Abstract
Exposure to metals poses potential health risks, including insulin resistance (IR), to those exposed to them in excess. Limited studies have examined such risks in occupational workers, including welders, and these have yielded inconsistent results. Thus, we examined the associations between exposure to welding metals and IR in welders. We recruited 78 welders and 75 administrative staff from a shipyard located in northern Taiwan. Personal exposure to heavy metals, including chromium (Cr), manganese (Mn), iron (Fe), nickel (Ni), copper (Cu), zinc (Zn), and cadmium (Cd), was monitored through particulate matter with an aerodynamic diameter of less than 2.5 μm (PM2.5) and urine analysis by inductively coupled plasma mass spectrometry (ICP–MS). After each participant fasted overnight, blood samples were collected and analyzed for IR assessment through updated homeostasis model assessment (HOMA2) modeling. Air sampling in the personal breathing zone was performed during a Monday shift prior to the blood and urine sample collection the following morning. The welders’ median personal Cr, Mn, Fe, Ni, Cu, and Zn airborne PM2.5 levels and urinary Cd levels were significantly higher than those of the administrative staff. After adjustment for covariates, logarithmic PM2.5-Mn, PM2.5-Fe, PM2.5-Cu, and PM2.5-Zn levels were positively correlated with logarithmic fasting plasma glucose (P-FGAC) levels (PM2.5-Mn: β = 0.0105, 95% C.I.: 0.0027–0.0183; PM2.5-Fe: β = 0.0127, 95% C.I.: 0.0027–0.0227; PM2.5-Cu: β = 0.0193, 95% C.I.: 0.0032–0.0355; PM2.5-Zn: β = 0.0132, 95% C.I.: 0.0005–0.0260). Logarithmic urinary Zn was positively correlated with logarithmic serum insulin and HOMA2-IR levels and negatively correlated with logarithmic HOMA2-insulin sensitivity (%S; βinsulin = 0.2171, 95% C.I.: 0.0025–0.4318; βIR = 0.2179, 95% C.I.: 0.0027–0.4330; β%S = −0.2180, 95% C.I.: −0.4334 to −0.0026). We observed that glucose homeostasis was disrupted by Mn, Fe, Cu, and Zn exposure through increasing P-FGAC and IR levels in shipyard welders.
1. Introduction
Widespread heavy metal hazards perturb both the workplace and environment. Exposure to heavy metals continues to generate serious health impacts on humans. Heavy metals, such as chromium (Cr), manganese (Mn), iron (Fe), nickel (Ni), copper (Cu), zinc (Zn), and cadmium (Cd), can disturb human metabolomics, contributing to morbidity and mortality [1,2]. Industrial processes remain the primary source of heavy metals that may cause impaired health and well-being for workers [3]. Therefore, the recognition, evaluation, and control of heavy metals in the workplace are vital measures for sustainable development in enterprises.
Insulin resistance (IR) is a systemic disorder defined as the compromised ability of insulin to regulate insulin-mediated glucose disposal or inhibit hepatic glucose production and adipose tissue lipolysis. IR also plays a substantial pathophysiological role in type 2 diabetes (T2DM) [4]. Long-term IR has been associated with several metabolic abnormalities and notable public health problems, including cardiovascular disease and abnormalities, visceral adiposity, endothelial dysfunction, kidney disease, hypertension, coronary artery disease, and dyslipidemias [5,6]. The deficiencies and excesses of trace elements were implicated in the increasing risk of T2DM through interfering with blood glucose homeostasis [7,8].
Essential metals, such as Mn, Fe, Cu, and Zn, are essential for the function of various enzymatic systems of the human body. For example, Zn is required for insulin biosynthesis and crystallization, activation of the kinase 3 phosphatidylinositol enzyme, and induction of the translocation of glucose transporter 4 [9,10]. However, an excess intake of these metals could consequently lead to an increased risk of IR. An overload of Fe could modify hepatocytes’ insulin sensitivity by interfering with insulin receptors and intracellular insulin signaling [11]. Additionally, exposure to Cu in excess could create oxidative stress, a factor in the onset and progression of T2DM [12].
In addition to essential metals, toxic metals without any known biological function, such as Cd, have been associated with an increase in the occurrence of diabetes and the risk of metabolic syndrome [13]. The metals could affect hormone states by substituting for essential metals, such as Fe and Zn, in biological systems. Additionally, in vitro models illustrated that metals can catalyze an oxidative stress reaction that leads to decreased insulin gene promoter activity and insulin messenger ribonucleic acid (mRNA) expression in islet β-cells [7].
Both essential and toxic metals are unambiguously present in the environment, and pollution sources could result in various metal profiles [14,15]. Industrial process and operations, such as welding, mining, and refining, continue to be prominent sources of metals and produce unique metal mixtures [15]. Our biomonitoring studies determined that welding fumes heavily contain Cr, Mn, Fe, Ni, Cu, Zn, and Cd. Welders experienced higher concentrations of those metals in their urine than did administrative staff who did not work in welding [16].
Epidemiological studies have investigated the impact of metal exposure on IR responses in the general population [17,18], but these studies have yielded inconsistent results because most of them only measured limited metals. Few studies have examined the associations between metal exposure and insulin homeostasis in occupational workers, including welders. Thus, the evaluation of heavy metals in the workplace and their associations with IR are essential measures of sustainable development in enterprises. This study (1) quantified personal exposure to metals in particulate matter with an aerodynamic diameter of less than 2.5 μm (PM2.5) in welding fumes (2) evaluated the IR of welders and administrative staff and (3) identified associations between exposure to metals from welding fumes and IR in welders and administrative staff.
2. Materials and Methods
2.1. Ethics
The Institutional Review Board of Tri-Service General Hospital, National Defense Medical Center, Taiwan, approved this study (TSGHIRB 2-106-05-180). All participants voluntarily provided informed consent.
2.2. Study Participants
We conducted a cross-sectional study and recruited 153 healthy male workers, comprising 78 welders and 75 administrative staff, from a shipyard located in northern Taiwan (Figure 1). The welders served as the exposed group that had been chronically exposed to heavy metals, and the administrative staff served as the reference group. We collected participants’ airborne PM2.5 samples during a Monday shift prior to a physical examination and collected blood and urine samples on Tuesday. Selection criteria comprised men aged 20–65 years with >1 year of employment in the plant, no diagnosis of diabetes or cardiovascular diseases, and no moderate to severe renal dysfunction. Renal function was estimated using the Taiwanese modification of diet in renal disease (TMDRD) formula [19,20]. We also excluded participants with a diagnosis of diabetes or cardiovascular diseases. Trained interviewers met the participants to collect their demographic information, namely age, work experience, height, weight, waist circumference, number of years working in the shipyard, health condition, and information on lifestyle habits, encompassing cigarette smoking and alcohol consumption. Numerous studies have reported that social smokers or occasional smokers are exposed to various health threats, including cardiovascular diseases [21]. Participants who stated that they had no habit of smoking were defined as nonsmokers. Alcohol intake was deemed positive if intake occurred at least 4 days per week.
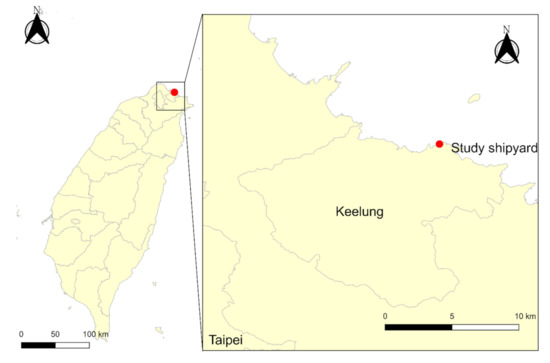
Figure 1.
Geographic location of the study shipyard.
2.3. Exposure Assessment for Metals in Workplace Air
All participants were requested to wear a Personal Environmental Monitor (PEM, SKC Ltd., Blandford, Dorset, UK) sampler with polytetrafluoroethylene filters (diameter: 37 mm, pore size: 0.45 μm, Cat. No. 225-17-04, SKC Ltd.) at a flow rate of 2.0 L/min during their working hours to monitor their personal PM2.5 levels of seven targeted heavy metals, namely Cr, Mn, Fe, Ni, Cu, Zn, and Cd. The levels of the targeted heavy metals in the shipyard workers’ personal breathing zone were quantified using inductively coupled plasma mass spectrometry (ICP-MS, iCAP RQ, Thermo Scientific, Waltham, MA, USA) combined with microwave-assisted acid digestion, which provides superior detectability of trace elements [22,23]. The detection limits of Cr, Mn, Fe, Ni, Cu, Zn, and Cd were 5.3, 3.0, 12.3, 5.7, 2.9, 17.9, and 0.7 ng/L, respectively, and were obtained using seven repeated analyses of deionized water. The measured levels below the lower detection limit were imputed using a monotone imputation method (IBM SPSS 22.0, IBM Corp., Armonk, NY, USA). We also collected data from the nearest Taiwan Environmental Protection Agency’s (TWEPA’s) monitoring station in Keelung from the same time period as the personal air sampling to use as control levels.
2.4. Urinary Metal Determination
Urine samples were collected using BD centrifuge tubes (Becton, Dickinson and Company, Franklin Lakes, NJ, USA) and stored at −80 °C until analysis. They were prepared through centrifugation of samples at 1500× g for 10 min to remove the supernatant, followed by dilution three times with 1.3% nitric acid (HNO3), filtration through a 0.22-μm syringe filter, and storage in a plastic centrifuge tube for measuring heavy metals. The levels of Cr, Mn, Fe, Ni, Cu, Zn, and Cd were quantified using inductively coupled plasma mass spectrometry (ICP-MS, iCAP RQ, Thermo Scientific). The detection limits of Cr, Mn, Fe, Ni, Cu, Zn, and Cd were 5.3, 3.0, 12.3, 5.7, 2.9, 17.9, and 0.7 ng/L, respectively, and were obtained using seven repeated analyses of deionized water. The measured levels below the lower detection limit were imputed using a monotone imputation method (IBM SPSS 22.0, IBM Corp.).
2.5. Biochemical Assays
Blood specimens were collected using the BD Vacutainer system (Becton, Dickinson and Company), and biochemical assays were performed immediately after collection. The hexokinase method was used for analyzing fasting plasma glucose (P-FGAC), glycerol phosphate dehydrogenase method for serum triglycerides (S-TGs), catalase elimination method for serum high density lipoprotein (S-HDL), Jaffe method for creatinine, chemiluminescence method for serum insulin (S-insulin), and high-performance liquid chromatography method for blood glycated hemoglobin (B-HbA1c) levels. The levels of P-FGAC, S-TG, S-HDL, and creatinine were measured using the automated ADVIA Chemistry XPT system (Siemens Healthineers AG, Erlangen, Germany) [24]. The S-insulin level was determined using the automated ADVIA Centaur XPT system (Siemens Healthineers AG) [25], and the B-HbA1c level was quantified using the automated D-100 System (Bio-Rad Laboratories, Inc., Hercules, CA, USA) [26].
2.6. Updated Homeostatic Model Assessment
The parameters of the updated Homeostatic Model Assessment (HOMA2), namely estimated insulin resistance (IR), β cell function (%B), and insulin sensitivity (%S), were obtained using the HOMA2 calculator software developed by the Diabetes Trials Unit at the University of Oxford [27].
2.7. Statistical Analysis
Because of the skewness of the continuous variables, especially the metals (Cr, Mn, Fe, Ni, Cu, Zn, and Cd) and biochemical markers (P-FGAC, S-insulin, and B-HbA1c), descriptive statistics were described as the median and 25th–75th percentile. Categorical variables were described as frequency and percent in descriptive statistics. In inferential statistics, to compare the differences in values and frequencies of risk factors and outcomes between the exposed and reference groups, the Mann–Whitney U and χ2 tests were applied. All data from the shipyard welders were then included in single-pollutant multiple linear regression to identify the significant and risky metals to welders’ P-FGAC, S-insulin, B-HbA1c, HOMA2-IR, HOMA2-%B, and HOMA2-%S levels. The welders’ ages, smoking habits, alcohol intake, respirator usage, T2DM family histories, body mass indexes (BMIs), background PM2.5 levels, and urinary creatinine levels served as covariates. The multiple linear regression formula is expressed as follows:
where β0 + β1×1 + β2×2 + … + βn×n represents the best fit line for the data points in the coordinate system of the regression model, and ε is the residual, which represents the deviation of observed y values from their mean. We also adopted a wild-bootstrap process integrated in IBM SPSS statistics software for Windows version 22.0 (IBM SPSS 22.0, IBM Corp.) to quantify the uncertainty estimation of the glucose homeostasis markers. The number of samples was set to 1000, and the results of the uncertainty analysis are presented in the Supplementary Materials. Statistical significance was set at α = 0.05 in all tests. Statistical analysis was conducted using IBM SPSS statistics software.
y = β0 + β1x1 + β2x2 + … + βnxn + ε.
3. Results
3.1. Characteristics of Study Participants
The demographic characteristics of the 153 workers by job title are presented in Table 1. The study population consisted of 78 welders with an average age of 46.7 ± 11.1 years who served as welders for an average of 24.6 ± 15.8 years and 75 administrative staff with an average age of 44.1 ± 13.4 who served as administrative staff for an average of 18.9 ± 16.5 years. No statistically significant differences were noted in age or alcohol intake proportion between the welders and administrative staff. However, compared with the administrative staff, the welders had served significantly more years in their profession, had increased smoking habits, wore respirators during their shift more often, and had significantly lower proportions of high school diplomas and family histories of T2DM.

Table 1.
Sociodemographic characteristics of participants by job title.
3.2. Comparisons of PM2.5 and Urinary Metal Levels between Exposed and Reference Groups
A comparison of the median levels of personal air sampling PM2.5, background PM2.5, and metals in the PM2.5, and urine between the welders and administrative staff is presented in Table 2. The median personal sampling, Cr, Mn, Fe, Ni, Cu, Zn, and Cd PM2.5 concentrations of the welders were 1013.1, 0.224, 40.25, 200.9, 0.120, 0.653, 30.2, and 0.0072 μg/m3, respectively, and significantly exceeded the median levels of the administrative staff, which measured 185.0, 0.055, 0.63, 7.9, 0.067, 0.167, 5.9, and 0.0036 μg/m3, respectively. Furthermore, the median urinary Cd concentration of welders (0.66 ng/mL) was significantly higher than that of the administrative staff (0.57 ng/mL). No statistically significant differences in the background PM2.5 levels were observed between the welders and administrative staff.

Table 2.
PM2.5 and urinary metal levels by job title.
3.3. Comparisons of Physical and Biochemical Markers between Exposed and Reference Groups
A comparison of the physical and biochemical markers, including the HOMA2 parameters, between the welders and administrative staff is presented in Table 3. The median P-FGAC and HOMA2-%S of welders (P-FGAC: 95.0 mg/dL; HOMA2-%S: 88.0 mg/dL) were significantly higher than those of the administrative staff (P-FGAC: 91.0 mg/dL; HOMA2–%S: 67.6 mg/dL). By contrast, the median waist circumference and S-insulin, HOMA2-IR, and HOMA2–%B levels of the welders (waist circumference: 85.0 cm; S-insulin: 8.6 mU/L; HOMA2-IR: 1.13 mU/L; HOMA2-%B: 92.8 mU/L) were significantly lower than those of the administrative staff (waist circumference: 89.0 cm; S-insulin: 11.8 mU/L; HOMA2-IR: 1.48 mU/L; HOMA2-%B: 117.3 mU/L). The differences in BMI, systolic blood pressure (SBP), diastolic blood pressure (DBP), and levels of B-HbA1c, S-triglycerides, S-HDL, and serum and urinary creatinine between the welders and administrative staff did not reach statistical significance. Notably, the eGFR obtained by adopting the TMDRD formula was significantly lower in the welders (79.5 mL/min/1.73 m2) than in the administrative staff (85.4 mL/min/1.73 m2).

Table 3.
Physical and biochemical markers by job title.
3.4. Correlation between Metals in PM2.5 and Urinary Excretion of Metals
The correlation among the logarithmized levels of personal air sampling PM2.5, metals in PM2.5, and the urinary excretion of metals in the 78 shipyard welders is presented in Table 4. Personal air sampling PM2.5 was significantly and positively correlated with U-Zn and U-Cd, and PM2.5–Zn levels were significantly and positively correlated with U-Zn.

Table 4.
Spearman’s correlation coefficients among logarithmized PM2.5 and urinary metals in shipyard welders. (n = 78).
3.5. Effects of Metals in PM2.5 on Plasma Glucose, S-Insulin, B-HbA1c, and HOMA2 Parameters
The effects of metals in PM2.5 on the P-FGAC, S-insulin, B-HbA1c, and HOMA2 parameters in the unadjusted model and the covariate-adjusted model in welders are presented in Table 5. After adjustment for covariates, namely age, smoking status, alcohol intake, regular use of a respirator during work, family history of T2DM, BMI, and background PM2.5, we observed that the logarithmized PM2.5-Mn, PM2.5-Fe, PM2.5-Cu, and PM2.5-Zn levels were significantly and positively correlated with the logarithmized P-FGAC (Mn: β = 0.0105, 95% C.I.: 0.0027–0.0183; Fe: β = 0.0127, 95% C.I.: 0.0027–0.0227; Cu: β = 0.0193, 95% C.I.: 0.0032–0.0355; Zn: β = 0.0132, 95% C.I.: 0.0005–0.0260).

Table 5.
Effects of PM2.5 metals on glucose homeostasis markers in shipyard welders. (n = 78).
3.6. Effects of Urinary Metals on Plasma Glucose, S-Insulin, B-HbA1c, and HOMA2 Parameters
The effects of urinary metals on the P-FGAC, S-insulin, B-HbA1c, and HOMA2 parameters in the unadjusted and covariate-adjusted models for welders are presented in Table 6. After adjusting for the covariates, namely age, smoking status, alcohol intake, regular use of respirator during work, family history of T2DM, BMI, and urinary creatinine, we observed that the logarithmized U-Zn was significantly correlated with increased logarithmized S-insulin and HOMA2-IR levels (βinsulin = 0.2171, 95% C.I.: 0.0025–0.4318; βIR = 0.2179, 95% C.I.: 0.0027–0.4330) and decreased logarithmized HOMA2-%S levels (β%S = −0.2180, 95% C.I.: −0.4334 to −0.0026).

Table 6.
Effects of urinary metals on glucose homeostasis markers in shipyard welders. (n = 78).
4. Discussion
We provided evidence of the relationships among PM2.5 metals, urinary metals, and biomarkers linked to glucose homeostasis and IR measures. Notably, higher Mn, Fe, Cu, and Zn levels in PM2.5 were significantly associated with increased P-FGAC. Urinary Zn was also significantly linked to IR measures in shipyard welders. Exposure to metals in welding fumes in a shipyard environment may increase the risk of diabetes. To our knowledge, this study is the first to examine the glucose homeostasis and IR responses induced by metal exposure in shipyard welders.
Typical risk factors of developing IR and prediabetes include a family history of T2DM, an age of ≥45 years, being overweight or obese, a lack of physical activity, hypertension or hyperlipidemia, cigarette smoking, and excessive alcohol use [28]. In this study, most of the covariates in the linear regression analysis were adjusted for.
In this study, the PM2.5 impactor system was adopted to assess welding fume exposure. Most of the parent materials are mild steel used in welding processes for shipbuilding and repairing. Cena et al. investigated the particle size distributions of mild steel gas metal arc welding fumes and reported that a majority of particles in welding fumes had cutoff diameters ranging from 0.01 to 1.0 μm [29]. Additionally, Rice et al. revealed that PM2.5 can penetrate deep into the lungs, and therefore, lead to severe health problems [30]. We observed the median PM2.5-Mn level of the welders was higher than the American Conference of Governmental Industrial Hygienists’ (ACGIH’s) 20 μg/m3 threshold limit value (TLV) for respirable Mn fumes. Both the welders’ and administrative staff’s median PM2.5-Cd levels were lower than the ACGIH’s 2 μg/m3 TLV for respirable Cd, but the welders’ median levels of PM2.5-Cd and urinary Cd were significantly higher than the administrative staff’s. The median levels of PM2.5-Fe and PM2.5-Zn of the study participants were lower than the ACGIH’s TLV for respirable iron oxide and zinc oxide, and no significant difference was observed in urinary Fe and Zn levels between the exposed group and the unexposed controls. The welders had higher median exposure levels of PM2.5-Cr, PM2.5-Ni, and PM2.5-Cu than did the administrative staff. However, currently, neither the United States Occupational Safety and Health Administration, the United States National Institute for Occupational Safety and Health, nor the ACGIH have standards for respirable Cr, Ni, or Cu [31].
The relationship between occupational metal exposure and an increased risk of diabetes was reported in steel production workers [32], coke oven workers [33], and nonferrous metal production workers [34,35]. After adjusting for age, Cappelletti et al. determined a significant 1.39 times increase in the relative risk of diabetes in steel production workers compared with the general population from the same province [32]. Liu et al. observed that urinary Cu, Zn, and Cd levels were significantly higher in both diabetic and hyperglycemic coke oven workers compared with normoglycemic workers. Furthermore, the increased urinary Cu and Zn levels were related to the elevation of the diabetes and hyperglycemia odds ratios, respectively [33]. An epidemiological study revealed that significantly elevated high-fasting-glucose (fasting glucose ≥ 93.6 mg/dL) odds ratios were observed in the groups with the highest quartiles of urinary Ni (≥9.06 μg/L) and Zn (≥584.43 μg/L) levels. The trend tests of the quartiles of urinary Ni and Zn levels on the risks of high-FPG reached statistical significance [34]. Yang et al. also observed a significant increase in log-transformed P-FGAC in nonferrous production workers with urinary Zn levels over 369 μg/L; the trend tests of the quartiles of urinary Zn levels on P-FGAC also reached statistical significance [35]. The present study demonstrated the significant relationship between occupational Mn, Fe, Cu, and Zn exposure and blood glucose homeostasis in shipyard welders.
Although epidemiological studies have established the relationship between PM and the increased risk of T2DM, reports on the mechanisms for the relationship between inhaled metal particles and diabetes remain limited. Chuang et al. observed that intratracheal-instilled exposure to nanosized zinc oxide induced systemic inflammation and oxidative stress in Sprague–Dawley rats [36]. In an animal study, Pan et al. highlighted the metabolic mechanisms that may be essential to the responses to zinc oxide nanoparticles [37]. Pavanello et al. determined that steel production workers occupationally exposed to Fe, Ni, Cu, and Zn in PM10 (PM with an aerodynamic diameter of less than 10 μm) were positively associated with elevated expressions of micro-RNA miR-196b [38], which is involved in a posttranscriptional regulation mechanism of insulin biosynthesis in mice [39]. By contrast, these metals also play vital roles in regulating normal physiological functions involved in the homeostasis of glucose and insulin. For example, zinc ions target to tyrosine phosphatase 1B, which is a crucial regulator for insulin receptor phosphorylation [40]. Zinc also induces glucose transport into cells through enhancing the insulin signaling pathway [41]. Ahn et al. determined a significantly negative relationship between levels of serum zinc and HOMA-IR in a Korean general population without diabetes [42].
In this study, the urinary metals served as the biomarkers of exposure. Many metals, including Cd, that cause chronic kidney disease (CKD) [20,43,44,45] have also been associated with renal tubular dysfunction in welders [46]. Moreover, CKD is a common comorbid disease in patients with T2DM [47]. In this study, participants with an eGFR of less than 60 mL/min/1.73 m2 were excluded to avoid the confounding bias of renal dysfunction in the relationship between urinary metals and IR.
This study has certain limitations. First, the lack of data on dietary essential and micronutrient intake possibly confounded the results concerning urinary metal excretion. The other limitation was the lack of data on the exposure to metals outside occupational settings, such as from vehicle traffic emissions. However, the shipyard workers spent >10 h/day at the shipyard, including work and rest periods, but only <1 h/day in traffic. The contribution of traffic sources to the metal exposure of shipyard workers is thus assumed to be limited.
5. Conclusions
In the present study, the airborne Mn, Fe, Cu, and Zn levels in PM2.5 were observed as significant risk factors for P-FGAC. Urinary Zn was also significantly correlated with increasing IR measures. Because of the long-term development of diabetes, a follow-up study on the welders must be conducted. Furthermore, developing immediate preventive measures, including adequate ventilation and the use of personal protection equipment (gloves and respirators), to protect the health of shipyard workers is critical.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/su132413924/s1. Table S1: Effects of PM2.5 metals on Log P–FGAC (mg/dL) in shipyard welders, Table S2: Effects of PM2.5 metals on Log B–HbA1c (%) in shipyard welders, Table S3: Effects of PM2.5 metals on Log S–insulin (mU/L) in shipyard welders, Table S4: Effects of PM2.5 metals on Log HOMA2–IR in shipyard welders, Table S5: Effects of PM2.5 metals on Log HOMA2–%B in shipyard welders, Table S6: Effects of PM2.5 metals on Log HOMA2–%S in shipyard welders, Table S7: Effects of urinary metals on Log P–FGAC (mg/dL) in shipyard welders. (n = 78), Table S8: Effects of urinary metals on Log B–HbA1c (%) in shipyard welders. (n = 78); Table S9: Effects of urinary metals on Log S–insulin (mU/L) in shipyard welders. (n = 78); Table S10: Effects of urinary metals on Log HOMA2–IR in shipyard welders. (n = 78), Table S11: Effects of urinary metals on Log HOMA2–%B in shipyard welders. (n = 78), Table S12: Effects of urinary metals on Log HOMA2–%S in shipyard welders. (n = 78).
Author Contributions
Conceptualization, T.-Y.S., C.-H.L. and C.-H.P.; methodology, T.-Y.S. and C.-H.L.; software, C.-H.L.; validation, H.A.J., C.-H.L. and C.-H.P.; formal analysis, T.-Y.S. and Y.-T.H.; investigation, T.-Y.S. and Y.-T.H.; resources, C.-H.L.; data curation, C.-H.L.; writing—original draft preparation, T.-Y.S.; writing—review and editing, H.A.J.; visualization, T.-Y.S.; supervision, C.-H.L.; project administration, C.-H.P.; funding acquisition, C.-H.L. All authors have read and agreed to the published version of the manuscript.
Funding
This study was partially supported by grants from the Ministry of Science and Technology, Taiwan (MOST 107-2314-B-016-045-MY3).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of Tri-Service General Hospital, National Defense Medical Center in Taiwan (TSGHIRB 2-106-05-180 on 2018/02/14).
Informed Consent Statement
Informed consent was obtained from all participants involved in the study.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author C.-H.L. The data are not publicly available due to them containing information that could compromise research participant privacy.
Conflicts of Interest
The authors declare no competing interests.
Abbreviations
PM2.5 (particulate matters with an aerodynamic diameter less than 2.5 μm); Cr (chromium); Mn (manganese); Fe (iron); Ni (nickel); Cu (copper); Zn (zinc); Cd (cadmium); BMI (body mass index); SBP (systolic blood pressure); DBP (diastolic blood pressure); P-FGAC (fasting plasma glucose); S-TG (serum triglycerides); S-HDL (serum high density lipoprotein); U-Creat (urinary creatinine); S-insulin (serum insulin); B-HbA1c (blood glycated hemoglobin); HOMA2-IR (updated homeostasis model assessment for insulin resistance); HOMA2-%B (updated homeostasis model assessment for β cell function); HOMA2-%S (updated homeostasis model assessment for insulin sensitivity); T2DM (type 2 diabetes mellitus).
References
- Fu, Z.; Xi, S. The effects of heavy metals on human metabolism. Toxicol. Mech. Methods 2020, 30, 167–176. [Google Scholar] [CrossRef]
- Rai, P.K.; Lee, S.S.; Zhang, M.; Tsang, Y.F.; Kim, K.H. Heavy metals in food crops: Health risks, fate, mechanisms, and management. Environ. Int. 2019, 125, 365–385. [Google Scholar] [CrossRef] [PubMed]
- Roig-Navarro, A.F.; Lopez, F.J.; Serrano, R.; Hernandez, F. An assessment of heavy metals and boron contamination in workplace atmospheres from ceramic factories. Sci. Total. Environ. 1997, 201, 225–234. [Google Scholar] [CrossRef]
- Chatterjee, S.; Khunti, K.; Davies, M.J. Type 2 diabetes. Lancet 2017, 389, 2239–2251. [Google Scholar] [CrossRef]
- Petersen, K.F.; Dufour, S.; Savage, D.B.; Bilz, S.; Solomon, G.; Yonemitsu, S.; Cline, G.W.; Befroy, D.; Zemany, L.; Kahn, B.B.; et al. The role of skeletal muscle insulin resistance in the pathogenesis of the metabolic syndrome. Proc. Natl. Acad. Sci. USA 2007, 104, 12587–12594. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- DeFronzo, R.A.; Ferrannini, E. Insulin resistance. A multifaceted syndrome responsible for NIDDM, obesity, hypertension, dyslipidemia, and atherosclerotic cardiovascular disease. Diabetes Care 1991, 14, 173–194. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.W.; Yang, C.Y.; Huang, C.F.; Hung, D.Z.; Leung, Y.M.; Liu, S.H. Heavy metals, islet function and diabetes development. Islets 2009, 1, 169–176. [Google Scholar] [CrossRef] [Green Version]
- Feng, W.; Cui, X.; Liu, B.; Liu, C.; Xiao, Y.; Lu, W.; Guo, H.; He, M.; Zhang, X.; Yuan, J.; et al. Association of urinary metal profiles with altered glucose levels and diabetes risk: A population-based study in China. PLoS ONE 2015, 10, e0123742. [Google Scholar]
- Kelishadi, R.; Hashemipour, M.; Adeli, K.; Tavakoli, N.; Movahedian-Attar, A.; Shapouri, J.; Poursafa, P.; Rouzbahani, A. Effect of zinc supplementation on markers of insulin resistance, oxidative stress, and inflammation among prepubescent children with metabolic syndrome. Metab. Syndr. Relat. Disord. 2010, 8, 505–510. [Google Scholar] [CrossRef]
- Ranasinghe, P.; Pigera, S.; Galappatthy, P.; Katulanda, P.; Constantine, G.R. Zinc and diabetes mellitus: Understanding molecular mechanisms and clinical implications. Daru 2015, 23, 44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fargion, S.; Dongiovanni, P.; Guzzo, A.; Colombo, S.; Valenti, L.; Fracanzani, A.L. Iron and insulin resistance. Aliment. Pharmacol. Ther. 2005, 22 (Suppl. S2), 61–63. [Google Scholar] [CrossRef]
- Bjorklund, G.; Dadar, M.; Pivina, L.; Dosa, M.D.; Semenova, Y.; Aaseth, J. The role of zinc and copper in insulin resistance and diabetes mellitus. Curr. Med. Chem. 2020, 27, 6643–6657. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.K.; Kim, Y. Blood cadmium, mercury, and lead and metabolic syndrome in South Korea: 2005–2010 Korean National Health and Nutrition Examination Survey. Am. J. Ind. Med. 2013, 56, 682–692. [Google Scholar] [CrossRef]
- Suvarapu, L.N.; Baek, S.O. Determination of heavy metals in the ambient atmosphere. Toxicol. Ind. Health 2017, 33, 79–96. [Google Scholar] [CrossRef]
- Anyanwu, B.O.; Ezejiofor, A.N.; Igweze, Z.N.; Orisakwe, O.E. Heavy Metal Mixture Exposure and Effects in Developing Nations: An Update. Toxics 2018, 6, 65. [Google Scholar] [CrossRef] [Green Version]
- Lai, C.H.; Chou, C.C.; Chuang, H.C.; Lin, G.J.; Pan, C.H.; Chen, W.L. Receptor for advanced glycation end products in relation to exposure to metal fumes and polycyclic aromatic hydrocarbon in shipyard welders. Ecotoxicol. Environ. Saf. 2020, 202, 110920. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Yang, A.; Cheng, N.; Huang, W.; Huang, P.; Liu, N.; Bai, Y. Sex-specific associations of blood and urinary manganese levels with glucose levels, insulin resistance and kidney function in US adults: National health and nutrition examination survey 2011–2016. Chemosphere 2020, 258, 126940. [Google Scholar] [CrossRef]
- Wallia, A.; Allen, N.B.; Badon, S.; El Muayed, M. Association between urinary cadmium levels and prediabetes in the NHANES 2005–2010 population. Int. J. Hyg. Environ. Health 2014, 217, 854–860. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, L.I.; Guh, J.Y.; Wu, K.D.; Chen, Y.M.; Kuo, M.C.; Hwang, S.J.; Chen, T.H.; Chen, H.C. Modification of diet in renal disease (MDRD) study and CKD epidemiology collaboration (CKD-EPI) equations for Taiwanese adults. PLoS ONE 2014, 9, e99645. [Google Scholar] [CrossRef] [PubMed]
- Jin, R.; Zhu, X.; Shrubsole, M.J.; Yu, C.; Xia, Z.; Dai, Q. Associations of renal function with urinary excretion of metals: Evidence from NHANES 2003–2012. Environ. Int. 2018, 121, 1355–1362. [Google Scholar] [CrossRef]
- Schane, R.E.; Ling, P.M.; Glantz, S.A. Health effects of light and intermittent smoking: A review. Circulation 2010, 121, 1518–1522. [Google Scholar] [CrossRef]
- Dabek-Zlotorzynska, E.; Celo, V.; Ding, L.; Herod, D.; Jeong, C.-H.; Evans, G.; Hilker, N. Characteristics and sources of PM2.5 and reactive gases near roadways in two metropolitan areas in Canada. Atmos. Environ. 2019, 218, 116980. [Google Scholar] [CrossRef]
- Celo, V.; Dabek-Zlotorzynska, E.; Mathieu, D.; Okonskaia, I. Validation of a simple microwave-assisted acid digestion method using microvessels for analysis of trace elements in atmospheric PM2. 5 in monitoring and fingerprinting studies. Open Chem. Biomed. Methods. J. 2010, 3, 143–152. [Google Scholar]
- Tahmasebi, H.; Higgins, V.; Woroch, A.; Asgari, S.; Adeli, K. Pediatric reference intervals for clinical chemistry assays on Siemens ADVIA XPT/1800 and Dimension EXL in the CALIPER cohort of healthy children and adolescents. Clin. Chim. Acta. 2019, 490, 88–97. [Google Scholar] [CrossRef]
- Li, H.; Wang, D.; Guo, X.; Xia, L.; Wu, Q.; Cheng, X. Comparison of four matrixes for diluting insulin in routine clinical measurements. J. Clin. Lab. Anal. 2020, 34, e23396. [Google Scholar] [CrossRef]
- Jaisson, S.; Leroy, N.; Guillard, E.; Desmons, A.; Gillery, P. Analytical performances of the D-100TM hemoglobin testing system (Bio-Rad) for HbA1c assay. Clin. Chem. Lab. Med. 2015, 53, 1473–1479. [Google Scholar] [CrossRef]
- The Diabetes Trials Unit, University of Oxford HOMA2 Calculator. Available online: https://www.dtu.ox.ac.uk/homacalculator/ (accessed on 1 July 2021).
- American Diabetes Association. 2. Classification and Diagnosis of Diabetes. Diabetes Care 2017, 40 (Suppl. S1), S11–S24. [Google Scholar] [CrossRef] [Green Version]
- Cena, L.G.; Chisholm, W.P.; Keane, M.J.; Cumpston, A.; Chen, B.T. Size Distribution and Estimated Respiratory Deposition of Total Chromium, Hexavalent Chromium, Manganese, and Nickel in Gas Metal Arc Welding Fume Aerosols. Aerosol. Sci. Technol. 2014, 48, 1254–1263. [Google Scholar] [CrossRef] [PubMed]
- Rice, M.B.; Ljungman, P.L.; Wilker, E.H.; Dorans, K.S.; Gold, D.R.; Schwartz, J.; Koutrakis, P.; Washko, G.R.; O’Connor, G.T.; Mittleman, M.A. Long-term exposure to traffic emissions and fine particulate matter and lung function decline in the Framingham heart study. Am. J. Respir. Crit. Care Med. 2015, 191, 656–664. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- United States Occupational Safety and Health Administration Permissible Exposure Limits—Annotated Tables. Available online: https://www.osha.gov/annotated-pels/table-z-1 (accessed on 18 March 2021).
- Cappelletti, R.; Ceppi, M.; Claudatus, J.; Gennaro, V. Health status of male steel workers at an electric arc furnace (EAF) in Trentino, Italy. J. Occup. Med. Toxicol. 2016, 11, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, B.; Feng, W.; Wang, J.; Li, Y.; Han, X.; Hu, H.; Guo, H.; Zhang, X.; He, M. Association of urinary metals levels with type 2 diabetes risk in coke oven workers. Environ. Pollut. 2016, 210, 1–8. [Google Scholar] [CrossRef]
- Yang, A.; Liu, S.; Cheng, N.; Pu, H.; Dai, M.; Ding, J.; Li, J.; Li, H.; Hu, X.; Ren, X.; et al. Multiple metals exposure, elevated blood glucose and dysglycemia among Chinese occupational workers. J. Diabetes Complicat. 2017, 31, 101–107. [Google Scholar] [CrossRef]
- Yang, A.; Liu, S.; Cheng, Z.; Pu, H.; Cheng, N.; Ding, J.; Li, J.; Li, H.; Hu, X.; Ren, X.; et al. Dose-response analysis of environmental exposure to multiple metals and their joint effects with fasting plasma glucose among occupational workers. Chemosphere 2017, 186, 314–321. [Google Scholar] [CrossRef] [PubMed]
- Chuang, H.C.; Juan, H.T.; Chang, C.N.; Yan, Y.H.; Yuan, T.H.; Wang, J.S.; Chen, H.C.; Hwang, Y.H.; Lee, C.H.; Cheng, T.J. Cardiopulmonary toxicity of pulmonary exposure to occupationally relevant zinc oxide nanoparticles. Nanotoxicology 2014, 8, 593–604. [Google Scholar] [CrossRef]
- Pan, C.H.; Chuang, K.J.; Chen, J.K.; Hsiao, T.C.; Lai, C.H.; Jones, T.P.; BeruBe, K.A.; Hong, G.B.; Ho, K.F.; Chuang, H.C. Characterization of pulmonary protein profiles in response to zinc oxide nanoparticles in mice: A 24-hour and 28-day follow-up study. Int. J. Nanomed. 2015, 10, 4705–4716. [Google Scholar]
- Pavanello, S.; Bonzini, M.; Angelici, L.; Motta, V.; Pergoli, L.; Hoxha, M.; Cantone, L.; Pesatori, A.C.; Apostoli, P.; Tripodi, A.; et al. Extracellular vesicle-driven information mediates the long-term effects of particulate matter exposure on coagulation and inflammation pathways. Toxicol. Lett. 2016, 259, 143–150. [Google Scholar] [CrossRef]
- Panda, A.C.; Sahu, I.; Kulkarni, S.D.; Martindale, J.L.; Abdelmohsen, K.; Vindu, A.; Joseph, J.; Gorospe, M.; Seshadri, V. miR-196b-mediated translation regulation of mouse insulin2 via the 5’UTR. PLoS ONE 2014, 9, e101084. [Google Scholar]
- Haase, H.; Maret, W. Protein tyrosine phosphatases as targets of the combined insulinomimetic effects of zinc and oxidants. Biometals 2005, 18, 333–338. [Google Scholar] [CrossRef] [PubMed]
- Tang, X.; Shay, N.F. Zinc has an insulin-like effect on glucose transport mediated by phosphoinositol-3-kinase and Akt in 3T3-L1 fibroblasts and adipocytes. J. Nutr. 2001, 131, 1414–1420. [Google Scholar] [CrossRef] [Green Version]
- Ahn, B.I.; Kim, M.J.; Koo, H.S.; Seo, N.; Joo, N.S.; Kim, Y.S. Serum zinc concentration is inversely associated with insulin resistance but not related with metabolic syndrome in nondiabetic Korean adults. Biol. Trace. Elem. Res. 2014, 160, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Tsai, T.L.; Kuo, C.C.; Pan, W.H.; Chung, Y.T.; Chen, C.Y.; Wu, T.N.; Wang, S.L. The decline in kidney function with chromium exposure is exacerbated with co-exposure to lead and cadmium. Kidney Int. 2017, 92, 710–720. [Google Scholar] [CrossRef] [PubMed]
- Ding, X.; Zhang, Q.; Wei, H.; Zhang, Z. Cadmium-induced renal tubular dysfunction in a group of welders. Occup. Med. (Lond.) 2011, 61, 277–279. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuo, C.C.; Navas-Acien, A. Commentary: Environmental chemicals and diabetes: Which ones are we missing? Int. J. Epidemiol. 2015, 44, 248–250. [Google Scholar] [CrossRef] [Green Version]
- Liu, G.; Sun, L.; Pan, A.; Zhu, M.; Li, Z.; ZhenzhenWang, Z.; Liu, X.; Ye, X.; Li, H.; Zheng, H.; et al. Nickel exposure is associated with the prevalence of type 2 diabetes in Chinese adults. Int. J. Epidemiol. 2015, 44, 240–248. [Google Scholar] [CrossRef] [PubMed]
- Thomas, M.C.; Cooper, M.E.; Zimmet, P. Changing epidemiology of type 2 diabetes mellitus and associated chronic kidney disease. Nat. Rev. Nephrol. 2016, 12, 73–81. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).