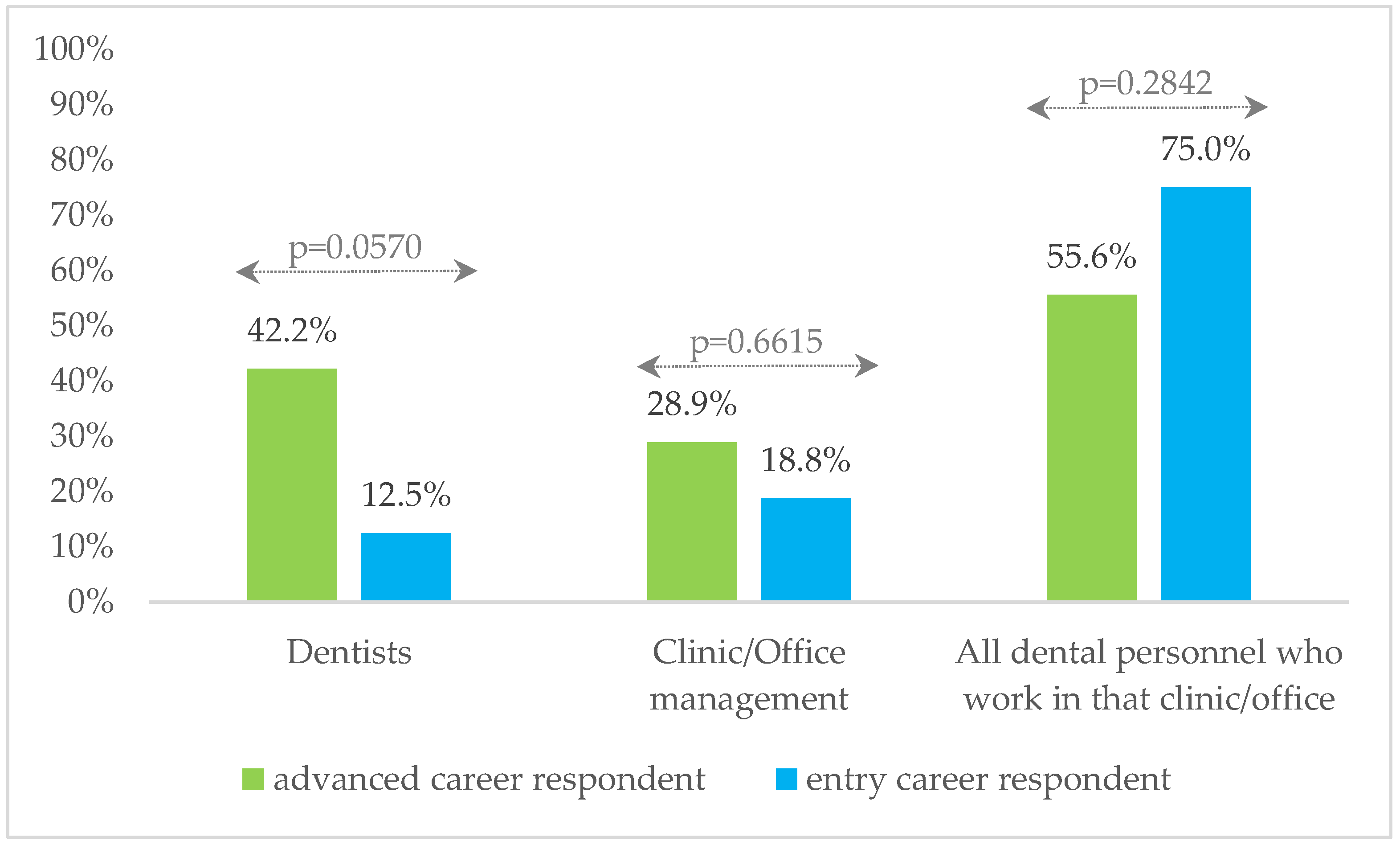
| B1.* If the State/Health Ministry would decide in favor of legal immunity during the COVID-19 pandemic, who should benefit? (a) Dentists, (b) Clinic/Office management, (c) All dental personnel who work in that clinic/office, (d) I do not know, (e) Other opinions (specify) |
| C1.** In the event of such complaints, the cause could be the failure to implement/respect the safety measures and protocols specific to the pandemic context: (a) Dentists, (b) Clinic/Office management, (c) Patient, (d) I do not know, (e) Other institution (specify) C2.** Protocols and pandemic-specific safety measures had NOT always been possible because of: (a) Patient flow, (b) Costs/financial pressure on the clinic/office, (c) Patients’ reluctance/refusal to follow protocols, (d) I do not know, (e) Other reason (specify) |
| Variable | Statistics | |
|---|---|---|
| Gender | Female, n (%) Male, n (%) | 47 (77.0) 14 (23.0) |
| Age, years | Median (Q1–Q3) Mean (SD) | 31.5 (28–37) 33.3 (6.5) |
| Years of experience | Median (Q1–Q3) Mean (SD) | 5 (2–11) 7.9 (7.8) |
| Dental specialty Dento-alveolar surgeon Dental and maxillofacial surgeon Endodontics Orthodontics Periodontics Prosthodontics Pediatric dentistry General dentistry | n (%) | 10 (16.4) 7 (11.5) 2 (3.3) 11 (18.0) 6 (9.8) 4 (6.6) 7 (11.5) 20 (32.8) |
| Status in the institution Administrative manager Medical manager Dentist Other | n (%) | 5 (8.2) 8 (13.1) 37 (60.7) 11 (18.0) |
| Question | Answer Options | n (%) |
|---|---|---|
| A1 | Yes No | 44 (72.1) 17 (27.9) |
| A2 | (a) College of Dentistry (b) County Public Health Directorate (c) Courts (d) Dental office/clinic where they have been treated (e) I do not know (f) Other institution | 19 (31.1) 41 (67.2) 2 (3.3) 30 (49.2) 2 (3.3) 3 (4.9) |
| A3 | (a) Against dentist (b) Against the clinic/office management (c) Against sanitary and pharmaceutical products providers (d) I do not know (e) Other institution | 19 (31.1) 43 (70.5) 7 (11.5) 6 (9.8) 0 (0.0) |
| A4 | (a) The dentist who performed the dental care (b) Clinic/office Administration (c) Dentist/Office/Clinic Malpractice Insurance (d) I do not know (e) Other institution | 30 (49.2) 34 (55.7) 8 (13.1) 12 (19.7) 0 (0.0) |
| A5 | (a) The dentist/dental clinic/office management (b) Medical Malpractice experts (c) Patients (d) I do not know (e) Other institution | 6 (9.8) 25 (41.0) 36 (59.0) 4 (6.6) 2 (3.3) * |
| Question | Answer Options | n (%) |
|---|---|---|
| B1 | (a) Dentists (b) Clinic/Office management (c) All dental personnel who work in that clinic/office (d) I do not know | 21 (34.4) 18 (29.5) 37 (60.7) 5 (8.2) |
| Question | Answer Options | n (%) |
|---|---|---|
| C1 | (a) Dentists (b) Clinic/Office management (c) Patient (d) I do not know (e) Other institution | 35 (57.4) 51 (83.6) 27 (44.3) 1 (1.6) 2 (3.3) |
| C2 | (a) Patient flow (b) Costs/financial pressure on the clinic/office (c) Patients’ reluctance/refusal to follow protocols (d) I do not know (e) Other reason | 21 (34.4) 35 (57.4) 29 (47.5) 7 (11.5) 3 (4.9) * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aluaș, M.; Bolboacă, S.D.; Mesaroș, A.-Ș.; Lucaciu, P.O. Romanian Dentists’ Perception of Legal Liability Related to COVID-19 Infection during Dental Treatments in Times of the Pandemic Outbreak. Sustainability 2022, 14, 9744. https://doi.org/10.3390/su14159744
Aluaș M, Bolboacă SD, Mesaroș A-Ș, Lucaciu PO. Romanian Dentists’ Perception of Legal Liability Related to COVID-19 Infection during Dental Treatments in Times of the Pandemic Outbreak. Sustainability. 2022; 14(15):9744. https://doi.org/10.3390/su14159744
Chicago/Turabian StyleAluaș, Maria, Sorana D. Bolboacă, Anca-Ștefania Mesaroș, and Patricia Ondine Lucaciu. 2022. "Romanian Dentists’ Perception of Legal Liability Related to COVID-19 Infection during Dental Treatments in Times of the Pandemic Outbreak" Sustainability 14, no. 15: 9744. https://doi.org/10.3390/su14159744
APA StyleAluaș, M., Bolboacă, S. D., Mesaroș, A.-Ș., & Lucaciu, P. O. (2022). Romanian Dentists’ Perception of Legal Liability Related to COVID-19 Infection during Dental Treatments in Times of the Pandemic Outbreak. Sustainability, 14(15), 9744. https://doi.org/10.3390/su14159744









