Abstract
Families with children who have attention deficit hyperactivity disorder (ADHD) tend to display unpleasant psychological reactions arising from the pressure exerted by the social and school context, and from experiences linked to difficulties their children have. The present research seeks to examine the effectiveness of a mindfulness program on various dimensions related to well-being and psychological flexibility in parents of children with ADHD. The program is based on protocols of Mindfulness-Based Stress Reduction (MBSR) and Mindfulness-Based Cognitive Therapy (MBCT), enhanced through the specific inclusion of relational keys, self-compassion exercises and framed within self-care. Participants were 22 fathers and mothers of children and teenagers diagnosed with ADHD. Psychological flexibility (AAQ II), cognitive fusion (CFQ), mindfulness (FFMQ), coping (COPE), and self-compassion (SCS) measures were used. Results showed a significant increase in mindfulness skills, psychological flexibility, self-compassion, and in the use of humor (COPE) as a strategy for coping with personal problematic events. We discuss the results which emerged, the limitations of the study, as well as proposals for improvement.
1. Introduction
Stress is a process through which the body triggers a series of internal resources to cope with a real or imaginary threat. A whole series of physiological changes occur that prepare the body to either fight or flee from the stressful situation [1]. Should they persist over time, these combat or fleeing processes may lead to serious health problems, such as chronic pain [2] or illnesses of the immune system [3] which may be linked to cancer [4].
It is now known that parents of children diagnosed with ADHD are forced to respond to a series of excessive demands, overlapping of tasks, having to cope with internal and external crises, conflictive relations with their children or with other people, as well as living with uncertainty and under pressure imposed by both others and themselves [5]. All of this can lead to stress responses in people. In situations like these, the mind becomes disturbed and does not allow us to see clearly what is happening, which can often get in the way of achieving key goals, and which can affect the development of children’s social responsibility [6].
Attention deficit hyperactivity disorder (ADHD) is diagnosed in 5–7% of children and teenagers around the world, and in 4.4% of the adult population [7,8]. It should be remembered that it is a diagnosis which displays significant comorbidity and overlaps with learning difficulties [9], hence, its high degree of diagnostic prevalence.
In today’s social and school context, characterized by its competitiveness and focus on results (occasionally leading to excessive amounts of homework, frequent distraction, under-performance, failure at school, etc.), it is not uncommon for parents of children with ADHD to display unpleasant thoughts and feelings resulting from such difficulties. How adults respond to these situations will also influence how younger people cope. How parents interact or relate to such personal events will thus make a major difference vis-à-vis either helping to improve relations with their children, overcoming long-term difficulties and increasing parental satisfaction and well-being or, on the contrary, worsening the desperation and stress, with the subsequent damage this causes to the relation and to satisfaction in various key areas [10].
One of the most commonly used interventions in these cases is Behavioral Parent Training (BPT). It is an intervention oriented towards control, and is aimed at helping parents to prevent stress patterns when interacting with their children. It places the emphasis on learning and the use of behavioral modification techniques such as social contingencies through reinforcement, extinction, negative punishments and time-outs. Nevertheless, its effectiveness has been found to be limited, added to which its effects are not long-term without the supervision and continued follow-up of a specialized therapist [11]. Today, many professionals point out that learning stress management skills and enhanced personal self-care can prove key to developing healthy relations with children [12,13].
In 2004, Steven Hayes [14] coined the term “third generation therapies” to refer to a group of innovative psychological therapies which adopt a common approach to human suffering and distress. These approaches have heralded a turning point in terms of how to address suffering and distress, shifting from the classical symptom-based focus designed to reduce the latter and so provide relief, to centering attention on the life which is important to the person (the life they value and which gives them life satisfaction). This shift in focus involves fostering contextual procedures that train the person in a new form of relating to thoughts and feelings, rather than highlighting the latter’s actual content. These are methods characterized by their training in skills designed to boost a willingness to experience what is happening at the present moment and focusing attention on the realization of actions that are consistent with what is important for the person.
From this perspective, psychological inflexibility is perceived as a behavior-regulating process that entails avoiding and/or escaping from personal experiences (thoughts, emotions, sensations, and so on) which are felt to be aversive, even when doing so involves behaving in a manner that is incompatible with the person’s goals. In contrast, Hayes (2006) defines psychological flexibility as the ability to consciously take experiences in the present moment and direct actions in the direction of what is important to the person [15].
Brussell et al. (2016) studied the relation between parental psychological flexibility and the development of adaptive parenting practices and showed that the highest levels of specific psychological flexibility for raising children are associated with fewer problems at all age levels and have major implications for children’s well-being [16].
Mindfulness strategies involve directing attention towards what one is thinking and feeling at a given moment, and becoming aware of all of it, pinpointing personal barriers and learning to maintain valued actions in the presence of these personal events [17,18]. Such practices have proven effective at training for a different way of relating to the most unpleasant thoughts and feelings, so that they do not become an obstacle to engaging in more serene and meaningful activities. In order to achieve this, deictic and hierarchical framing has been introduced into mindfulness practices and these have shown a way to relate to personal events that can empower the person to face up to circumstances (see psychological flexibility) [19]. From this perspective, training in mindfulness is framed within the person’s self-care and promotion of well-being and emerges as an antidote to stress.
Mindfulness exercises may basically be divided into two types depending on where attention is focused [20]. If kept within a specific stimulus (one’s own breathing, the soles of one’s feet, a sound, an object, etc.), we are referring to focused attention practices, whereas open monitoring involves directing attention to any thought or feeling that arises at the present moment, as a means of being aware of how personal events flow inside us. Focused attention practices allow for greater improvement in attentional control, while open monitoring practices curb reactions to what we think and feel [21]. Open monitoring-based exercises train people to identify thoughts and to “deliteralize” them; in other words, to understand them for what they are and not as part of reality (cognitive fusion). In this way, the person in question becomes a mere observer of their personal events without attempting to do anything about them.
Transferred to addressing the difficulties linked to raising children with ADHD, mindfulness and self-care might be reflected in an enhanced reactivity to the more unpleasant emotions [22] and, as a result, to an enrichment of relations with children, a greater contribution to developing attentional skills with them, a better treatment of oneself, enhanced satisfaction when parenting and in the development of self-care and personal well-being [23].
This study seeks to improve the coping skills of parents whose children have ADHD by boosting acceptance of difficult thoughts and feelings, learning to treat oneself well when faced with problematic feelings (e.g., blame) and encouraging self-care and well-being as a result of significant action for the person in their role as parents. This has already been carried out in school [24,25] and family [23] contexts in order to deal with stress, and has yielded satisfactory results. As a result, in the present work, a protocol of mindfulness practices has been developed which has been improved with elements taken from new definitions of psychological flexibility [19], introducing these skills as a form of self-care.
The aim of this study is to determine the effectiveness of a 12-session group intervention of mindfulness and self-care on skills that provide a healthy basis for coping with problematic situations in parents of children with a diagnosis of ADHD. The initial hypothesis is that the intervention protocol will improve mindfulness capacity, acceptance of unpleasant private events, and enhance personal self-care.
2. Materials and Methods
2.1. Participants
Participants were 22 fathers/mothers who belonged to a local association of parents of children with ADHD. An introductory informative talk was given, organized by the association. In addition to framing the mindfulness practices within self-care and presenting this as a remedy for stress, the protocol was offered to members of the association as well as to any other person who might be interested, with specific information about the research also being provided.
The final study sample was composed of 19 women and 3 men, who signed an informed consent agreement which set out the motives, scope, as well as the confidential and anonymous processing of data, thereby complying with the ethical precepts established in the Declaration of Helsinki. All of the participants stayed until the end of the protocol (12 weekly sessions).
2.2. Measures
2.2.1. Psychological Flexibility (AAQ-II)
In order to measure psychological flexibility, the second version of the Acceptance and Action Questionnaire (AAQ-II) [26] was used in its Spanish adaptation [27]. In this questionnaire, responses are scored on a 7-option Likert-type scale, with responses ranging from 1 (never true) to 7 (always true). Total scores ranged from 10 to 70, with higher scores indicating a higher degree of experiential avoidance and, therefore, lower levels of psychological flexibility. The mean of the normative sample was 18.51 points (SD = 7.05) [27]. Previous studies indicate there was satisfactory internal consistency, with a mean alpha coefficient of 0.84, with the reliability of the tests-retests at 3 and 12 months being 0.81 and 0.79, respectively. As to validity data, the AAQ-II scores correlated significantly with all the psychological symptoms evaluated by the SCL-90-R (between r = 0.55 and r = 0.58), with depression scores (r = 0.45), degree of worries (r = 0.56), anxiety sensitivity index (r = 0.43), general self-efficacy (r = −0.40), mental health index (r = −0.58) and physical health index (r = −0.44) [27].
2.2.2. COPE 28 (Brief COPE)
COPE 28 was the Spanish adaptation of the brief version of COPE [28,29]. There are 14 scales with 2 items each, which are answered through a Likert-type scale of 0 to 4 points, with frequency use of the strategy being 0 (never) to 4 (almost always). This questionnaire typically measures both dysfunctional and adaptive coping responses. The 14 scales are: active coping, planning, emotional support, social support, religion, reframing, acceptance, humor, denial, self-distraction, self-blame, disengagement, venting, and substance use. The reliability of the questionnaires measured by Cronbach’s alpha exceeded 0.60 [28].
2.2.3. Five Facets of the Mindfulness Questionnaire (FFMQ)
The Spanish adaptation of the original questionnaire was used [30,31]. This questionnaire is comprised of 39 items that evaluate five facets of mindfulness. Each of the items is evaluated on a Likert scale ranging from 1 (never or rarely true) to 5 (very often or always true). The factors are: observation, including noting and attending to internal and external experiences such as thoughts, feelings, and sensations; describing or labeling these internal experiences; acting with awareness, which refers to focusing on one’s activities in the moment as opposed to behaving mechanically; acting without judgment, which refers to perceiving the internal experience in a non-judgmental manner, and finally, not reacting to internal experience, allowing this to flow without getting caught up in its content. Cronbach indices in the questionnaire ranged between 0.80 and 0.91, and 0.88 for the FFMQ total score. Talking about convergent and divergent validity, all of the scales correlated negatively with all of the psychopathological factors (depression, anxiety, paranoia, obsession, somatization, hostility and psychological inflexibility), except observing. The scale that shows higher correlations with psychopathology measures is the non-judging of inner experience factor [31].
2.3.4. Self-Compassion Scale (SCS)
This is the Spanish translation of the original SCS [32], which evaluates six different aspects of self-compassion: self-compassion, self-criticism, normalization, isolation, mindfulness, and over-identification. Each of the items is scored on a 5-point Likert scale, ranging from 1 (almost never) to 5 (almost always). The internal consistency was an alpha coefficient of 0.92 in the development sample and the reliability test-retest for the total scale was 0.92. Validity analyses showed positive associations with measures of social connectedness, life satisfaction, self-esteem, and emotional processing and negative associations with measures of psychological distress, self-criticism, and rumination.
2.3.5. Cognitive Fusion Questionnaire (CFQ)
The Cognitive Fusion Questionnaire (CFQ) [33] is a scale made up of seven items evaluating the level of cognitive fusion on a 7-point Likert-type scale, ranging from 7 (always) to 1 (never). Higher scores indicate a higher level of cognitive fusion. The version in Spanish [34], which is the one used, displays a Cronbach alpha of 0.87. The mean of the normative sample was 21.70 points (SD = 8.68). CFQ correlate significantly and positively with rumination (r = 0.63), experiential avoidance (r = 0.67), depression (r = 0.43), anxiety (r = 0.53), and negatively with satisfaction with life (r = −0.38).
2.3. Design
This was a longitudinal study with pre-test and post-test measures with no controlled or randomized comparison group by using a purposeful sample and convenience method.
2.4. Procedure
The protocol which was applied is an adaptation of the works of Kabat-Zinn [35,36,37] and the proposal on Mindfulness-Based Cognitive Therapy (MBCT) for depression [38] already used previously by the former author [17], to which have been added: (a) relational keys (hierarchical relation with the deictic “I” and behavioral regulation function) which have been isolated experimentally and have evidenced their effectiveness at improving mindfulness interventions [39], (b) elements of self-care, and (c) specific practice in caring for oneself when faced with complex situations.
This protocol is made up of 12 sessions of 1.5 hours each. All the sessions had the following structure: (a) short initial practice, (b) review of the weekly practice, (c) introduction to the session, (d) central practice, (e) self-care, (f) conclusion with another short practice, (g) summary, (h) proposal of activities for the week (summary of content, see Table 1). The protocol was implemented by the first author with the help of a co-therapist and lasted a total of 12 weeks.

Table 1.
Summary of protocol content.
Participants joined the program voluntarily following an informative session organized by a local non-government body of relatives of people diagnosed with ADHD. The session set out the basic fundamentals of mindfulness training and how the program would be developed.
Pre-test evaluation was conducted during the first session, and the final tests (post-tests) were given out when the protocol had concluded (session 12).
2.5. Statistical Analysis
Wilcoxon-related samples of non-parametric tests were used to identify intragroup differences, and the size of the r effect was calculated according to Rosenthal (1994).
Statistical analyses were carried out using the SPSS 25 statistical package, assuming a confidence level of 95%.
3. Results
With the exception of the humor scale, in which we found significantly higher scores in the post-test (M = 2.81, SD = 1.44) compared to the pre-test (M = 1.95, SD = 1.29), Z = −2.431, p = 0.015, with a moderate size effect r = 0.51, and no significant differences were found compared to the post-test in the rest of the COPE 28 scale (Table 2 and Figure 1).

Table 2.
Means (standard deviations), Z-value and level of significance, and effect size in COPE factors in pre-test and post-test.
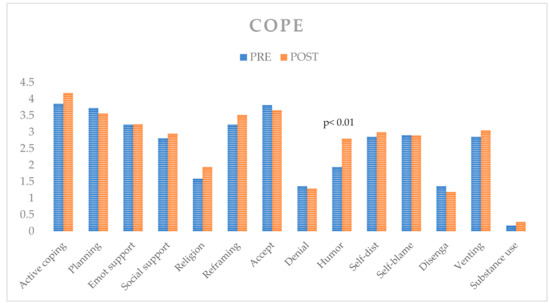
Figure 1.
Coping results (COPE).
With the exception of the normalization scale, in the Self-Compassion Scale (SCS), the rest (self-compassion, self-criticism, isolation, mindfulness, and over-identification) recorded significant differences. Particularly noteworthy are the values in self-compassion, self-criticism, mindfulness, over-identification and the total, with values between Z = −2.654 in the case of mindfulness, and Z = −3.817 in the case of self-compassion and large effect sizes, ranging between r = 0.56 in the case of mindfulness and r = 0.81 in the case of the self-compassion scale (Table 3 and Figure 2).

Table 3.
Means (standard deviations), Z-value and level of significance, and effect size in SCS (Self-Compassion Scale) factors in pre-test and post-test.
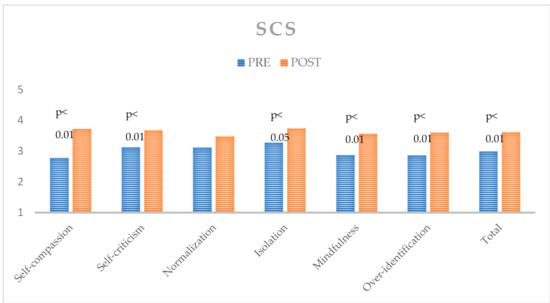
Figure 2.
Self-compassion results (SCS).
As regards to the measure of mindfulness (FFMQ), we observed significant differences in the scales of observation, acting with awareness and acceptance without reaction, and in total, with large size effects, ranging between r = 0.60 in the case of the acting with awareness scale, and r = 0.75 in the observation scale (Table 4 and Figure 3).

Table 4.
Means (standard deviations), Z-value and level of significance, and effect size in FFMQ (Five Facets of the Mindfulness Questionnaire) factors in pre-test and post-test.
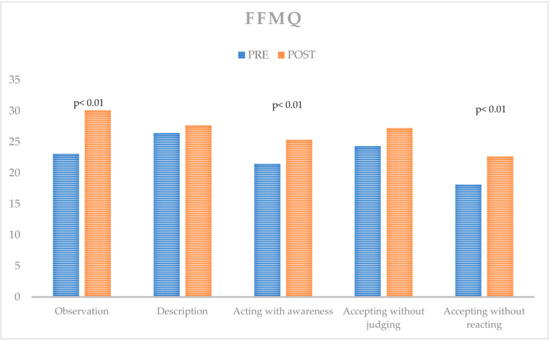
Figure 3.
Mindfulness results (FFMQ).
As regards to psychological flexibility or level of avoidance (AAQ-II), we found significantly lower scores in the post-test (M = 22.52, SD = 6.58) compared to the pre-test (M = 32.91, SD = 8.14), Z = −3.925, p < 0.001, with a high size effect r = 0.84. With regard to the level of cognitive fusion (CFQ), significant differences were also found in the post-test (M = 25.19, SD = 6.68) compared to the pre-test (M = 34.18, SD = 7.00), Z = −3.861, p < 0.001, and an effect size r = 0.84 (Table 5 and Figure 4).

Table 5.
Means (standard deviations), Z-value and level of significance, and effect size in the AAQ (Acceptance and Action Questionnaire) and CFQ (Cognitive Fusion Questionnaire) in pre-test and post-test.
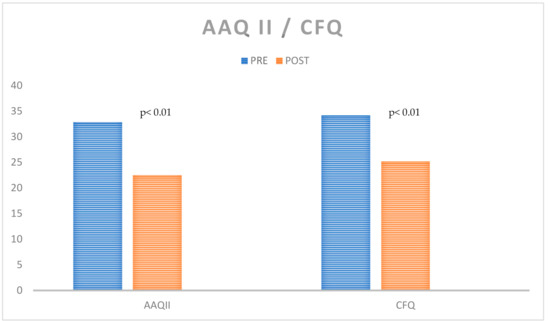
Figure 4.
Acceptance and defusion results (AAQ II and CFQ).
4. Discussion
The results obtained are encouraging with regard to the effectiveness of a training protocol in mindfulness framed within self-care, and which also includes elements from the latest definitions of psychological flexibility.
This optimism stems firstly from a significant improvement in participants’ skills when focusing attention on personal events and acting consciously without reacting impulsively when facing situations. Optimism may also derive from the usefulness of the training vis-à-vis reducing distress relief behaviors in parents in the face of unpleasant personal events, and which opens up a wider range of possibilities for effective action in situations involving emotional impact. This enables people to develop their well-being through a commitment to actions that entail greater life meaningfulness when faced with unpleasant personal events associated with parenting children who have ADHD.
On the other hand, although the results obtained from the COPE indicate that applying the protocol did not prove very useful in terms of making participants change their coping strategies in situations of stress, the importance of the only scale which proved to be an exception should be pointed out: humor, which displayed significantly higher scores after mindfulness intervention. These results reinforce the idea of a change in the way people relate to the more unpleasant thoughts and feelings. Hayes, Strosahl and Wilson [40] have stated that humor is a powerful tool for learning to relate more effectively to negative thoughts as well as being a possible result of distancing and/or cognitive defusion techniques.
Finally, the results also seem to point to a shift in the level of self-compassion. The study appears to suggest that, after training, participants are more friendly towards themselves, judge themselves less often and approach their difficulties as something shared with other people and not as something that should be eliminated or avoided. This way of dealing with personal vulnerability and more unpleasant thoughts and feelings helps to reduce stress, which is defined as a struggle, not wanting to experience what is being experienced at a given moment, thereby leading to personal well-being. As an alternative, the person accepts vulnerability, curbs self-criticism, leaves room for acceptance of what is being experienced and gets in touch with what is important at that moment, engaging in actions that are aligned with life satisfaction in their role as parents.
Despite the optimism to emerge from the results, it is important to point out the limitations of the research carried out and which entail the need to approach the results with caution. Firstly, the study involved no control group, such that it is not clear whether the outcomes are due solely to the intervention or also to the influence of engaging in a social activity once a week.
Secondly, the general intervention explicitly introduces various elements with the aim of improving classical mindfulness protocols (control as a problem, relational keys, self-care, self-compassion), such that it is impossible to say what the differential impact of each of these elements might be on the final results. In this regard, further inquiry into more controlled environments is required and in which the different elements can be isolated in order to conclude with greater certainty how effective each is.
Finally, even though the results are encouraging, the research does display certain limitations. One major initial limitation is that the sample size is small. In addition, the lack of any control group forces us to be cautious with regard to the conclusions. Although it would not seem that the skills taken into account might change over a short period of three months, including a control group in subsequent studies would enable more accurate conclusions to be drawn concerning the implementation of the intervention. Extending the target to other parents who must also face situations of stress and unpleasant emotions might allow for a larger sample size, which would permit a control group to be included and even several experimental groups to be introduced which could gradually embrace innovative aspects of the intervention and thereby gain a more precise understanding of the contribution made by each. It seems that intervention improves coping strategies when participants face stress, although, for the time being, this does not allow any conclusions to be drawn with regard to how this might be reflected in the difficulties faced by their children. Follow-up studies exploring the impact of training in mindfulness are needed, not only with participants but also in their family context.
5. Conclusions
It can be concluded that introducing innovative aspects in parental behavioral training (BPT) allows us to move forward in implementing effective procedures for developing more meaningful parenting. The group mindfulness protocol allows for a relation with personal events, which enables the person to avoid being controlled by intense emotions linked to the situation, but rather to exert control over actions at complicated moments concerning what is important; in this case, the type of qualities as a father and/or mother that one values and wishes to enhance.
In addition, it is important to highlight how training procedures in mindfulness may be enriched by embracing the latest definitions of psychological flexibility [39] that underpin the importance of framing personal events as something the person is aware of and can perceive inside themselves, and which are also different to themselves and can therefore come to form part of their awareness. From this position as observer, the person is able to choose the action to be carried out and which is aligned with what is important in the person’s role as father and/or mother. In conclusion, all of the person’s real empowerment process when facing circumstances has enormous potential in developing the life satisfaction and well-being of parents of children with ADHD.
Author Contributions
All authors made a substantial contribution to the theoretical framework, design, data collection, and interpretation of this study. All authors have read and agree to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Schneiderman, N.; Ironson, G.; Siegel, S. Stress and health: Psychological, behavioral and biological determinants. Annu. Rev. Clin. Psychol. 2005, 1, 607–628. [Google Scholar] [CrossRef]
- Black, D.S.; Slavich, G.M. Mindfulness meditation and the immune system: A systematic review of randomized controlled trials. Ann. New York Acad. Sci. 2016, 1373, 13–24. [Google Scholar] [CrossRef]
- Segerstrom, S.C.; Miller, G.E. Psychological stress and the human immune system: A meta-analytic study of 30 years of inquiry. Psychol. Bull. 2004, 130, 601–630. [Google Scholar] [CrossRef]
- Mitchell, A.J.; Chan, M.; Bhatti, H.; Halton, M.; Grassi, L.; Johansen, C.; Meader, N. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: A metaanalysis of 94 interview-based studies. Lancet Oncol. 2011, 12, 160–174. [Google Scholar] [CrossRef]
- Fernández, M.L.Á. Redes de apoyo social y padres de niños con trastornos del desarrollo. Diferencias estructurales y funcionales basadas en la tipología. Rev. Psicol. Educ. 2016, 11, 7–24. [Google Scholar]
- Martín-Antón, L.J.; Carbonero, M.A.; Valdivieso, J.A.; Monsalvo, E. Influence of some personal and family variables on social responsibility among primary education students. Front. Psychol. 2016, 11, 1124. [Google Scholar] [CrossRef]
- Díaz, A.; Jiménez, J.E.; Rodríguez, C.; Afonso, M.; Artiles, C. Consideraciones de los estudios de prevalencia del trastorno por déficit de atención con o sin hiperactividad (TDAH). Rev. Psicol. Educ. 2013, 8, 155–170. [Google Scholar]
- Cairncross, M.; Miller, C.J. The effectiveness of mindfulness-based therapies for ADHD: A meta-analytic review. J. Atten. Disord. 2020, 24, 627–643. [Google Scholar] [CrossRef]
- Rodríguez-Pérez, C.; García-Sánchez, J.N.; González-Castro, P.; Álvarez-García, D.; González-Pienda, J.A.; Bernardo, A.; Álvarez-Pérez, L. TDAH y el solapamiento con las Dificultades de Aprendizaje en escritura. Rev. Psicol. Educ. 2011, 6, 37–56. [Google Scholar]
- Segal, R.; Hinojosa, J. The activity setting of homework: An analysis of three cases and implications for occupational therapy. Am. J. Occup. 2006, 60, 50–59. [Google Scholar] [CrossRef][Green Version]
- Lee, P.C.; Niew, W.I.; Yang, H.J.; Chen, V.C.; Lin, K.C. A meta-analysis of behavioral parent training for children with attention deficit hyperactivity disorder. Res. Dev. Disabil. 2012, 33, 2040–2049. [Google Scholar] [CrossRef] [PubMed]
- Rodrigo, M.J.; Máiquez, M.L.; García, M.; Mendoza, R.; Rubio, A.; Martínez, A.; Martín, J.C. Relaciones padres-hijos y estilos de vida en la adolescencia. Psicothema 2004, 16, 203–210. [Google Scholar]
- Betta Olivares, R.; Morales Messerer, G.; Rodríguez Ureta, K.; Guerra Vio, C. La frecuencia de emisión de conductas de autocuidado y su relación con los niveles de estrés traumático secundario y de depresión en psicólogos clínicos. Pensam. Psicológico 2007, 3. [Google Scholar] [CrossRef]
- Hayes, S.C. Acceptance and commitment therapy, relational frame theory, and the third wave of behavioral and cognitive therapies. Behav. Ther. 2004, 35, 639–665. [Google Scholar] [CrossRef]
- Hayes, S.C.; Luoma, J.B.; Bond, F.W.; Masuda, A.; Lillis, J. Acceptance and commitment therapy: Model, processes and outcomes. Behav. Res. Ther. 2006, 44, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Brassell, A.; Rosenberg, E.; Parent, J.; Rough, J.N.; Fondacaro, K.; Seehuus, M. Parent´s psychological flexibility: Associations with parenting and child psychosocial well-being. J. Contextual Behav. Sci. 2016, 5, 111–120. [Google Scholar] [CrossRef]
- Salgado, C.F. Comparación de dos protocolos de intervención basados en la Terapia de Aceptación y Compromiso y Entrenamiento en Mindfulness en personas con Trastorno Mental Crónico. Análisis Modif. Conducta 2016, 42, 75–98. [Google Scholar] [CrossRef][Green Version]
- Greco, L.A.; Hayes, S.C. Acceptance and Mindfulness Treatments for Children and Adolescents: A Practitioner’s Guide; New Harbinger Publications: Oakland, CA, USA, 2008. [Google Scholar]
- Luciano, C. Evolución de ACT. Análisis Modif. Conducta 2016, 41, 1–28. [Google Scholar] [CrossRef]
- Hervás, G.; Cebolla, A.; Soler, J. Intervenciones psicológicas basadas en mindfulness y sus beneficios: Estado actual de la cuestión. Clínica Salud 2016, 27, 115–124. [Google Scholar] [CrossRef]
- Vago, D.R.; Silbersweig, D.A. Self-awareness, self-regulation, and self-transcendence (S-ART): A framework for understanding the neurobiological mechanisms of mindfulness. Front. Hum. Neurosci. 2012, 6, 296. [Google Scholar] [CrossRef]
- Van der Oord, S.; Bögels, S.M.; Peijnenburg, D. The effectiveness of mindfulness training for children with ADHD and mindful parenting for their parents. J. Child Fam. Stud. 2012, 21, 139–147. [Google Scholar] [CrossRef] [PubMed]
- Harnett, P.H.; Dawe, S. The Contribution of Mindfulness-based therapies for children and families and proposed conceptual integration. Child Adolesc. Ment. Health 2012, 17, 195–208. [Google Scholar] [CrossRef] [PubMed]
- Broderick, P.C.; Metz, S. Learning to Breathe: A pilot trial of a mindfulness curriculum for adolescents. Adv. Sch. Ment. Health Promot. 2009, 2, 35–46. [Google Scholar] [CrossRef]
- López-González, L.; Amutio, A.; Oriol, X.; Bisquerra, R. Hábitos relacionados con la relajación y la atención plena (mindfulness) de estudiantes de secundaria: Influencia en el clima de aula y el rendimiento académico. Rev. Psicodidáctica 2016, 21, 121–138. [Google Scholar] [CrossRef]
- Bond, F.W.; Hayes, S.C.; Baer, R.A.; Carpenter, K.M.; Guenole, N.; Orcutt, H.K.; Waltz, T.; Zettle, R.D. Preliminary psychometric properties of the Acceptance and Action Questionnaire—II: A revised measure of psychological flexibility and experiential avoidance. Behav. Ther. 2011, 42, 676–688. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, F.J.; Langer Herrera, A.I.; Luciano, C.; Cangas, A.J.; Beltran, I. Measuring experiential avoidance and psychological inflexibility: The Spanish version of the Acceptance and Action Questionnaire—II. Psicothema 2013, 25, 123–129. [Google Scholar] [CrossRef]
- Carver, C.S. You want to measure coping but your protocol’s too long: Consider the Brief COPE. Int. J. Behav. Med. 1997, 4, 92–100. [Google Scholar] [CrossRef]
- Morán, C.; Landero, R.; González, M.C. COPE 28: Un análisis psicométrico de la versión en español del Brief COPE. Univ. Psychol. 2010, 9, 543–552. [Google Scholar] [CrossRef]
- Baer, R.A.; Smith, G.T.; Hopkins, J.; Krietemeyer, J.; Toney, L. Using self-report assessment methods to explore facets of mindfulness. Assessment 2006, 13, 27–45. [Google Scholar] [CrossRef]
- Cebolla, A.; Soler, J.; Guillen, V.; Botella, C. Psychometric properties of the Spanish validation of the Five Facets of Mindfulness Questionnaire (FFMQ). Eur. J. Psychiatry 2012, 26, 118–126. [Google Scholar] [CrossRef]
- Neff, K.D. Development and validation of a scale to measure self-compassion. Self Identity 2003, 2, 223–250. [Google Scholar] [CrossRef]
- Gillanders, D.T.; Bolderston, H.; Bond, F.W.; Dempster, M.; Flaxman, P.E.; Campbell, L.; Remington, B. The development and initial validation of the Cognitive Fusion Questionnaire. Behav. Ther. 2014, 45, 83–101. [Google Scholar] [CrossRef] [PubMed]
- Romero-Moreno, R.; Márquez-González, M.; Losada, A.; Gillanders, D.T.; Fernández- Fernández, V. Cognitive fusion in dementia caregiving: Psychometric properties of the Spanish version of the Cognitive Fusion Questionnaire. Behav. Psychol. 2014, 22, 117–132. [Google Scholar]
- Kabat-Zinn, J. Vivir con Plenitud las Crisis: Cómo Utilizar la Sabiduría del Cuerpo y de la Mente para Enfrentarnos al Estrés, el Dolor y la Enfermedad; Editorial Kairos: Barcelona, Spain, 2016. [Google Scholar]
- Kabat-Zinn, J. La práctica de la atención plena. Available online: https://www.casadellibro.com/libro-la-practica-de-la-atencion-plena/9788472456464/1160091 (accessed on 10 September 2020).
- Kabat-Zinn, J. Mindfulness en la Vida Cotidiana. Donde Quiera que Vayas Ahí Estás; Paidós: Barcelona, Spain, 2009. [Google Scholar]
- Segal, Z.V.; Williams, J.M.; Teasdale, J.D. Terapia Cognitiva de la Depresión Basada en la Consciencia Plena. Un Nuevo Abordaje Para la Prevención de las Recaídas; Desclée de Brouwer: Bilbao, Spain, 2006. [Google Scholar]
- López-López, J.C.; Luciano, C. An experimental analysis of defusion interactions based on deictic and hierarchical framings and their impact on cognitive performance. Psychol. Rec. 2017, 67, 485–497. [Google Scholar] [CrossRef]
- Hayes, S.C.; Strosahl, K.D.; Wilson, K.G. Acceptance and Commitment Therapy: The Process and Practice of Mindful Change; Guilford Press: New York, NY, USA, 2011. [Google Scholar]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).