Preventive Strategies for Upper Extremity Deep Venous Thrombosis Following Elective Upper Limb Surgery: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Literature Search
2.3. Data Extraction and Quality Assessment
3. Results
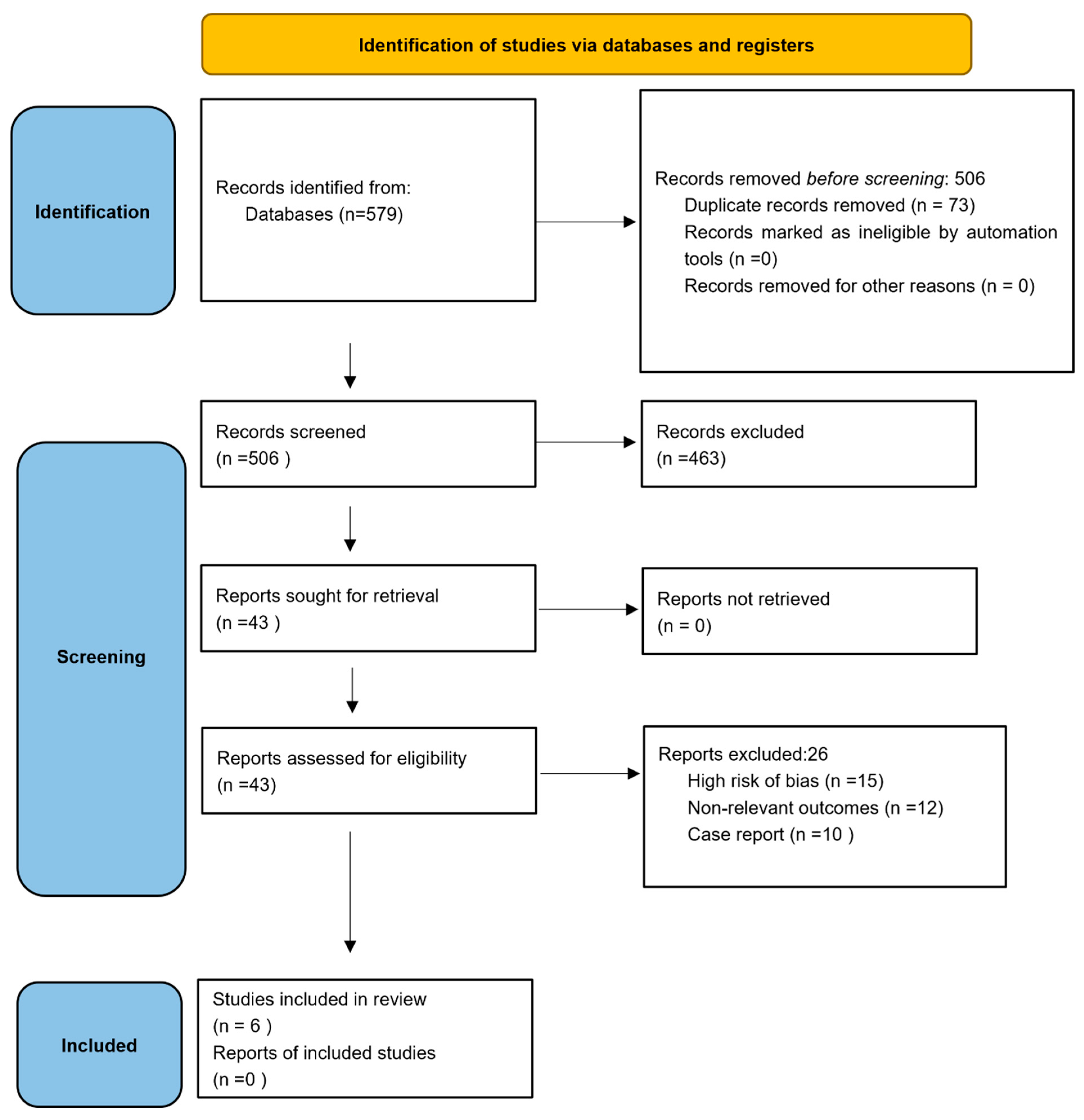
3.1. Study Selection
3.2. Study Characteristics
3.3. Preventive Strategies
3.4. DVT and Complications
3.5. Study Heterogeneities
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alyea, E.; Gaston, T.; Austin, L.S.; Wowkanech, C.; Cypel, B.; Pontes, M.; Williams, G. The Effectiveness of Aspirin for Venous Thromboembolism Prophylaxis for Patients Undergoing Arthroscopic Rotator Cuff Repair. Orthopedics 2019, 42, e187–e192. [Google Scholar] [CrossRef] [PubMed]
- Jameson, S.S.; James, P.; Howcroft, D.W.; Serrano-Pedraza, I.; Rangan, A.; Reed, M.R.; Candal-Couto, J. Venous thromboembolic events are rare after shoulder surgery: Analysis of a national database. J. Shoulder Elb. Surg. 2011, 20, 764–770. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, H.; Yamamoto, N.; Nagamoto, H.; Sano, H.; Tanaka, M.; Itoi, E. Venous thromboembolism after elective shoulder surgery: A prospective cohort study of 175 patients. J. Shoulder Elb. Surg. 2014, 23, 605–612. [Google Scholar] [CrossRef] [PubMed]
- Navarro, R.A.; Maria Burke, M.F.; Costouros, J.G.; Yian, E.H. Risk of Thromboembolism in Shoulder Arthroplasty: Effect of Implant Type and Traumatic Indication. Clin. Orthop. Relat. Res. 2013, 471, 1576–1581. [Google Scholar] [CrossRef] [PubMed]
- Turan, H.; Kahramanoglu, I.; Ay, M.; Tokgozoglu, N.; Sal, V.; Bese, T.; Demirkiran, F.; Arvas, M. Postoperative upper extremity deep vein thrombosis in a gynecologic oncology patient: A case report. Int. J. Surg. Case Rep. 2016, 29, 120–122. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 10, n71. Available online: https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-021-01626-4 (accessed on 12 July 2025). [CrossRef] [PubMed]
- Willis, A.A.; Warren, R.F.; Craig, E.V.; Adler, R.S.; Cordasco, F.A.; Lyman, S.; Fealy, S. Deep vein thrombosis after reconstructive shoulder arthroplasty: A prospective observational study. J. Shoulder Elb. Surg. 2009, 18, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Koch, O.; du Plessis, A.; Olorunju, S.; McLoughlin, H.; Le Roux, T. Incidence of deep vein thrombosis following shoulder replacement surgery: A prospective study. SA Orthop. J. 2017, 16, 33–39. [Google Scholar] [CrossRef]
- Delluc, A.; Wells, P.S. Low failure rate reported of diagnosis algorithm for suspected upper extremity deep vein thrombosis. Evid. Based Med. 2014, 19, 189. [Google Scholar] [CrossRef] [PubMed]
- Slim, K.; Nini, E.; Forestier, D.; Kwiatkowski, F.; Panis, Y.; Chipponi, J. Methodological index for non-randomized studies (minors): Development and validation of a new instrument. ANZ J. Surg. 2003, 73, 712–716. Available online: https://www.ncbi.nlm.nih.gov/pubmed/12956787 (accessed on 12 July 2025). [CrossRef] [PubMed]
- Alizadehasl, A.; Jebelli, S.F.H.; Forati, S.; Zonooz, Y.A.; Salehi, M.M.; Hakimian, H.; Aliabadi, R.Y.; Aliabadi, A.Y. The Role of Anticoagulation on Venous Thromboembolism Primary Prophylaxis in Low- to Intermediate-Risk Ambulatory Cancer Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Asian Pac. J. Cancer Prev. 2024, 25, 2237–2246. [Google Scholar] [CrossRef] [PubMed]
- Smith, T.O.; Daniell, H.; Hing, C. Upper extremity deep vein thrombosis in orthopaedic and trauma surgery: A systematic review. Eur. J. Orthop. Surg. Traumatol. 2011, 21, 79–85. [Google Scholar] [CrossRef]
- Sheth, H.; Remtulla, R.; Moradi Tuchayi, A.; Smith, R. Evaluation of Upper Extremity Deep Vein Thrombosis Risk Factors and Management. J. Cancer Sci. Clin. Ther. 2018, 2, 18–24. [Google Scholar] [CrossRef]
- Meizoso, J.P.; Proctor, K.G. Venous Thromboembolism After Trauma. In Trauma Induced Coagulopathy; Moore, H.B., Neal, M.D., Moore, E.E., Eds.; Springer International Publishing: Cham, Switzerland, 2021; pp. 515–533. [Google Scholar]
- Tran, A.; Lutsey, P.L.; Carrier, M. Minor trauma and venous thromboembolism: The threshold for antithrombotic prophylaxis. Haematologica 2024, 109, 3860–3867. [Google Scholar] [CrossRef] [PubMed]
- Badr, S. Upper Extremity Deep Venous Thrombosis (UEDVT). Intern. Med. 2015, 5, 6. [Google Scholar] [CrossRef]
- Panamsky, L.; Gomes, S.; McAuley, E.; Hopman, W.; Marosi, K.; Srivastava, S. Thromboprophylaxis Following Hip and Knee Surgery: A Review of Current Practices in a Canadian Tertiary Care Center. Can. J. Gen. Intern. Med. 2022, 17, 33–40. [Google Scholar] [CrossRef]
- Sobieraj, D.M.; Coleman, C.I.; Tongbram, V.; Lee, S.; Colby, J.; Chen, W.T.; Makanji, S.S.; Ashaye, A.; Kluger, J.; White, C.M. Venous Thromboembolism Prophylaxis in Orthopedic Surgery [Internet]; Report No.: 12-EHC020-EF; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2012. [PubMed]
- Cowan, S.; Ghayyad, K.; Conlon, M.J.; Naik, M.; Zeini, I.; Hawks, M.; Ahmed, A.; Kachooei, A.R. Trends in the Epidemiology of Deep Vein Thrombosis and Pulmonary Embolism in Patients Undergoing Surgery. Cureus 2024, 16, e74925. [Google Scholar] [CrossRef] [PubMed]
- Tsai, J.; Grant, A.M.; Beckman, M.G.; Grosse, S.D.; Yusuf, H.R.; Richardson, L.C. Determinants of Venous Thromboembolism among Hospitalizations of US Adults: A Multilevel Analysis. PLoS ONE 2015, 10, e0123842. [Google Scholar] [CrossRef] [PubMed]
- Urbankova, J.; Quiroz, R.; Goldhaber, S.Z. Intermittent pneumatic compression and deep vein thrombosis prevention in postoperative patients. Phlebology 2006, 21 (Suppl. 1), 19–22. [Google Scholar] [CrossRef]
- Langridge, B.J.; Goodall, R.J.; Onida, S.; Shalhoub, J.; Davies, A.H. Venous thromboembolism prevention in lower limb trauma–Can we do better? Phlebology 2019, 34, 291–293. [Google Scholar] [CrossRef] [PubMed]
| Complications Related to Preventive Strategies | Complications Related to Upper Extremities DVT | Complications Related to Lower Extremities DVT | Statistical Methods Used | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group 1 | Total | Group 2 | Total | Group 1 | Total | Group 2 | Total | Group 1 | Total | Group 2 | Total | Authors | |
| NM | NM | NM | NM | 14 (PE) no mention to the site of origin | NM | NM | NM | NM | NM | NM | NM | not specifically mentioned | Navarro [4] |
| NM | NM | NM | NM | 1 (PE) | 1 | NM | NM | NM | NM | NM | NM | X2 analysis or the Fisher exact test | Takahashi [3] |
| not specifically mentioned | NM | NM | NM | not specifically mentioned | NM | NM | NM | not specifically mentioned | NM | NM | NM | not specifically mentioned | Jameson [2] |
| Bleeding events, peptic ulceration, and gastric irritation, dyspepsia, hematoma | NM | NM | NM | 1 (PE) | NM | 0 (PE) | NM | 1 (PE) | NM | 0 (PE) | NM | SAS 9.4 Platform, (IBM) Wilson methods, Newcombe method, Firth method | Alyea [1] |
| NM | NM | NM | NM | NM | NM | NM | NM | NM | NM | NM | NM | NM | Koch [8] |
| NM | NM) | NM | NM | 1 (fatal PE), 2 (non-fatal PE) | 3 | NM | NM | NM | NM | NM | NM | SPSS (version 31) computer software | Willis [7] |
| Laterality | VTE Risk Factors | VTE Risk Factors | Operative Procedure | |||||
|---|---|---|---|---|---|---|---|---|
| Right | Left | Group 1 | Total | Group 2 | Total | Group 1 | Group 2 | Authors |
| 1474 | 1100 | NM | NM | NM | RSAs, TSAs, HAs | NM | Navarro [4] | |
| NM | NM | (non-DVT group): mean age 60 ± 14, male: female ratio 2.4:1, mean BMI 24.3 ± 3.3, mean operative time 135 min, with smoking habit 45%, with DVT risk-related comorbidity 63% | 165 | (DVTgroup): mean age 66 ± 7, male: female ratio 4:1, mean BMI: 24.3 ± 3.8, mean operative time 139 min, with smoking habit 70%, with DVT risk-related comorbidity (HTN, DM, prostate cancer) 80%. | 10 | ARCR, A-patch, ABR, other | NM | Takahashi [3] |
| NM | NM | those aged over 60 years, obese, Surgical procedure (those undergoing operations where the total combined anesthetic and surgical time is greater than 90 min), Patient comorbidities | NM | NM | NM | Total Shoulder Replacement, Arthroscopy, Proximal Humeral Fracture Surgery | NM | Jameson [2] |
| 564 | 350 | old age, revision surgery, smoking and cancer history, history of PE and high cholesterol and blood pressure inherited and acquired hypercoagulable states. | NM | old age, revision surgery, smoking and cancer history, history of PE and high cholesterol and blood pressure inherited and acquired hypercoagulable states. | NM | PCR | PCR | Alyea [1] |
| NM | NM | the patients with a BMI of >50 kg/m2 have three times higher risk of VTE than the non-obese. | NM | NM | NM | compression and Doppler ultrasound | NM | Willis [7] |
| NM | NM | Age has been shown to be significant risk factor for VTE disease. | NM | NM | NM | standard deltopectoral approach | NM | Koch [8] |
| Preventive Strategies (Pharmacological) | Preventive Strategies (Mechanical Prophylaxis) | ||||
|---|---|---|---|---|---|
| Dosage | Timing of Administration | Mode of Delivery | Dosage | Timing of Administration | |
| no preventive strategies were mentioned. | NM | NM | NM | NM | Navarro [4] |
| pneumatic compression devices | During surgery | NM | elastic stocking | During surgery | Takahashi [3] |
| chemical thromboprophyl axis (LMWH prophylaxis) | NM | NM | not specifically discussed | NM | Jaameson [2] |
| 81 mg/d aspirin for 4 weeks | postoperatively | NM | compression boots and early mobilization | postoperatively | Alyea [1] |
| thromboprophyl axis (LMWH prophylaxis) | NM | NM | NM | NM | Koch [8] |
| Postoperative thromboprophyl axis with pharmacologic agents is widely advocated to improve survival rates and reduce health care costs | NM | NM | NM | NM | Willis [7] |
| Confidence Intervals | The Study’s Main Findings | Authors |
|---|---|---|
| 95% | No statistically significant associations between procedure type or surgery indication and odds of PE, DVT, VTE, or 90-day mortality were observed. incidence of symptomatic DVT 0.51% and 0.54% for symptomatic PE for all patients with primary shoulder arthroplasties. | Navarro [4] |
| 95% | incidence of asymptomatic DVT after surgery: 5.7%. symptomatic PE: 0%. DVT occurred at 1 or 2 days post-op | Takahashi [3] |
| 95% | Low incidence of symptomatic VTE (0.41%). Risk factors included age > 70 years, traumatic indication. VTE led to prolonged hospital stay and readmission | Jaameson [2] |
| 95% | VTE) after shoulder surgery are relatively rare. The implementation of national thromboprophylaxis guidelines did not significantly impact the rates of VTE after shoulder surgery | Alyea [1] |
| 95% | In a study involving 57 participants who underwent various types of shoulder replacements, the incidence of deep vein thrombosis (DVT) was found to be 12.3% (7 out of 57) with a confidence interval of 95% [5.1, 23.7]. Two DVTs were observed in the upper limb, while two others occurred in the lower leg. All DVTs were reported to be of acute onset, with two causing partial vein obstruction. The cardiology department managed the treatment, and symptomatic DVTs were observed in one patient with axillary vein DVT and one with brachial vein DVT. Four participants were already on thromboprophylaxis at the time of diagnosis. No fatalities were reported. There was no significant association between smoking and DVT risk. Females with reverse shoulder replacements had longer post-operative stays. The average Caprini score was 5.8, with higher scores in individuals with positive duplex Doppler, females with DVT, and males having lower scores. Among participants with shoulder replacements due to trauma, one had a DVT despite receiving thromboprophylaxis. The average BMI was 32.1, and the mean age was 62.6 years. The duration of surgery did not differ significantly between participants with and without DVT. One participant had a previous DVT history and developed a symptomatic axillary vein DVT post-surgery. | Koch [8] |
| 95% | In this study on shoulder arthroplasty, the prevalence of deep vein thrombosis (DVT) was found to be 13%. Surveillance Doppler ultrasound conducted on the second postoperative day detected 10 DVTs (prevalence of 10%) in 9 patients, and an additional 3 new DVTs (incidence of 6%) were documented in 3 patients 12 weeks after surgery. DVTs were observed in both the upper and lower extremities during the acute and subacute postoperative periods. Upper extremity DVTs were exclusively found in the operative extremity, with involvement of the axillary and brachial veins. Lower extremity DVTs included ipsilateral and contralateral cases, involving the popliteal, posterior tibial, and peroneal veins. Three patients experienced pulmonary embolism, with 2 cases confirmed by spiral CT scan. One patient died due to cardiovascular collapse from a massive pulmonary embolism. The prevalence of DVT in this study was significantly higher than that in the general population and age-matched control subjects, but not significantly different from the prevalence after hip replacement surgery. However, the prevalence was significantly lower than that after knee replacement surgery. | Willis [7] |
| Willis et al. (2009) [7] | Takahashi et al. (2014) [3] | Navarro et al. (2013) [4] | Koch et al. (2017) [8] | Jameson et al. (2011) [2] | Alyea et al. (2019) [1] | |
|---|---|---|---|---|---|---|
| 2 | 2 | 2 | 2 | 2 | 2 | A clearly stated aim |
| 1 | 2 | 2 | 2 | 2 | 2 | Inclusion of consecutive patients |
| 0 | 2 | 2 | 2 | 2 | 1 | Prospective collection of data |
| 1 | 0 | 2 | 2 | 1 | 2 | Endpoints appropriate to the aim of the study |
| 0 | 0 | 0 | 0 | 0 | 0 | Unbiased assessment of the study endpoint |
| 1 | 2 | 1 | 0 | 1 | 2 | Follow-up period appropriate to the aim of the study |
| 0 | 0 | 2 | 1 | 0 | 0 | Loss to follow-up less than 5% |
| 0 | 2 | 2 | 2 | 2 | 2 | Prospective calculation of the study size |
| Additional criteria in the case of comparative study: | ||||||
| 1 | 1 | 0 | - | - | 2 | An adequate control group |
| 0 | 2 | 0 | - | - | 2 | Contemporary groups |
| 1 | 2 | 2 | - | - | 2 | Baseline equivalence of groups |
| 2 | 2 | 2 | - | - | 2 | Adequate statistical analyses |
| 9/24 | 17/24 | 17/24 | 11/16 | 10/16 | 19/24 | Total (out of 16 or 24) |
 High quality,
High quality,  Moderate quality,
Moderate quality,  poor quality.
poor quality.| Limitations | Recommendations for Future Research | Authors |
|---|---|---|
| Not all patients underwent screening (with ultrasound, venography, or CT) either before or after the surgery. describing only the symptomatic cases of VTE. unable to evaluate the associations of many risk factors and incidence of VTE. the incidence of DVT is probably higher than reported. it still may be underpowered to detect the 0.9% observed difference in VTE and mortality rates between elective and traumatic arthroplasties. | The data in this study may be considered hypothesis-generating and useful for sample-size calculations in future prospective studies regarding routine VTE prophylaxis in the shoulder arthroplasty population. | Navarro [4] |
| lateral decubitus position was not included, DVT prophylaxis was not controlled, US was performed in only 85 patients at 3 weeks to 3 months after surgery. ultrasound examination for patients who had total knee arthroplasty was performed at 3 days after surgery or later. ex post analysis of the statistical power for DVT were lower than 0.4. | prospective studies including greater numbers of patients are needed to determine the risk factors | Takahashi [3] |
| not all patients underwent screening (with ultrasound, venography, or CT) either before or after the surgery. describing only the symptomatic cases of VTE. unable to evaluate the associations of many risk factors and incidence of VTE. the incidence of DVT is probably higher than we reported. it still may be underpowered to detect the 0.9% observed difference in VTE and mortality rates between elective and traumatic arthroplasties. | the data in this study may be considered hypothesis-generating and useful for sample-size calculations in future prospective studies regarding routine VTE prophylaxis in the shoulder arthroplasty population. | Jaameson [2] |
| selection bias and lack of randomization. Small sample size: The study included 914 patients, with 430 in the aspirin group and 484 in the control group. Low event rate: The overall incidence of VTE events was very low, with only 7 events (6 DVTs and 1 PE) occurring during the study period. This low event rate makes it difficult to draw definitive conclusions about the effectiveness of aspirin in preventing VTE. Lack of standardization: The study did not report on the specific criteria or protocols used for VTE screening and diagnosis. This could have led to variability in the detection and reporting of VTE events. Limited generalizability: The study was conducted at a single institution, which may limit the generalizability of the findings to other populations or settings. Outdated data: The study included patients treated between 2010 and 2015, which may not reflect the current standard of care or the use of newer VTE prophylaxis strategies. | A larger sample size would have increased the statistical power to detect any meaningful differences between the groups. Conduct a prospective, randomized controlled trial would provide more robust evidence on the effectiveness of aspirin for VTE prevention in patients undergoing arthroscopic rotator cuff repair. Standardize VTE screening and diagnosis: Establish clear, standardized protocols for the assessment and diagnosis of VTE events. Assess long-term outcomes | Alyea [1] |
| Small sample size (57 participants), Conducted at a single institution, Potential selection bias in participant inclusion, Lack of a control group for comparison, Insufficient information on statistical methods used, Follow-up duration not specified. | Conduct studies with larger sample sizes to enhance statistical power and generalizability. Include multiple healthcare institutions to capture diverse patient populations and account for variations in surgical techniques and postoperative care. Design randomized controlled trials with control groups to compare DVT incidence against baseline rates. Provide detailed reporting of statistical methods used in the analysis. Conduct studies with long-term follow-up to assess the incidence of DVT and potential complications over time. Investigate risk factors associated with DVT after shoulder replacement surgery to identify high-risk subgroups. Evaluate the effectiveness of thromboprophylaxis measures in reducing DVT incidence. | Koch [8] |
| The study presented several limitations that should be considered when interpreting the findings. Firstly, the sample size was small, which may limit the statistical power and generalizability of the results. Secondly, the study was conducted at a single center, further reducing the generalizability to other settings. Thirdly, the study employed an observational design, which prevents the establishment of causal relationships between variables. Fourthly, certain patient groups were excluded from the study, introducing potential selection bias and limiting the applicability of the findings to a broader population. Finally, the relatively short follow-up period of 12 weeks may have missed the detection of long-term deep vein thrombosis (DVT) cases, potentially underestimating the true incidence and impact of DVT in the studied population. | Increase sample size to improve statistical power and generalizability. Conduct multicenter studies to minimize biases and enhance population diversity. Perform comparative studies with other joint arthroplasties (hip, knee) to assess DVT prevalence. Design prospective controlled trials to evaluate preventive interventions or treatment strategies. Extend follow-up period to capture long-term DVT cases and assess outcomes. Conduct comprehensive risk factor analysis for DVT in shoulder arthroplasty patients. Evaluate effectiveness of preventive measures (pharmacological, mechanical) for reducing DVT incidence. Include patient-reported outcomes and functional assessments in evaluations. | Willis [7] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alsharidah, A.S.; Aljubran, A.A.; Alkharisi, M.; Alnafie, T.; Almuteri, D.; Almarhabi, Z.; Alawami, N.; Alkulaib, S.; Aljarash, H.; Abdullah, Z.; et al. Preventive Strategies for Upper Extremity Deep Venous Thrombosis Following Elective Upper Limb Surgery: A Systematic Review. Clin. Pract. 2025, 15, 221. https://doi.org/10.3390/clinpract15120221
Alsharidah AS, Aljubran AA, Alkharisi M, Alnafie T, Almuteri D, Almarhabi Z, Alawami N, Alkulaib S, Aljarash H, Abdullah Z, et al. Preventive Strategies for Upper Extremity Deep Venous Thrombosis Following Elective Upper Limb Surgery: A Systematic Review. Clinics and Practice. 2025; 15(12):221. https://doi.org/10.3390/clinpract15120221
Chicago/Turabian StyleAlsharidah, Aeshah Salem, Alya Ali Aljubran, Maha Alkharisi, Taif Alnafie, Dhai Almuteri, Zahra Almarhabi, Noor Alawami, Shaykhah Alkulaib, Hashmiah Aljarash, Zain Abdullah, and et al. 2025. "Preventive Strategies for Upper Extremity Deep Venous Thrombosis Following Elective Upper Limb Surgery: A Systematic Review" Clinics and Practice 15, no. 12: 221. https://doi.org/10.3390/clinpract15120221
APA StyleAlsharidah, A. S., Aljubran, A. A., Alkharisi, M., Alnafie, T., Almuteri, D., Almarhabi, Z., Alawami, N., Alkulaib, S., Aljarash, H., Abdullah, Z., & Almaqhawi, A. (2025). Preventive Strategies for Upper Extremity Deep Venous Thrombosis Following Elective Upper Limb Surgery: A Systematic Review. Clinics and Practice, 15(12), 221. https://doi.org/10.3390/clinpract15120221







