Abstract
The COVID-19 pandemic has placed the inequalities in health services in countries around the world under severe pressure. As crucial pillars in the prevention and control of COVID-19, fever clinics and fever sentinels are important sites for the screening, diagnosis, and isolation of patients. This study comprehensively evaluated the spatial-layout characteristics, configuration quantity, and service capacity of 42 fever clinics and 418 fever sentinels in Harbin from the perspective of supply by using GIS spatial-analysis methods such as kernel density analysis. From the perspective of demand, we evaluated the accessibility of fever clinics with the modified two-step floating catchment area (2SFCA) method; the OD cost matrix method and Voronoi diagram method were used to evaluate the accessibility and service pressure of fever sentinels. This study found that a monocentric clustering characterizes the spatial layout of fever clinics, and the design of fever clinics in new urban areas and marginal rural areas is relatively lacking. The spatial layout of fever sentinels includes blank areas, and the service pressure in the central city area is relatively high. Combined with the assessment results, the study discussed optimization strategies and implementation paths for improving the public health and epidemic prevention system for COVID-19 in terms of four aspects: the transformation of governance practice, the spatial-planning response, the digital infrastructure response, and guarantees of policies and regulations.
1. Introduction
The COVID-19 pandemic, which began in 2019, has presented a critical test for health services worldwide, prompting increased attention to “health equity” issues [,,]. The concept of “health equity” is the focus of one of the sustainable-development goals put forth by the World Health Organization (WHO) and one of the strategies of “Health China 2030”. The WHO defines health equity as the notion that everyone, regardless of social status, economic income, or circumstances, should have access to health services as needed to maintain their health status []. In this context, reducing inequalities in healthcare services, as one of the dimensions of achieving “health equity”, has become a concern among governments and public health planners [,,,]. During the COVID-19 outbreak, inequalities in healthcare services have posed a direct threat to people’s health, including, but not limited to, cross-infection due to lax management of primary healthcare institutions, the shortage of beds, doctors, and other resources in healthcare institutions, which makes it difficult for patients to seek medical treatment, and a lack of access to healthcare services for patients with non-infectious diseases.
Fever clinics and fever sentinels are key medical settings for the early detection of COVID-19. In China, nearly 60% of confirmed COVID-19 patients come from fever clinics []. Fever clinics play an important role in the timely screening and rapid isolation of COVID-19 patients. After the outbreak of COVID-19, the relevant research on fever clinics and fever sentinels increased rapidly from the perspectives of epidemiology, nursing, public emergency management, architecture, and other disciplines that focus on the emergency management process and enhancement strategies for fever clinics and fever sentinels [,,,], the standardization and innovative construction of internal architectural spaces [,], and the configuration standards and emergency response capabilities of primary healthcare institutions [,,]. Due to the different levels of construction of healthcare institutions and the differences in the development of COVID-19 in each city, the construction and settings of fever sentinels also display uneven and mismatched problems. Some scholars have treated fever clinics and fever sentinels as urban and rural public healthcare service institutions and explored the problems of their configuration rationality and spatial accessibility. For example, Wang et al. used the network-analysis method to calculate the coverage area and found that it took a 60-min journey to the fever clinic to achieve coverage of the whole area of residents []. Zhang et al. simulated the spatial accessibility of fever clinics in Beijing under three levels of prevention and control: low, medium, and high []. Yong et al. selected a collection of COVID-19-affected communities in Shenzhen, China to analyze the cumulative opportunity to visit fever clinics and evaluate the rationality of fever-clinic medical resources []. Song et al. established a multi-objective model based on the 2SFCA method to study the allocation of community healthcare resources so as to improve the accessibility of medical resources for all people [].
The accessibility of healthcare facilities includes both potential accessibility and realistic accessibility. Potential accessibility refers to the spatial distribution of medical facilities and the possibility that a given location or individual can reach the locations of medical services [,]. Realistic accessibility refers to the actual utilization rate of individuals who can reach medical locations and obtain medical services [,]. As research progresses, the realistic accessibility of healthcare services is becoming more widely used because it can combine service capacity and time to reflect accessibility. The accessibility research methods include the shortest-distance (time) method, Huff’s model, the gravity model approach and its improved model, and the two-step floating catchment area (2SFCA) method and its improved model. The shortest distance (time) method focuses on the distance factor and weakly considers the size factor of supply and demand points [,,]. Huff’s model considers the facility size and distance factors, but also does not consider the size of the demand points []. The gravity-model approach uses the Euclidean distance as the accessibility measure and ignores the influence of the actual transportation network []. The 2SFCA method and its modified model consider multiple factors of supply-point service capacity, demand-point size, actual travel distance, and distance threshold, and the distance decay is extended in the modified form, which is more widely used. Tao evaluated the spatial accessibility of healthcare services under multiple transportation modes using a multi-mode Gaussian-based two-step floating catchment-area method []. In the work by Jin, combined with the population data of subdistrict communities, the hierarchical two-step floating catchment-area method was used to carry out a study on the spatial accessibility of public healthcare service facilities at all levels in Shenzhen, China []. Neng proposed a three-step floating catchment-area method (3SFCA) that incorporates inter-facility competition factors to evaluate the accessibility of basic healthcare in Central Texas [].
To summarize the content of studies on fever clinics and fever sentinels and the methods of research on the accessibility of healthcare facilities, it can be stated that there are still fewer studies on the analysis of healthcare service parity and its optimization strategies in healthcare surveillance facilities. Meanwhile, there is a lack of attention given to fever sentinels, which are also healthcare surveillance facilities. It is necessary to build an evaluation framework that is suitable for both types of hierarchical healthcare monitoring institutions—fever clinics and fever sentinels. In addition, some studies have focused on the inequality of healthcare services, but have not proposed detailed and effective optimization strategies and implementation paths [,,]. Moreover, in terms of measurement methods, the current studies have a large range of population data units and low data accuracy, and they use simple methods to measure the accessibility of fever clinics that lack attention to high-precision population distribution data, medical-service capacity, demand-point scale, and other aspects.
In summary, this study explores the spatial-layout characteristics of fever clinics and fever sentinels as a response to COVID-19 prevention and control, as well as the inequalities in their healthcare services’ accessibility, and discusses the optimization strategies and certain implementation paths by taking seven districts of Harbin City as an example. In Section 2, we review the relevant literature, identify the causes and related studies that trigger inequalities in fever clinic services, and propose a conceptual framework for the causes of inequalities in fever clinic services. In Section 3, an empirical study is described to validate our conceptual framework, and our empirical study data, research methods, and research framework are presented. We selected fever clinics and fever sentinels in seven districts of Harbin as the research objects. In Section 4, the spatial-layout characteristics of the fever clinics and fever sentinels in the seven districts of Harbin are analyzed in terms of both supply and demand, and the number of configurations and the service capacity are analyzed. We also combine the actual traffic-network data and high-precision population distribution data, apply the modified two-step moving floating catchment area method to comprehensively evaluate the accessibility of fever clinic services, and apply the OD cost matrix method and Voronoi diagram method to evaluate the accessibility and capacity of fever sentinels; we also evaluate the health-equity levels of these two levels of healthcare surveillance institutions in Harbin City. In Section 5, we propose strategies for improving and optimizing fever clinics and fever sentinels in terms of both spatial planning and governance systems. Section 6 concludes this study and provides recommendations for further research. The developments of this study can provide theoretical references and case studies for the construction of systems of healthcare surveillance institutions, such as fever clinics and fever sentinels, in other cities.
2. Inequality in Healthcare Services of Fever Clinics and Fever Sentinels
2.1. COVID-19 Exacerbates Inequities in Healthcare Accessibility
The level of healthcare services is mainly influenced by urban and rural systems, as well as economic, social, ethnic, occupational, and gender factors [,,]. With the combination of these multiple influences, building equity in healthcare services in a region will be a long and slow process of change []. However, during the COVID-19 pandemic, the infectious and harmful nature of the virus, as well as the large differences in the conditions of local healthcare facilities and the level of healthcare personnel [], had an impact. As a result, the number of fever clinics and fever sentinels during the COVID-19 period was relatively low, which further exacerbated the inequalities in medical services accessible during COVID-19 [,].
2.2. The Spatial Structure of China’s Large Cities Affects the Layout of Healthcare Facilities and the Accessibility of Fever Clinics
In the process of the rapid urbanization in China, the spatial structure of cities has mostly shown a compact pattern of outward expansion []. In contrast, the centers of older urban areas have a longer history of development and an obvious accumulation effect, gathering more high-quality medical-service facilities and tertiary-industry service facilities, such as for education and commerce, in the cities []. This has led to unevenness in the spatial distribution of high-quality medical resources and fever clinics in large cities, showing the spatial layout characteristics of a high concentration in the city center and an extreme lack in peripheral areas. Si et al. found that Beijing’s high-quality large-scale medical resources show an obvious monocentric layout, which is different from the balanced development patterns of old and new cities in Paris and Tokyo or the surrounding suburbs in New Delhi and London []. Luo et al. found that 60% of large general hospitals in Wuhan are located in the area of the second ring road [], and Chen et al. found that general hospitals in Nanjing were agglomerated in the older urban areas and that there were blind service areas in the newer urban areas []. The reliance of fever clinics on the construction of existing high-quality medical facilities has led to a spatial layout of fever clinics that also shows monocentric characteristics, as they are concentrated in the older urban areas of the city, and they show an extreme shortage in the peripheral areas of the city, further exacerbating the inequalities in the accessibility of fever clinics during the COVID-19 epidemic.
2.3. The Dual Rural–Urban System in China and the Construction of COVID-19 Fever Clinics
Due to the dual rural–urban system in China, there are significant differences in construction standards between urban and rural areas in terms of medical facility conditions, medical service levels, and medical space security [,]. The problems of low levels of emergency medical and healthcare services, a shortage of basic emergency medical equipment, and a lack of public health service professionals are more prominent in rural areas [,]. The “sentinel” function of primary rural healthcare institutions in the event of the COVID-19 epidemic is also facing serious challenges [].
2.4. The Lag in the Construction of New Urban Areas, Planning Patterns, and Inequalities in Accessibility of COVID-19 Fever Clinics
During the construction of new urban areas in China, the excessive pursuit of a construction scale for commercial, residential, and large public buildings has led to a lag in the construction of convenient medical, primary school, elderly, and other public service facilities, and the construction scales and service levels vary widely [,]. Additionally, as China’s car consumption continues to increase, the planning model of “large street outline, wide road, low road network density” in new urban areas enhances the convenience of automobile cities, but makes it difficult for residents to obtain more convenient medical services by walking. The lack of medical services in new urban areas and the excessive size of urban neighborhoods exacerbate the inequalities in access to fever clinics for residents of new urban areas.
2.5. The Maintenance and Control Measures of the Emergency Medical Facilities Need to Be Improved
In response to the spread of the SARS virus, the Chinese government proposed relevant construction specifications in terms of emergency medical facilities. However, after the SARS virus passed, most of the emergency medical facilities were closed, became idle, or were converted into operating clinics due to hospital profit management and other reasons. The emergency medical facilities lacked regular management of emergency disposal processes, management systems, and rescue capabilities for public health emergencies. During the COVID-19 outbreak, some cities demonstrated poor emergency handling of fever clinics, and cross-infection within fever clinics occurred [,]. During the COVID-19 epidemic, many primary healthcare institutions without the capacity to respond to the COVID-19 epidemic chose to stop operating, resulting in primary healthcare institutions playing a more important role in the emergency response system. This led to a lack of the “sentinel” role of primary care in the emergency response system. This further exacerbates the inequalities in access to COVID-19 fever clinics and fever sentinels between urban and rural populations.
By exploring the causes of medical service inequality, this study constructed a conceptual framework of medical-service inequality in fever clinics and fever sentinels in the context of the COVID-19 outbreak. In order to verify the conceptual framework of the causes of inequality, we selected Harbin as an example, attempting to quantitatively explore the medical-service inequality associated with fever clinics and fever sentinels and to enrich the theoretical exploration and practical literature on medical-service inequality under the developing concept of “health equality”.
3. Materials and Methods
3.1. Research Scope and Hierarchical Assessment Framework
Harbin is the capital city of Heilongjiang Province, with a total population of 9,485,000 in 2020. Due to its geographic characteristics, such as numerous bordering cities, frequent international trade, and the cold weather in the winter in Heilongjiang Province, Harbin has become a potentially risk-prone area for COVID-19, and there have been many small-scale epidemic rebound problems during the COVID-19 epidemic. With the COVID-19 epidemic entering the normalization stage, the importance of monitoring medical institutions has become increasingly important. Since the outbreak of COVID-19, Harbin has built an epidemic prevention system of “hospitals designated for admission–fever clinic–primary healthcare institutions”, which is one of the typical cases of the evaluation of the configuration of epidemic prevention institutions in large cities in China.
3.1.1. Study Area
As the research area, we selected seven districts of Harbin—Daoli, Nangang, Daowai, Xiangfang, Pingfang, Songbei, and Hulan—with 42 fever clinics and 418 fever sentinels, which were used as the study subjects (Figure 1). On 22 January 2020, the Harbin Health Care Commission announced a list of 72 medical institutions with fever clinics in the city [], 42 fever clinics of which were located in the study area. Due to the strict construction requirements for fever clinics, all fever clinics in Harbin were set up within tertiary or secondary hospitals, including 24 tertiary hospitals and 18 secondary hospitals. Fever sentinels were set up in primary healthcare institutions, and there were 418 primary healthcare institutions in the study area, which can be divided into four categories: community health-service centers, community health-service stations located in urban areas, township hospitals, and village clinics located in rural areas.
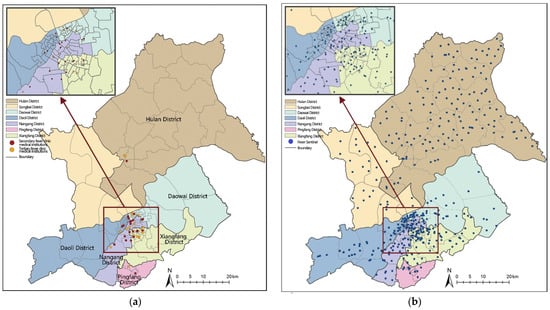
Figure 1.
Distribution of fever clinics (a) and fever sentinels (b) in seven districts of Harbin.
3.1.2. Assessment Framework Construction
We analyzed the characteristics of the two types of medical-monitoring institutions in order to adopt the most appropriate evaluation methods. There was hierarchical monitoring between fever clinics and fever sentinels. In the event of a large-scale COVID-19 outbreak, fever clinics and hospitals designated for admission conducted integrated screening and treatment; the number of beds in the medical institutions relied on by a fever clinic became an important indicator of its service capacity under extreme circumstances. Fever sentinels did not have the characteristic of long-term stays, and mainly displayed two characteristics—full coverage and high efficiency in epidemic prevention and surveillance. Complete coverage means screening, reporting, and detecting at the residential points, and high efficiency means that the number of people served under the jurisdiction of the sentinel represents a reasonable carrying capacity. Therefore, this study used the modified 2SFCA method to evaluate the accessibility of the fever clinic—with the number of beds as the index and 30 min as the service threshold—to conduct the accessibility assessment; the OD cost matrix method was used to evaluate the accessibility of the sentinel site, with time as the index, and the Voronoi diagram method was used to evaluate its service and management pressure. Thus, the evaluation methods and procedures used to assess the medical institutions were adapted to two levels, and different functional characteristics were formed (Figure 2).
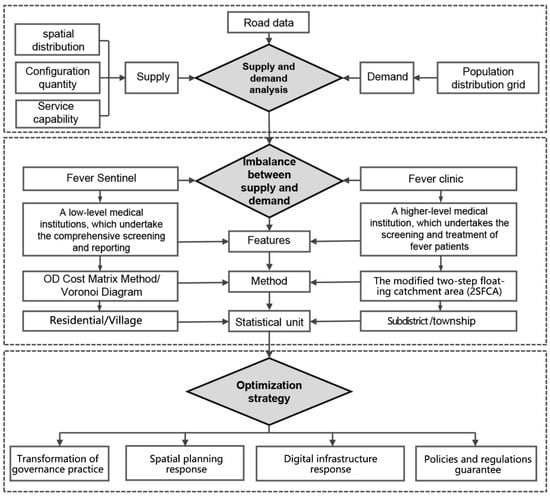
Figure 2.
Research framework.
3.2. Data
The data analyzed in this study consisted of the following five parts. ① The administrative division data of the subdistricts (townships): The administrative division data of the subdistricts (townships) were obtained from the Civil Affairs Department of Harbin, and the shapefile boundary range data for subdistricts (townships) were drawn, aligned, and corrected using the ArcGIS 10.2 software. ② Residential and administrative village point data: The data on the residents were obtained from the Gaode website by using “residential” as a keyword for search crawling. The data on administrative villages were obtained from the secondary class land-use raster data released by the Resource and Environment Science and Data Center, vectorizing them to obtain the village noodles, and, finally, using the “element-to-point” tool to obtain the residential and village point data. ③ Raster data of the population distribution in the study area: The raster data of the population distribution in the study area were derived from an open-source population distribution raster at a 100 m resolution for 2010, which was provided by the World Pop website and corrected with data from the sixth China’s census data (Figure 3). ④ Road traffic network vector data in the study area: The study area’s vector data for road traffic networks were derived from the open-source GIS vector dataset in OSM (Open Street Map). ⑤ Information on fever clinics and sentinels in the study area: The data of fever clinics in the study area were obtained from the official website of the Harbin Healthcare Commission, while geographic information data were converted into geographic coordinate data in the GIS database according to the address data from the Gaode map. Moreover, data such as the service level and the number of beds in fever clinics were obtained from the official website of each medical institution; a small amount of data was supplied by the “Famous Doctors” and “China Hospital Ranking” websites. The data on the fever sentinels were obtained from the Gaode website by using “community health service center,” “community health service station,” “township hospital,” and “village clinic” as keywords.
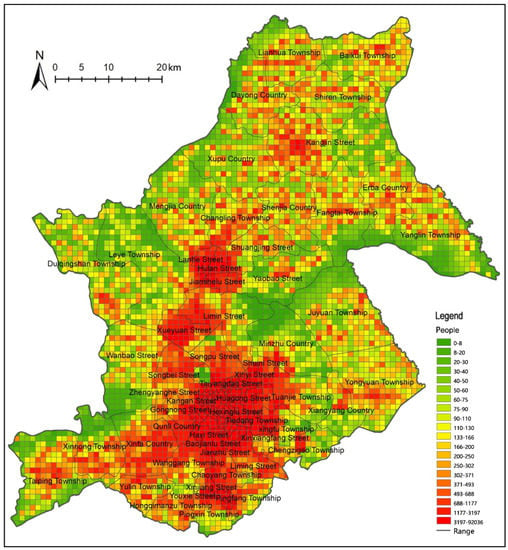
Figure 3.
Population distribution raster fishnet map.
We classified the data provided above and created a geodatabase using ArcGIS 10.2. Finally, a spatial GIS database was created for the study area, consisting of seven districts, 128 subdistricts (townships), 1977 residential points, 1099 village points, 42 fever clinics, and 418 fever sentinels (Table 1).

Table 1.
Study Data Statistics.
3.3. Methods
3.3.1. Kernel Density Analysis
Kernel density analysis can be used to calculate the concentration of point elements in the spatial distributions of their surrounding neighborhoods, such as in the accumulation of populations, public service facilities, points of interest (POIs), etc. By setting a kernel function at each point element and distributing its value within the specified threshold range (), the density value at the point to be estimated decreases with increasing distance from the point element and drops to zero at the distance to the search threshold. In this study, the fever clinics and fever sentinels were analyzed by using this function, i.e., the density value was at its maximum at the central location of each fever clinic and fever sentinel, the estimated points decayed with increasing distance from the central location of the fever clinic and fever sentinel, and the density values at the same geographical location were superimposed, as shown in Equation (1).
where is the kernel density estimate, is the kernel density equation, denotes the distance from the estimated point to the fever clinic or fever sentinel point i, n is the number of fever clinics or fever sentinels within the distance threshold, and is the distance threshold.
3.3.2. The Modified Two-Step Floating Catchment Area (2SFCA) Method
Accessibility refers to the service capacity obtained from the demand point to the supply point, which is negatively correlated with the time consumed from the demand point to the supply point, but positively correlated with the scale of service provided by the supply point. It has the following advantages: (1) It takes into account the reality that residents will seek medical treatment across regions and excludes the limitation of the administrative boundary range; (2) it conducts two searches that are centered successively on supply and demand points and evaluates them from the perspective of combining supply and demand; (3) in terms of methodological improvement, this study improves the commonly used two-step moving search method in terms of three aspects—precision of demand point data, measurement of travel time based on actual road network speed, and establishment of a spatial decay rule using a Gaussian function, as follows.
In the first step, we use fever clinics as the supply point (), while the distance of the road network corresponding to the time threshold t0 to the fever clinic is used as the search radius to establish the search area, and all of the residential points () that fall within the search area are searched. Using a Gaussian decay function to decay by distance and assigning weights to population numbers, the weighted populations are aggregated and the supply-to-demand ratio is calculated as shown in Equation (2).
where is the scale of supply at point , which is represented in this study by the number of hospital beds; Dk denotes the scale of demand at point , which is represented by the total population; is the actual road-network-based travel time between locations i and j. In this study, the OD cost matrix is used for calculation. Finally, is a Gaussian decay function considering spatial friction. Its specific form is given by the following equation:
In the second step, we take the population unit () as the demand point, establish a search area with the radius of the road network distance corresponding to the time threshold () for people to visit the fever clinic, find all of the fever clinic points () that fall within the search area, and sum up the service supply–demand ratio () provided by all fever-clinic points after quadratic Gaussian decay to obtain the accessibility () at the population unit (), as shown in Equation (3).
3.3.3. OD Cost Matrix Method
The “OD cost matrix” function in the “Network Analysis Module” of GIS can be used to find and calculate the minimum time cost and path from starting point i to destination point j in the traffic topology network. In the study, the OD matrix is used to count the minimum time cost between the residential (village) unit and the fever sentinels.
3.3.4. Voronoi Diagram Method
According to the nearest neighbor principle, the Voronoi diagram can be used to divide the respective service areas of discrete points in the plane so that the distance Pn from any point Qn in the service area to other discrete points is greater than the discrete point P1 in the area []. In this study, the service area of a fever sentinel is established through the Voronoi diagram to preliminarily divide the population served by each fever sentinel and evaluate the service pressure of each fever sentinel.
4. Results
4.1. Spatial Distribution Characteristics of Fever Clinics and Fever Sentinels
The kernel density analysis of 42 fever clinics in the study area revealed a more apparent monocentric clustering feature (Figure 4). More specifically, 37 fever clinics are gathered in the core areas of Nangang, Xiangfang, Daoli, and Daowai, the four old urban areas. The two gathering points are close to each other, forming a single-center clustering pattern of fever clinics. Two fever clinics are located in the southern part of the study area, in Pingfang District. Three are distributed in Hulan District in the north. The fever clinics in the southern and northern areas show certain clustering distribution characteristics.
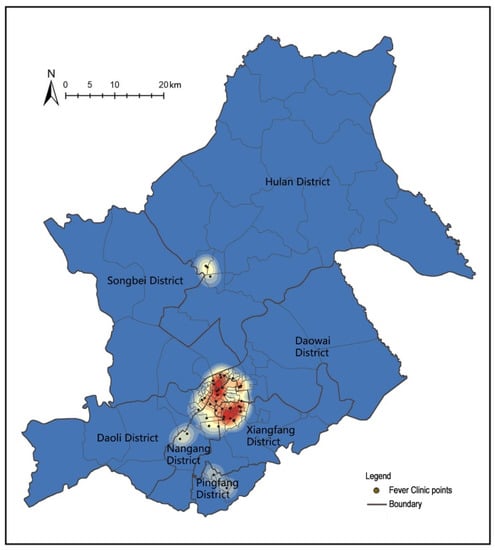
Figure 4.
Kernel density analysis of fever clinics in seven districts of Harbin.
There are 418 fever sentinels in the study area, including city fever sentinels (94 community healthcare centers and 59 community healthcare stations) and rural fever sentinels (29 township hospitals and 236 village clinics). Fever sentinels are characterized by “dense subdistricts and sparse townships” (Figure 5). There is a large difference between different administrative regions. The result for the urban area south of the Songhua River is significantly higher than that for the Songbei District and Hulan District to the north of the Songhua River. A large cluster has formed south of the Songhua River, and the rest are scattered.
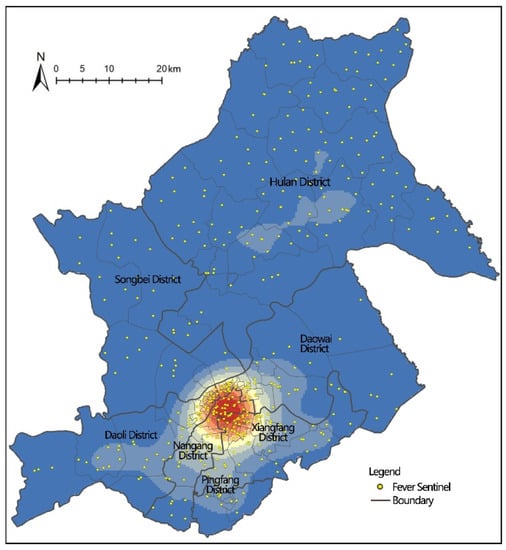
Figure 5.
Kernel density analysis of fever sentinels in seven districts of Harbin.
4.2. Characteristics of the Numbers of Fever Clinics and Allocated Fever Sentinel Sites
According to the distribution of the 42 fever clinics across the seven districts, the study area’s layout demonstrates a more obvious distribution of three gradients. The first tier includes Xiangfang District and Nangang District, with 13 and 12 fever clinics, respectively. The second includes Daowai District and Daoli District, with seven and five fever clinics, respectively. The third tier includes Hulan District, Pingfang District, and Songbei District, with three, two, and zero fever clinics, respectively.
We comparatively analyzed the capacities of the fever clinic services in the large urban areas by referring to the configurations of fever clinics in other Chinese cities. According to a statistical analysis of the number of fever clinics set up in China’s 14 major cities by Liu Lu, the number of fever clinics per 100,000 people in 14 cities was 0.65 []. The study area’s average fever clinic configuration is 0.08 per 100,000 people, which is relatively higher than the average of these 14 cities. However, the uneven internal service-capacity configuration became increasingly prominent. Among them, Xiangfang District, Pingfang District, and Nangang District all have a higher capacity for fever clinic services, with 1.42, 0.89, and 1.05 fever clinics per 100,000 people, respectively. Meanwhile, Daoli District, Hulan District, and Songbei District do not achieve the average standard in the service capacity configuration, and Hulan District and Songbei District have relatively insufficient fever clinic configurations—especially Songbei District, which has the least. Thus, the capacity of these districts’ fever clinics should be increased in the future (Figure 6).
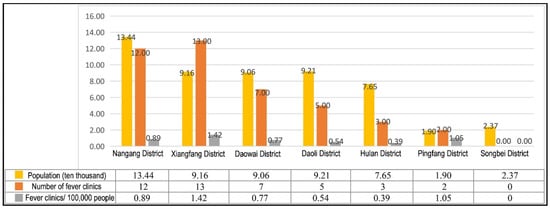
Figure 6.
Fever clinic configuration and service capacity in seven districts of Harbin.
Regarding the configuration of the number of fever sentinels, except for the Daowai and Songbei Districts, the other five jurisdictions meet the standard requirement of one community healthcare center per subdistrict, but the layout of community health service stations in the Daowai and Songbei Districts is relatively high. Community healthcare stations have formed a supplement, and it can be seen that the number of fever sentinel points in the subdistricts is generally reasonable.
In the configuration of township fever sentinels, the number of township healthcare centers in each township unit in Xiangfang District, Daoli District, and Pingfang District is less than one. All three are located south of the Songhua River. In addition, taking the administrative village as the unit for counting the number of village fever sentinels, with the exception of Nangang District and Xiangfang District, the allocation of the other five districts is lower than the average of 0.26/per administrative village (Table 2). It can be seen that the number of fever sentinels in townships is relatively poor. Among them, the allocation of village clinics is generally low, township hospitals are relatively common south of the Songhua River, and the role of rural primary healthcare institutions in the emergency response system is insufficient.

Table 2.
Evaluation of fever clinic configuration in seven districts of Harbin.
4.3. Analysis of the Accessibility of Fever Clinics
4.3.1. Choice of Research Methodology
When a major epidemic occurs, on the one hand, patients tend to travel to fever clinics in private cars or “120” ambulances to minimize the risk of transmission caused by the movement of people and to receive timely treatment; on the other hand, patients should avoid using public transportation as much as possible and should choose to walk, cycle, or use a private car or “120” ambulance.
We constructed the road traffic network dataset based on the average traffic speeds on various classes of roads in the city (Table 3). Nowadays, cities are actively building a 30-min medical lifecycle. This study uses 30 min as the travel threshold to measure the accessibility of fever clinics. We created a new OD cost matrix based on the created network analysis layer, set the impedance to a time of 30 min in the layer attribute analysis settings, and calculated the population demand points that could be served by the 42 fever clinics within the travel threshold and the shortest travel time.

Table 3.
All levels of road speed Settings.
Then, using the attenuation coefficient to weight and summarize the total population of demand points that could be served by each fever clinic, we used the number of beds to represent the service capacity to calculate the supply–demand ratio Rj of the 42 fever clinic hospitals. We searched 4914 demand points for population i again, considered the reachable fever clinics (j) within the threshold (t0) range, performed a second attenuation of the searched supply–demand ratios Rj of all hospitals, weighted the summation; finally, the accessibility of fever clinics for population i of 4914 demand points was obtained.
The results of the accessibility analysis were classified into five levels using the natural discontinuity grading method (Table 4). Grades I to V indicate that the accessibility to the fever clinic is gradually improving, and we obtain an accessibility grading chart with five classification levels (Figure 7).

Table 4.
Table for grading the accessibility of subdistrict (township) fever clinics.
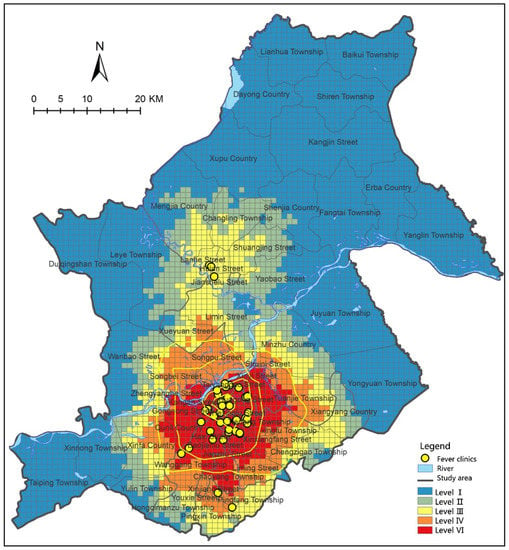
Figure 7.
Accessibility of fever clinics in seven subdistricts (townships) of Harbin.
4.3.2. Fever Clinic Accessibility Results
From the accessibility-analysis diagram, the accessibility of 128 subdistricts (townships) shows a clear pattern of decreasing from the city center to the peripheral urban fringe areas. All class V subdistricts (townships) are located within the city’s second ring, and the accessibility value of each subdistrict is 1.04 beds per 100 people. The accessibility between the second and third rings can be divided into two gradients. The higher gradient is noted for the region south of the Songhua River, which is a class V accessibility area, and a relatively lower gradient is noted for the region north of the Songhua River, which is a class IV accessibility area. The accessibility of the subdistricts (townships) outside the city’s third ring decays at a slower rate in the direction of the southern Pingfang District and the northern Hulan District. This is because the relatively discrete fever clinics in the Pingfang and Hulan Districts, respectively, improve access to subdistricts (townships) in Pingfang and localized areas in Hulan.
We aggregated the accessibility data obtained by taking a 1 × 1 km grid unit as the smallest unit in the study area, resulting in 128 subdistricts (townships), and we calculated the arithmetic mean. It was found that 78 of the 128 subdistricts (townships) in the study area have accessibility values at level V, 15 at level IV, nine at level III, nine at level II, and 17 at level I. Overall, the percentage of subdistricts (townships) with accessibility values of IV and V is 72.66%. In addition, there are 26 subdistricts (townships) at levels I and II, among which eight subdistricts (townships) have an accessibility value of zero. These numbers indicate that the accessibility balance of the subdistricts (townships) in the study area is poor.
The accessibility data of 128 subdistricts (townships) in the study area were aggregated into seven jurisdictions, and we calculated the arithmetic mean. Then, we could obtain the accessibility data of each district (Table 5). The accessibility of each district from high to low was as follows: Nangang District > Xiangfang District > Pingfang District > Daoli District > Dao Wai District > Songbei District > Hulan District. In Nangang District, with the exception of Hongqi Manzu Township at level II and Wanggang Town at level IV, 18 subdistricts are at level V. The overall accessibility is good. This is due to Hongqi Manzu Township being located in a suburban area. It is connected to the central city via a low-grade road, hindering its access to medical resources. The fever clinics in the Daowai and Daoli Districts are concentrated in the areas close to the central city. The peripheral townships cannot access fever clinic services within the transportation threshold. This issue means that Juyuan Township and Yongyuan Township in Daowai District and Xinnong Township and Taiping Township in Daoli District have an accessibility value of almost zero. With the regularization of epidemic prevention work, these peripheral townships urgently require improved fever clinic services. For example, the Taiping Township in Daoli District poses a more significant challenge to regular epidemic prevention work due to its proximity to Taiping International Airport and the great and complex flow of people. The Songbei and Hulan Districts have the worst accessibility. Songbei District has not yet set up fever clinics. Some of its accessible subdistricts are influenced by Hulan District. In Hulan District, three subdistricts (townships) are located in class II accessible areas, while eight townships have accessibility values of zero. There is a considerable variation in the accessibility of fever clinics in the subdistricts (townships) in Hulan District, since it has the largest administrative area among the seven districts. The transportation distance between the marginal townships and the three fever clinics in Hulan District is considerable, making it difficult to obtain medical services from fever clinics within the travel threshold.

Table 5.
Accessibility of fever clinics in each administrative region and subdistricts (townships).
4.4. Fever Sentinel Accessibility and Service Pressure Analysis
4.4.1. The Accessibility of Fever Sentinels
Relevant studies have shown that the walking speed of adults is 1.24 m/s, the walking distance in 15 min is approximately 1500 m, and the maximum acceptable distance for the needs of subdistrict-level medical facilities is 3 km. Due to the large size of the rural area and the scattered distribution of villages, the scope can be appropriately expanded. This study takes 3000 and 5000 m as adjacent points (Table 6).

Table 6.
Travel distance classification for fever sentinels.
Within the subdistrict range, the residential points with a reachable distance to the fever sentinels of between 0 and 1500 m are mainly concentrated in the third ring. Overall, 82% of the residential points are within 1500 m of the fever sentinels. The residential points that can reach fever sentinels with distances between 1500 and 3000 m are mainly located in the Haxi subdistrict and Qunli subdistrict of Nangang District, the College Road subdistrict of Hulan District, and the Songpu subdistrict and Songbei subdistrict of Songbei. The worst accessibility for residential points with a distance of more than 3000 m is concentrated here. It can be seen that the areas with average and poor access to urban fever sentinels are clustered in the zones of new development in the city.
Within the rural area range (Figure 8), 63% of the village points are within 3000 m of the fever sentinels, which is a reasonable range for fever sentinels in the township; 23% of the village points are far from the fever sentinels, with a distance of 3000–5000 m, which is not conducive to effective monitoring; 14% of the village points have a reachable distance of more than 5000 m; these are mainly concentrated in the northeast corner of Juyuan Town and Yongyuan Town in Daowai District and the southwest corner of Leye Town in Songbei District. The full coverage of the districts should be expanded, and basic medical facilities should be added to the southwest of Songbei District and the northeast of Daowai District.
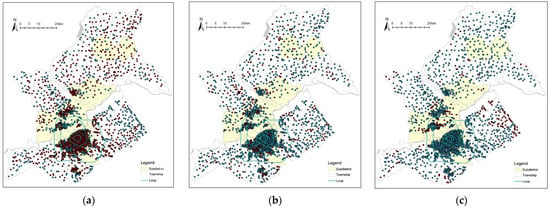
Figure 8.
Travel distance classification for fever sentinels. (a) Distribution of residential points with reachable distance within 1500 m and village points with reachable distance within 3000 m (red points); (b) Distribution of residential points with reachable distance between 1500 and 3000 m and village points with reachable distance between 3000 and 3000 m (red points); (c) Distribution of residential points with reachable distance more than 3000 m and village points with reachable distance more than 5000 m (red points).
4.4.2. Fever Sentinel Service Pressure Analysis
Based on the principle of distance optimization, a Voronoi diagram was used to construct the service ranges of the fever sentinels. By establishing a Voronoi diagram for 418 fever sentinels, the service areas of 418 fever sentinels were obtained.
For subdistrict fever sentinels, the population served by community health-service centers is 25,000–30,000 [], and the population served by community health-service stations is 12,500–25,000. The population served by the township hospitals is not clearly defined, and the number of villages was mostly used as the configuration standard. Referring to the population standard of township hospitals issued by the Anhui Provincial Health and Health Commission [], this study set the service population standard of the township hospitals at 25,000 to 30,000 people (Table 7). The service capacity of the village clinics is relatively low, and it only meets the service needs of one village unit. According to the distribution of the total village population in the study areas, 5000 and 10,000 people were taken as the critical points for the proportions of the population served by village clinics. We connected the population distribution grid with the service areas generated by the Voronoi diagram to obtain the population in the service area of each fever sentinel, to evaluate the current service pressure of fever sentinels, and to provide directions for subsequent optimization (Figure 9).

Table 7.
Population size classification of various fever sentinel services.
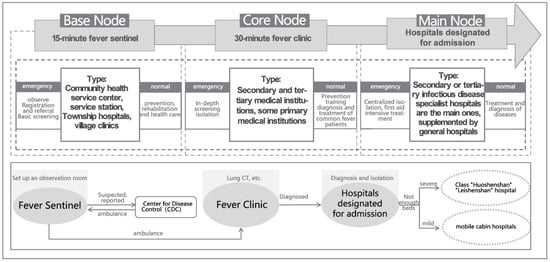
Figure 9.
Schematic diagram of population pressure zoning in the Voronoi diagram service area of the fever sentinel.
The analysis showed that 18% of the fever sentinels’ service areas are overpopulated, and these are mainly located in the centers of the old urban areas and in parts of the new urban areas. The large population in the central urban areas leads to tremendous pressure on epidemic prevention measures. Inadequate construction of primary medical facilities in new urban areas has also caused a certain pressure for epidemic prevention. Overall, 24% of the fever sentinels serve a small population, which is mainly located within the study area’s marginal regions, mostly in areas served by village clinics. This is due to the sparse and scattered population and low utilization of medical resources in the peripheral townships of the study area. The Statistical Information Center of the National Health and Medical Commission released statistics on the medical and health institutions in the country in 2020. Among them (apart from primary healthcare institutions), the number of village clinics showed a significant downward trend under the impacts of the epidemic []. Firstly, most village clinics currently do not have the ability to receive patients during COVID-19. Secondly, the village clinic surveillance network has not been fully formed, the daily utilization rate of village clinics has declined, they have been operating inefficiently, and the degree of inefficient operation during COVID-19 has risen. This has created an obstacle to the formation of a rural epidemic-prevention system. The village clinics’ environment should be regularly screened in the future to maintain their operational capacity.
5. Discussion and Proposals
5.1. The History of Urban–Rural Development and Inequalities in Medical COVID-19 Monitoring Institutions
At the overall level of the research area, the total configuration of fever clinics is satisfactory, but there are large inequalities in the accessibility of fever-clinic care within the region. Firstly, fever-clinics show monocentric clustering characteristics in the old urban areas. The accessibility of fever clinic services decreases rapidly from the center to the periphery. This is because most of the higher-grade medical institutions are older and their locations were chosen according to a more reasonable pattern of the urban spatial layout at that time, but with the rapid expansion of the urban space, the problem of the inequality of medical services is being gradually exposed. Such inequalities also exist in China’s other major cities, such as Beijing and Guangzhou [,]. Secondly, there is an imbalance in supply between old and new urban areas. Old urban areas have richer medical resources due to their longer developmental history, while new urban areas are slow to build high-grade medical institutions due to lagging planning and construction and the slower development of production and living functions, which affect the supply of fever clinic services in new urban areas. Third, there is a supply inequality between urban and rural areas. The accessibility of fever clinics in subdistricts is better than that in rural areas, and some townships are liable to become weak and blank areas in the COVID-19 epidemic prevention system due to the low grade of internal roads and the large administrative area, which increases the distance of access to fever clinics. Fourth, the accessibility of fever sentinels in subdistricts is also better than that in township areas, where there are some areas of weak monitoring and areas with excessive pressure on services. The accessibility of fever sentinels in new urban areas, such as Songbei District and Qunli subdistrict, is poor. The number of fever sentinels in rural areas is smaller, the number of village clinics among fever sentinels is insufficient, and they are vulnerable to marginalization during COVID-19 outbreaks. At the same time, rural areas have poor accessibility to fever sentinel sites due to the long distances from settlements and long road travel times, making it more difficult to monitor and prevent COVID-19.
5.2. Reconstruction of the Spatial Planning and Governance System for Urban Fever Clinics and Fever Sentinels
In summary, we propose several strategies for the optimization of fever clinics and fever sentinels in terms of four aspects: transformation of governance practices, spatial-planning response, digital infrastructure enhancement, and policy and regulatory safeguards.
5.2.1. Transformation of Governance Practice: Response to Public Health Emergencies under the Concept of “Peacetime and Epidemic Combination”
With the normalization of COVID-19 prevention and control, the number of visits to fever clinics and fever sentinels may decrease. According to the experience after the SARS epidemic, fever clinics are prone to problems such as vacancy and decreases in the rate of utilization of medical resources. Therefore, in line with the concept of “peacetime and epidemic combination”, we should take into account the functional transition between the emergency period and the regular period and improve the system for the construction of regular fever clinics and fever sentinels. We should improve the scale of medical services and the level of professionals in fever clinics and improve the condition of medical equipment. We should encourage fever clinics to undertake medical functions, such as emergency treatment, examination, and intensive care, while screening for patients with infectious diseases. This will enable them to truly play the roles of “outposts” and “fortresses” in the framework of “peacetime and epidemic combination”. Fever sentinel sites, as primary medical institutions, should be responsible for monitoring and reporting during epidemics and should continue to serve their functions of medical care and rehabilitation during normal periods. The system of building fever clinics and fever sentinels is not only an emergency measure under COVID-19, but can also be an effective strategy for responding to the long-term goal of “Healthy China” and for addressing the problems of aging, flooding, and the prevention of infectious diseases.
5.2.2. Spatial Planning Response: Layout of Fever Clinics and Fever Sentinels for Health Equity
The spatial layout of fever clinics and fever sentinels should be integrated into the hierarchical and network layout of urban and rural living spheres. Based on the planning and construction of urban and rural lifecycles, a three-tier network of epidemic prevention and treatment institutions should be built at multiple levels, including “fever sentinels–fever clinics–hospitals designated for admission” (Figure 10). The travel time and load-bearing functions of each level should be reasonably allocated in order to form a COVID-19 epidemic prevention system using early monitoring linked with emergency response. At the same time, the construction of the “15-min nucleic acid circle” and the planning and layout of residential nucleic acid testing points can be integrated into the COVID-19 epidemic prevention system of fever sentinel sites to accelerate the formation of a hierarchical and balanced COVID-19 epidemic prevention system []. This would systematically resolve the problem of the unequal accessibility of fever clinics and fever sentinels between urban and rural areas, as well as between new and old urban areas, and guide fever clinics in towns and new urban areas by building branch hospitals, new hospitals, and medical communities to improve the construction of urban and rural COVID-19 epidemic prevention systems.
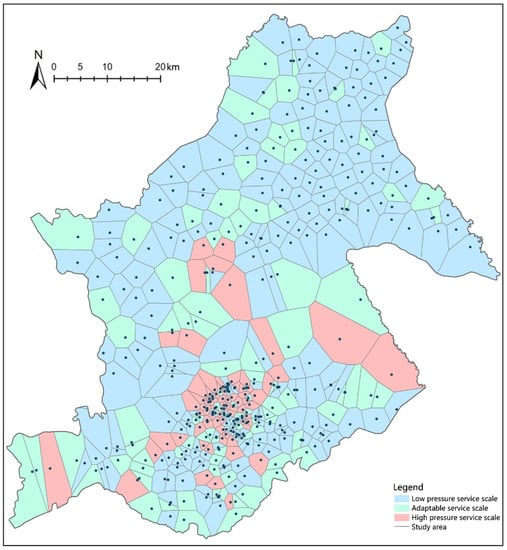
Figure 10.
Construction of a hierarchical system of epidemic prevention medical institutions and transformation of combined functions of epidemic control.
5.2.3. Digital Infrastructure Response: Building a Smart COVID-19 Epidemic Prevention Technology System
Adapting to the trend of the development of the construction of digital infrastructure in urban and rural areas, service assessments and optimal allocations of COVID-19 fever clinics and fever sentinel sites are actively carried out by using big data, AI, and other intelligent planning methods. Firstly, after the outbreak of a public health emergency, monitoring and early warning are performed through a big data platform. Intelligent mapping of COVID-19 outbreaks is based on development trends and trajectory algorithms [], including the identification of potential risk sources, monitoring of susceptible populations, research and judgment of high-risk areas, and sharing of medical resources for epidemic prevention, in order to optimize the efficiency of medical services and the resource-sharing capacity of fever clinics and fever sentinels. Secondly, the big data for intelligent transportation are used to coordinate the optimal route for epidemic prevention referral within the concept of “fever sentinel–fever clinic–hospitals designated for admission” under the state of the emergency response; this can optimize the regional control and emergency routes in densely populated areas and reduce the transmission risk of potential COVID-19 patients when they move in geographical space.
5.2.4. Policies and Regulations Guarantee: Improving the Medical Prevention and Control Mechanism and Emergency Measures in Public Health
The mechanism of collaboration between the medical-service system and the public-health system should be strengthened in terms of a policy guarantee. The existing treatment-centered medical-service system is fragmented with regard to disease prevention and control and public-health emergency management. There are problems such as the emphasis on medical-care over prevention, the division of medical care and prevention, and the separation of prevention and control. It is necessary to establish an improved, permanent public medical prevention and treatment system that integrates medicine and prevention and divides work. This would strengthen the construction of a collaborative system for the whole process of disease prevention and treatment, strengthen the medical conditions and medical facilities of basic medical institutions, upgrade the professional level of primary medical services, address the blind spots and weak areas of fever clinics and fever sentinels, and improve the prevention and control mechanisms and emergency measures of the public-health medical service system in emergency command, monitoring, early warning, prevention, control, medical treatment, and community governance.
6. Conclusions
In this study, we developed a conceptual framework to identify the causes of inequality in fever clinics and fever sentinels during the COVID-19 pandemic. We selected Harbin as an example and used a combination of GIS spatial analyses, such as kernel density analysis, the improved 2SFCA method, and the Voronoi diagram method, to identify the unequal configurations of 42 fever clinics and 418 fever sentinels as an empirical basis for the conceptual framework. Finally, optimization strategies were proposed in terms of four aspects, including governance concept transformation, spatial-planning response, digital infrastructure response, and policy and regulation safeguards. In the future, city managers, medical departments, and urban-planning departments should pay more attention to these factors, which can lead to inequity in medical resources and services amid public-health emergencies.
This study explored the theoretical causes of the inefficiency in emergencies and unbalanced supply of fever clinics and fever sentinels during the COVID-19 pandemic. The study took Harbin City as an example to quantitatively analyze and evaluate the spatial layout of fever clinics and fever sentinels, discovering the imbalance in medical resources available to residents, expanding upon the dimension of “efficient and accessible health facility layout and comprehensive coverage” in public health emergencies, and enriching the theoretical research framework for health equity. At the practical level, the study evaluated the configuration of fever clinics and fever sentinels in Harbin, providing a complete evaluation process for the study area and other cities and providing a reference for the scientific evaluation and configuration of medical facilities for the prevention of the COVID-19 epidemic. Finally, the optimization strategy and implementation path proposed in this study can provide new ideas for government departments, public-health managers, and urban planners.
There were some limitations in this study. First, although the accessibility of healthcare services is also influenced by the economic, racial, age, and gender aspects of the population, this study did not include an analysis of the impacts of individual differences in the population on the accessibility of healthcare services due to limitations of the precision of the demographic data. In addition, for example, when evaluating medical institutions used for COVID-19, only the number of beds and accessibility were considered, but differentiated data on the medical institutions, such as the number of physicians and medical resources, need to be further collected and analyzed. Moreover, in the calculation of road travel time, this study only considered road grades and did not consider the congestion on some urban roads or the difficulty of securing access to some township roads in winter due to ice and snow, which provides a direction for further research.
Author Contributions
Conceptualization, D.X. and Y.F.; methodology, D.X.; software, D.X.; validation, Q.W., Y.F. and S.W.; formal analysis, D.X.; investigation, Q.W.; resources, S.W.; data curation, Y.F.; writing—original draft preparation, D.X.; writing—review and editing, Q.W.; visualization, Q.W. and S.W.; supervision, D.X.; project administration, Y.F.; funding acquisition, S.W. All authors have read and agreed to the published version of the manuscript.
Funding
This research was sponsored by Harbin Institute of Technology Central University Basic Research Fund Project: spatial-planning evaluation technology for universities and surroundings based on emergency response to public security emergencies (AUEA574010820), (Host: Wu Songtao).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Sara, R.; Morgan, H.; Rebecca, M.; Casoni, M. How the trump administration’s pandemic health care response failed racial health equity: Case studies of structural racism and a call for equity mindfulness in federal health policy making. J. Health Politics Policy Law 2021, 46, 761–783. [Google Scholar] [CrossRef]
- Abedi, V.; Olulana, O.; Avula, V.; Chaudhary, D.; Khan, A.; Shahjouei, S.; Li, J.; Zand, R. Racial, economic, and health inequality and COVID-19 infection in the United States. J. Racial Ethn. Health Disparities 2020, 8, 732–742. [Google Scholar] [CrossRef] [PubMed]
- Azar, K.M.J.; Shen, Z.; Romanelli, R.J.; Lockhart, S.H.; Smits, K.; Robinson, S.; Brown, S.; Pressman, A.R. Disparities in outcomes among COVID-19 patients in a large health care system in California. Health Aff. 2020, 39, 1253–1262. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Unmasking and Overcoming Health Inequities in Urban Settings; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Corburn, J. Urban place and health equity: Critical issues and practices. Int. J. Environ. Res. Public Health 2017, 14, 117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Michael, M. Medical care, social determinants of health, and health Equity. World Med. Health Policy 2018, 10, 195–197. [Google Scholar] [CrossRef]
- Marmot, M.; Friel, S.; Bell, R.; Houweling, T.A.J.; Taylor, S. Closing the gap in a generation: Health equity through action on the social determinants of health. The Lancet. 2008, 372, 1661–1669. [Google Scholar] [CrossRef]
- Paterson, I.; Judge, K. Equality of Access to Healthcare; Routledge: London, UK, 2002. [Google Scholar]
- Why is the “Shanghai program” of fever clinic recommended for national study. Healthy China Obs. 2020, 6, 59.
- Nayan, N.; Kumar, M.K.; Nair, R.K.; Manral, I.; Kapoor, R. Clinical triaging in cough clinic alleviates COVID-19 overload in emergency department in India. SN Compr. Clin. Med. 2021, 3, 22–27. [Google Scholar] [CrossRef] [PubMed]
- Shen, J.; He, Q.; Shen, T.; Wu, Z.; Tan, M.; Chen, Y.; Weng, Q.; Nie, L.; Zhang, H.; Zheng, B. “An integrated system, three separated responsibilities”, a new fever clinic management model, in prevention and control of novel coronavirus pneumonia. World J. Clin. Cases 2021, 9, 9. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Li, L.; Liu, Y.; Wu, L.; Lu, C.; Wang, W.; Zheng, X.; Wan, J.; Jin, Y.; Yu, W. Establishing quality evaluation system of nursing management in fever clinics: A delphi method. J. Nurs. Manag. 2021, 29, 2542–2556. [Google Scholar] [CrossRef]
- Jiang, H.; Liu, J.; Ren, N.; He, R.; Li, M.; Dong, Q. Emergency management in fever clinic during the outbreak of COVID-19: An experience from Zhuhai. Epidemiol. Infect. 2020, 148, e174. [Google Scholar] [CrossRef] [PubMed]
- Cheng, A.; Chen, Y.; Gao, Y.; Sun, P.; Chang, R.; Zhou, B.; Qiu, H.; Cheng, F. Mobile isolation wards in a fever clinic: A novel operation model during the COVID-19 pandemic. Epidemiol. Infect. 2021, 149, e61. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Zhou, H.; Wu, X.; Huang, W.; Jia, B. Strategies for qualified triage stations and fever clinics during the outbreak of COVID-2019 in the county hospitals of western Chongqing. J. Hosp. Infect. 2020, 105, 128–129. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wolfson, J.A.; Leung, C.W. An opportunity to emphasize equity, social determinants, and prevention in primary Care. Ann. Fam. Med. 2020, 18, 290–291. [Google Scholar] [CrossRef] [PubMed]
- Zafri, N.M.; Nurullah, M.; Neema, M.N.; Waliullah, M. Spatial accessibility to healthcare facilities in coastal region of Bangladesh. Int. J. Health Plan. Manag. 2021, 36, 643–655. [Google Scholar] [CrossRef]
- Brodar, K.E.; Hong, N.; Liddle, M.; Hernandez, L.; Waks, J.; Sanchez, J.; Delamater, A.; Davis, E. Transitioning to telehealth services in a pediatric diabetes clinic during COVID-19: An interdisciplinary quality improvement initiative. J. Clin. Psychol. Med. Settings 2021, 10, 1–12. [Google Scholar] [CrossRef]
- Wang, D.; Tian, Y.; Qian, Z.; Tang, Y. An analysis on spatial accessibility of fever clinics and designated hospitals in response to epidemic events of infectious diseases:A case study of Hunan province. Chin. J. Health Policy 2021, 14, 74–79. [Google Scholar] [CrossRef]
- Zhang, J.; Han, P.; Yang, L. Spatial accessibility of fever clinics for multi-tiered prevention and control on COVID-19 in Beijing. J. Peking Univ. Health Sci. 2021, 53, 543–548. [Google Scholar] [CrossRef]
- Yong, Q.; Liu, D.; Li, G.; Wu, W.; Sun, W.; Liu, S. Reducing exposure to COVID-19 by improving access to fever clinics: An empirical research of the Shenzhen area of China. BMC Health Serv. Res. 2021, 21, 959. [Google Scholar] [CrossRef]
- Song, Y.; Wu, Y. Research on the allocation of community health-care facilities in Shenzhen under the background of COVID-19 normalized prevention and control. Spec. Zone Econ. 2021, 3, 51–53. [Google Scholar]
- Kwan, M.P. Space-time and integral measures of individual accessibility: A comparative analysis using a point-based framework. Geogr. Anal. 1998, 30, 191–216. [Google Scholar] [CrossRef]
- Luo, W.; Wang, F. Measures of spatial accessibility to health care in a GIS environment: Synthesis and a case study in the Chicago region. Environ. Plan. B Plan. Des. 2003, 30, 865–884. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kwan, M.P.; Weber, J. Scale and accessibility: Implications for the analysis of land use-travel interaction. Appl. Geogr. 2008, 28, 110–123. [Google Scholar] [CrossRef]
- Zhan, Q.; Xi, W.; Sliuzas, R. A GIS-based method to assess the shortage areas of community health service—Case study in Wuhan, China. In Proceedings of the 2011 International Conference on Remote Sensing, Environment and Transportation Engineering, Nanjing, China, 24–26 June 2011; IEEE: Atlanta, GA, USA, 2011. [Google Scholar] [CrossRef]
- Haesen, S.; Rauch, A.; Elger, B.; Rost, M. Equivalence of care? Accessibility and availability of dialysis services for older prisoners in Switzerland. Int. J. Prison. Health 2021. ahead-of-print. [Google Scholar] [CrossRef]
- Hulland, E.N.; Wiens, K.E.; Shirude, S.; Morgan, J.D.; Pigott, D.M. Travel time to health facilities in areas of outbreak potential: Maps for guiding local preparedness and response. BMC Med. 2019, 17, 232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Naghawi, H. Using geographic information system in analyzing hospital accessibility: A case study in New Orleans. Jordan J. Civ. Eng. 2012, 6, 353–360. [Google Scholar]
- Yang, Q.; Xu, J. An analysis model of public service facilities based on attraction accessibility. Planners 2015, 7, 96–101. [Google Scholar] [CrossRef]
- Wei, C.; Wheeler, K.K.; Huang, Y.; Lin, S.M.; Sui, D.Z.; Xiang, H. Evaluation of spatial accessibility to ohio trauma centers using a GIS-Based Gravity Model. Br. J. Med. Med. Res. 2015, 10, 1–10. [Google Scholar] [CrossRef]
- Tao, Z.; Yao, Z.; Kong, H.; Duan, F.; Li, G. Spatial accessibility to healthcare services in Shenzhen, China: Improving the multi-modal two-step floating catchment area method by estimating travel time via online map APIs. BMC Health Serv. Res. 2018, 18, 345. [Google Scholar] [CrossRef] [Green Version]
- Jin, M.; Liu, L.; Tong, D.; Gong, Y.; Liu, Y. Evaluating the Spatial accessibility and distribution balance of multi-level medical service facilities. Int. J. Environ. Res. Public Health 2019, 16, 1150. [Google Scholar] [CrossRef] [Green Version]
- Neng, W.; Bin, Z.; Troy, S. A three-step floating catchment area method for analyzing spatial access to health services. Int. J. Geogr. Inf. Sci. 2012, 26, 1073–1089. [Google Scholar] [CrossRef]
- Wei, L.; Yi, Q. An enhanced two-step floating catchment area (E2SFCA) method for measuring spatial accessibility to primary care physicians. Health Place 2009, 15, 1100–1107. [Google Scholar] [CrossRef]
- Liang, X.; Ma, R.; Cheng, Y.; Gong, Q.; Li, J.; Zhu, B. The Right to Accessible COVID-19 Testing in the Post-Epidemic Period under the Urban–Rural Integration: Haishu District, Ningbo City, China. Sustainability 2022, 14, 1636. [Google Scholar] [CrossRef]
- Kanuganti, S.; Sarkar, A.K.; Singh, A.P. Quantifying accessibility to health care using two-step floating catchment area method (2SFCA): A case study in rajasthan. Transp. Res. Procedia 2016, 17, 391–399. [Google Scholar] [CrossRef]
- Henning-Smith, C.; Hernandez, A.; Lahr, M.; Kozhimannil, K. Rural-Urban Differences in Access to, Attitudes Toward, and Satisfaction with Care Among Medicare Beneficiaries. Health Serv. Res. 2020, 55, 20–21. [Google Scholar] [CrossRef]
- Booysen, F.; Gordon, T. Trends and socio-economic inequality in public perceptions of healthcare delivery in South Africa. Int. J. Qual. Health Care 2020, 32, 135–139. [Google Scholar] [CrossRef]
- Strauss, P.; Winter, S.; Waters, Z.; Toussaint, D.W.; Watson, V.; Lin, A. Perspectives of trans and gender diverse young people accessing primary care and gender-affirming medical services: Findings from Trans Pathways. Int. J. Transgender Health 2022, 23, 295–307. [Google Scholar] [CrossRef]
- Smith, J.A. Reflections on the framing of ‘health equity’ in the Nationa l Primary Health Care Strategic Framework: A cause for celebration or concern? Health Promot. J. Aust. 2014, 25, 42–45. [Google Scholar] [CrossRef]
- Okonkwo, N.E.; Aguwa, U.T.; Jang, M.; Barré, I.A.; Page, K.R.; Sullivan, P.S.; Beyrer, C.; Baral, S. COVID-19 and the US response: Accelerating health inequities. BMJ Evid. Based Med. 2020, 26, 176–179. [Google Scholar] [CrossRef]
- Emanuel, E.J.; Persad, G.; Upshur, R.; Thome, B.; Parker, M.; Glickman, A.; Zhang, C.; Boyle, C.; Smith, M.; Phillips, J.P. Fair Allocation of Scarce Medical Resources in the Time of Covid-19. N. Engl. J. Med. 2020, 382, 2049–2055. [Google Scholar] [CrossRef]
- Solnica, A.; Barski, L.; Jotkowitz, A. Allocation of scarce resources during the COVID-19 pandemic: A Jewish ethical perspective. J. Med. Ethics 2020, 46, 444–446. [Google Scholar] [CrossRef] [Green Version]
- Yu, H.; Liu, Y.; Zhao, J.; Li, G. Urban total factor productivity: Does urban spatial structure matter in China? Sustainability 2019, 12, 214. [Google Scholar] [CrossRef] [Green Version]
- Cavallo, R.; Komossa, S.; Marzot, N.; Pont, M.B.; Kuijper, J. (Eds.) The Inevitable Spatial Blend: Infrastructures and City: Between New and Old Urban Configurations; IOS Press: Amsterdam, The Netherlands, 2014; pp. 387–392. [Google Scholar] [CrossRef]
- Si, Z.; Ying, Z. Research on the spatial layout of medical facilities in Beijing from the perspective of international comparative. City Plan. Rev. 2020, 44, 47–54, 89. [Google Scholar] [CrossRef]
- Luo, B.; Xia, W.; Wei, Q.; Zhang, Q. Rethink Profoundly on the Special Planning of Urban Medical and Health Facilities Under the Background of COVID-19: An Empirical Analysis of Wuhan. Mod. Urban Res. 2020, 10, 2–11. [Google Scholar] [CrossRef]
- Chen, Y.; Song, J.; Lin, X. Nanjing Urban-rural Medical Facilities Planning. Planners 2013, 29, 83–88. [Google Scholar] [CrossRef]
- Ma, C.; Song, Z.; Zong, Q. Urban-rural inequality of opportunity in health care: Evidence from China. Int. J. Environ. Res. Public Health 2021, 18, 7792. [Google Scholar] [CrossRef]
- Liu, P.; Guo, W.; Liu, H.; Hua, W.; Xiong, L. The integration of urban and rural medical insurance to reduce the rural medical burden in China: A case study of a county in Baoji City. BMC Health Serv. Res. 2018, 18, 796. [Google Scholar] [CrossRef] [Green Version]
- Melvin, S.C.; Wiggins, C.; Burse, N.; Thompson, E.; Monger, M. The role of public health in COVID-19 emergency response efforts from a rural health perspective. Prev. Chronic Dis. 2020, 17, E70. [Google Scholar] [CrossRef]
- Wagner, T.; Ramirez, C.; Godoy, B. Covid-19 rural health inequities: Insights from a real-world scenario. J. Commun. Healthc. 2022, 15, 22–26. [Google Scholar] [CrossRef]
- Silver, A. Could rural China’s healthcare deal with COVID-19? BMJ 2021, 375, n2759. [Google Scholar] [CrossRef]
- Yang, Z.; Zhu, X.; Moodie, D. Optimization of land use in a new urban district. J. Urban Plan. Dev. 2014, 141, 05014010. [Google Scholar] [CrossRef]
- Zhuang, L.; Ye, C. Disorder or reorder? The spatial production of state-level new areas in China. Sustainability 2018, 10, 3628. [Google Scholar] [CrossRef] [Green Version]
- He, Y. Reflections on the COVID-19 pandemic: A perspective from China. Aust. Soc. Work. 2021, 74, 519–520. [Google Scholar] [CrossRef]
- Wei, Y.; Sha, F.; Zhao, Y.; Jiang, Q.; Hao, Y.; Chen, F. Better modelling of infectious diseases: Lessons from COVID-19 in China. BMJ 2021, 375, n2365. [Google Scholar] [CrossRef]
- People’s Government of Heilongjiang Province. Harbin Announced 72 Fever Clinics. Available online: https://www.hlj.gov.cn/n200/2020/0123/c43-10918604.html (accessed on 28 January 2020).
- Boots, B.N. Weighting Thiessen Polygons. In Economic Geography; Taylor & Francis, Ltd.: Abingdon, UK, 2016; Volume 56, pp. 248–259. [Google Scholar] [CrossRef]
- Liu, L.; Wang, L. A study on spatial distribution of fever clinics in Shanghai during the epidemic of COVID-19 pneumonia. Shanghai Urban Plan. Rev. 2020, 2, 87–93, 98. [Google Scholar]
- Liu, J.; Zhu, Q. Research of equalizing layout of public service facilities: Take health facilities of central six districts of Beijing for example. Urban Dev. Stud. 2016, 23, 6–11. [Google Scholar] [CrossRef]
- Health Commission of Anhui Province. Anhui: Redrawing the “Runway” for Township Health Centers. Available online: http://wjw.ah.gov.cn/public/7001/56213701.html (accessed on 13 July 2021).
- Department of Planning, Development and Information Technology. Statistical Bulletin of China’s Health Development in 2020. Available online: http://www.nhc.gov.cn/guihuaxxs/s10743/202107/af8a9c98453c4d9593e07895ae0493c8.shtml (accessed on 13 July 2021).
- Chen, J. Research on the layout and development direction of medical institutions in Beijing core area and Tongzhou District. Beijing Plan. Rev. 2019, 6, 95–98. [Google Scholar]
- Chen, Q.; Qi, Y. Discussion on spatial strategy of medical institutions in Guangzhou. In Space Governance for High-Quality Development—Proceedings of the 2020 China Urban Planning Annual Conference (17 Detailed Planning); Urban Planning Society of China: Beijing, China, 2021; pp. 277–282. [Google Scholar] [CrossRef]
- An, P.; Xu, Z.; Li, L. Exploration of the development of the medical system under the guidance of resilient cities—Take the state-level new area of Tianfu new area in Sichuan province as an example. In Space Governance for High Quality Development 2021 China Urban Planning Annual Conference (01 Urban Safety and Disaster Prevention Planning); Urban Planning Society of China: Beijing, China, 2021; pp. 434–445. [Google Scholar] [CrossRef]
- Pal, D.; Ghosh, D.; Santra, P.K.; Mahapatra, G.S. Mathematical analysis of a COVID-19 epidemic model by using data driven epidemiological parameters of diseases spread in India. Biophysics 2022, 67, 231–244. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).