Social Capital and Self-Rated Health among Older Adults Living in Urban China: A Mediation Model
Abstract
:1. Introduction
1.1. Defining Social Capital
1.2. Cognitive Social Capital, Structural Social Capital, and SRH
2. Materials and Methods
2.1. Sampling
2.2. Measurements
2.3. Data Analysis
3. Results
3.1. Sample Characteristics
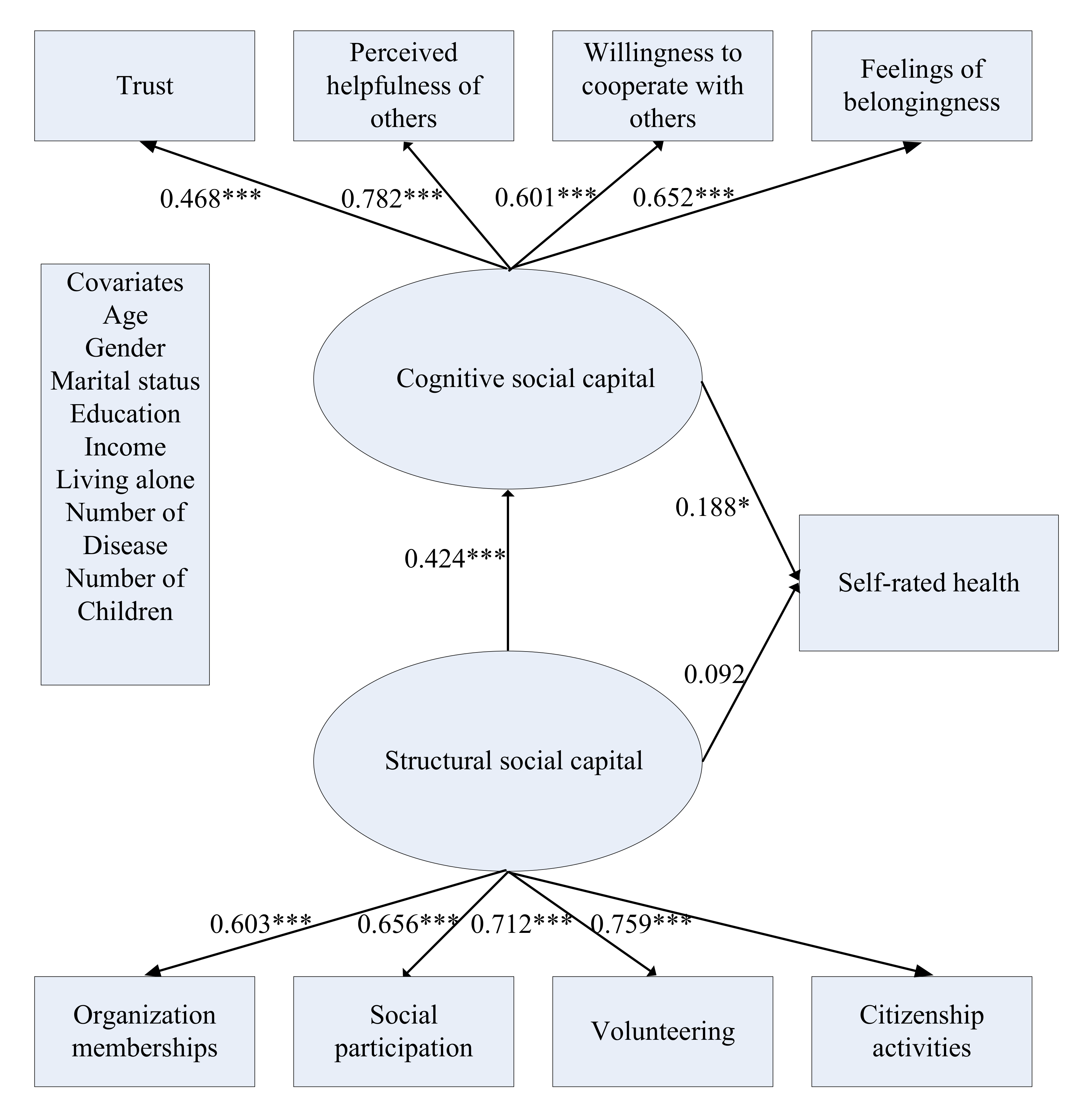
3.2. Measurement Model
3.3. Direct Effect of Structural Social Capital on SRH
3.4. Mediating Role of Cognitive Social Capital
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- National Bureau of Statistics of China. China Statistical Yearbook–2018; China Statistics Press: Beijing, China, 2018.
- Shum, M.H.; Lou, V.W.; He, K.Z.; Chen, C.C.; Wang, J. The “Leap Forward” in Nursing Home Development in Urban China: Future Policy Directions. J. Am. Med. Dir. Assoc. 2015, 16, 784–789. [Google Scholar] [CrossRef] [PubMed]
- Schnittker, J.; Bacak, V. The Increasing Predictive Validity of Self-Rated Health. PLoS ONE 2014, 9, e84933. [Google Scholar] [CrossRef] [PubMed]
- Garbarski, D. Research in and Prospects for the Measurement of Health Using Self-Rated Health. Public Opin. Q. 2016, 80, 977–997. [Google Scholar] [CrossRef] [Green Version]
- Haring, R.; Feng, Y.-S.; Moock, J.; Völzke, H.; Dörr, M.; Nauck, M.; Wallaschofski, H.; Kohlmann, T. Self-perceived quality of life predicts mortality risk better than a multi-biomarker panel, but the combination of both does best. BMC Med. Res. Methodol. 2011, 11, 103. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Wang, R.; Zhao, Y.; Ma, X.; Wu, M.; Yan, X.; He, J. The relationship between self-rated health and objective health status: A population-based study. BMC Public Heal. 2013, 13, 320. [Google Scholar] [CrossRef]
- Yiengprugsawan, V.; Welsh, J.; Kendig, H. Social capital dynamics and health in mid to later life: Findings from Australia. Qual. Life Res. 2018, 27, 1277–1282. [Google Scholar] [CrossRef] [PubMed]
- Yip, W.; Subramanian, S.; Mitchell, A.D.; Lee, D.T.; Wang, J.; Kawachi, I. Does social capital enhance health and well-being? Evidence from rural China. Soc. Sci. Med. 2007, 64, 35–49. [Google Scholar] [CrossRef]
- Norstrand, J.A.; Xu, Q. Social Capital and Health Outcomes Among Older Adults in China: The Urban-Rural Dimension. Gerontology 2011, 52, 325–334. [Google Scholar] [CrossRef] [Green Version]
- Schultz, J.; O’Brien, A.M.; Tadesse, B. Social capital and self-rated health: Results from the US 2006 social capital survey of one community. Soc. Sci. Med. 2008, 67, 606–617. [Google Scholar] [CrossRef]
- LaPalombara, J.; Putnam, R.D. Making Democracy Work: Civic Traditions in Modern Italy. Polit. Sci. Q. 1993, 108, 549. [Google Scholar] [CrossRef]
- Coleman, J.S. Foundations of Social Theory; Harvard University Press: Cambridge, MA, USA, 1990. [Google Scholar]
- Lin, N. Building a network theory of social capital. Connections 1999, 22, 28–51. [Google Scholar]
- Nyqvist, F.; Cattan, M.; Andersson, L.; Forsman, A.K.; Gustafson, Y. Social capital and loneliness among the very old living at home and in institutional settings: A comparative study. J. Aging Health 2013, 25, 1013–1035. [Google Scholar] [CrossRef]
- Kawachi, I.; Kennedy, B.P.; Glass, R. Social capital and self-rated health: A contextual analysis. Am. J. Public Health 1999, 89, 1187–1193. [Google Scholar] [CrossRef] [PubMed]
- Perry, M.; Williams, R.L.; Wallerstein, N.; Waitzkin, H. Social Capital and Health Care Experiences Among Low-Income Individuals. Am. J. Public Health 2008, 98, 330–336. [Google Scholar] [CrossRef] [PubMed]
- Agampodi, T.C.; Agampodi, S.B.; Glozier, N.; Siribaddana, S. Measurement of social capital in relation to health in low and middle income countries (LMIC): A systematic review. Soc. Sci. Med. 2015, 128, 95–104. [Google Scholar] [CrossRef] [PubMed]
- Poortinga, W.; Dunstan, F.D.; Fone, D.L. Neighbourhood deprivation and self-rated health: The role of perceptions of the neighbourhood and of housing problems. Health Place 2008, 14, 562–575. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, K.L.; Quinn, S.C.; Goodman, R.M.; Butler, J.; Wallace, J. A meta-analysis of social capital and health: A case for needed research. J. Health Psychol. 2013, 18, 1385–1399. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ehsan, A.; Klaas, H.S.; Bastianen, A.; Spini, D. Social capital and health: A systematic review of systematic reviews. SSM Popul. Health 2019, 8, 100425. [Google Scholar] [CrossRef]
- Snelgrove, J.W.; Pikhart, H.; Stafford, M. A multilevel analysis of social capital and self-rated health: Evidence from the British Household Panel Survey. Soc. Sci. Med. 2009, 68, 1993–2001. [Google Scholar] [CrossRef] [PubMed]
- Lau, Y.K.; E Ataguba, J. Investigating the relationship between self-rated health and social capital in South Africa: A multilevel panel data analysis. BMC Public Health 2015, 15, 266. [Google Scholar] [CrossRef]
- Koutsogeorgou, E.; Nyqvist, F.; Nygard, M.; Cerniauskaite, M.; Quintas, R.; Raggi, A.; Leonardi, M. Social capital and self-rated health among older adults: A comparative analysis of Finland, Poland and Spain. Ageing Soc. 2015, 35, 653–667. [Google Scholar] [CrossRef]
- Pollack, C.E.; Knesebeck, O.V.D. Social capital and health among the aged: Comparisons between the United States and Germany. Health Place 2004, 10, 383–391. [Google Scholar] [CrossRef] [PubMed]
- Collplanas, L.; Gomez, G.D.V.; Bonilla, P.; Masat, T.; Puig, T.; Monteserin, R. Promoting social capital to alleviate loneliness and improve health among older people in Spain. Health Soc. Care Comm. 2017, 25, 145–157. [Google Scholar] [CrossRef] [PubMed]
- Brehm, J.; Rahn, W. Individual-Level Evidence for the Causes and Consequences of Social Capital. Am. J. Polit. Sci. 1997, 41, 999. [Google Scholar] [CrossRef] [Green Version]
- Lindström, M. Social capital, the miniaturisation of community and self-reported global and psychological health. Soc. Sci. Med. 2004, 59, 595–607. [Google Scholar] [CrossRef] [PubMed]
- Benyamini, Y.; Idler, E.L. Self-Rated Health and Mortality: A Review of Twenty-Seven Community Studies. J. Health Soc. Behav. 1997, 38, 21. [Google Scholar] [Green Version]
- Wolinsky, F.D.; Tierney, W.M. Self-Rated Health and Adverse Health Outcomes: An Exploration and Refinement of the Trajectory Hypothesis. J. Gerontol. Ser. B 1998, 53, S336–S340. [Google Scholar] [CrossRef] [Green Version]
- Pfeiffer, E. A Short Portable Mental Status Questionnaire for the Assessment of Organic Brain Deficit in Elderly Patients†. J. Am. Geriatr. Soc. 1975, 23, 433–441. [Google Scholar] [CrossRef]
- Chi, I.; Boey, K.W. Hong Kong Validation of Measuring Instruments of Mental Health Status of the Elderly. Clin. Gerontol. 1993, 13, 35–51. [Google Scholar] [CrossRef]
- De Silva, M.J.; Huttly, S.R.; Harpham, T.; Kenward, M.G. Social capital and mental health: A comparative analysis of four low income countries. Soc. Sci. Med. 2007, 64, 5–20. [Google Scholar] [CrossRef]
- Grootaert, C.; Narayan, D.; Jones, V.N.; Woolcock, M. Integrated Questionnaire for the Measurement of Social Capital; World Bank: Washington, DC, USA, 2004. [Google Scholar]
- Kline, R.B. Principles and Practice of Structural Equation Modeling, 3rd ed.; The Guilford Press: New York, NY, USA, 2011. [Google Scholar]
- Muthén, L.K.; Muthén, B. Mplus User’s Guide, 6th ed.; Muthén & Muthén: Los Angeles, CA, USA, 2010. [Google Scholar]
- Li, C.H. Confirmatory factor analysis with ordinal data: Comparing robust maximum likelihood and diagonally weighted least squares. Behav. Res. Methods 2016, 48, 936–949. [Google Scholar] [CrossRef] [PubMed]
- Muthén, L.K.; Muthén, B. Mplus User’s Guide, 7th ed.; Muthén & Muthén: Los Angeles, CA, USA, 2012. [Google Scholar]
- Distefano, C.; Liu, J.; Jiang, N.; Shi, D. Examination of the Weighted Root Mean Square Residual: Evidence for trustworthiness? Struct. Equ. Model. 2018, 25, 453–466. [Google Scholar] [CrossRef]
| N (%) | Mean (SD) | |
|---|---|---|
| Age | 70.67 (7.35) | |
| 60–69 | 221 (48.5) | |
| 70–79 | 171 (37.5) | |
| 80 and above | 64 (14.0) | |
| Gender | ||
| Men | 206 (45.2) | |
| Women | 250 (54.8) | |
| Marital status | ||
| Married | 342 (75.0) | |
| Other marital status | 114 (25.0) | |
| Education | ||
| Primary school or lower | 159 (34.9) | |
| Secondary school or above | 295 (64.7) | |
| Monthly household income | ||
| Less than RMB5000 | 243 (53.3) | |
| RMB5000 or above | 209 (45.8) | |
| Self-rated health | ||
| Very good | 47 (10.3) | |
| Good | 186 (40.8) | |
| Fair | 186 (40.8) | |
| Poor | 32 (7.0) | |
| Very poor | 4 (0.9) | |
| Number of children | 1.89 (1.07) | |
| Chronic disease | 1.21 (1.03) | |
| Had respiratory system diseases | 28 (6.1) | |
| Had circulation system diseases | 248 (54.4) | |
| Had musculoskeletal diseases | 117 (25.7) | |
| Had cerebrovascular diseases | 28 (6.1) | |
| Had digestive system diseases | 67 (14.7) | |
| Had endocrine and metabolic diseases. | 66 (14.5) | |
| Living alone | 79 (17.3) |
| Factor indicator | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Trust in local community | 4.12 | 0.82 | 1.00 | |||||||
| 2. Perceived helpfulness of others | 3.55 | 0.94 | 0.35 *** | 1.00 | ||||||
| 3. Willingness to cooperate with others | 3.92 | 0.83 | 0.30 *** | 0.59 *** | 1.00 | |||||
| 4. Feelings of belonging | 4.20 | 0.69 | 0.36 *** | 0.50 *** | 0.60 *** | 1.00 | ||||
| 5. Organization memberships | 1.73 | 1.39 | 0.09 | 0.18 *** | 0.14 ** | 0.18 *** | 1.00 | |||
| 6. Volunteering | 0.35 | 0.48 | 0.06 | 0.23 *** | 0.14 ** | 0.13 ** | 0.30 *** | 1.00 | ||
| 7. Social participation | 3.43 | 1.80 | 0.08 | 0.19 *** | 0.13 ** | 0.15 ** | 0.48 *** | 0.37 *** | 1.00 | |
| 8. Citizenship activities | 0.35 | 0.48 | 0.08 | 0.24 *** | 0.13 ** | 0.12 * | 0.36 *** | 0.35 *** | 0.35 *** | 1.00 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lu, N.; Zhang, J. Social Capital and Self-Rated Health among Older Adults Living in Urban China: A Mediation Model. Sustainability 2019, 11, 5566. https://doi.org/10.3390/su11205566
Lu N, Zhang J. Social Capital and Self-Rated Health among Older Adults Living in Urban China: A Mediation Model. Sustainability. 2019; 11(20):5566. https://doi.org/10.3390/su11205566
Chicago/Turabian StyleLu, Nan, and Jingyue Zhang. 2019. "Social Capital and Self-Rated Health among Older Adults Living in Urban China: A Mediation Model" Sustainability 11, no. 20: 5566. https://doi.org/10.3390/su11205566
APA StyleLu, N., & Zhang, J. (2019). Social Capital and Self-Rated Health among Older Adults Living in Urban China: A Mediation Model. Sustainability, 11(20), 5566. https://doi.org/10.3390/su11205566





