Treating Temporomandibular Disorders Through Orthodontics: A Scoping Review of Evidence, Gaps, and Clinical Guidance
Abstract
1. Introduction
2. Methods
2.1. Protocol Reporting
2.2. Eligibility Criteria
2.3. Information Sources and Search Strategy
2.4. Selection Process
2.5. Data Collection Process
2.6. Critical Appraisal (Risk of Bias)
2.7. Synthesis Methods
2.8. Ethics and Funding
3. Results
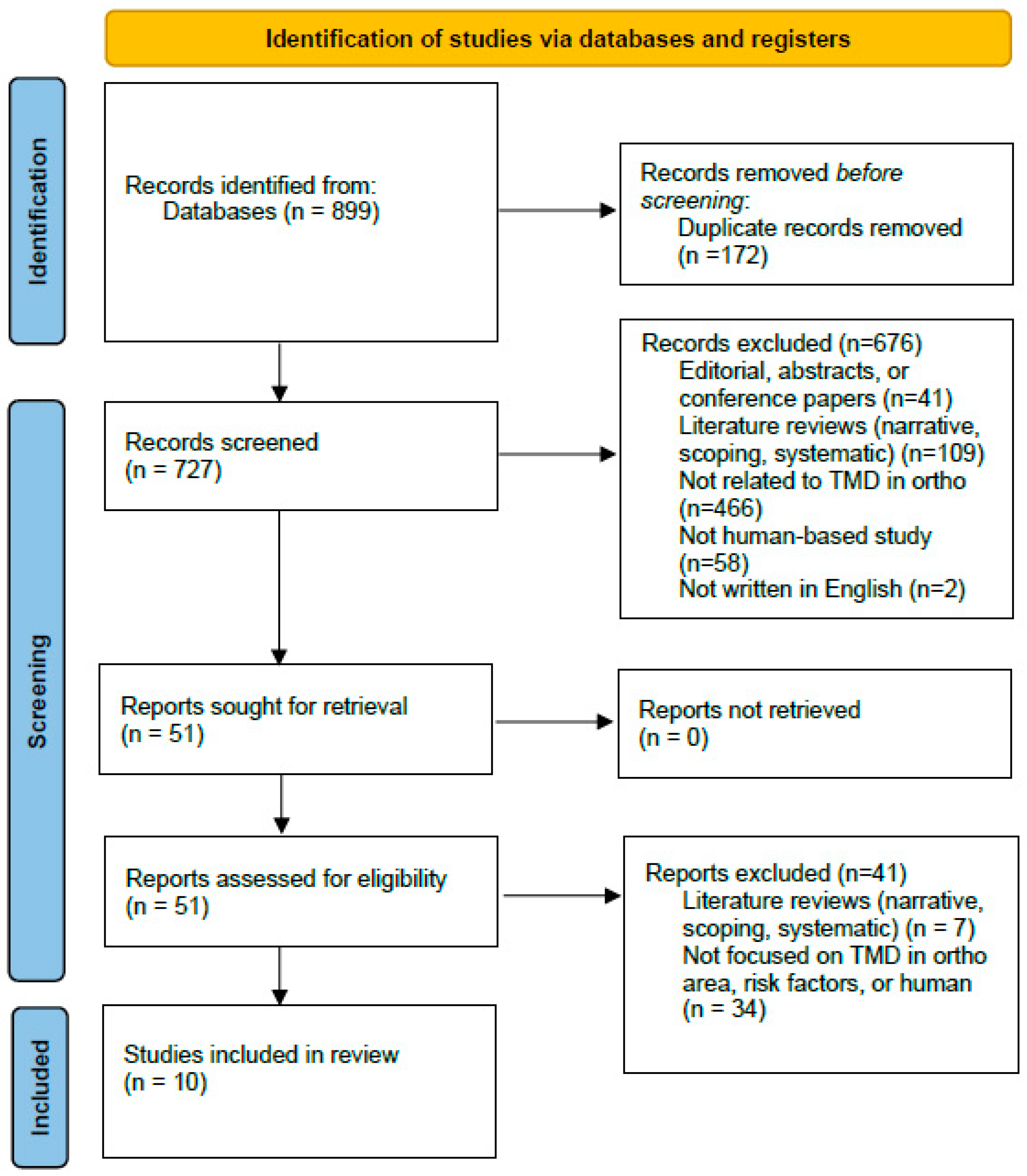
3.1. Article Selection
3.2. Study Characteristics
3.3. Orthodontic-TMD Relationship Findings
4. Discussion
4.1. Principle Findings and Context
4.2. Non-Surgical Orthodontic Interventions
4.3. Surgical Orthodontic Interventions
4.4. Outcomes by Domain (Pain, Function, Joint Sounds, PROs)
4.5. Diagnostics and Applicability
4.6. Risk of Bias, Heterogeneity, and Durability
4.7. Limitations and the Evidence of This Review
4.8. Implications for Practice
4.9. Future Research
4.10. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- National Institute of Dental and Craniofacial Research. TMD (Temporomandibular Disorders). Available online: https://www.nidcr.nih.gov/health-info/tmd# (accessed on 27 May 2025).
- Kitsoulis, P.; Marini, A.; Iliou, K.; Galani, V.; Zimpis, A.; Kanavaros, P.; Paraskevas, G. Signs and symptoms of temporomandibular joint disorders related to the degree of mouth opening and hearing loss. BMC Ear Nose Throat Disord. 2011, 11, 5. [Google Scholar] [CrossRef] [PubMed]
- Yadav, U.; Ahmed, J.; Ongole, R.; Shenoy, N.; Sujir, N.; Natarajan, S. Influence of Psychosocial Factors and Parafunctional Habits in Temporomandibular Disorders: A Cross-Sectional Study. Perm. J. 2020, 24, 19.144. [Google Scholar] [CrossRef]
- Ferreira, C.L.P.; da Silva, M.A.M.R.; de Felício, C.M. Signs and symptoms of temporomandibular disorders in women and men. Codas 2016, 28, 17–21. [Google Scholar] [CrossRef]
- Minervini, G.; Franco, R.; Marrapodi, M.M.; Fiorillo, L.; Cervino, G.; Cicciù, M. Prevalence of temporomandibular disorders in children and adolescents evaluated with Diagnostic Criteria for Temporomandibular Disorders: A systematic review with meta-analysis. J. Oral Rehabil. 2023, 50, 522–530. [Google Scholar] [CrossRef] [PubMed]
- Alrizqi, A.H.; Aleissa, B.M. Prevalence of Temporomandibular Disorders Between 2015–2021: A Literature Review. Cureus 2023, 15, e37028. [Google Scholar] [CrossRef] [PubMed]
- Chisnoiu, A.M.; Picos, A.M.; Popa, S.; Chisnoiu, P.D.; Lascu, L.; Picos, A.; Chisnoiu, R. Factors involved in the etiology of temporomandibular disorders—A literature review. Clujul Med. 2015, 88, 473–478. [Google Scholar] [CrossRef]
- Lai, Y.C.; Yap, A.U.; Türp, J.C. Prevalence of temporomandibular disorders in patients seeking orthodontic treatment: A systematic review. J. Oral Rehabil. 2020, 47, 270–280. [Google Scholar] [CrossRef]
- de Godoi Gonçalves, D.A.; Dal Fabbro, A.L.; Campos, J.A.D.B.; Bigal, M.E.; Speciali, J.G. Symptoms of temporomandibular disorders in the population: An epidemiological study. J. Orofac. Pain 2010, 24, 270–278. [Google Scholar]
- Ferendiuk, E.; Zajdel, K.; Pihut, M. Incidence of otolaryngological symptoms in patients with temporomandibular joint dysfunctions. Biomed. Res. Int. 2014, 2014, 824684. [Google Scholar] [CrossRef][Green Version]
- Ohrbach, R.; Sharma, S. Temporomandibular disorders: Definition and etiology. Semin. Orthod. 2024, 30, 237–242. [Google Scholar] [CrossRef]
- Celić, R.; Jerolimov, V.; Pandurić, J. A study of the influence of occlusal factors and parafunctional habits on the prevalence of signs and symptoms of TMD. Int. J. Prosthodont. 2002, 15, 43–48. [Google Scholar]
- Kapos, F.P.; Exposto, F.G.; Oyarzo, J.F.; Durham, J. Temporomandibular disorders: A review of current concepts in aetiology, diagnosis and management. Oral Surg. 2020, 13, 321–334. [Google Scholar] [CrossRef]
- Sharma, S.; Wactawski-Wende, J.; LaMonte, M.J.; Zhao, J.; Slade, G.D.; Bair, E.; Greenspan, J.D.; Fillingim, R.B.; Maixner, W.; Ohrbach, R. Incident injury is strongly associated with subsequent incident temporomandibular disorder: Results from the OPPERA study. Pain 2019, 160, 1551–1561. [Google Scholar] [CrossRef]
- Bair, E.; Ohrbach, R.; Fillingim, R.B.; Greenspan, J.D.; Dubner, R.; Diatchenko, L.; Helgeson, E.; Knott, C.; Maixner, W.; Slade, G.D. Multivariable modeling of phenotypic risk factors for first-onset TMD: The OPPERA prospective cohort study. J. Pain 2013, 14, T102–T115. [Google Scholar] [CrossRef]
- Yap, A.U.; Chen, C.; Wong, H.C.; Yow, M.; Tan, E. Temporomandibular disorders in prospective orthodontic patients. Angle Orthod. 2021, 91, 377–383. [Google Scholar] [CrossRef]
- Shalish, M.; Leibovich, A.; Zakuto, A.; Slutzky, H.; Chaushu, S.; Almoznino, G. The association between orthodontic treatment and temporomandibular disorders diagnosis and disease characteristics. J. Oral Rehabil. 2024, 51, 487–499. [Google Scholar] [CrossRef]
- Pollack, B. Cases of note: Michigan jury awards $850,000 in ortho case: A tempest in a teapot. J. Mich. Dent. Assoc. 1988, 70, 540–542. [Google Scholar] [PubMed]
- Coronel-Zubiate, F.-T.; Marroquín-Soto, C.; Geraldo-Campos, L.-A.; Aguirre-Ipenza, R.; Urbano-Rosales, L.-M.; Luján-Valencia, S.-A.; Tozo-Burgos, J.-G.; Arbildo-Vega, H.-I. Association between orthodontic treatment and the occurrence of temporomandibular disorders: A systematic review and meta-analysis. J. Clin. Exp. Dent. 2022, 14, e1032–e1043. [Google Scholar] [CrossRef] [PubMed]
- Khursheed Alam, M.; Abutayyem, H.; Alzabni, K.M.D.; Almuhyi, N.H.S.; Alsabilah, K.A.S.; Alkubaydan, F.S.T.; Alswairki, H.J.; Hajeer, M.Y.; Awawdeh, M.A. The Impact of Temporomandibular Disorders on Orthodontic Management: A Systematic Review and Meta-Analysis. Cureus 2023, 15, e44243. [Google Scholar] [CrossRef] [PubMed]
- Conti, A.; Freitas, M.; Conti, P.; Henriques, J.; Janson, G. Relationship between signs and symptoms of temporomandibular disorders and orthodontic treatment: A cross-sectional study. Angle Orthod. 2003, 73, 411–417. [Google Scholar] [CrossRef]
- Michelotti, A.; Rongo, R.; D’Antò, V.; Bucci, R. Occlusion, orthodontics, and temporomandibular disorders: Cutting edge of the current evidence. J. World Fed. Orthod. 2020, 9, S15–S18. [Google Scholar] [CrossRef] [PubMed]
- Kandasamy, S.; Greene, C.S. The evolution of temporomandibular disorders: A shift from experience to evidence. J. Oral Pathol. Med. 2020, 49, 461–469. [Google Scholar] [CrossRef] [PubMed]
- Lockerman, L.Z. Disclosure orthodontic and TMD—New study. Evid. Based Dent. 2024, 25, 73–74. [Google Scholar] [CrossRef]
- Ruf, S.; Bock, N.C. Long-term (≥15 years) effects of Class II treatment: A longitudinal and cross-sectional study on signs and symptoms of temporomandibular disorders. Eur. J. Orthod. 2019, 41, 172–179. [Google Scholar] [CrossRef] [PubMed]
- Pancherz, H.; Salé, H.; Bjerklin, K. Signs and symptoms of TMJ disorders in adults after adolescent Herbst therapy: A 6-year and 32-year radiographic and clinical follow-up study. Angle Orthod. 2015, 85, 735–742. [Google Scholar] [CrossRef]
- Huang, X.; Cen, X.; Liu, J. Effect of protraction facemask on the temporomandibular joint: A systematic review. BMC Oral Health 2018, 18, 38. [Google Scholar] [CrossRef]
- Macfarlane, T.V.; Kenealy, P.; Kingdon, H.A.; Mohlin, B.O.; Pilley, J.R.; Richmond, S.; Shaw, W.C. Twenty-year cohort study of health gain from orthodontic treatment: Temporomandibular disorders. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 692.e1–692.e8. [Google Scholar] [CrossRef]
- Abrahamsson, C.; Henrikson, T.; Nilner, M.; Sunzel, B.; Bondemark, L.; Ekberg, E.C. TMD before and after correction of dentofacial deformities by orthodontic and orthognathic treatment. Int. J. Oral Maxillofac. Surg. 2013, 42, 752–758. [Google Scholar] [CrossRef]
- Al-Groosh, D.H.; Abid, M.; Saleh, A.K. The relationship between orthodontic treatment and temporomandibular disorders: A dental specialists’ perspective. Dent. Press J. Orthod. 2022, 27, e2220406. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Kaku, M.; Yamamoto, T.; Yashima, Y.; Izumino, J.; Kagawa, H.; Ikeda, K.; Tanimoto, K. Correction of skeletal class II severe open bite with temporomandibular joint disorder treated by miniscrew anchorage and molar extraction: A case report. J. Med. Case Rep. 2019, 13, 207. [Google Scholar] [CrossRef]
- Kato, C.; Ono, T. Anterior open bite due to temporomandibular joint osteoarthrosis with muscle dysfunction treated with temporary anchorage devices. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 848–859. [Google Scholar] [CrossRef] [PubMed]
- Lee, G.H.; Park, J.H.; Lee, S.M.; Moon, D.N. Orthodontic Treatment Protocols for Patients with Idiopathic Condylar Resorption. J. Clin. Pediatr. Dent. 2019, 43, 292–303. [Google Scholar] [CrossRef] [PubMed]
- Zibo, H.N.; Baburin, A.; Tamme, T.; Voog-Oras, Ü. Short-term postoperative changes in temporomandibular joints and masticatory muscles of Angle class II patients after mandibular advancement surgery: Clinical findings. Stomatologija 2022, 24, 71–79. [Google Scholar]
- Giray, B.; Sadry, S. Modifications in Class I and Class II Div. 1 malocclusion during orthodontic treatment and their association with TMD problems. Cranio 2021, 39, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Hoshi, K.; Deguchi, T.; Goto, M.; Chida, T.; Takeshita, N.; Takahashi, I.; Takano-Yamamoto, T. Stomatognathic functional improvement in a patient with a canted occlusal plane and temporomandibular disorder treated with an edgewise appliance and miniscrews. Am. J. Orthod. Dentofac. Orthop. 2022, 161, 140–157. [Google Scholar] [CrossRef]
- Kau, C.H.; Almakky, O.; Louis, P.J. Team approach in the management of revision surgery to correct bilateral temporomandibular joint replacements. J. Orthod. 2020, 47, 156–162. [Google Scholar] [CrossRef]
- Myllymäki, E.; Heikinheimo, K.; Suominen, A.; Evälahti, M.; Michelotti, A.; Svedström-Oristo, A.-L.; Rice, D.P. Longitudinal trends in temporomandibular joint disorder symptoms, the impact of malocclusion and orthodontic treatment: A 20-year prospective study. J. Oral Rehabil. 2023, 50, 739–745. [Google Scholar] [CrossRef]
- Paunonen, J.; Helminen, M.; Sipilä, K.; Peltomäki, T. Temporomandibular disorders in Class II malocclusion patients after surgical mandibular advancement treatment as compared to non-treated patients. J. Oral Rehabil. 2019, 46, 605–610. [Google Scholar] [CrossRef]
- Baxi, S.; Bhatia, V.; Tripathi, A.; Dubey, M.P.; Kumar, P.; Mapare, S. Temporary Anchorage Devices. Cureus 2023, 15, e44514. [Google Scholar] [CrossRef]
- Anderson, G.C.; Gonzalez, Y.M.; Ohrbach, R.; Truelove, E.L.; Sommers, E.; Look, J.O.; Schiffman, E.L. Research Diagnostic Criteria for Temporomandibular Disorders: Future Directions. J. Orofac. Pain 2010, 24, 79–88. [Google Scholar]
- Michelotti, A.; Iodice, G. The role of orthodontics in temporomandibular disorders. J. Oral Rehabil. 2010, 37, 411–429. [Google Scholar] [CrossRef]
- Mohlin, B.; Axelsson, S.; Paulin, G.; Pietilä, T.; Bondemark, L.; Brattström, V.; Hansen, K.; Holm, A.-K. TMD in relation to malocclusion and orthodontic treatment. Angle Orthod. 2007, 77, 542–548. [Google Scholar] [CrossRef] [PubMed]
- Lopatiene, K.; Dumbravaite, A. Risk factors of root resorption after orthodontic treatment. Stomatologija 2008, 10, 89–95. [Google Scholar] [PubMed]
- Dimitroulis, G. Management of temporomandibular joint disorders: A surgeon’s perspective. Aust. Dent. J. 2018, 63, S79–S90. [Google Scholar] [CrossRef] [PubMed]
- Zong, C.; Dessel, J.V.; Velde, G.V.; Willems, G.; de Llano-Pérula, M.C. Dynamic changes in tooth displacement and bone morphometry induced by orthodontic force. Sci. Rep. 2022, 12, 13672. [Google Scholar] [CrossRef]
| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
| Author (Year) | Types of TMD | Study Design | Diagnostic Method(s) | Key Outcome |
|---|---|---|---|---|
| Giray & Sadry (2021) [36] | Not specified | Prospective | CE, Lat ceph, Pan, JVA, occlusion analysis | No association with TMD development |
| Hoshi et al. (2022) [37] | MP, DD | Case Report | CE, MRI, CT, interview | Ortho + mini-implants → pain resolved; no recurrence at 2 years |
| Kaku et al. (2019) [32] | OA, DDwR | Case Report | MRI | Ortho + stabilization splint → pain resolved during treatment |
| Kato & Ono (2018) [33] | OA | Case Report | EMG, CBCT | Pain resolved; no recurrence at 2 years |
| Kau et al. (2020) [38] | TMD (significant pain), ICR | Case Report | CBCT, full ortho records, clinical photos | Ortho + orthognathic surgery → symptoms eliminate |
| Lee et al. (2019) [34] | ICR, TMD | Case Report | CBCT, Lat ceph, Pan | Ortho + mini-implants + stabilization splint → symptoms resolved; no recurrence at 2 years |
| Myllymäki et al. (2023) [39] | MP, arthralgia, TMJ clicking | Prospective | Questionnaire, CE | No association between orthodontic treatment and TMD symptoms |
| Paunonen et al. (2019) [40] | Myalgia, MP, arthralgia, DJD, DDWR, DDWoR | Longitudinal | Questionnaire, CE | Ortho + orthognathic surgery ↓ TMD prevalence |
| Ruf & Bock (2019) [25] | Myalgia, Arthralgia, DJD, DD | Longitudinal | CE | Herbst-based orthodontics: ↓ symptoms post-treatment; no long-term effect |
| Zibo et al. (2022) [35] | Myalgia, arthralgia | Longitudinal | Cephalometric radiographs | Ortho + orthognathic surgery: no effect on prevalence/severity |
| Author (Year) | Intervention | Key Outcome Metrics Used | Duration/Follow-Up | Overall Signal |
|---|---|---|---|---|
| Giray & Sadry (2021) [36] | Non-surgical | T-Scan® occlusal parameters (e.g., disclusion time), chewing pattern analysis; Joint Vibration Analysis (JVA) for TMD screening | During active treatment (~6 months) | No effect on TMD onset/progression |
| Myllymäki et al. (2023) [39] | Non-surgical | Self-reported TMD symptoms questionnaire at ages 12/15/32; PAR Index (occlusal severity/changes); multivariable logistic regression (OR, 95% CI) (e.g., TMJ sounds, headache) | Longitudinal (~20 years) | No effect (treatment not a driver); risk factors noted |
| Ruf & Bock (2019) [25] | Non-surgical | RDC/TMD & DC/TMD clinical classification; Helkimo Index; prevalence of signs/symptoms across timepoints | Long-term (≥15 years) | Mixed/no durable effect |
| Hoshi et al. (2022) [37] | Non-surgical | 6-DOF jaw-movement recording (Gnathohexagraph: incisal/condylar path lengths; symmetry); TMJ MRI (disk position); cephalometrics; clinical TMJ sounds & pain | ~24 months (with extended retention notes) | Improved |
| Kato & Ono (2018) [33] | Non-surgical | Surface EMG of masticatory muscles (masseter/temporalis/digastric) during MVC; CBCT of TMJ; cephalometrics; clinical symptom status | ~2–2.5 years | Improved |
| Kaku et al. (2019) [32] | Non-surgical | TMJ MRI (disk displacement), cephalometric angles (ANB, FMA, etc.); occlusal relationships; clinical TMD symptoms; panoramic/Schüller radiographs | ~2 years | Improved |
| Lee et al. (2019) [34] | Non-surgical | Clinical joint symptom status (pain/clicking); occlusal stability; routine orthodontic records/radiographs (case-level reporting) | ~2 years | Improved |
| Paunonen et al. (2019) [40] | Surgical | DC/TMD Axis I subdiagnoses (e.g., myalgia, arthralgia); symptom questionnaire; comparison of prevalence vs. non-treated Class II controls | Medium term (~4–8 years) | Improved (pain prevalence) |
| Zibo et al. (2022) [35] | Surgical | Mandibular movement amplitude (incl. mouth opening and deviation), TMJ pain, pathological TMJ sounds, masticatory muscle tenderness on palpation; cephalometrics, overjet/overbite | Short-term (14 days & 6 months) | No clear benefit (short-term) |
| Kau et al. (2020) [38] | Surgical | Maximum interincisal opening (MIO), lateral excursions, subjective pain/dysfunction, airway dimension (post-op), occlusal stability | Short-term (months) | Improved |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hung, M.; Gardner, J.D.; Lee, S.; Birmingham, W.C.; Stevens, R.M.; Schwartz, C.; Karimi, N.; Mohajeri, A. Treating Temporomandibular Disorders Through Orthodontics: A Scoping Review of Evidence, Gaps, and Clinical Guidance. Clin. Pract. 2025, 15, 182. https://doi.org/10.3390/clinpract15100182
Hung M, Gardner JD, Lee S, Birmingham WC, Stevens RM, Schwartz C, Karimi N, Mohajeri A. Treating Temporomandibular Disorders Through Orthodontics: A Scoping Review of Evidence, Gaps, and Clinical Guidance. Clinics and Practice. 2025; 15(10):182. https://doi.org/10.3390/clinpract15100182
Chicago/Turabian StyleHung, Man, Jacob Daniel Gardner, Samantha Lee, Wendy C. Birmingham, Richard M. Stevens, Connor Schwartz, Nader Karimi, and Amir Mohajeri. 2025. "Treating Temporomandibular Disorders Through Orthodontics: A Scoping Review of Evidence, Gaps, and Clinical Guidance" Clinics and Practice 15, no. 10: 182. https://doi.org/10.3390/clinpract15100182
APA StyleHung, M., Gardner, J. D., Lee, S., Birmingham, W. C., Stevens, R. M., Schwartz, C., Karimi, N., & Mohajeri, A. (2025). Treating Temporomandibular Disorders Through Orthodontics: A Scoping Review of Evidence, Gaps, and Clinical Guidance. Clinics and Practice, 15(10), 182. https://doi.org/10.3390/clinpract15100182








