COVID-19 Burnout Subject to the Dynamic Zero-COVID Policy in Hong Kong: Development and Psychometric Evaluation of the COVID-19 Burnout Frequency Scale
Abstract
:1. Introduction
1.1. Dynamic Zero-COVID Strategy
1.2. “Pandemic Fatigue”
1.3. Pandemic Burnout Assessment
2. Materials and Methods
2.1. Study Design and Study Participants
2.2. Procedure
2.2.1. Phase 1: Development of the Scale
2.2.2. Phase 2: Validation of the Scale
3. Results
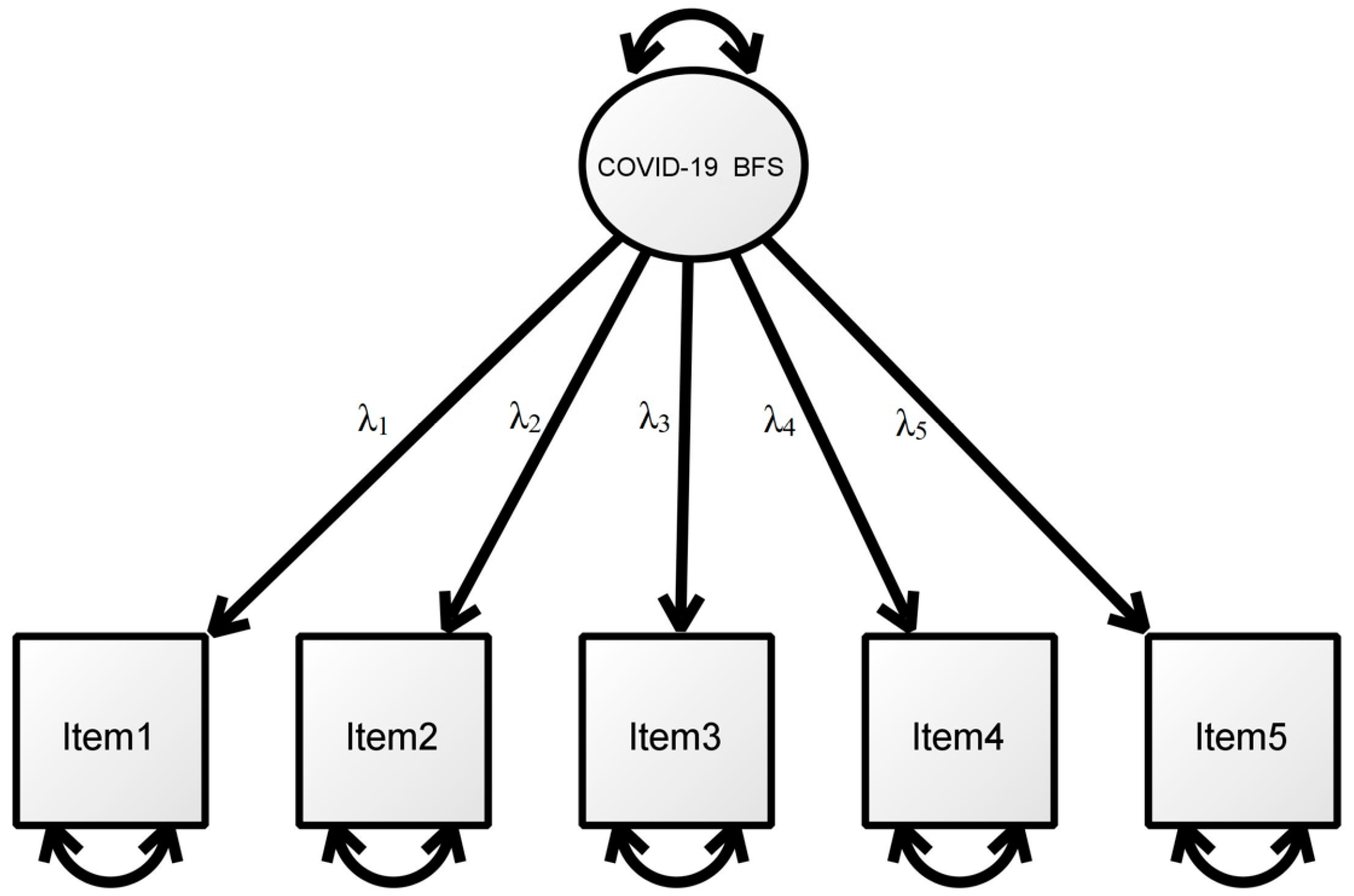
3.1. Factorial Validity of the COVID-19 Burnout Frequency Scale
3.2. Internal Consistency
3.3. Convergent and Concurrent Validity
4. Discussion
5. Limitations and Future Directions
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Burki, T. Dynamic zero COVID policy in the fight against COVID. Lancet Respir. Med. 2022, 10, e58–e59. [Google Scholar] [CrossRef]
- Haktanir, A.; Can, N.; Seki, T.; Kurnaz, M.F.; Dilmaç, B. Do we experience pandemic fatigue? current state, predictors, and prevention. Curr. Psychol. 2021, 1–12. [Google Scholar] [CrossRef]
- Tee, M.L.; Tee, C.A.; Anlacan, J.P.; Aligam, K.J.G.; Reyes, P.W.C.; Kuruchittham, V.; Ho, R.C. Psychological impact of COVID-19 pandemic in the Philippines. J. Affect. Disord. 2020, 277, 379–391. [Google Scholar] [CrossRef] [PubMed]
- McGinty, E.E.; Presskreischer, R.; Han, H.; Barry, C.L. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA 2020, 324, 93–94. [Google Scholar] [CrossRef]
- Galanis, P.; Vraka, I.; Fragkou, D.; Bilali, A.; Kaitelidou, D. Nurses’ burnout and associated risk factors during the COVID-19 pandemic: A systematic review and meta-analysis. J. Adv. Nurs. 2021, 77, 3286–3302. [Google Scholar] [CrossRef]
- Anastasiou, E.; Duquenne, M.-N. First-wave COVID-19 pandemic in Greece: The role of demographic, social, and geographical factors in life satisfaction during lockdown. Soc. Sci. 2021, 10, 186. [Google Scholar] [CrossRef]
- Lee, S.H.; Patel, P.C.; Phan, P.H. Are the self-employed more stressed? New evidence on an old question. J. Small Bus. Manag. 2020, 1–27. [Google Scholar] [CrossRef]
- Vindegaard, N.; Benros, M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef]
- Centre for Health Protection of the Department of Health. Latest situation of COVID-19 (as of 3 March 2022). 2022. Available online: https://www.chp.gov.hk/files/pdf/local_situation_covid19_en_20220303.pdf (accessed on 11 May 2022).
- Queen, D.; Harding, K. Societal pandemic burnout: A COVID legacy. Int. Wound J. 2020, 17, 873. [Google Scholar] [CrossRef]
- Gewin, V. Pandemic burnout is rampant in academia. Nature 2021, 591, 489–492. [Google Scholar] [CrossRef]
- Petherick, A.; Goldszmidt, R.; Andrade, E.B.; Furst, R.; Hale, T.; Pott, A.; Wood, A. A worldwide assessment of changes in adherence to COVID-19 protective behaviours and hypothesized pandemic fatigue. Nat. Hum. Behav. 2021, 5, 1145–1160. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; West, R.; Harvey, N. The concept of “fatigue” in tackling COVID-19. BMJ 2020, 371, m4171. [Google Scholar] [CrossRef] [PubMed]
- Murphy, J.F.A. Pandemic fatigue. Ir. Med. J. 2020, 113, 90. [Google Scholar] [PubMed]
- Zerbe, K.J. Pandemic fatigue: Facing the body’s inexorable demands in the time of COVID-19. J. Am. Psychoanal. Assoc. 2020, 68, 475–478. [Google Scholar] [CrossRef]
- Marcus, J. Quarantine fatigue is real. Atlantic 2020, 11. Available online: https://www.theatlantic.com/ideas/archive/2020/05/quarantine-fatigue-real-and-shaming-people-wont-help/611482/ (accessed on 24 June 2022).
- Harvey, N. Behavioral fatigue: Real phenomenon, naïve construct, or policy contrivance? Front. Psychol. 2020, 11, 589892. [Google Scholar] [CrossRef]
- World Health Organization. Pandemic Fatigue: Reinvigorating the Public to Prevent COVID-19; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Aaronson, L.S.; Teel, C.S.; Cassmeyer, V.; Neuberger, G.B.; Pallikkathayil, L.; Pierce, J.; Press, A.N.; Williams, P.D.; Wingate, A. Defining and measuring fatigue. Image J. Nurs. Scholarsh. 1999, 31, 45–50. [Google Scholar] [CrossRef]
- Ford, J.L.; Douglas, M.; Barrett, A.K. The role of pandemic fatigue in seeking and avoiding information on COVID-19 among young adults. Health Commun. 2022, 1–14. [Google Scholar] [CrossRef]
- Reicher, S.; Drury, J. Pandemic fatigue? How adherence to COVID-19 regulations has been misrepresented and why it matters. BMJ 2021, 372, n137. [Google Scholar] [CrossRef]
- Bartoszek, A.; Walkowiak, D.; Bartoszek, A.; Kardas, G. Mental well-being (depression, loneliness, insomnia, daily life fatigue) during COVID-19 related home-confinement—A study from Poland. Int. J. Environ. Res. Public Health 2020, 17, 7417. [Google Scholar] [CrossRef]
- Thagard, P. What is COVID Fatigue? Psychology Today. 2020. Available online: https://www.psychologytoday.com/us/blog/hot-thought/202011/what-is-covid-fatigue (accessed on 23 June 2022).
- Maslach, C.; Jackson, S.E. Maslach Burnout Inventory Manual, 2nd ed.; Consulting Psychologists Press: Palo Alto, CA, USA, 1986. [Google Scholar]
- Maslach, C.; Leiter, M.P. Understanding the burnout experience: Recent research and its implications for psychiatry. World Psychiatry 2016, 15, 103–111. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- mindhk. Pandemic Fatigue. 2022. Available online: https://www.mind.org.hk/wp-content/uploads/2022/03/EN-pandemic-fatigue-1.pdf (accessed on 10 April 2022).
- Dugas, M.J.; Hedayati, M.; Karavidas, A.; Buhr, K.; Francis, K.; Phillips, N.A. Intolerance of uncertainty and information processing: Evidence of biased recall and interpretations. Cogn. Ther. Res. 2005, 29, 57–70. [Google Scholar] [CrossRef]
- Azoulay, E.; De Waele, J.; Ferrer, R.; Staudinger, T.; Borkowska, M.; Povoa, P.; Iliopoulou, K.; Artigas, A.; Schaller, S.J.; Hari, M.S. Symptoms of burnout in intensive care unit specialists facing the COVID-19 outbreak. Ann. Intensive Care 2020, 10, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Pressley, T. Factors contributing to teacher burnout during COVID-19. Educ. Res. 2021, 50, 325–327. [Google Scholar] [CrossRef]
- Yıldırım, M.; Solmaz, F. COVID-19 burnout, COVID-19 stress and resilience: Initial psychometric properties of COVID-19 Burnout Scale. Death Stud. 2022, 46, 524–532. [Google Scholar] [CrossRef]
- Kristensen, T.S.; Borritz, M.; Villadsen, E.; Christensen, K.B. The Copenhagen Burnout Inventory: A new tool for the assessment of burnout. Work Stress 2005, 19, 192–207. [Google Scholar] [CrossRef]
- Talaee, N.; Varahram, M.; Jamaati, H.; Salimi, A.; Attarchi, M.; Sadr, M.; Hassani, S.; Farzanegan, B.; Monjazebi, F.; Seyedmehdi, S.M. Stress and burnout in health care workers during COVID-19 pandemic: Validation of a questionnaire. J. Public Health 2020, 30, 531–536. [Google Scholar] [CrossRef]
- Malach-Pines, A. The burnout measure, short version. Int. J. Stress Manag. 2005, 12, 78. [Google Scholar] [CrossRef]
- Chau, S.W.; Lewis, T.; Ng, R.; Chen, J.Y.; Farrell, S.M.; Molodynski, A.; Bhugra, D. Wellbeing and mental health amongst medical students from Hong Kong. Int. Rev. Psychiatry 2019, 31, 626–629. [Google Scholar] [CrossRef] [Green Version]
- Lam, L.T.; Lam, M.K.; Reddy, P.; Wong, P. Factors Associated with Work-Related Burnout among Corporate Employees Amidst COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 1295. [Google Scholar] [CrossRef]
- Ng, A.P.P.; Chin, W.Y.; Wan, E.Y.F.; Chen, J.; Lau, C.S. Prevalence and severity of burnout in Hong Kong doctors up to 20 years post-graduation: A cross-sectional study. BMJ Open 2020, 10, e040178. [Google Scholar] [CrossRef] [PubMed]
- Kwan, K.Y.; Chan, L.W.; Cheng, P.; Leung, G.K.; Lau, C. Burnout and well-being in young doctors in Hong Kong: A territory-wide cross-sectional survey. Hong Kong Med. J. 2021, 27, 330. [Google Scholar] [CrossRef] [PubMed]
- Low, Z.X.; Yeo, K.A.; Sharma, V.K.; Leung, G.K.; McIntyre, R.S.; Guerrero, A.; Lu, B.; Sin Fai Lam, C.C.; Tran, B.X.; Nguyen, L.H. Prevalence of burnout in medical and surgical residents: A meta-analysis. Int. J. Environ. Res. Public Health 2019, 16, 1479. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Woo, T.; Ho, R.; Tang, A.; Tam, W. Global prevalence of burnout symptoms among nurses: A systematic review and meta-analysis. J. Psychiatr. Res. 2020, 123, 9–20. [Google Scholar] [CrossRef] [PubMed]
- Shiu, C.; Chen, W.-T.; Hung, C.-C.; Huang, E.P.-C.; Lee, T.S.-H. COVID-19 stigma associates with burnout among healthcare providers: Evidence from Taiwanese physicians and nurses. J. Formos. Med. Assoc. 2021. [Google Scholar] [CrossRef]
- Meadows, K.; Bentzen, N.; Touw-Otten, F. Cross-cultural issues: An outline of the important principles in establishing cross-cultural validity in health outcome assessment. In Cross Cultural Health Outcome Assessment; A User’s, Guide; Hutchinson, A., Bentzen, N., König-Zahn, C., Eds.; European Research Group on Health Outcomes: Ruinen, The Netherlands, 1997; Volume I, pp. 34–40. [Google Scholar]
- Bradburn, N.M.; Sudman, S.; Wansink, B. Asking Questions: The Definitive Guide to Questionnaire Design—For Market Research, Political Polls, and Social and Health Questionnaires; John Wiley & Sons: Hoboken, NJ, USA, 2004. [Google Scholar]
- Fokkema, M.; Greiff, S. How performing PCA and CFA on the same data equals trouble: Overfitting in the assessment of internal structure and some editorial thoughts on it. Eur. J. Psychol. Assess. 2017, 33, 399–402. [Google Scholar] [CrossRef]
- Orçan, F. Exploratory and confirmatory factor analysis: Which one to use first? J. Meas. Eval. Educ. Psychol. 2018, 9, 414–421. [Google Scholar]
- Fung, S.-F.; Fung, A.L.C. Development and evaluation of the psychometric properties of a brief parenting scale (PS-7) for the parents of adolescents. PLoS ONE 2020, 15, e0228287. [Google Scholar] [CrossRef]
- Fung, S.-f.; Kong, C.Y.W.; Liu, Y.-m.; Huang, Q.; Xiong, Z.; Jiang, Z.; Zhu, F.; Chen, Z.; Sun, K.; Zhao, H. Validity and Psychometric Evaluation of the Chinese Version of the 5-Item WHO Well-Being Index. Front. Public Health 2022, 10, 872436. [Google Scholar] [CrossRef]
- Jin, J.; Fung, S.-F. Social physique anxiety scale: Psychometric evaluation and development of a Chinese adaptation. Int. J. Environ. Res. Public Health 2021, 18, 10921. [Google Scholar] [CrossRef]
- Schroeders, U.; Wilhelm, O.; Olaru, G. Meta-heuristics in short scale construction: Ant colony optimization and genetic algorithm. PLoS ONE 2016, 11, e0167110. [Google Scholar] [CrossRef] [PubMed]
- Fabrigar, L.R.; Wegener, D.T.; MacCallum, R.C.; Strahan, E.J. Evaluating the use of exploratory factor analysis in psychological research. Psychol. Methods 1999, 4, 272. [Google Scholar] [CrossRef]
- Fung, S.-F.; Chow, E.O.-W.; Cheung, C.-K. Development and validation of a brief self-assessed wisdom scale. BMC Geriatr. 2020, 20, 54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jennrich, R.I.; Sampson, P. Rotation for simple loadings. Psychometrika 1966, 31, 313–323. [Google Scholar] [CrossRef] [PubMed]
- Field, A. Discovering Statistics Using IBM SPSS Statistics; Sage: Thousand Oaks, CA, USA, 2013. [Google Scholar]
- Fung, S.-F.; Chow, E.O.-W.; Cheung, C.-K. Development and evaluation of the psychometric properties of a brief wisdom development scale. Int. J. Environ. Res. Public Health 2020, 17, 2717. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hair, J.F., Jr.; Black, W.C.; Babin, B.J.; Anderson, R.E. Multivariate Data Analysis, 7th ed.; Prentice Hall: Upper Saddle River, NJ, USA, 2009. [Google Scholar]
- Brown, T.A. Confirmatory Factor Analysis for Applied Research; Guilford Publications: New York, NY, USA, 2015. [Google Scholar]
- Jöreskog, K.G. A general approach to confirmatory maximum likelihood factor analysis. Psychometrika 1969, 34, 183–202. [Google Scholar] [CrossRef]
- DiStefano, C.; Morgan, G.B. A comparison of diagonal weighted least squares robust estimation techniques for ordinal data. Struct. Equ. Modeling Multidiscip. J. 2014, 21, 425–438. [Google Scholar] [CrossRef]
- Li, C.-H. Confirmatory factor analysis with ordinal data: Comparing robust maximum likelihood and diagonally weighted least squares. Behav. Res. Methods 2016, 48, 936–949. [Google Scholar] [CrossRef] [Green Version]
- Browne, M.W.; Cudeck, R. Alternative ways of assessing model fit. Sociol. Methods Res. 1992, 21, 230–258. [Google Scholar] [CrossRef]
- Hu, L.t.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Modeling Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Jebb, A.T.; Ng, V.; Tay, L. A review of key Likert scale development advances: 1995–2019. Front. Psychol. 2021, 12, 637547. [Google Scholar] [CrossRef] [PubMed]
- Schreiber, J.B.; Nora, A.; Stage, F.K.; Barlow, E.A.; King, J. Reporting structural equation modeling and confirmatory factor analysis results: A review. J. Educ. Res. 2006, 99, 323–338. [Google Scholar] [CrossRef]
- Bentler, P.M.; Bonett, D.G. Significance tests and goodness of fit in the analysis of covariance structures. Psychol. Bull. 1980, 88, 588. [Google Scholar] [CrossRef]
- Kline, R.B. Principles and Practice of Structural Equation Modeling; Guilford Publications: New York, NY, USA, 2015. [Google Scholar]
- Tabachnick, B.G.; Fidell, L.S.; Ullman, J.B. Using Multivariate Statistics; Pearson: Boston, MA, USA, 2007; Volume 5. [Google Scholar]
- McDonald, R.P. Test Theory: A Unified Treatment; Psychology Press: London, UK, 1999. [Google Scholar]
- Revelle, W.; Zinbarg, R.E. Coefficients alpha, beta, omega, and the glb: Comments on Sijtsma. Psychometrika 2009, 74, 145–154. [Google Scholar] [CrossRef]
- Cronbach, L.J. Coefficient alpha and the internal structure of tests. Psychometrika 1951, 16, 297–334. [Google Scholar] [CrossRef] [Green Version]
- Hinkin, T.R. A brief tutorial on the development of measures for use in survey questionnaires. Organ. Res. Methods 1998, 1, 104–121. [Google Scholar] [CrossRef]
- Ahorsu, D.K.; Lin, C.-Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The fear of COVID-19 scale: Development and initial validation. Int. J. Ment. Health Addict. 2020, 20, 1537–1545. [Google Scholar] [CrossRef] [Green Version]
- Yadav, U.N.; Yadav, O.P.; Singh, D.R.; Ghimire, S.; Rayamajhee, B.; Mistry, S.K.; Rawal, L.B.; Ali, A.M.; Tamang, M.K.; Mehta, S. Perceived fear of COVID-19 and its associated factors among Nepalese older adults in eastern Nepal: A cross-sectional study. PLoS ONE 2021, 16, e0254825. [Google Scholar] [CrossRef]
- Ligo, V.A.C.; Chang, C.M.; Yi, H. Contested solidarity and vulnerability in social media-based public responses to COVID-19 policies of mobility restrictions in Singapore: A qualitative analysis of temporal evolution. BMC Public Health 2021, 21, 2232. [Google Scholar] [CrossRef]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.M.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef]
- Bennett, C.M. Learning to live with COVID-19 in Australia: Time for a new approach. Public Health Res. Pract. 2021, 31, e3132110. [Google Scholar] [CrossRef] [PubMed]
- Young-Xu, Y.; Korves, C.; Roberts, J.; Powell, E.I.; Zwain, G.M.; Smith, J.; Izurieta, H.S. Coverage and estimated effectiveness of mRNA COVID-19 vaccines among US veterans. JAMA Netw. Open 2021, 4, e2128391. [Google Scholar] [CrossRef] [PubMed]
- Rosseel, Y. lavaan: An R package for structural equation modeling. J. Stat. Softw. 2012, 48, 1–36. [Google Scholar] [CrossRef] [Green Version]
- De Vaus, D. Analyzing Social Science Data: 50 Key Problems in Data Analysis; Sage: Thousand Oaks, CA, USA, 2002. [Google Scholar]
- Streiner, D.L.; Norman, G.R.; Cairney, J. Health Measurement Scales: A Practical Guide to Their Development and Use; Oxford University Press: Oxford, UK, 2015. [Google Scholar]
- Liu, J.; Liu, M.; Liang, W. The dynamic COVID-zero strategy in China. China CDC Wkly. 2022, 4, 74–75. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Fardin, M.A.; Shirazi, M.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; McIntyre, R.S.; Tran, B.; Quek, T.T. Mental health of the general population during the 2019 coronavirus disease (COVID-19) pandemic: A tale of two developing countries. Psychiatry Int. 2021, 2, 71–84. [Google Scholar] [CrossRef]
- Wang, C.; Chudzicka-Czupała, A.; Grabowski, D.; Pan, R.; Adamus, K.; Wan, X.; Hetnał, M.; Tan, Y.; Olszewska-Guizzo, A.; Xu, L. The association between physical and mental health and face mask use during the COVID-19 pandemic: A comparison of two countries with different views and practices. Front. Psychiatry 2020, 11, 569981. [Google Scholar] [CrossRef]
- Wang, C.; Tripp, C.; Sears, S.F.; Xu, L.; Tan, Y.; Zhou, D.; Ma, W.; Xu, Z.; Chan, N.A.; Ho, C. The impact of the COVID-19 pandemic on physical and mental health in the two largest economies in the world: A comparison between the United States and China. J. Behav. Med. 2021, 44, 741–759. [Google Scholar] [CrossRef]
| Item | First Subsample |
|---|---|
| 1. I feel emotionally exhausted because of the COVID-19 pandemic and the preventive measures. | 0.849 |
| 2. I feel stressed by adhering to the COVID-19 preventive measures. | 0.887 |
| 3. I feel irritable and have a shortening fuse with the COVID-19 preventive measures. | 0.890 |
| 4. I feel hopeless as the COVID-19 pandemic continues despite preventive measures. | 0.840 |
| 5. I feel trapped in my city due to the travel ban and restrictions during the COVID-19 pandemic. | 0.809 |
| Second Subsample | Combo | ||
|---|---|---|---|
| Item | Model 1 | Model 2 | |
| Item 1 | λ1 | 0.798 | 0.813 |
| Item 2 | λ2 | 0.902 | 0.900 |
| Item 3 | λ3 | 0.907 | 0.908 |
| Item 4 | λ4 | 0.811 | 0.820 |
| Item 5 | λ5 | 0.746 | 0.759 |
| Model fit | |||
| N | 543 | 1087 | |
| RMSEA | <0.001 | 0.018 | |
| RMSEA 90% CI | <0.001–0.026 | <0.001–0.048 | |
| SRMR | 0.007 | 0.010 | |
| χ2 | 1.628 | 6.678 | |
| df | 5 | 5 | |
| χ2/df | 0.325 | 1.335 | |
| CFI | 0.999 | 0.999 | |
| TLI | 0.999 | 0.999 |
| Model | CFI | TLI | SRMR | RMSEA | 90%CI of RMSEA | ΔCFI |
|---|---|---|---|---|---|---|
| Configural Invariance | 0.999 | 0.999 | 0.013 | 0.016 | (0.000, 0.051) | |
| Metric Invariance | 0.999 | 0.999 | 0.024 | 0.054 | (0.032, 0.076) | 0.004 |
| Scalar Invariance | 0.999 | 0.999 | 0.014 | 0.013 | (0.000, 0.033) | 0.002 |
| Strict Invariance | 0.999 | 0.999 | 0.014 | 0.013 | (0.000, 0.033) | 0.002 |
| Item | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| 1 | - | 0.696 | 0.672 | 0.608 | 0.572 |
| 2 | 0.699 | - | 0.768 | 0.657 | 0.614 |
| 3 | 0.674 | 0.774 | - | 0.659 | 0.634 |
| 4 | 0.618 | 0.671 | 0.673 | - | 0.590 |
| 5 | 0.574 | 0.616 | 0.631 | 0.603 | - |
| Mean | 4.08 | 3.89 | 4.59 | 3.50 | 3.96 |
| SD | 1.973 | 2.101 | 2.115 | 2.212 | 2.148 |
| Skewness | −0.018 | 0.055 | −0.326 | 0.298 | 0.122 |
| Kurtosis | −1.289 | −1.368 | −1.343 | 0.074 | 0.074 |
| rit | 0.742 | 0.811 | 0.809 | 0.743 | 0.694 |
| aiid | 0.886 | 0.871 | 0.871 | 0.886 | 0.896 |
| Scale/Measures | COVID-19 BFS |
|---|---|
| Fear of COVID-19 Scale | 0.131 |
| I support the government adopting the “living with COVID” policy instead of the “Dynamic Zero COVID-19 strategy”. | 0.292 |
| The “Dynamic Zero COVID-19 strategy” is not sustainable in the long run. | 0.340 |
| Do you have any chronic illness (e.g., diabetes, kidney problem, cancer)? | 0.090 |
| Age | −0.334 |
| COVID-19 vaccination status | −0.149 |
| Have your family members or close friends ever been infected with COVID-19? | −0.107 |
| “Dynamic Zero COVID-19 strategy” is an effective measure to protect my city against COVID-19. | −0.345 |
| I support the “Dynamic Zero COVID-19 strategy” continuing and remaining the ultimate goal in the long run. | −0.368 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lau, S.S.S.; Ho, C.C.Y.; Pang, R.C.K.; Su, S.; Kwok, H.; Fung, S.-f.; Ho, R.C. COVID-19 Burnout Subject to the Dynamic Zero-COVID Policy in Hong Kong: Development and Psychometric Evaluation of the COVID-19 Burnout Frequency Scale. Sustainability 2022, 14, 8235. https://doi.org/10.3390/su14148235
Lau SSS, Ho CCY, Pang RCK, Su S, Kwok H, Fung S-f, Ho RC. COVID-19 Burnout Subject to the Dynamic Zero-COVID Policy in Hong Kong: Development and Psychometric Evaluation of the COVID-19 Burnout Frequency Scale. Sustainability. 2022; 14(14):8235. https://doi.org/10.3390/su14148235
Chicago/Turabian StyleLau, Sam S. S., Cherry C. Y. Ho, Rebecca C. K. Pang, Susan Su, Heather Kwok, Sai-fu Fung, and Roger C. Ho. 2022. "COVID-19 Burnout Subject to the Dynamic Zero-COVID Policy in Hong Kong: Development and Psychometric Evaluation of the COVID-19 Burnout Frequency Scale" Sustainability 14, no. 14: 8235. https://doi.org/10.3390/su14148235
APA StyleLau, S. S. S., Ho, C. C. Y., Pang, R. C. K., Su, S., Kwok, H., Fung, S.-f., & Ho, R. C. (2022). COVID-19 Burnout Subject to the Dynamic Zero-COVID Policy in Hong Kong: Development and Psychometric Evaluation of the COVID-19 Burnout Frequency Scale. Sustainability, 14(14), 8235. https://doi.org/10.3390/su14148235









