Contraceptive Method Information and Method Switching in India
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source and Sample Selection
2.2. Study Variables
2.3. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Variables | n | Reuse | Modern Method to Pill | Traditional Method to Pill | Modern Method to LARC | Traditional Method to LARC |
|---|---|---|---|---|---|---|
| Side effects * Manage to side effects * Other methods | ||||||
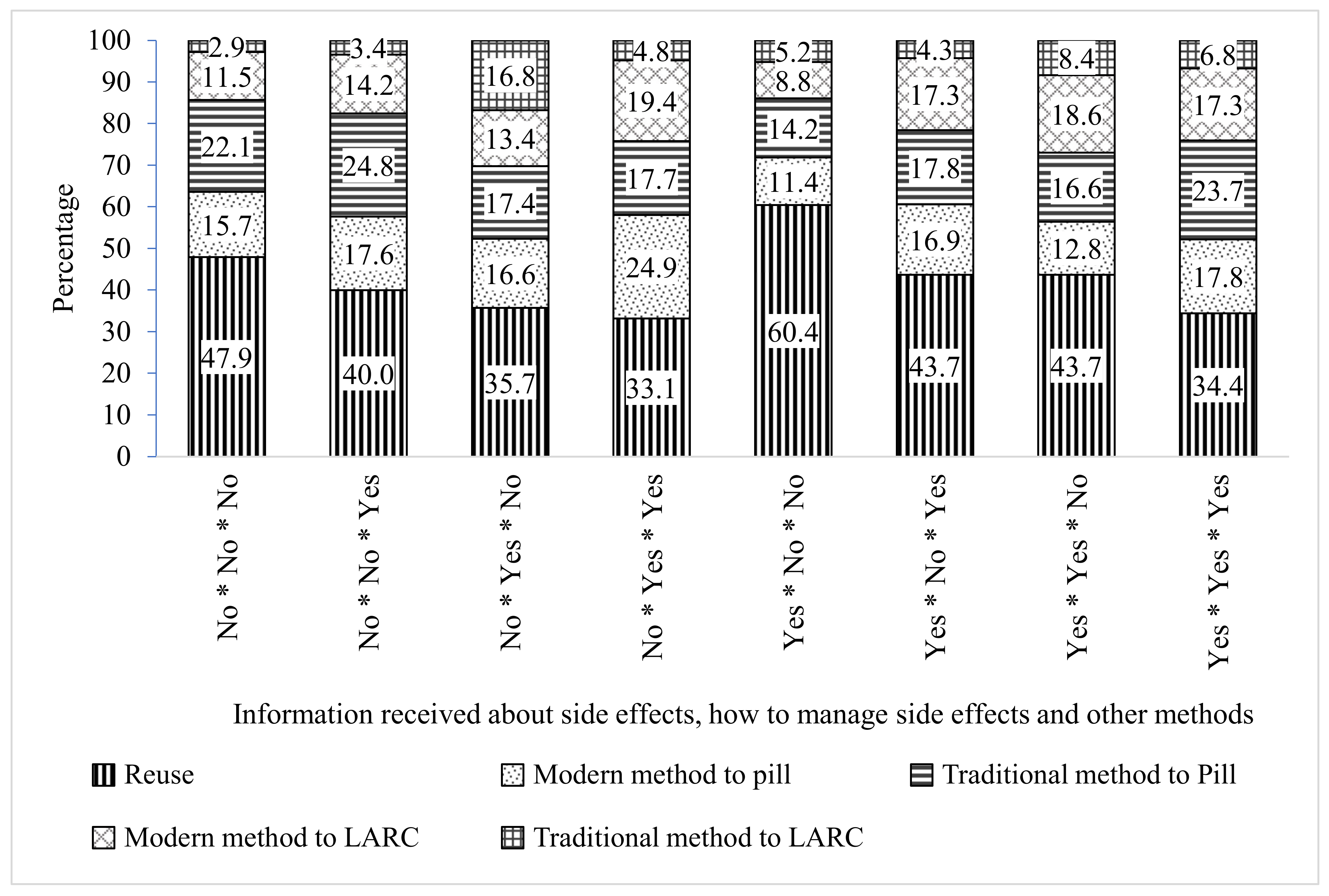
| No * No * No | 2414 | 47.9 (45.8, 49.9) | 15.7 (14.3, 17.3) | 22.1 (20.4, 23.8) | 11.5 (10.3, 12.8) | 2.9 (2.3, 3.6) |
| No * No * Yes | 1021 | 40.0 (37.1, 43.0) | 17.6 (15.4, 20.0) | 24.8 (22.3, 27.5) | 14.2 (12.2, 16.4) | 3.4 (2.5, 4.7) |
| No * Yes * No | 65 | 35.7 (23.7, 49.8) | 16.6 (8.6, 29.6) | 17.4 (9.2, 30.6) | 13.4 (6.4, 26.0) | 16.8 (8.7, 29.9) |
| No * Yes * Yes | 215 | 33.1 (26.7, 40.2) | 24.9 (19.2, 31.7) | 17.7 (12.9, 23.9) | 19.4 (14.4, 25.8) | 4.8 (2.5, 9.0) |
| Yes * No * No | 259 | 60.4 (53.7, 66.7) | 11.4 (7.8, 16.4) | 14.2 (10.1, 19.5) | 8.8 (5.7, 13.3) | 5.2 (2.9, 9.1) |
| Yes * No * Yes | 372 | 43.7 (38.6, 48.9) | 16.9 (13.4, 21.2) | 17.8 (14.1, 22.2) | 17.3 (13.7, 21.7) | 4.3 (2.6, 7.0) |
| Yes * Yes * No | 325 | 43.7 (38.1, 49.4) | 12.8 (9.4, 17.1) | 16.6 (12.7, 21.3) | 18.6 (14.5, 23.5) | 8.4 (5.7, 12.2) |
| Yes * Yes * Yes | 3854 | 34.4 (32.9, 35.9) | 17.8 (16.6, 19.0) | 23.7 (22.4, 25.1) | 17.3 (16.2, 18.6) | 6.8 (6.0, 7.6) |
| Women’s education | ||||||
| No education | 1716 | 44.5 (41.9, 47.1) | 14.4 (12.7, 16.3) | 24.8 (22.6, 27.1) | 10.5 (9.0, 12.2) | 5.8 (4.7, 7.1) |
| Primary | 1159 | 48.3 (45.7, 51.0) | 13.1 (11.3, 15.0) | 25.1 (22.8, 27.5) | 9.6 (8.1, 11.3) | 3.9 (3.0, 5.1) |
| Secondary | 4689 | 39.3 (37.9, 40.7) | 18.3 (17.2, 19.4) | 23.4 (22.2, 24.6) | 14.4 (13.4, 15.4) | 4.7 (4.1, 5.4) |
| Higher | 961 | 27.7 (25.0, 30.5) | 19.8 (17.5, 22.3) | 12.0 (10.1, 14.1) | 32.3 (29.6, 35.2) | 8.2 (6.7, 10) |
| Age groups (years) | ||||||
| 15–24 | 1756 | 42.9 (40.9, 45.0) | 17.0 (15.5, 18.7) | 28.5 (26.6, 30.4) | 8.1 (7.1, 9.3) | 3.4 (2.7, 4.3) |
| 25–29 | 2892 | 42.9 (41.1, 44.7) | 16.7 (15.4, 18.2) | 19.6 (18.1, 21.1) | 15.6 (14.3, 17.0) | 5.2 (4.5, 6.1) |
| 30–34 | 2098 | 38.8 (36.6, 41.0) | 16.7 (15.1, 18.4) | 19.7 (18.0, 21.6) | 19.0 (17.3, 20.8) | 5.8 (4.8, 6.9) |
| >34 | 1779 | 32.7 (30.4, 35.1) | 17.8 (15.9, 19.8) | 22.8 (20.8, 25.0) | 19.8 (17.8, 21.8) | 7.0 (5.8, 8.4) |
| Access to Mass media | ||||||
| No | 2518 | 48.4 (46.6, 50.3) | 13.3 (12.0, 14.6) | 27.2 (25.6, 28.9) | 7.6 (6.6, 8.6) | 3.5 (2.9, 4.3) |
| Yes | 6007 | 36.2 (35.0, 37.4) | 18.8 (17.8, 19.8) | 20.2 (19.2, 21.3) | 18.8 (17.8, 19.8) | 6.0 (5.4, 6.6) |
| Parity | ||||||
| 1 | 2166 | 31.6 (29.9, 33.4) | 20.8 (19.3, 22.4) | 28.3 (26.6, 30.1) | 14.5 (13.2, 15.8) | 4.8 (4.1, 5.7) |
| 2 | 3409 | 43.0 (41.3, 44.7) | 15.5 (14.3, 16.7) | 19.1 (17.8, 20.5) | 16.8 (15.6, 18.1) | 5.6 (4.9, 6.5) |
| 3 | 1613 | 45.5 (42.9, 48.2) | 14.2 (12.5, 16.2) | 20.8 (18.7, 23.0) | 13.4 (11.7, 15.3) | 6.0 (4.9, 7.4) |
| 4 | 1242 | 46.2 (43.1, 49.3) | 14.3 (12.2, 16.6) | 19.6 (17.3, 22.2) | 15.6 (13.5, 18.0) | 4.3 (3.2, 5.8) |
| 4+ | 95 | 35.7 (27.9, 44.3) | 28.9 (21.7, 37.3) | 31.6 (24.2, 40.1) | 3.7 (1.5, 8.8) | _ |
| Place of residence | ||||||
| Urban | 2396 | 34.9 (33.2, 36.6) | 18.3 (17.0, 19.8) | 17.0 (15.7, 18.4) | 23.6 (22.1, 25.1) | 6.2 (5.4, 7.1) |
| Rural | 6129 | 42.9 (41.6, 44.2) | 16.3 (15.3, 17.3) | 25.4 (24.3, 26.5) | 10.8 (10.0, 11.6) | 4.7 (4.2, 5.3) |
| Wealth quintiles | ||||||
| Poorest | 1302 | 51.8 (49.2, 54.4) | 13.1 (11.4, 14.9) | 28.6 (26.3, 31.0) | 3.8 (2.9, 5.0) | 2.7 (2.0, 3.7) |
| Poorer | 2033 | 46.6 (44.4, 48.8) | 14.0 (12.5, 15.6) | 29.0 (27.0, 31.0) | 7.2 (6.1, 8.4) | 3.3 (2.6, 4.2) |
| Middle | 1764 | 40.3 (37.9, 42.7) | 17.4 (15.6, 19.4) | 28.6 (26.5, 30.9) | 9.3 (8.0, 10.9) | 4.3 (3.4, 5.4) |
| Richer | 1589 | 35.2 (33.0, 37.5) | 21.7 (19.8, 23.7) | 20.0 (18.2, 21.9) | 17.7 (16, 19.6) | 5.4 (4.4, 6.6) |
| Richest | 1837 | 28.8 (26.8, 30.9) | 18.4 (16.7, 20.3) | 7.9 (6.8, 9.3) | 35.1 (33, 37.3) | 9.7 (8.4, 11.2) |
| Religion | ||||||
| Hindu | 5180 | 39.2 (37.9, 40.4) | 17.4 (16.4, 18.4) | 23.0 (21.9, 24.1) | 15.3 (14.3, 16.2) | 5.2 (4.6, 5.8) |
| Muslims | 1856 | 49.8 (47.6, 52.0) | 16.9 (15.3, 18.6) | 21.0 (19.3, 22.8) | 9.3 (8.1, 10.6) | 3.0 (2.3, 3.9) |
| Other | 1489 | 22.6 (19.8, 25.6) | 14.2 (11.9, 16.8) | 22.4 (19.7, 25.5) | 29.7 (26.7, 33.0) | 11.1 (9.1, 13.4) |
| Caste | ||||||
| General | 3390 | 40.8 (39.3, 42.4) | 17.0 (15.9, 18.2) | 22.9 (21.6, 24.2) | 14.3 (13.2, 15.4) | 5.0 (4.3, 5.7) |
| SC/ST | 2862 | 37.9 (36.0, 39.9) | 18.2 (16.7, 19.8) | 26.2 (24.5, 28.1) | 13.0 (11.7, 14.5) | 4.7 (3.9, 5.6) |
| OBC | 2273 | 41.2 (39.2, 43.2) | 15.7 (14.3, 17.3) | 18.0 (16.5, 19.6) | 18.9 (17.4, 20.6) | 6.2 (5.2, 7.2) |
| The duration between initiation of contraception and interview (year) | ||||||
| 1 | 3462 | 43.4 (41.8, 45.1) | 17.8 (16.5, 19.1) | 20.4 (19.1, 21.8) | 14.3 (13.1, 15.5) | 4.1 (3.5, 4.8) |
| 2 | 2249 | 43.1 (41.1, 45.1) | 15.4 (14.0, 16.9) | 23.2 (21.6, 25.0) | 13.4 (12.0, 14.8) | 4.9 (4.1, 5.9) |
| 3 | 1598 | 36.4 (34.1, 38.7) | 16.2 (14.5, 18.1) | 24.3 (22.3, 26.4) | 16.1 (14.5, 18.0) | 7.0 (5.9, 8.3) |
| 4 | 930 | 33.0 (30.0, 36.2) | 17.0 (14.7, 19.6) | 25.1 (22.4, 28.1) | 18.2 (15.8, 20.9) | 6.6 (5.2, 8.5) |
| 5 | 286 | 17.8 (13.5, 23.2) | 26.6 (21.4, 32.6) | 22.4 (17.6, 28.1) | 27.8 (22.5, 33.8) | 5.3 (3.1, 8.9) |
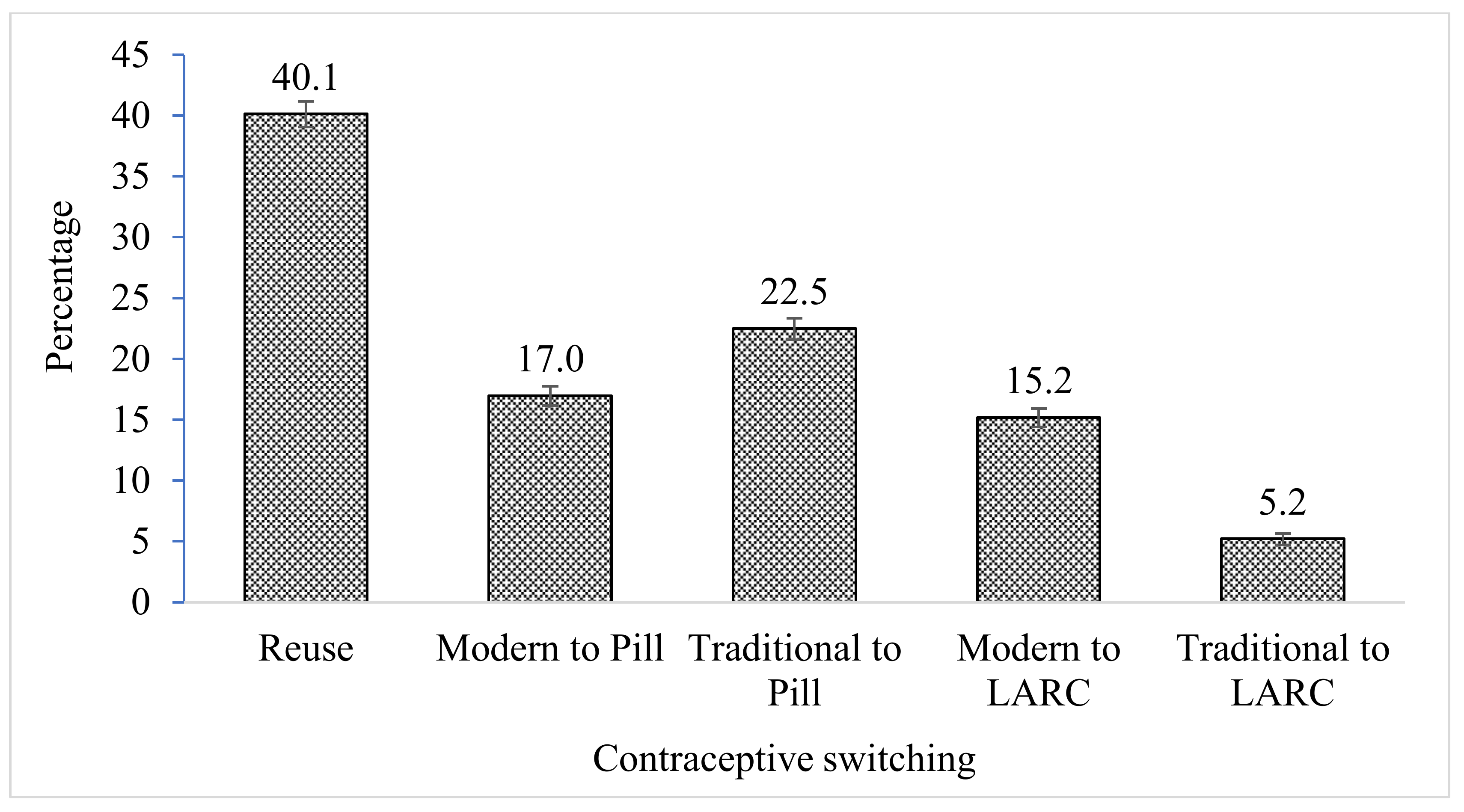
| Total | 8525 | 40.1 (39.1, 41.2) | 17.0 (16.2, 17.8) | 22.5 (21.6, 23.4) | 15.2 (14.4, 16.0) | 5.2 (4.8, 5.7) |
References
- International Institute for Population Sciences (IIPS) and ICF. National Family Health Survey (NFHS-4), 2015–2016; IIPS: Mumbai, India, 2017. [Google Scholar]
- Bruce, J. Fundamental Elements of the Quality of Care: A Simple Framework. Stud. Fam. Plan. 1990, 21, 61–91. [Google Scholar] [CrossRef]
- Jain, A.K. Fertility reduction and the quality of family planning services. Stud. Fam. Plan. 1989, 20, 1–16. [Google Scholar] [CrossRef]
- Ali, M.M. Quality of care and contraceptive pill discontinuation in rural Egypt. J. Biosoc. Sci. 2001, 33, 161–172. [Google Scholar] [CrossRef] [PubMed]
- Tumlinson, K.; Pence, B.W.; Curtis, S.L.; Marshall, S.W.; Speizer, I.S. Quality of Care and Contraceptive Use in Urban Kenya. Int. Perspect. Sex. Reprod. Health 2015, 41, 69–79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Magnani, R.J.; Hotchkiss, D.R.; Florence, C.S.; Shafer, L.A. The impact of the family planning supply environment on contraceptive intentions and use in Morocco. Stud. Fam. Plan. 1999, 30, 120–132. [Google Scholar] [CrossRef] [PubMed]
- Mensch, B.; Arends-Kuenning, M.; Jain, A. The impact of the quality of family planning services on contraceptive use in Peru. Stud. Fam. Plan. 1996, 27, 59–75. [Google Scholar] [CrossRef]
- Arends-Kuenning, M.; Kessy, F.L. The impact of demand factors, quality of care and access to facilities on contraceptive use in Tanzania. J. Biosoc. Sci. 2007, 39, 1–26. [Google Scholar] [CrossRef] [PubMed]
- Gubhaju, B. Barriers to sustained use of contraception in Nepal: Quality of care, socioeconomic status, and method-related factors. Biodemography Soc. Biol. 2009, 55, 52–70. [Google Scholar] [CrossRef] [PubMed]
- RamaRao, S.; Lacuesta, M.; Costello, M.; Pangolibay, B.; Jones, H. The Link between Quality of Care and Contraceptive Use. Int. Perspect. Sex. Reprod. Health 2003, 29, 76. [Google Scholar] [CrossRef]
- Koenig, M.A.; Hossain, M.B.; Whittaker, M. The influence of quality of care upon contraceptive use in rural Bangladesh. Stud. Fam. Plan. 1997, 28, 278–289. [Google Scholar] [CrossRef]
- Hong, R.; Montana, L.; Mishra, V. Family planning services quality as a determinant of use of IUD in Egypt. BMC Health Serv. Res. 2006, 6, 79–87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santhya, K.G. Changing Family Planning Scenario in India: An Overview of Recent Evidence; Population Council: New Delhi, India, 2003. [Google Scholar]
- Agrahari, K.; Mohanty, S.K.; Chauhan, R.K. Socio-Economic Differentials in Contraceptive Discontinuation in India. SAGE Open 2016, 6, 2158244016646612. [Google Scholar] [CrossRef] [Green Version]
- Rai, R.K.; Unisa, S. Dynamics of contraceptive use in India: Apprehension versus future intention among non-users and traditional method users. Sex. Reprod. Healthc. 2013, 4, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Jain, A.K. Information about methods received by contraceptive users in India. J. Biosoc. Sci. 2017, 49, 798–810. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- International Institute for Population Studies (IIPS) & Macro International. National Family Health Survey (NFHS-3), 2005–2006; IIPS: Mumbai, India, 2007; Volume I. [Google Scholar]
- Festin, M.P.R.; Kiarie, J.; Solo, J.; Spieler, J.; Malarcher, S.; Van Look, P.F.; Temmerman, M. Moving towards the goals of FP2020 —Classifying contraceptives. Contraception 2016, 94, 289–294. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hubacher, D.; Trussell, J. A definition of modern contraceptive methods. Contraception 2015, 92, 420–421. [Google Scholar] [CrossRef] [PubMed]
- Curtis, S.L.; Blanc, A.K. Determinants of Contraceptive Failure, Switching, and Discontinuation: An Analysis of DHS Contraceptive Histories (No. 6); Macro International: Calverton, MD, USA, 1997. [Google Scholar]
- Retherford, R.D.; Choe, M.K. Statistical Models for Causal Analysis; John Wiley & Sons: Hoboken, NJ, USA, 2011. [Google Scholar]
- Government of India. India’s Vision FP 2020; Ministry of Health and Family Welfare (MOHFW): New Delhi, India, 2014; Available online: https://advancefamilyplanning.org/sites/default/files/resources/FP2020-Vision-Document%20India.pdf (accessed on 17 August 2018).
- Government of India; Ministry of Health and Family Welfare. Mission Parivar Vikas. 2016. Available online: http://www.nhmmp.gov.in/WebContent/FW/Scheme/Scheme2017/Mission_Parivar_Vikas.pdf (accessed on 18 August 2018).
- Government of India. Update on ASHA Programme. 2017. Available online: http://nhsrcindia.org/sites/default/files/Update%20on%20ASHA%20Programme-%20January-2017.pdf (accessed on 10 October 2018).
- Staveteig, S.; Shrestha, N.; Gurung, S.; Kampa, K.T. Barriers to Family Planning Use in Eastern Nepal: Results from a Mixed Methods Study; DHS Qualitative Research Studies No. 21; ICF: Rockville, MD, USA, 2018. [Google Scholar]
| Discontinued Methods | Reuse | Other Modern Methods to Pill | Traditional Methods to Pill | Other Modern Methods to LARC | Traditional Methods to LARC |
|---|---|---|---|---|---|
| Pill | 83.4 (82.1, 84.6) | ─ | ─ | 33.4 (30.8, 36.0) | ─ |
| IUD | 14.6 (13.4, 15.8) | 14.0 (12.3, 15.9) | ─ | ─ | ─ |
| Injectables | 2.0 (1.6, 2.6) | 3.8 (2.9, 4.9) | ─ | ─ | ─ |
| Diaphragm | ─ | 0.08 (0.01, 0.50) | ─ | ─ | ─ |
| Condom | ─ | 81.5 (79.4, 83.4) | ─ | 64.1 (61.5, 66.7) | ─ |
| Rhythm/Periodic | ─ | ─ | 43.3 (41.1, 45.5) | ─ | 55.6 (50.9, 60.2) |
| Withdrawal | ─ | ─ | 46.7 (44.5, 49) | ─ | 40.1 (35.6, 44.7) |
| Other traditional methods | ─ | ─ | 0.2 (0.1, 0.5) | ─ | ─ |
| Lactational Amenorrhea | ─ | ─ | 9.8 (8.5, 11.2) | ─ | 4.3 (2.8, 6.7) |
| Female condom | ─ | 0.15 (0.04, 0.61) | ─ | 1.6 (1.0, 2.4) | ─ |
| Other modern methods | ─ | 0.40 (0.18, 0.91) | ─ | 0.9 (0.5, 1.7) | ─ |
| Number of observations | 3422 | 1318 | 1695 | 1478 | 612 |
| Combinations of Method Information | Reuse vs. Modern Method to Pill | Reuse vs. Traditional Method to Pill | Reuse vs. Modern Method to LARC | Reuse vs. Traditional Method to LARC |
|---|---|---|---|---|
| SE-No * MSE-No * OM-No (Ref.) | 1.00 | 1.00 | 1.00 | 1.00 |
| SE-No * MSE-No * OM-Yes | 1.41 (1.14, 1.75) ** | 1.45 (1.20, 1.76) *** | 1.38 (1.07, 1.76) * | 1.35 (0.88, 2.07) |
| SE-No * MSE-Yes * OM-No | 1.24 (0.54, 2.88) | 0.89 (0.39, 2.02) | 1.34 (0.53, 3.42) | 6.80 (2.83, 16.4) *** |
| SE-No * MSE-Yes * OM-Yes | 2.21 (1.47, 3.32) *** | 1.10 (0.70, 1.71) | 2.37 (1.50, 3.74)*** | 2.27 (1.07, 4.82) * |
| SE-Yes * MSE-No * OM-No | 0.59 (0.38, 0.93) * | 0.52 (0.35, 0.79) ** | 0.57 (0.34, 0.97) * | 1.35 (0.69, 2.64) |
| SE-Yes * MSE-No * OM-Yes | 1.14 (0.82, 1.59) | 0.87 (0.63, 1.21) | 1.35 (0.95, 1.93) | 1.42 (0.78, 2.58) |
| SE-Yes * MSE-Yes * OM-No | 0.89 (0.60, 1.32) | 0.83 (0.59, 1.19) | 1.51 (1.04, 2.19) * | 2.74 (1.65, 4.57) *** |
| SE-Yes * MSE-Yes * OM-Yes | 1.45 (1.24, 1.69) *** | 1.41 (1.22, 1.62) *** | 1.58 (1.32, 1.88) *** | 2.45 (1.84, 3.27) *** |
| Variables | Reuse vs. Modern Method to Pill | Reuse vs. Traditional Method to Pill | Reuse vs. Modern Method to LARC | Reuse vs. Traditional Method to LARC |
|---|---|---|---|---|
| Women’s education | ||||
| No education (Ref.) | 1.00 | 1.00 | 1.00 | 1.00 |
| Primary | 0.78 (0.61, 0.99) * | 0.94 (0.77, 1.14) | 0.72 (0.54, 0.95) * | 0.53 (0.36, 0.77) ** |
| Secondary | 1.01 (0.82, 1.25) | 1.01 (0.85, 1.21) | 0.83 (0.65, 1.06) | 0.50 (0.36, 0.70) *** |
| Higher | 1.12 (0.84, 1.51) | 0.95 (0.71, 1.28) | 1.33 (0.98, 1.81) | 0.75 (0.49, 1.15) |
| Age groups | ||||
| 15–24 (Ref.) | 1.00 | 1.00 | 1.00 | 1.00 |
| 25–29 | 1.11 (0.93, 1.33) | 0.95 (0.81, 1.11) | 1.28 (1.03, 1.59) * | 1.11 (0.81, 1.52) |
| 30–34 | 1.24 (1.01, 1.52) * | 1.18 (0.98, 1.43) | 1.35 (1.07, 1.72) * | 1.17 (0.83, 1.65) |
| >34 | 1.59 (1.27, 2.01) *** | 1.81 (1.47, 2.23) *** | 1.44 (1.11, 1.88) ** | 1.48 (1.02, 2.14) * |
| Access to Mass media | ||||
| No (Ref.) | 1.00 | 1.00 | 1.00 | 1.00 |
| Yes | 1.40 (1.20, 1.64) *** | 1.01 (0.89, 1.15) | 1.46 (1.21, 1.76) *** | 1.30 (0.99, 1.7) |
| Parity | ||||
| 1 (Ref.) | 1.00 | 1.00 | 1.00 | 1.00 |
| 2 | 0.52 (0.44, 0.61) *** | 0.43 (0.37, 0.50) *** | 0.94 (0.78, 1.12) | 0.91 (0.70, 1.19) |
| 3 | 0.49 (0.40, 0.62) *** | 0.43 (0.35, 0.53) *** | 0.95 (0.75, 1.22) | 1.04 (0.74, 1.48) |
| 4+ | 0.52 (0.40, 0.68) *** | 0.35 (0.27, 0.45) *** | 1.76 (1.31, 2.36) *** | 0.93 (0.59, 1.47) |
| Not reported | 1.42 (0.90, 2.24) | 1.17 (0.75, 1.83) | 0.33 (0.13, 0.87) * | - |
| Place of residence | ||||
| Urban (Ref.) | 1.00 | 1.00 | 1.00 | 1.00 |
| Rural | 1.09 (0.93, 1.27) | 0.95 (0.82, 1.11) | 0.83 (0.71, 0.98) * | 1.14 [0.89, 1.45) |
| Wealth quintiles | ||||
| Poorest (Ref.) | 1.00 | 1.00 | 1.00 | 1.00 |
| Poorer | 1.12 (0.90, 1.40) | 1.07 (0.91, 1.28) | 2.12 (1.51, 2.98) *** | 1.45 (0.95, 2.22) |
| Middle | 1.52 (1.20, 1.92) ** | 1.16 (0.96, 1.41) | 2.88 (2.03, 4.10) *** | 2.21 (1.43, 3.44) *** |
| Richer | 2.01 (1.56, 2.58) *** | 0.84 (0.67, 1.05) | 5.86 (4.12, 8.34) *** | 3.32 (2.10, 5.25) *** |
| Richest | 1.80 (1.36, 2.40) *** | 0.33 (0.24, 0.43) *** | 10.37 (7.2, 15.0) *** | 5.56 (3.44, 8.98) *** |
| Religion | ||||
| Hindu (Ref.) | 1.00 | 1.00 | 1.00 | 1.00 |
| Muslims | 1.17 (0.99, 1.39) | 0.76 (0.65, 0.89) ** | 0.76 (0.62, 0.94) ** | 0.69 (0.50, 0.95) * |
| Other | 1.38 (1.06, 1.78) * | 1.79 (1.42, 2.25) *** | 3.14 (2.49, 3.96) *** | 2.92 (2.15, 3.96) *** |
| Caste | ||||
| General (Ref.) | 1.00 | 1.00 | 1.00 | 1.00 |
| SC/ST | 1.43 (1.20, 1.70) *** | 1.05 (0.90, 1.23) | 1.46 (1.21, 1.78) *** | 1.19 (0.9, 1.57) |
| OBC | 0.89 (0.76, 1.05) | 0.74 (0.64, 0.87) *** | 1.31 (1.11, 1.55) ** | 1.15 (0.9, 1.48) |
| The duration between initiation of contraception and interview (year) | ||||
| 1 (Ref.) | 1.00 | 1.00 | 1.00 | 1.00 |
| 2 | 0.87 (0.74, 1.02) | 1.10 (0.95, 1.26) | 0.93 (0.78, 1.11) | 1.18 (0.90, 1.54) |
| 3 | 1.06 (0.89, 1.27) | 1.42 (1.21, 1.67) *** | 1.24 (1.03, 1.51) * | 1.85 (1.41, 2.44) *** |
| 4 | 1.27 (1.01, 1.60) * | 1.71 (1.39, 2.10) *** | 1.35 (1.06, 1.71) * | 1.67 (1.18, 2.36) ** |
| 5 | 3.48 (2.31, 5.25) *** | 2.67 (1.75, 4.08) *** | 3.34 (2.17, 5.15) *** | 2.23 (1.14, 4.36) * |
| Constant | 0.20 (0.14, 0.29) *** | 0.80 (0.59, 1.07) | 0.03 (0.02, 0.05) *** | 0.02 (0.01, 0.04) *** |
| Number of observation | 8525 | |||
| Log-likelihood ratio | −11135.1 | |||
| LR chi2(124) | 2276.7 | |||
| P-value | <0.001 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rana, M.J.; Goli, S.; Mishra, R.; Gautam, A.; Datta, N.; Nanda, P.; Verma, R. Contraceptive Method Information and Method Switching in India. Sustainability 2021, 13, 9831. https://doi.org/10.3390/su13179831
Rana MJ, Goli S, Mishra R, Gautam A, Datta N, Nanda P, Verma R. Contraceptive Method Information and Method Switching in India. Sustainability. 2021; 13(17):9831. https://doi.org/10.3390/su13179831
Chicago/Turabian StyleRana, Md. Juel, Srinivas Goli, Rakesh Mishra, Abhishek Gautam, Nitin Datta, Priya Nanda, and Ravi Verma. 2021. "Contraceptive Method Information and Method Switching in India" Sustainability 13, no. 17: 9831. https://doi.org/10.3390/su13179831
APA StyleRana, M. J., Goli, S., Mishra, R., Gautam, A., Datta, N., Nanda, P., & Verma, R. (2021). Contraceptive Method Information and Method Switching in India. Sustainability, 13(17), 9831. https://doi.org/10.3390/su13179831








