Vulnerabilities to COVID-19 in Bangladesh and a Reconsideration of Sustainable Development Goals
Abstract
1. Introduction
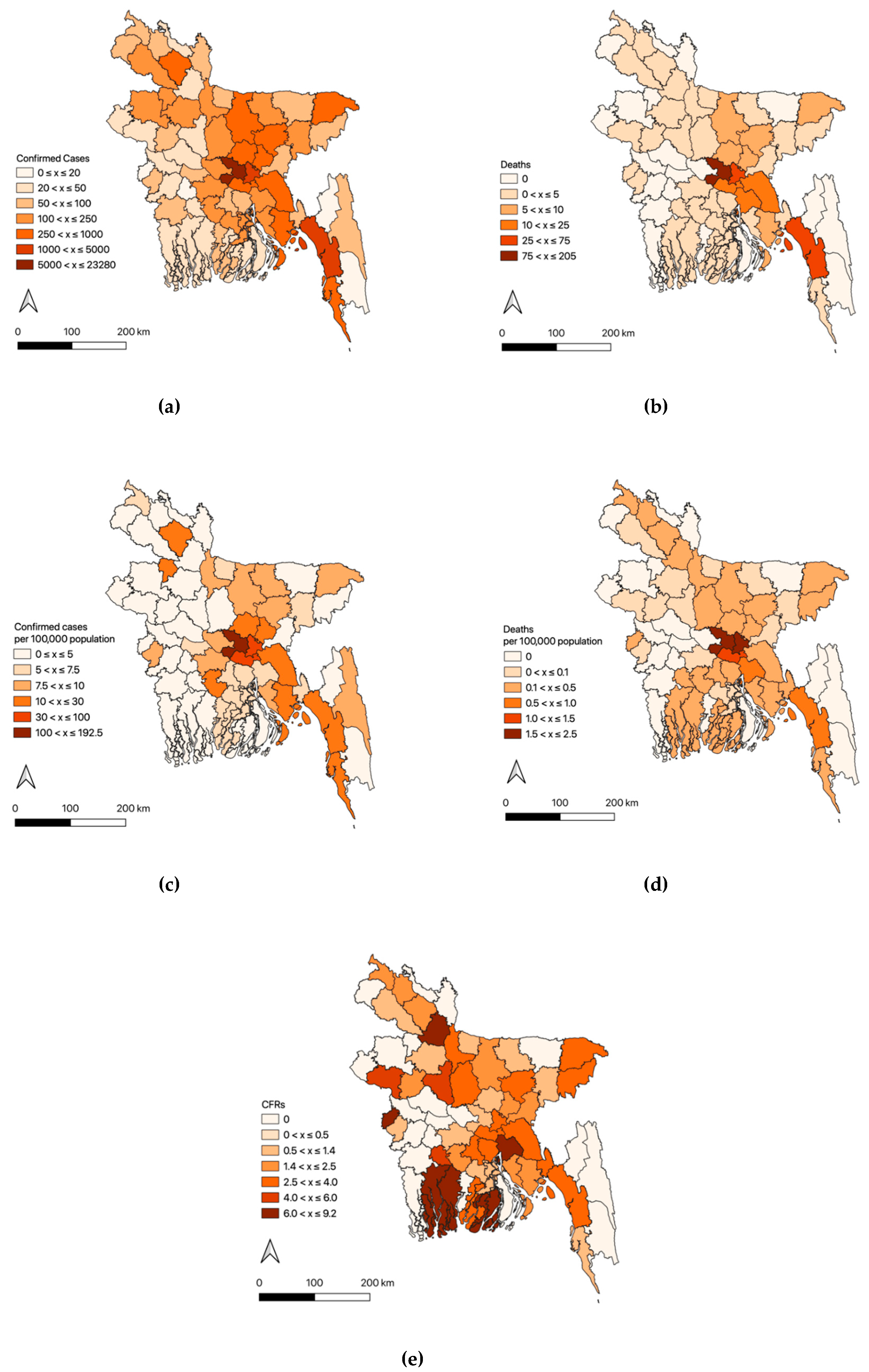
2. Chronology and Epidemiology of COVID-19 in Bangladesh
3. Vulnerabilities to COVID-19
3.1. Garment Industry: Garment Workers
3.2. Financial Vulnerabilities: Slum Dwellers
3.3. Social Exclusion: Rohingya Refugees and Dalits
3.4. Pre-Existing Health Conditions: High Non-Communicable Diseases Risk Holders
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Coronavirus: BGMEA Says Orders Worth $3.15 Billion Cancelled So Far. 12 April 2020. Available online: https://www.dhakatribune.com/bangladesh/2020/04/12/coronavirus-bgmea-reports-3-15-billion-in-order-cancellations (accessed on 19 June 2020).
- Anner, M. Abandoned? The Impact of Covid-19 on Workers and Businesses at the Bottom of Global Garment Supply Chains, Research Report. Pennstate Center for Global Workers’ Rights in Association with the Worker Rights Consortium. 27 March 2020. Available online: https://www.workersrights.org/wp-content/uploads/2020/03/Abandoned-Penn-State-WRC-Report-March-27-2020.pdf (accessed on 10 May 2020).
- ADB. The Informal Sector and Informal Employment in Bangladesh Country Report 2010. 2010. Available online: https://www.adb.org/sites/default/files/publication/30084/informal-sector-informal-employment-bangladesh.pdf (accessed on 19 June 2020).
- Mclean, D. Calls for Inclusion of Migrants and Displaced in COVID-19 Response. 9 April 2020. Available online: https://www.undrr.org/news/calls-inclusion-migrants-and-displaced-covid-19-response (accessed on 19 June 2020).
- Institute of Epidemiology, Disease Control and Research (IEDCR). Bangladesh Covid-19 Update. 24 May 2020. Available online: http://iedcr.gov.bd (accessed on 19 June 2020).
- All Mass Transport Services to Be Shut Down If Coronavirus Situation Worsens. 20 March 2020. Available online: https://www.dhakatribune.com/bangladesh/2020/03/20/coronavirus-all-transportation-services-will-shut-down-if-situation-deteriorates (accessed on 19 June 2020).
- Coronavirus: Govt Extends Holiday Until May 5. 23 April 2020. Available online: https://unb.com.bd/category/Bangladesh/govt-extends-holiday-until-may-5/50330 (accessed on 19 June 2020).
- Govt extends Shutdown Till May 16. 4 May 2020. Available online: https://www.dhakatribune.com/health/coronavirus/2020/05/04/bangladesh-extends-shutdown-till-may-16 (accessed on 19 June 2020).
- WHO. Coronavirus Disease (COVID-2019) Bangladesh Situation Reports-13. 25 May 2020. Available online: https://www.who.int/bangladesh/emergencies/coronavirus-disease-(covid-19)-update/coronavirus-disease-(covid-2019)-bangladesh-situation-reports (accessed on 19 June 2020).
- World Bank. Bangladesh Interactive Poverty Maps. 10 November 2016. Available online: https://www.worldbank.org/en/data/interactive/2016/11/10/bangladesh-poverty-maps (accessed on 19 June 2020).
- WHO. Coronavirus Disease (COVID-2019) Bangladesh Situation Reports-9. 27 April 2020. Available online: https://www.who.int/bangladesh/emergencies/coronavirus-disease-(covid-19)-update/coronavirus-disease-(covid-2019)-bangladesh-situation-reports (accessed on 19 June 2020).
- Wikipedia. Mortality Due to COVID-19. Available online: https://en.wikipedia.org/wiki/Mortality_due_to_COVID-19 (accessed on 25 May 2020).
- Share of Under-60 Age Group in India’s Covid Deaths Rises. 1 May 2020. Available online: https://timesofindia.indiatimes.com/india/share-of-under-60-age-group-in-indias-covid-deaths-rises/articleshow/75481761.cms (accessed on 19 June 2020).
- Antara, I.J. Rapid Research Response to Covid-19. Series: Gender 04, Research Update. 20 May 2020. Available online: https://bigd.bracu.ac.bd/wp-content/uploads/2020/05/Phase-II_Media-Tracking_RMG-TU.pdf (accessed on 19 June 2020).
- Covid-19 Impact and Responses: Bangladesh. 13 May 2020. Available online: https://www.fairwear.org/covid-19-dossier/covid-19-guidance-for-production-countries/covid-19-impact-and-responses-bangladesh/ (accessed on 19 June 2020).
- Workers’ Wages Rise in 6 Grades, RMG Workers’ Pay Structure Revised after PM’s Directive Amid Unrest for Eight Days. 14 January 2019. Available online: https://www.thedailystar.net/business/bangladesh-garment-workers-salary-structure-be-revised-1686979 (accessed on 19 June 2020).
- Why Are Wages So Low for Garment Workers in Bangladesh? Country Offers Cheap Labour and Manufacturing Expertise–with Often Limited Oversight. 21 January 2019. Available online: https://www.theguardian.com/business/2019/jan/21/low-wages-garment-workers-bangladesh-analysis (accessed on 19 June 2020).
- Starving’ Bangladesh Garment Workers Protest for Pay during COVID-19 Lockdown. 13 April 2020. Available online: https://www.arabnews.com/node/1658186/world (accessed on 19 June 2020).
- Haque, M.F.; Sarker, M.A.R.; Rahman, M.S.; Rakibuddin, M. Discrimination of Women at RMG Sector in Bangladesh. J. Soc. Political Sci. 2020, 3, 112–118. [Google Scholar] [CrossRef]
- Kabir, H.; Maple, M.; Fatema, S.R. Vulnerabilities of Women Workers in the Readymade Garment Sector of Bangladesh: A Case Study of Rana Plaza. J. Int. Women’s Stud. 2018, 19, 224–235. Available online: http://vc.bridgew.edu/jiws/vol19/iss6/14 (accessed on 19 June 2020).
- Sili, L. The economic gender gap in the garment sector in Bangladesh and Ghana. 31 January 2018. Available online: https://www.theigc.org/blog/economic-gender-gap-garment-sector-bangladesh-ghana (accessed on 19 June 2020).
- Coronavirus: Two Million Bangladesh Jobs ‘at Risk’ as Clothes Orders Dry up. 29 April 2020. Available online: https://www.bbc.com/news/world-asia-52417822 (accessed on 19 June 2020).
- COVID-19: Are We Preparing the Homeless and Slum-Dwellers? 27 March 2020. Available online: http://unb.com.bd/category/Special/covid-19-are-we-preparing-the-homeless-and-slum-dwellers/48033 (accessed on 19 June 2020).
- Haider, M. Bangladesh: Transforming Life in the Slums. 2020. Available online: https://www.undp.org/content/undp/en/home/ourwork/ourstories/bangladesh--how-to-transform-life-in-the-slum.html (accessed on 19 June 2020).
- Dhaka’s Slums in the Dark about Covid-19. 22 March 2020. Available online: https://www.dhakatribune.com/health/2020/03/22/capital-s-slums-in-the-dark-about-covid-19 (accessed on 19 June 2020).
- Coronavirus: Poor Income Drops 80% in Bangladesh. 17 April 2020. Available online: https://www.aa.com.tr/en/asia-pacific/coronavirus-poor-income-drops-80-in-bangladesh/1808837 (accessed on 19 June 2020).
- Bangladesh Poor Slum Dwellers under Shadow of Covid-19. 6 April 2020. Available online: http://www.uniindia.com/bangladesh-s-poor-slum-dwellers-under-shadow-of-covid-19/world/news/1943758.html (accessed on 19 June 2020).
- Transparency International Bangladesh (TIB). Indigenous and Dalit Peoples of Bangladesh: Challenges and Way Forward for Inclusion in Rights and Services. March 2019. Available online: https://www.ti-bangladesh.org/beta3/index.php/en/communications/reports/research-report (accessed on 19 June 2020).
- Buvinic, M. Social Inclusion in Latin America. In Social Exclusion and Economic Development; Buvinici, M., Mazza, J., Eds.; Baltimore Johns Hopkins University Press: Baltimore, MD, USA, 2005. [Google Scholar]
- Thorat, S.; Newman, K.S. Caste and economic discrimination: Causes, consequences and remedies. Econ. Political Wkly. 2007, 42, 4121–4124. [Google Scholar]
- Hossain, M.S. Multiple Deprivations: Schooling Experience of Dalit Children in Bangladesh. Master’s Thesis, University in the Hague, Hague, The Netherlands, 2016. [Google Scholar]
- Coronavirus: Bangladesh Locks Down a Million in Rohingya Camps. 9 April 2020. Available online: https://www.bbc.com/news/world-asia-52227924 (accessed on 19 June 2020).
- 3 More Rohingyas Test Positive for Covid-19 in Cox’s Bazar. 15 May 2020. Available online: https://www.dhakatribune.com/bangladesh/nation/2020/05/15/3-more-rohingya-test-positive-for-covid-19-in-cox-s-bazar (accessed on 19 June 2020).
- Coronavirus: Rohingya Camps at Risk as Tests Slow Down. 17 April 2020. Available online: https://www.dhakatribune.com/bangladesh/2020/04/17/coronavirus-rohingya-camps-under-risk-as-tests-slow-down (accessed on 19 June 2020).
- Risk Report, 2020, COVID-19 Impact on the Rohingya Response. 20 March 2020. Available online: https://www.acaps.org20200319 (accessed on 19 June 2020).
- Ahmed, B.; Orcutt, M.; Sammonds, P.; Burns, R.; Issa, R.; Abubakar, I.; Devakumar, D. Humanitarian Disaster for Rohingya Refugees: Impending Natural Hazards and Worsening Public Health Crises. Lancet Glob. Health 2018, 6, E487–E488. [Google Scholar] [CrossRef]
- International Dalit Solidarity Network (IDSN). Dalits of Bangladesh: Destined to a Life of Humiliation. 2006. Available online: https://idsn.org/ (accessed on 19 June 2020).
- Rahman, S. An Ethnographic Journey Through the Lives of Urban Dalits in Bangladesh, Final Report. 2016. Available online: https://bdplatform4sdgs.net/wp-content/uploads/2016/08/An-Ethnographic-Journey-Through-the-Lives-of-Urban-Dalits-in-Bangladesh.pdf (accessed on 19 June 2020).
- Kabir, A.; Farhana, N.; Akter, F.; Jesmin, S.; Ali, A. Sweeping practices, perceptions and knowledge about occupational safety and health hazards of street sweepers in Dhaka city, Bangladesh: A qualitative inquiry. Int. J. Community Med. Public Health 2015, 2, 237–243. [Google Scholar] [CrossRef]
- Plaban, G. Impact of COVID-19 on Waste and Sanitation Workers. 11 May 2020. Available online: https://www.thedailystar.net/opinion/news/impact-covid-19-waste-and-sanitation-workers-1901353 (accessed on 19 June 2020).
- United Nations Development Programme. Australia and UNDP Work Together with Bangladesh Govt in Combating COVID-19. 29 April 2020. Available online: https://www.bd.undp.org/content/bangladesh/en/home/presscenter/pressreleases/2020/04/29/australia-and-undp-work-together-with-bangladesh-govt-in-combati.html (accessed on 19 June 2020).
- Cesare, M.D.; Khang, Y.H.; Asaria, P.; Blakely, T.; Cowan, M.J.; Farzadfar, F.; Guerrero, R.; Ikeda, N.; Kyobutungi, C.; Msyamboza, K.P.; et al. Inequalities in Non-communicable Diseases and Effective Responses. Lancet 2013, 381, 585–597. [Google Scholar] [CrossRef]
- WHO. Arsenic-Mass Poisoning on an Unprecedented Scale. Global Status Report on Noncommunicable Diseases; WHO: Geneva, Switzerland, 2014. [Google Scholar]
- Khalequzzaman, M.; Chiang, C.; Choudhury, S.R.; Yatsuya, H.; Al-Mamun, M.A.; Al-Shoaibi, A.A.A.; Hirakawa, Y.; Hoque, B.A.; Islam, S.S.; Matsuyama, A.; et al. Prevalence of non-communicable disease risk factors among poor shantytown residents in Dhaka, Bangladesh: A community-based cross-sectional survey. BMJ Open 2017, 7, e014710. [Google Scholar] [CrossRef] [PubMed]
- WHO. Diabetes Country Profiles, Bangladesh. 2016. Available online: http://www.who.int/diabetes/country-profiles/bgd_en.pdf?ua=1 (accessed on 19 June 2020).
- Rawal, L.B.; Biswas, T.; Khandker, N.N.; Saha, S.R.; Chowdhury, M.M.B.; Khan, A.N.S.; Chowdhury, E.H.; Renzaho, A. Non-communicable disease (NCD) risk factors and diabetes among adults living in slum areas of Dhaka, Bangladesh. PLoS ONE 2017, 12, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, A. The Bangladesh Integrated Planning for Sustainable Water Management (IPSWAM) Programme, and Climate Change; Bangladesh Water Development Board: Dhaka, Bangladesh, 2006. [Google Scholar]
- Allison, M.A.; Khan, S.R.; Goodbred, S.L., Jr.; Kuehl, S.A. Stratigraphic evolution of the late Holocene Ganges-Brahmaputra lower delta plain. Sediment. Geol. 2003, 155, 317–342. [Google Scholar] [CrossRef]
- Nahian, M.A.; Ahmed, A.; Lázár, A.N.; Hutton, C.W.; Salehin, M.; Streatfield, P.K. Drinking water salinity associated health crisis in coastal Bangladesh. Elementa 2018, 6, 143. [Google Scholar] [CrossRef]
- Naser, A.M.; Rahman, M.; Unicomb, L.; Doza, S.; Ahmed, K.M.; Uddin, M.N.; Selim, S.; Gribble, M.O.; Anand, S.; Clasen, T.F.; et al. Drinking Water Salinity and Kidney Health in Southwest Coastal Bangladesh: Baseline Findings of a Community-based Stepped-wedge Randomised trial. Lancet 2017, 389, S15. [Google Scholar] [CrossRef]
- Khan, A.W.; Ahmad, S.A.; Sayed, S.; Hadi, A.S.; Khan, M.H.; Jalil, A.M.; Ahmed, R.; Faruquee, M. Arsenic contamination in ground water and its effect on human health with particular reference to Bangladesh. J. Prev. Soc. Med. 1997, 16, 65–73. [Google Scholar]
- WHO. Arsenic-Mass Poisoning on an Unprecedented Scale. March 2002. Available online: https://www.who.int/features/archives/feature206/en/ (accessed on 19 June 2020).
- Department of Public Health Engineering (DPHE). Status of Water Points. June 2018. Available online: http://old.dphe.gov.bd/download/Status%20of%20Water%20Points/Status%20Report%20June%202018.pdf (accessed on 19 June 2020).
- Sakamoto, M. Revisiting the village where arsenic contamination of underground water was first discovered in Bangladesh: Twenty-five years later. Unpublished work.
- Roh, T.; Steinmaus, C.; Marshall, G.; Ferreccio, C.; Liaw, J.; Smith, A.H. Age at Exposure to Arsenic in Water and Mortality 30–40 Years after Exposure Cessation. Am. J. Epidemiol. 2018, 187, 2297–2305. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.; Sohel, N.; Yunus, F.M.; Alam, N.; Nahar, Q.; Streatfield, P.K.; Yunus, M. Arsenic Exposure and Young Adult’s Mortality risk: A 13-year Follow-up Study in Matlab, Bangladesh. Environ. Int. 2019, 123, 358–367. [Google Scholar] [CrossRef] [PubMed]
- BGS & DPHE. Arsenic Contamination of Groundwater in Bangladesh. In British Geological Survey Technical Report WC/00/1; Kinniburgh, D.G., Smedley, P.L., Eds.; Keyworth: British Geological Survey: Nottingham, UK, 2001. [Google Scholar]
- World Bank. WB Update Says 10 Countries Move up in Income Bracket. 1 July 2015. Available online: https://www.worldbank.org/en/news/press-release/2015/07/01/new-world-bank-update-shows-bangladesh-kenya-myanmar-and-tajikistan-as-middle-income-while-south-sudan-falls-back-to-low-income (accessed on 19 June 2020).
- Sakamoto, M.; Ahmed, T.; Begum, S.; Huq, H. Water Pollution and the Textile Industry in Bangladesh: Flawed Corporate Practices or Restrictive Opportunities? Sustainability 2019, 11, 1951. [Google Scholar] [CrossRef]
| CorrelationCoefficient | 95% CIs | p-Value | Mean | SD | |
|---|---|---|---|---|---|
| Confirmed Cases per population | |||||
| Rural Population (%) | −0.778 | (−0.859, −0.658) | 0.000 | 82.2 | 10.2 |
| Primary employment: Agriculture (%) | −0.654 | (−0.762, −0.461) | 0.000 | 57.0 | 15.3 |
| Educational attainment:University completed (%) | 0.796 | (0.683, 0.871) | 0.000 | 2.78 | 1.56 |
| Households with tap water (%) | 0.854 | (0.769, 0.909) | 0.000 | 5.04 | 9.74 |
| Deaths per population | |||||
| Primary employment: Agriculture (%) | −0.709 | (−0.813, −0.5600 | 0.000 | 57.0 | 15.3 |
| Rural Population (%) | −0.569 | (−0.715, −0.376) | 0.000 | 82.2 | 10.2 |
| Households with Electricity (%) | 0.625 | (0.448, 0.755) | 0.000 | 50.1 | 17.1 |
| Primary employment: Industry (%) | 0.628 | (0.452, 0.757) | 0.000 | 10.4 | 8.51 |
| CFR | |||||
| Population ages 65 and above (%) | 0.222 | (−0.025, 0.444) | 0.077 | 4.99 | 0.83 |
| Age Group in Years | Number of Cases | % of Total | Number of Deaths | CFR |
|---|---|---|---|---|
| 0 to 4 | 17 | 0.6 | 2 | 11.8 |
| 5 to 14 | 134 | 5.1 | 0 | 0.00 |
| 15 to 24 | 526 | 19.9 | 1 | 0.20 |
| 24 to 34 | 556 | 21.1 | 2 | 0.40 |
| 35 to 44 | 492 | 18.6 | 9 | 1.60 |
| 45 to 54 | 417 | 15.8 | 18 | 4.30 |
| 55 to 64 | 283 | 10.7 | 30 | 10.6 |
| 65 to74 | 116 | 4.4 | 18 | 15.5 |
| 75 to 84 | 69 | 2.6 | 4 | 5.8 |
| > = 85 | 30 | 1.1 | 4 | 13.3 |
| Total | 2,640 | 100 | 87 | 3.3 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sakamoto, M.; Begum, S.; Ahmed, T. Vulnerabilities to COVID-19 in Bangladesh and a Reconsideration of Sustainable Development Goals. Sustainability 2020, 12, 5296. https://doi.org/10.3390/su12135296
Sakamoto M, Begum S, Ahmed T. Vulnerabilities to COVID-19 in Bangladesh and a Reconsideration of Sustainable Development Goals. Sustainability. 2020; 12(13):5296. https://doi.org/10.3390/su12135296
Chicago/Turabian StyleSakamoto, Maiko, Salma Begum, and Tofayel Ahmed. 2020. "Vulnerabilities to COVID-19 in Bangladesh and a Reconsideration of Sustainable Development Goals" Sustainability 12, no. 13: 5296. https://doi.org/10.3390/su12135296
APA StyleSakamoto, M., Begum, S., & Ahmed, T. (2020). Vulnerabilities to COVID-19 in Bangladesh and a Reconsideration of Sustainable Development Goals. Sustainability, 12(13), 5296. https://doi.org/10.3390/su12135296





