Exploring the Determinants of Online Health Information-Seeking Behavior Using a Meta-Analytic Approach
Abstract
1. Introduction
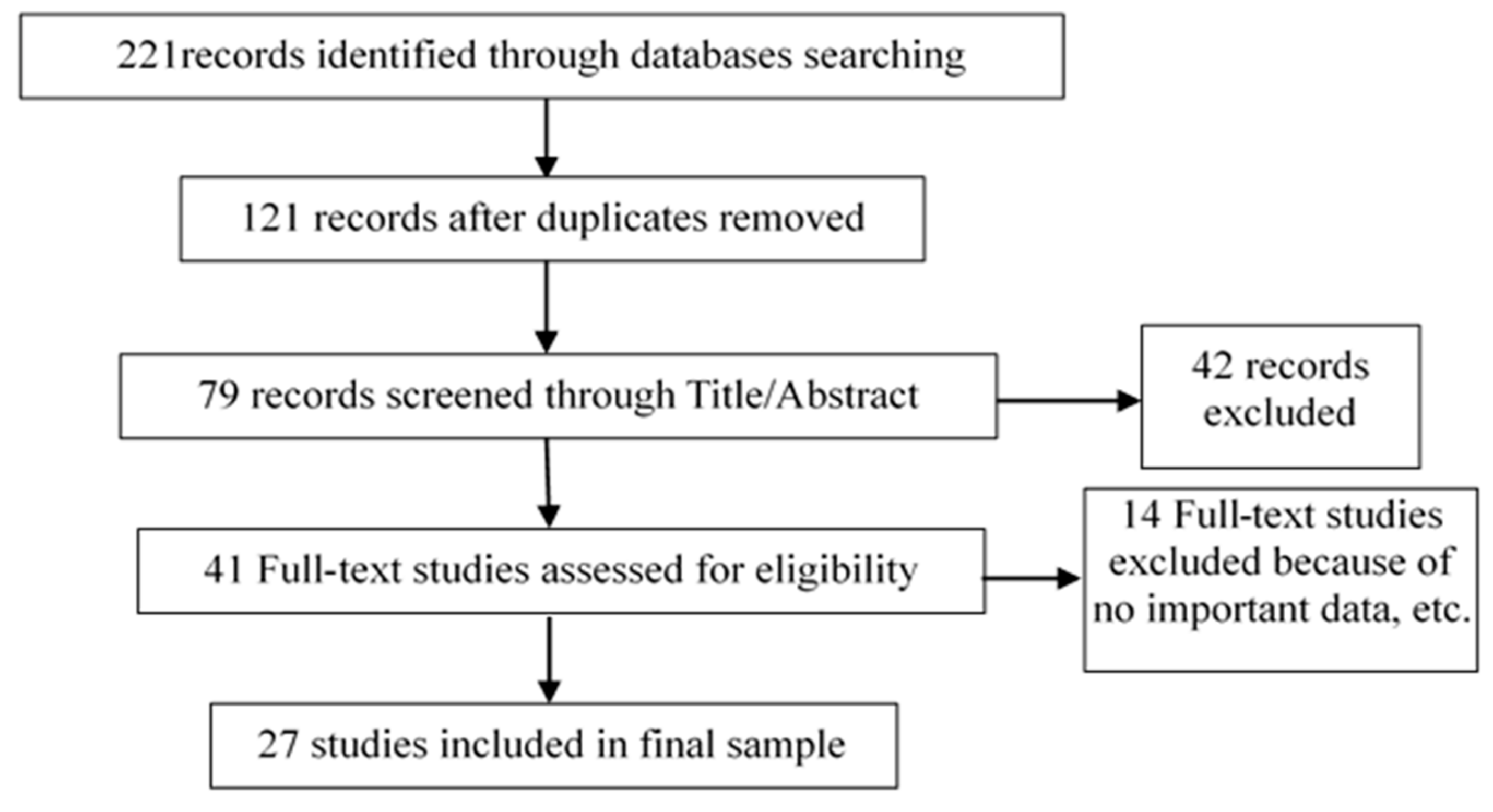
2. Materials and Methods
2.1. Literature Search Strategy
2.2. Selection Criteria for Sample Data and Quality Assessment
Data Collection and Coding
2.3. Meta-Analysis and Effect Size Calculations
3. Results
3.1. Characteristics of the Studies
3.2. Meta-Analysis
3.2.1. Publication Bias Analysis
3.2.2. Heterogeneity Tests
3.3. Meta-Analytic Results
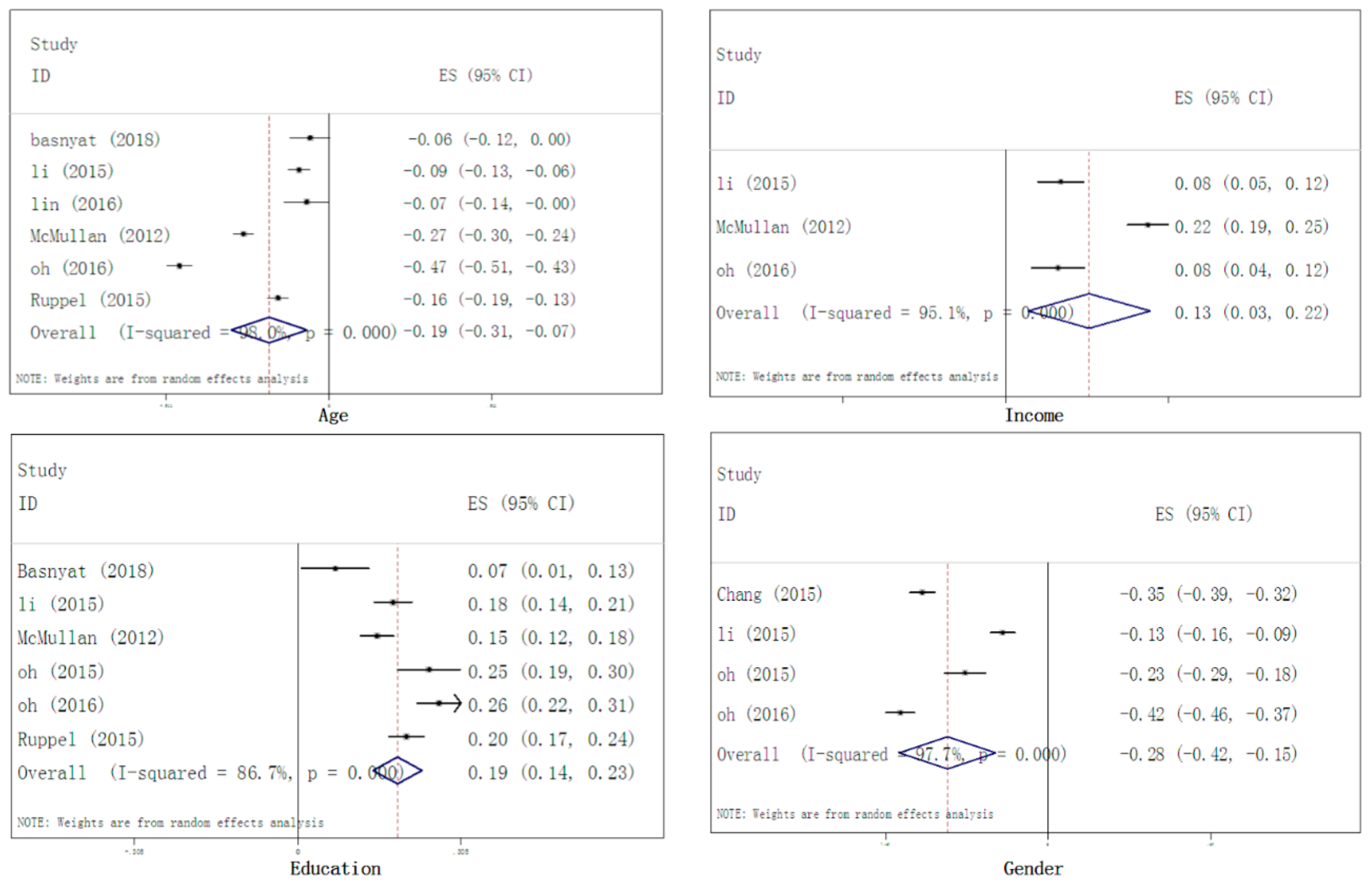
3.3.1. Demographic Characteristics Factors
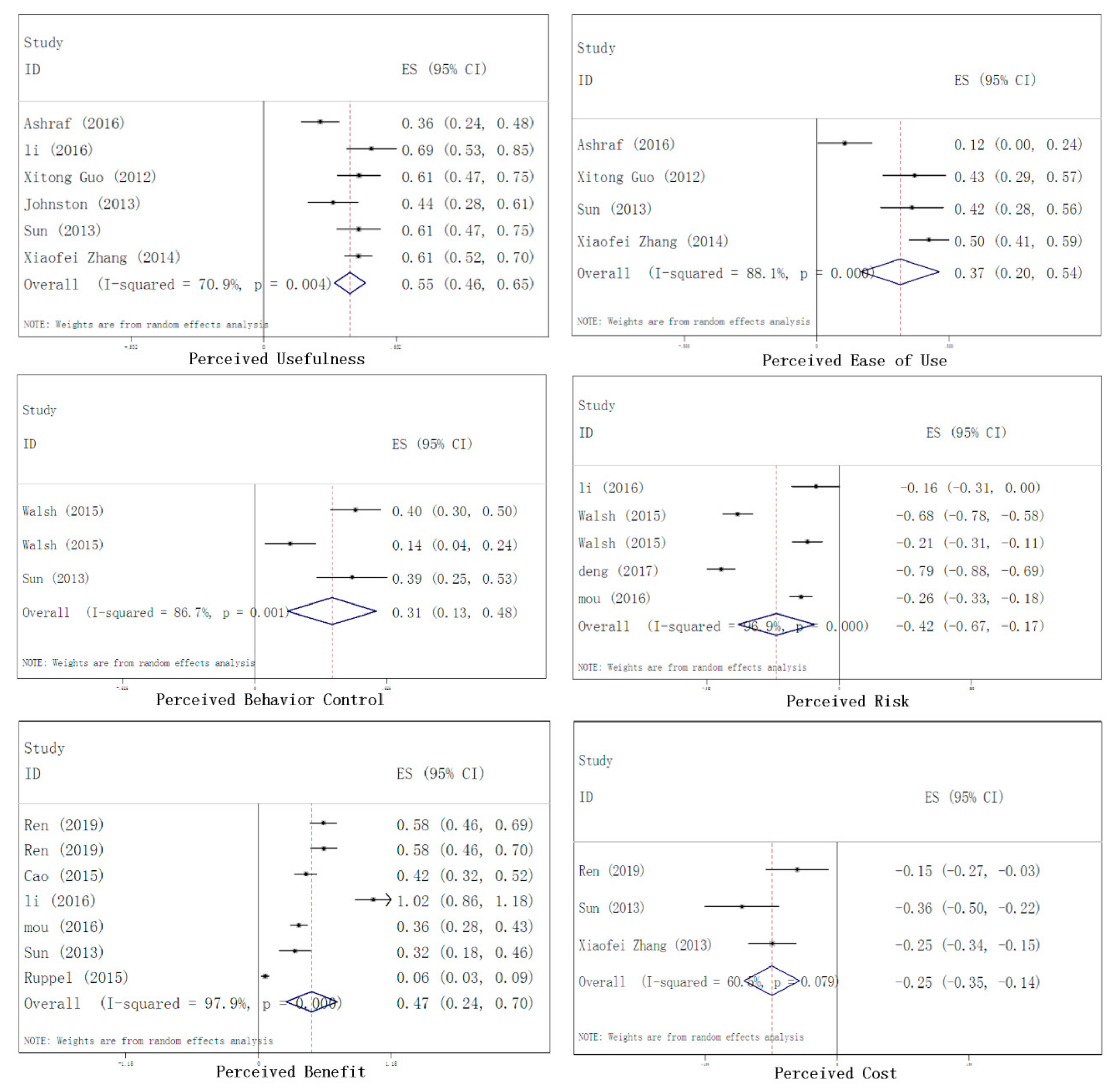
3.3.2. Cognitive Factors
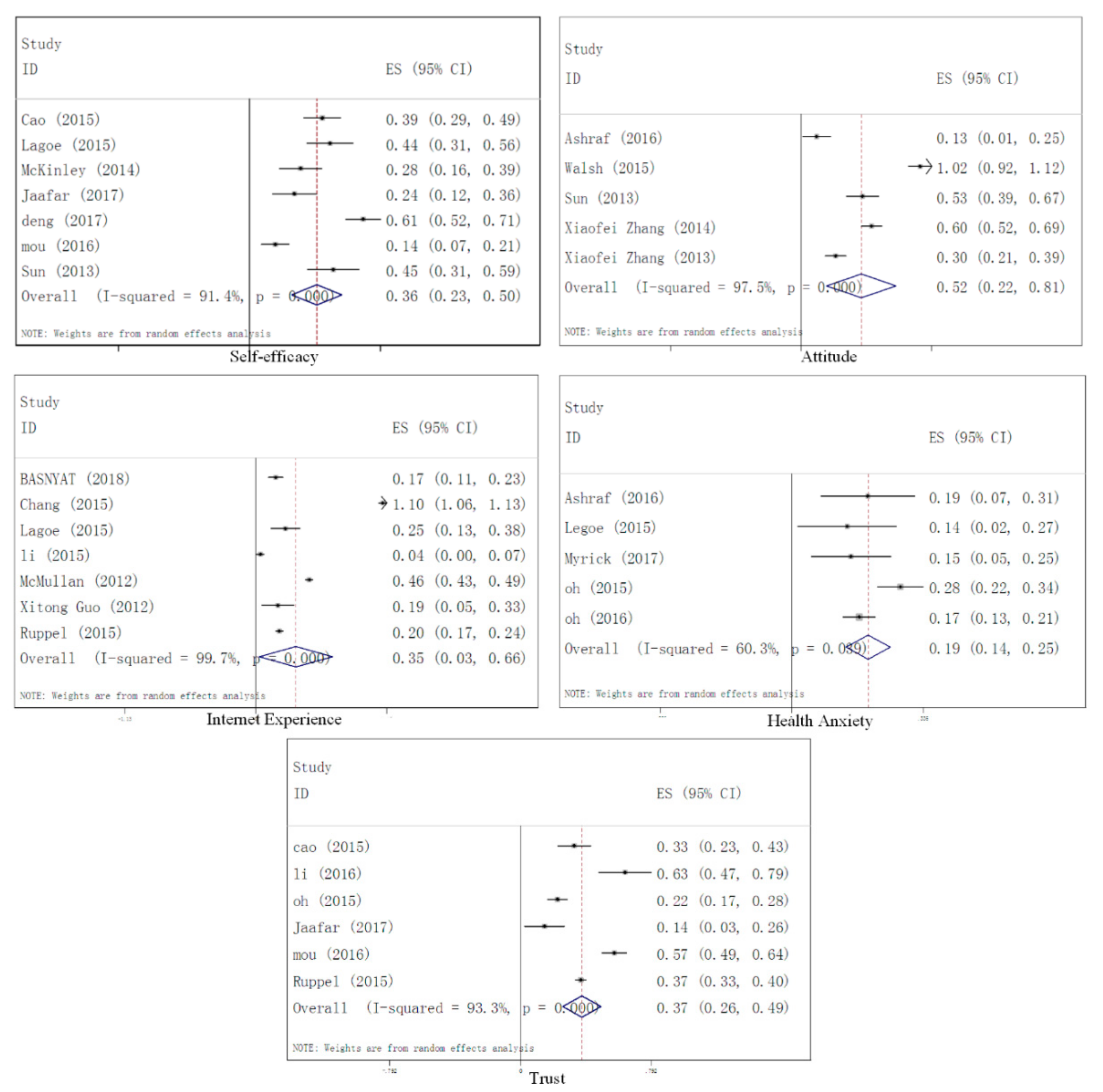
3.3.3. Internal Factors
3.3.4. External Factors
4. Discussion
5. Conclusions
Limitations of the Study and Future Research
Author Contributions
Funding
Conflicts of Interest
References
- Ren, C.; Deng, Z.; Hong, Z.; Zhang, W. Health information in the digital age: An empirical study of the perceived benefits and costs of seeking and using health information from online sources. Health Inf. Libr. J. 2019, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Jaafar, N.I.; Ainin, S.; Yeong, M.W. Why bother about health? A study on the factors that influence health information seeking behaviour among Malaysian healthcare consumers. Int. J. Med. Inform. 2017, 104, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Rowlands, I.J.; Loxton, D.; Dobson, A.; Mishra, G.D. Seeking health information online: Association with young australian women’s physical, mental, and reproductive health. J. Med. Internet Res. 2015, 17, 6–9. [Google Scholar] [CrossRef] [PubMed]
- Wilson, T.D. Human information behavior. Inf. Sci. 2000, 3, 49–56. [Google Scholar] [CrossRef]
- Kuske, S.; Schiereck, T.; Grobosch, S.; Paduch, A.; Droste, S.; Halbach, S.; Icks, A. Diabetes-related information-seeking behaviour: A systematic review. Syst. Rev. 2017, 6, 212. [Google Scholar] [CrossRef]
- Basnyat, I.; Nekmat, E.; Jiang, S.; Lin, J. Applying the Modified Comprehensive Model of Information Seeking to Online Health Information Seeking in the Context of India. J. Health Commun. 2018, 23, 563–572. [Google Scholar] [CrossRef] [PubMed]
- Chang, F.-C.; Chiu, C.-H.; Chen, P.-H.; Miao, N.-F.; Lee, C.-M.; Chiang, J.-T.; Pan, Y.-C. Relationship Between Parental and Adolescent eHealth Literacy and Online Health Information Seeking in Taiwan. Cyberpsychol. Behav. Soc. Netw. 2015, 18, 618–624. [Google Scholar] [CrossRef] [PubMed]
- Lagoe, C.; Atkin, D. Health anxiety in the digital age: An exploration of psychological determinants of online health information seeking. Comput. Hum. Behav. 2015, 52, 484–491. [Google Scholar] [CrossRef]
- McKinley, C.J.; Wright, P.J. Informational social support and online health information seeking: Examining the association between factors contributing to healthy eating behavior. Comput. Hum. Behav. 2014, 37, 107–116. [Google Scholar] [CrossRef]
- Oh, Y.S. Predictors of Self and Surrogate Online Health Information Seeking in Family Caregivers to Cancer Survivors. Soc. Work Health Care 2015, 54, 939–953. [Google Scholar] [CrossRef]
- Sun, Y.; Wang, N.; Guo, X.; Peng, Z. Understanding the Acceptance of Mobile Health. J. Electron. Commer. Res. 2013, 14, 183–200. [Google Scholar]
- Cao, W.; Zhang, X.; Xu, K.; Wang, Y. Modeling Online Health Information-Seeking Behavior in China: The Roles of Source Characteristics, Reward Assessment, and Internet Self-Efficacy. Health Commun. 2016, 31, 1105–1114. [Google Scholar] [CrossRef] [PubMed]
- Rains, S.A.; Tukachinsky, R. Information Seeking in Uncertainty Management Theory: Exposure to Information about Medical Uncertainty and Information-Processing Orientation as Predictors of Uncertainty Management Success. J. Health Commun. 2015, 20, 1275–1286. [Google Scholar] [CrossRef] [PubMed]
- Shaw, B.R.; DuBenske, L.L.; Han, J.Y.; Cofta-Woerpel, L.; Bush, N.; Gustafson, D.H.; McTavish, F. Antecedent characteristics of online cancer information seeking among rural breast cancer patients: An application of the Cognitive-Social Health Information Processing (C-SHIP) model. J. Health Commun. 2008, 13, 389–408. [Google Scholar] [CrossRef] [PubMed]
- Lin, W.Y.; Zhang, X.; Song, H.; Omori, K. Health information seeking in the Web 2.0 age: Trust in social media, uncertainty reduction, and self-disclosure. Comput. Hum. Behav. 2016, 56, 289–294. [Google Scholar] [CrossRef]
- Mou, J.; Shin, D.; Cohen, J. Health beliefs and the valence framework in health information seeking behaviors. Inf. Technol. People 2016, 29, 876–900. [Google Scholar] [CrossRef]
- Zhao, Y.; Ni, Q.; Zhou, R. What factors in fl uence the mobile health service adoption? A meta-analysis and the moderating role of age. Int. J. Inf. Manag. 2017, 43, 342–350. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J. Clin. Epidemiol. 2009, 151, 264–269. [Google Scholar]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017, 9, 358. [Google Scholar] [CrossRef] [PubMed]
- Wilhelmsen, N.C.; Eriksson, T. Medication adherence interventions and outcomes: An overview of systematic reviews. Eur. J. Hosp. Pharm. 2019, 26, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Lipsey, M.W.; Wilson, D.B. Practical Meta-Analysis; Sage Publications, Inc.: Thousand Oaks, CA, USA, 2001; ISBN 0761921680. [Google Scholar]
- Ahadzadeh, A.S.; Sharif, S.P.; Ong, F.S. Online health information seeking among women: The moderating role of health consciousness. Online Inf. Rev. 2018, 42, 58–72. [Google Scholar] [CrossRef]
- Kim, S.C.; Shah, D.V.; Namkoong, K.; Mctavish, F.M.; Gustafson, D.H. Predictors of Online Health Information Seeking Among Women with Breast Cancer: The Role of Social Support Perception and Emotional Well-Being. J. Comput. Commun. 2013, 18, 98–118. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.T.; Lin, J. A Self-Determination Perspective on Online Health Information Seeking: The Internet vs. Face-to-Face Office Visits with Physicians. J. Health Commun. 2016, 21, 714–722. [Google Scholar] [CrossRef] [PubMed]
- Li, Y. Impact of Impulsive Buying Behavior on Postimpulsive Buying Satisfaction. Soc. Behav. Personal. Int. J. 2015, 43, 339–351. [Google Scholar] [CrossRef]
- Li, Y.; Wang, X.; Lin, X.; Hajli, M. Seeking and sharing health information on social media: A net valence model and cross-cultural comparison. Technol. Forecast. Soc. Chang. 2018, 126, 28–40. [Google Scholar] [CrossRef]
- Miller, L.M.S.; Bell, R.A. Online health information seeking: The influence of age, information trustworthiness, and search challenges. J. Aging Health 2012, 24, 525–541. [Google Scholar] [CrossRef]
- Myrick, J.G. The role of emotions and social cognitive variables in online health information seeking processes and effects. Comput. Hum. Behav. 2017, 68, 422–433. [Google Scholar] [CrossRef]
- Oh, Y.S.; Song, N.K. Investigating relationships between health-related problems and online health information seeking. CIN Comput. Inform. Nurs. 2017, 35, 29–35. [Google Scholar] [CrossRef]
- Walsh, A.M.; Hamilton, K.; White, K.M.; Hyde, M.K. Use of online health information to manage children’s health care: A prospective study investigating parental decisions Healthcare needs and demand. BMC Health Serv. Res. 2015, 15, 1–10. [Google Scholar] [CrossRef]
- Guo, X.; Sun, Y.; Wang, N.; Peng, Z.; Yan, Z. The dark side of elderly acceptance of preventive mobile health services in China. Electron. Mark. 2013, 23, 49–61. [Google Scholar] [CrossRef]
- Deng, Z.; Liu, S. Understanding consumer health information-seeking behavior from the perspective of the risk perception attitude framework and social support in mobile social media websites. Int. J. Med. Inform. 2017, 105, 98–109. [Google Scholar] [CrossRef] [PubMed]
- Johnston, A.C.; Worrell, J.L.; Gangi, P.M.D.; Wasko, M. Online health communities: An assessment of the influence of participation on patient empowerment outcomes. Inf. Technol. People 2013, 26, 213–235. [Google Scholar] [CrossRef]
- Ruppel, E.K. Scanning Health Information Sources:Applying and Extending the Comprehensive Model of Information Seeking. J. Health Commun. 2015, 21, 208–216. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Guo, X.; Lai, K.; Guo, F.; Li, C. Understanding Gender Differences in m-Health Adoption: A Modified Theory of Reasoned Action Model. Telemed. E-Health 2014, 20, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Guo, X.; Guo, F.; Lai, K.H. Nonlinearities in personalization-privacy paradox in mHealth adoption: The mediating role of perceived usefulness and attitude. Technol. Health Care 2014, 22, 515–529. [Google Scholar] [PubMed]
- Hedges, L.V. Statistical Methology in Meta-Analysis; ERIC Publications: Princeton, NJ, USA, 1982; ISBN 978-0123363800. [Google Scholar]
- Pigott, T.D. Methods of meta-analysis: Correcting error and bias in research findings. Eval. Progr. Plan. 2006, 29, 236–237. [Google Scholar] [CrossRef]
- Rothstein, H.R.; Sutton, A.J.; Borenstein, M. Publication Bias in Meta-Analysis: Prevention, Assessment and Adjustments; Wiley: Hoboken, NJ, USA, 2006; ISBN 0470870141. [Google Scholar]
- Li, J.; Theng, Y.L.; Foo, S. Predictors of online health information seeking behavior: Changes between 2002 and 2012. J. Health Commun. 2016, 22, 804–814. [Google Scholar] [CrossRef]

| Publication | Impact Factor | Year of Publication | Country | Group | Sample Sizes |
|---|---|---|---|---|---|
| Ren [1] | 1.179 | 2019 | South Africa | Undergraduate | 282 |
| Ahadzade et al. [22] | 1.928 | 2016 | Malaysia | Malaysian females | 270 |
| Basnyat et al. [6] | 1.773 | 2018 | India | Population | 990 |
| Cao et al. [12] | 1.846 | 2016 | China | Population | 393 |
| Chang [7] | 2.65 | 2015 | China | Students | 3234 |
| Kim et al. [23] | 4.896 | 2013 | USA | Patients | 271 |
| Lagoe [8] | 4.306 | 2015 | USA | Adults | 245 |
| Lee & Lin [24] | 1.773 | 2016 | India | Population | 993 |
| Li [25] | 2.297 | 2015 | USA | Patients | 3014 |
| Li et al. [26] | 3.815 | 2018 | China | Undergraduate | 156 |
| Lin et al. [15] | 4.306 | 2016 | USA, South Korea, Hong Kong | College students | 789 |
| McKinley & Wright [9] | 4.306 | 2014 | USA | Undergraduate | 297 |
| Miller & Bell [27] | 2.007 | 2012 | USA | Adults | 3796 |
| Myrick [28] | 4.306 | 2017 | USA | Population | 375 |
| Oh [10] | 1.097 | 2015 | USA | Patients | 1113 |
| Oh & Song [29] | 1.029 | 2017 | Korea | Adults | 2351 |
| Walsh et al. [30] | 1.932 | 2015 | Australia | Parents | 391 |
| Xitong Guo et al. [31] | 3.553 | 2013 | China | Patients | 204 |
| Jaafar et al. [2] | 2.731 | 2017 | Malaysia | Patients | 271 |
| Deng [32] | 2.731 | 2017 | China | Patients or their family members | 436 |
| Johnston et al. [33] | 1.263 | 2013 | USA | Patients | 153 |
| Mou [16] | 1.263 | 2016 | South Africa | Undergraduate | 703 |
| Sun et al. [11] | 1.786 | 2013 | China | Patients | 204 |
| Rains & Tukachinsky [13] | 1.773 | 2015 | USA | Undergraduate students | 162 |
| Ruppel [34] | 1.773 | 2015 | USA | Patients | 3315 |
| Zhang et al. [35] | 0.787 | 2014 | China | Population | 491 |
| Zhang et al. [36] | 1.996 | 2014 | China | Population | 481 |
| Variable. | Fail-safe N | 5k + 10 | Fail-safe N/5k + 10 | p. Bias Risk | |
|---|---|---|---|---|---|
| Demographic Characteristics | Age | 1260.82 | 50 | 25.22 | low |
| Income | 198.24 | 40 | 4.96 | low | |
| Education | 986.19 | 50 | 19.72 | low | |
| Gender | 915.98 | 45 | 20.36 | low | |
| Cognitive Factors | Perceived usefulness | 938.17 | 40 | 23.45 | low |
| Perceived Ease of Use | 227.51 | 30 | 7.58 | low | |
| Perceived behavioral control | 91.55 | 25 | 3.66 | low | |
| Perceived risk | 683.32 | 35 | 19.52 | low | |
| Perceived benefit | 1212.52 | 45 | 26.94 | low | |
| Perceived cost | 58.25 | 25 | 2.33 | low | |
| Internal Factors | Self-efficacy | 642.37 | 55 | 11.68 | low |
| Attitude | 893.82 | 35 | 25.54 | low | |
| Internet experience | 4989.9 | 50 | 99.80 | low | |
| Health anxiety | 189.5 | 50 | 3.79 | low | |
| Trust | 884.1 | 45 | 19.65 | low | |
| External Factor | Social support | 132.78 | 25 | 5.31 | low |
| Subjective norm | 921.26 | 30 | 30.71 | low | |
| Variable | K | N | R | Heterogeneity Test | Tau-Squared | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Q | Df (Q) | p | I2 | τ2 | τ | Se | Var | |||||
| Demographic Characteristics | Age | 8 | 16,861 | −0.19 | 341.79 | 7 | 0.000 | 94.1 | 0.024 | 0.155 | 0.056 | 0.003 |
| Income | 6 | 14,498 | 0.13 | 51.01 | 5 | 0.000 | 95.6 | 0.006 | 0.077 | 0.034 | 0.001 | |
| Education | 8 | 18,084 | 0.19 | 158.12 | 7 | 0.000 | 95.6 | 0.012 | 0.110 | 0.041 | 0.002 | |
| Gender | 10 | 17,612 | −0.29 | 594.06 | 6 | 0.000 | 98.99 | 0.040 | 0.200 | 0.071 | 0.005 | |
| Cognitive Factors | Perceived usefulness | 6 | 1478 | 0.55 | 17.18 | 5 | 0.004 | 70.9 | 0.011 | 0.105 | 0.050 | 0.003 |
| Perceived ease of use | 4 | 1169 | 0.37 | 25.21 | 3 | 0.000 | 88.1 | 0.027 | 0.164 | 0.085 | 0.007 | |
| Perceived behavioral control | 3 | 986 | 0.31 | 15 | 2 | 0.001 | 86.7 | 0.019 | 0.138 | 0.086 | 0.007 | |
| Perceived risk | 6 | 2347 | −0.42 | 165.07 | 4 | 0.000 | 96.97 | 0.088 | 0.297 | 0.124 | 0.015 | |
| Perceived benefit | 7 | 5335 | 0.47 | 287.91 | 6 | 0.000 | 97.9 | 0.206 | 0.454 | 0.145 | 0.021 | |
| Perceived cost | 4 | 967 | −0.25 | 5.07 | 2 | 0.031 | 60.5 | 0.0052 | 0.072 | 0.058 | 0.003 | |
| Internal Factors | Self-efficacy | 9 | 2855 | 0.36 | 138.73 | 8 | 0.000 | 94.2 | 0.111 | 0.333 | 0.151 | 0.023 |
| Attitude | 5 | 1837 | 0.52 | 163.00 | 4 | 0.000 | 97.5 | 0.072 | 0.268 | 0.122 | 0.015 | |
| Internet experience | 8 | 15,791 | 0.35 | 2267.14 | 7 | 0.000 | 99.69 | 0.122 | 0.349 | 0.124 | 0.015 | |
| Health anxiety | 8 | 9083 | 0.19 | 105.11 | 7 | 0.000 | 93.3 | 0.149 | 0.386 | 0.055 | 0.003 | |
| Trust | 7 | 9747 | 0.37 | 756.65 | 6 | 0.000 | 99.2 | 0.072 | 0.268 | 0.103 | 0.011 | |
| External Factor | Social support | 3 | 1582 | 0.39 | 31.76 | 2 | 0.000 | 93.7 | 0.054 | 0.232 | 0.140 | 0.020 |
| Subjective norm | 4 | 1467 | 0.7 | 109.93 | 3 | 0.000 | 97.3 | 0.108 | 0.329 | 0.166 | 0.028 | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, J.; Xiu, G.; Shahzad, F. Exploring the Determinants of Online Health Information-Seeking Behavior Using a Meta-Analytic Approach. Sustainability 2019, 11, 4604. https://doi.org/10.3390/su11174604
Wang J, Xiu G, Shahzad F. Exploring the Determinants of Online Health Information-Seeking Behavior Using a Meta-Analytic Approach. Sustainability. 2019; 11(17):4604. https://doi.org/10.3390/su11174604
Chicago/Turabian StyleWang, Jian, Guoyi Xiu, and Fakhar Shahzad. 2019. "Exploring the Determinants of Online Health Information-Seeking Behavior Using a Meta-Analytic Approach" Sustainability 11, no. 17: 4604. https://doi.org/10.3390/su11174604
APA StyleWang, J., Xiu, G., & Shahzad, F. (2019). Exploring the Determinants of Online Health Information-Seeking Behavior Using a Meta-Analytic Approach. Sustainability, 11(17), 4604. https://doi.org/10.3390/su11174604






