Abstract
Background: Abfraction lesions are manifested as damage to hard tissues in the cervical area of dental crowns. The study aimed to assess the direct restoration of abfraction lesions according to the modified United States Public Health Service (USPHS) criteria for 24 months. The restorations were accomplished with Fuji Bulk–GC, Omnichroma Flow-Tokuyama, and Beautifil® II–Shofu dental materials, and the therapy was or was not associated with wearing thermoformed mouthguards. Methods: From the 53 selected and analyzed patients (n = 53), 28 patients (with restorations of abfraction lesions) belonged to the 1st group and 25 patients (with 105 restorations, who also wore mouthguards) belonged to the 2nd group. Blind determination assessments were effectuated at baseline and after 2, 6, 12, 18, and 24 months. Results showed that, regardless of the rating score, there are no significant statistical differences in the evaluation criteria between the two groups of patients Conclusions: For each material, the scores of USPHS criterion presented good clinical performances after 24 months, with no significant statistical differences between the fillings and the applied therapy in the two groups of patients.
1. Introduction
Non-carious cervical lesions (NCCLs) are represented by irreversible damage to the dental hard tissues (enamel, dentin, and cement) at the level of the cement–enamel junction (CEJ) [1,2]. The CEJ is stable over time [3] and presents four types of relationships: the dental cement overlaps the enamel; “edge-to-edge” junction; exposed dentin due to the existence of a gap between the enamel and cement; enamel covers the cement [4]. In areas affected by NCCLs, the tertiary reparative dentin presents sclerotic dentinal tubules, occluded by mineral precipitations of hydroxyapatite in other crystallographic forms. NCCLs are categorized as abrasion, attrition, erosion, abfraction, and biocorrosion [5,6]. NCCLs have a considerable prevalence today, and are actually related to people’s lifestyles and age [7].
Abfraction lesions are understood as having a multifactorial etiology, and represent an irreversible pathologic damage to the tooth’s hard tissue [2,8]. They are localized along dental crowns’ labial or buccal cervical zone, especially in premolars and the cervical area of incisors, canines, and molars [9,10,11]. According to El-Marakby et al. [12], abfraction lesions are frequent in the population over 40 years of age. Many researchers suggested the connection between the existence of non-physiological compressive occlusal forces, parafunction (e.g., bruxism), abrasion, and erosion [2,8,13,14,15,16,17]. Clinical appearances of abfractions are manifested as V- or wedge-shaped (with obviously delimited internal and external angles), or as C-profiled, forming lesions with circular walls. After the progression and the associated etiological factors, abfractions can be more profound than extensive. Sometimes they can be situated under the gingival margins [12]. The destruction of all hard dental tissues is progressive [18]. By depth, abfraction lesion are divided in three types: (a) lesions which penetrate only the enamel; (b) enamel and dentin lesions; and (c) lesions that penetrated the pulp tissue [19].
To diminish the initiation and progress of abfractions through the elusion/control of improper occlusal forces, the use of night guard appliances has been suggested [2]. Several kinds of oral parafunctional habits can affect the oral system, including bruxism [20,21,22]. Augmented action of the masticatory muscles (which can develop high biting forces of 400–1100 N) can determine the appearance of occlusal overloads and abfractions [23]. The therapy for occlusal overloads should include the use of intraoral devices (occlusal splints, thermoformed mouthguards) to protect the teeth and restorations from possibly excessive forces [24,25].
The aim of the study was to assess the direct restorations of abfraction lesions according to the modified United States Public Health Service (USPHS) criteria for a period of 24 months. The restorations were carried out with three types of dental materials, and the dental therapy was or was not associated with wearing thermoformed mouthguards.
2. Materials and Methods
The research was accomplished by implementing the ethical principles of the Declaration of Helsinki, good clinical practice, and GDPR practices regarding data protection. The research protocol was authorized by the Ethics Committee of the Dental Medicine Faculty, Titu Maiorescu University of Bucharest (No. 7 of 14.01.2019). All selected patients were notified regarding the study’s demands, and only those who willingly accepted the demands were admitted. The stages of the study and the necessity of monitoring were explained to each selected subject. Written informed consent was acquired ahead of the beginning of the study. The study was carried out in the Clinics of the Dental Medicine Faculties, from November 2019 to November 2022, with an 18-month intermission due to the context of the COVID-19 pandemic.
Before the selection of patients for the study, all the authors followed three practical calibration sessions regarding the precision of patients’ anamneses, clinical examination, and diagnosis; correct determination of abfraction’s degree; suitable use of the devices in conformity with the protocol (EMS Piezon, EMS Air-Flow, etc.); educational standards for adequate oral hygiene; proper application of all filling materials; the use of the same material and technique in the achievement of the thermoformed mouthguards; and the reliability of the study and acquired results. The patients selection for the study was performed by three authors, the treatment itself was performed by two other authors, and the follow-up observations were performed by the authors who were not involved in the other two stages of the study. Those who performed the direct restorations of the abfraction lesions were blinded to those who subsequently monitored the patients. The patients did not receive information regarding the location of each type of dental material applied.
A comparative study of the fillings (aspect, maintaining, and esthetical characteristics), applied as monotherapy for the 1st group of patients or applied in association with thermoformed mouthguards in 2nd group of patients, was realized. All patients included in the study were selected in conformity with the same inclusion and exclusion criteria. The trial has a blinded study design. Detailed anamnesis (with personal data, employment, the existence/absence of any allergies, nutritional habits, parafunctions/vicious habits, acute and/or chronic illnesses, etc.), accurate clinical examination (inspection of the oral cavity, assessment of oral hygiene status, localization and degree of abfraction lesions, differential diagnosis to other NCCLs types, etc.), and X-ray examinations (orthopantomograms or/and intraoral radiographs) were obtained to assess the eligibility of patients. The inclusion criteria in the study are presented in Table 1 and the exclusion criteria in Table 2.

Table 1.
Inclusion criteria for patients in the study.

Table 2.
Exclusion criteria for patients in the study.
Initially, 84 subjects were assessed for eligibility, but only 71 patients were enlisted in the study. The included patients were initially divided in 2 groups of 36 and 35 patients, but after being informed of the conditions of the study, the number of patients that agreed to wear the thermoformed mouthguards (second group) was less than that of the first group of patients. Patients who did not want to wear thermoformed mouthguards, but accepted the other requirements of the study, were transferred to the first group of patients. So, the 1st group of patients (n = 38) received esthetic fillings for the abfraction lesions, and the 2nd group (n = 33) were treated with esthetic fillings and thermoformed mouthguards. Of the 1st group of patients (n = 38), 1 patient was withdrawn voluntarily during the study, and 2 patients were excluded for lack of compliance. Of the 2nd group of patients (n = 33), 1 patient was withdrawn voluntarily. During follow-up, 14 patients were lost, out of which 3 patients belonging to the 1st group and 4 belonging to the 2nd group were withdrawn voluntarily and the rest were excluded for lack of compliance.
Finally, the number of evaluated patients was as follows: (n = 53), 28 for the 1st group (esthetic fillings of the abfraction lesions), and 25 for the 2nd group (esthetic fillings of the abfraction lesions and the use of thermoformed mouthguards). The age interval of the remaining and evaluated patients (53 patients, 29 male and 24 female), was 38–59 years (means 48.5 ± 10.5 years). The total number of studied abfraction lesions was 219, of which 114 (61 maxillary and 53 mandibular) belonged to the 1st group and 105 (57 maxillary and 48 mandibular) belonged to the 2nd group of patients (Table 3).

Table 3.
Samples of patients (n = 53).
2.1. Educational Measures for Adequate Oral Hygiene Technique
Oral hygiene training was performed with all selected patients 2 weeks before the restorative procedures. The presence/absence of dental plaque and calculus was revealed without any score with GC Tri Plaque ID Gel. Proper use of tooth-cleaning tools was presented and then practiced (modified Bass technique for tooth brushing [26] twice a day for three minutes, with Sensodyne Pronamel toothpaste and toothbrush, Pronamel Daily mouthwash–GSK). The scaling was performed with the EMS Piezon and EMS Air-Flow Master Units.
2.2. Dental Materials
The dental materials used for the restoration of abrasions were represented by GC Fuji Bulk (GC Corporation, Tokyo, Japan), Omnichroma Flow (Tokuyama Dental Corporation, Germany), and Beautifil® II (Shofu Dental, Kyoto, Japan). Fuji Bulk capsules (FuB) are a high-viscosity, rapid-setting, and self-curing universal shade glass ionomer cement, containing ultra-fine glass particles embedded in a higher-molecular-weight matrix of polyacrylic acid [27,28]. Omnichroma Flow (OmF) is a syringeable low-viscosity light-curing composite restorative material with a chameleonic effect. The composite matrix contains uniformly sized (260 nm) globulous filler radiopaque particles [29]. Beautifil® II (BeaII) is a bioactive, nanohybrid, fluoride-releasing, light-cured giomer. It is based on the technology of pre-reacted glass filler particles, which are embedded in the resin matrix [30].
2.3. Filling Technique
The color shade of each tooth with abfraction lesions was recorded before their restoration. A disposable saliva ejector was attached to the suction pump and cotton rolls were used to maintain a dry operating area. The restorations of the abfractions was performed without the use of gingival retraction cord, infiltration anesthesia, or rubber dam.
Every patient benefited from at least four restorations, carried out with Fuji Bulk capsules, Omnichroma Flow, and Beautifil® II. The materials were applied according to manufacturer’s instructions.
The selective-etch bonding technique for mineralized enamel was used. The abfraction area was dried without desiccation. GC cavity conditioner for the restored abfraction lesions was used. Then, one single layer of adhesive was applied depending on the filler. For GC Fuji Bulk, Universal Bond adhesive was used; Tokuyama was used for Omnichroma Flow; and FL-Bond II adhesive was applied for the Beautifil® II giomer. The restorative materials were placed in bulk and sculpted. Cervical matrices (Cure-Thru Clear Cervical Matrices, Premier Dental) were applied over the abfraction area and firmly pressed onto the surrounding enamel surface. A Woodpecker O-Light Curing Light was used for light curing. The restored area was defined with a flame-peak diamond bur, then finished with a rough disc (Sof-Lex Contouring and Polishing Discs-3M) and polished with medium and fine polishing cups (FlexiCups, Cosmedent, Chicago, IL, USA), silicon carbide brushes and polishing paste (Enamelize, Cosmedent, Chicago, USA). The patients were advised not apply any pressure on the restored teeth for 2 h.
2.4. Thermoformed Mouthguards
Thermoformed mouthguards were used to decrease the non-axial loading on the teeth. Thermoforming devices were vacuum manufactured out of a polymeric sheet plasticized by heating on a mold. After the depletion of the air, the specific shape was obtained, followed by processing and polishing [31]. Erkoflex soft-elastic thermoplastic ethylvinylacetate polymer sheets with 1.5 mm thickness (Erkodent, Erich Kopp GmbH, Pfalzgrafenweiler, Germany) were used.
2.5. Assessments Criteria of the Restorations in Treated Abfraction Lesions
The evaluation criteria used in this study for scoring the restorations accomplished in the abfraction treatment were represented by the modified United States Public Health Service (USPHS) criteria for direct clinical evaluation of the restoration [32,33]. Examinations were performed by visual inspection, the use of an explorer, or both (Table 4).

Table 4.
Modified USPHS criteria for direct clinical evaluation of restorations [32,33].
Both groups of patients benefited from the same dental treatment protocol, except for the thermoformed mouthguards, which were applied only in the 2nd group. The materials used for the direct restorations were randomly located, in order to achieve the blinding requirement of the study (only those who made the fillings knew which dental material was used and for which abfraction lesion). Two dentists restored the abfraction lesions.
Monitored patients (n = 53):
- -
- 1st group (n = 28) with 114 aesthetic fillings for abfraction lesions (61 maxillary and 53 mandibular), where 38 fillings with GC Fuji Bulk were performed, 37 with Omnichroma Flow, and 39 with Beautifil® II;
- -
- 2nd group of patients (n = 25), with 105 esthetic fillings for the abfraction lesions (57 maxillary and 48 mandibular), where 34 fillings were accomplished with GC Fuji Bulk, 36 with Omnichroma Flow, and 35 with Beautifil® II materials; also, the treatment for the patients of this group was associated with the use of thermoformed mouthguards. Of the 118 maxillary abfractions, the most restored teeth were premolars. Maxillary abfractions were represented by 84 premolars (71.18%) and 34 canines (28.81%). Mandibular abfractions were all observed in premolars (101). Of the total 219 abfractions, 185 (=84.47%) were located at the premolars.
For all the assessments of the researched criteria, the same type of dental mirror, probe, air cannula, dental unit, and dental loupe (Galilean-Style Dental Surgical Medical Binocular loupe, 3.5X magnification—Gain Express) were used. All parameters were recorded during evaluations by using a standardized case report form. Inconsistencies in the scores of the two evaluating dentists were solved by consensus during the assessment sessions. Patients were blinded regarding the used dental materials and their location. The assessments were accomplished by two dentists (other than the ones that treated the abfraction lesions) at baseline (after performing the fillings) and in follow-up assessments (2, 6, 12, 18, and 24 months later) (Figure 1).
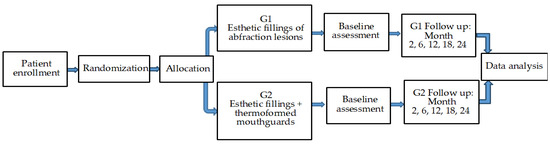
Figure 1.
Visit schedule of assessments.
The comparative analyses of the fillings and the behavior of the dental materials used in both groups of patients were performed in assessnents and after 24 months of follow-up.
2.6. Statistical Analyses
All statistical analyses were conducted in the IBM software SPSS 24 (Armonk, NY, USA).
Tests for differences among the two types of therapies applied in the first and second group of patients for each qualitative criterion used in the study (A, B, C, cumulative), each direct restorative material used (FuB, OmF, Beall), and every aspect (color match/stability, marginal discoloration, surface texture, anatomical contour/form, marginal adaptation/integrity, secondary/recurrent caries, retention of restoration/fracture) were carried out through means of the Pearson’s Chi Square test. In all cases, the significance level was considered 0.05; otherwise, it was specified. Missing corresponding p-values are due to lack of data.
3. Results
The flow diagram of the study is presented in Figure 2.
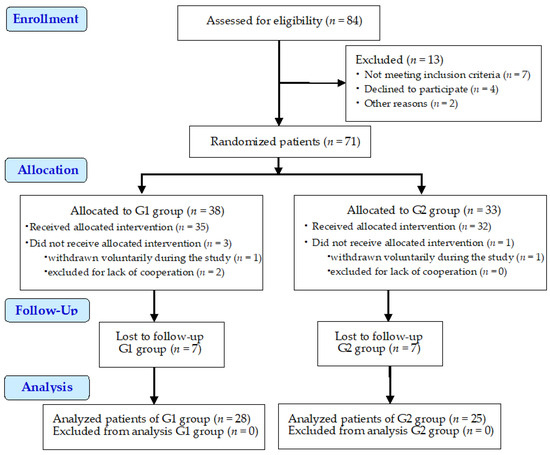
Figure 2.
Study flow diagram.
3.1. Clinical Results
The restorations of abfraction lesions in this study were accomplished with three types of direct restorative materials (a glass ionomer cement, Fuji Bulk; a composite resin with low viscosity, Omnichroma Flow; a nano-hybrid aesthetic giomer, Beautifil® II). The evaluation scores obtained by using the modified USPHS criteria of restorations referring to the 1st group of patients are presented in Table 5, and that for the 2nd group in Table 6.

Table 5.
Results of the assessed criteria in the 1st group of patients (n = 28, with 114 esthetic fillings of abfraction lesions).

Table 6.
Results of the assessed criteria in the 2nd group of patients (n = 25, with 105 esthetic fillings and thermoformed mouthguards).
The comparative results of the characteristics of the investigated restorations according to the modified USPHS criteria highlighted the following:
- -
- -
- -
- We mention that teeth with abfraction that were restored with one of the three types of materials did not require endodontic treatment.
Differences between the two groups of patients for each score level were checked, including the cumulative one since the interpretation can be divided for each variable and/or criterion.
The occurrence of new abfraction lesions was not observed in either group of patients during the assessments.
3.2. Statistical Results
Table 7 presents the comparative results regarding the studied criteria for the dental materials used for the rehabilitation of abfractions, with acceptable (B), unacceptable (C), and cumulative undesirable scores (B + C), as well as statistical results for both patient groups at all assessments.

Table 7.
Comparison of (B), (C), and (B + C) p values in both groups of patients, at all assessments.
The statistical results showed that, regardless of the rating score, there were no significant differences in the evaluated criteria between the two groups of patients, regardless of the restorative material used or score level. All of the patient’s teeth were rehabilitated with the same three types of restoration materials, by using the same technique, and the examination of their behavior during the two years of the study was performed by using the double-blind method.
4. Discussion
Fuji Bulk self-cure glass ionomer cement offers a balance between its restoring role and its protection of tooth hard tissue from acid challenges. It is indicated for use where acid resistance, less solubility, bulk curing, and speed of insertion represent priorities above aesthetics [27,28]. Light activation of conventional glass ionomer cements (GICs) permits the formation of supplemental cross-links [34]. The disadvantages include great polymerization contraction and cytotoxicity [35,36]. After Faridi et al. [37], the strength of the GICs was raised for the encapsulated form when compared to the manually mixed form. Through their bioactivity and fluoride-releasing properties, GICs prevent the occurrence of recurrent caries [38,39]. GICs with pre-reacted fillers of composite resins (CRs) exhibit reduced remineralization potential compared to traditional GICs, but are capable of inhibiting the demineralization of the enamel [40]. The incorporation in GICs of bioactive glasses can induce the precipitation of fluorapatite crystals in the demineralized dentin layer [41,42] and remineralization [41,43]. The use of giomers obtained through S-PRG technology determines the remineralization of the tooth’s hard structures, and they have a role in antibacterial activity [44,45,46,47,48].
Currently, CRs are the principal restorative materials due to their proper properties (aesthetics, reasonable durability) and relatively low cost, but their prime cause of failure is represented by secondary caries [49,50]. Omnichroma Flow is a one-shade flowable dental composite, with uniformly dimensioned supra-nano globulous filler, that uses Smart Chromatic Technology. They have high finish potential, increased stain resistance, low polymerization shrinkage, and high flexural and compressive strength. This composite is indicated for use in direct restorations in small cavities, cavity bases, cavity liners, and restoration of porcelain/composite [51,52].
Beautifil® II is a highly filled bioactive nano-hybrid dental CR containing SPRG-filler, and is resistant to acid attacks [53]. Bezerra et al. [54] evaluated the clinical behavior of GICs and CRs used in NCCL. CRs exhibited better outcomes than the conventional GICs in marginal adaptation and marginal discoloration, but GICs had better clinical results than CRs in the retention of the restorations. Yeo et al. [55] concluded that bulk-fill composite resins present significantly higher flexural strength than conventional composite resins. Boing et al. [56] compared the color match and the retention loss of GICs to RCs of restored NCCLs in a 2-year follow-up, and observed that in GICs the retention loss was lower compared to that of RCs, increased rugosity was noticed in GIC restorations, and the color in RCs was superior compared to GICs. In Heintze et al. [57], a meta-analysis of clinical outcome parameters in RC and GIC posterior restorations, the applied nanohybrid resins were not greatly superior to the hybrid or microhybrid RCs, but the restorations made with compomers and GICs demonstrated significantly shorter longevity. The survival rate after 10 years for RC restorations decreased to 85–90% (with no significant difference between hybrids, microhybrids, and nano-hybrids).
Ferracane [58] considers that many factors are responsible for the occurrence of marginal leakage and recurrent caries, and the clinical outcomes are different from in vitro results. Serin-Kalay [59] evaluated five commercially available bulk-fill RCs after their immersion in water and coffee, and bulk-fill dental materials presented a higher susceptibility to discoloration than conventional RCs. The esthetic features of GICs represent a subject that impedes their use in the case of patients with increased esthetic requirements [60].
At the beginning of this study, oral hygiene training was performed in the dental office for all the patients before completing the restorative procedures, until all of them applied the correct technique. The presence/absence of dental plaque and calculus was highlighted with GC Tri Plaque ID Gel without scoring. Patients brushed their teeth with the modified Bass technique twice a day for three minutes with 1 cm of Sensodyne Pronamel fluoride toothpaste with the Sensodyne Pronamel medium-hard toothbrush and micro-fine bristle heads, and rinsed their mouths daily for 1 min with approximately 10 mL of Pronamel daily mouthwash (GSK House, Brentford, UK). These dental hygiene procedures were verified during the study, and thus the health of the oral tissues was maintained. All selected and included patients had to show a Silness and Löe index score of 0 in the plaque index (no plaque is in the area adjacent to the gingiva) and in the gingival index (absence of inflammation, healthy gums). Teixeira et al. [61] studied the gingival tissues near NCCLs after their restoration with dental composites finished with two type of polishing techniques. Their results did not present differences in the examined periodontal parameters after 6 months. Nassar et al. [62] evaluated the biocompatibility of the restored abfractions with CRs (using different fillers finished with diverse polishers) for 3 months in patients with teeth affected by periodontal conditions and with diabetes mellitus. They found that the CRs with nanoparticles presented clinical biocompatibility, regardless of the type of polisher used.
The periodontium phenotypes, represented by the gingival and by the underlying osseous tissues, present a large variability and significantly different responses to injuries, and require specific treatment [63,64,65]. The treatment of cervical lesions can induce the occurrence of irritating lesions and chronic illness of the periodontium, especially when they are located at the level of the free gingiva, due to the technique applied in the isolation of the prosthetic field in filling the lesions and in the inappropriateness of the marginal sealing technique [66,67]. In this study, the abfraction restorations were carried out without the use of a gingival retraction cord or rubber dam on account of the fact that the cervical margins of the abfraction lesions were located at the level of the free gingival margin, so the structure of the marginal periodontium was not damaged.
Clinicians should choose suitable dental materials based on the proper features/properties and indications of an individual’s clinical state. Before any restorative intervention on abfraction lesions, the correspondence between the patient’s age and if the lesions endanger the tooth vitality and their function should be concluded because, in a significant number of cases, patients do not complain about their abfraction lesions as they are often painless and not remarkably visible. So, it is necessary to monitor these lesions at regular intervals, without any dental intervention, where no critical manifestations are observed, and where the lesions are shallow (less than 1 mm). The abfraction lesions should be monitored every 6–12 months and should accompany regular oral hygiene surveys [2].
Research about the biocompatibility and the specific properties of restorative materials, including the proper GIC and RC characteristics, filler particle features, surface changes, antimicrobial properties, remineralization, and wear behavior in the patient’s oral cavity, is called for and should be developed in the future [49,68].
The clinical relevance of the research, within its limits, consists of the results obtained for the investigated criteria, which suggests valuable outcomes for each of the restorative dental materials used (Fuji Bulk capsules, Omnichroma Flow, and Beautifil® II) in the restoration of abfraction lesions.
5. Conclusions
Within the study’s limitations, it has been shown that the scores for each USPHS criterion presented relevant clinical behavior after 24 months, with no significant statistical differences between the used restorative materials and the applied therapy in the two groups of patients.
Author Contributions
Conceptualization, B.C.C., A.B. (Alexandru Burcea), and E.S.B.; methodology, A.B. (Alexandru Burcea), E.S.B., B.C.C., L.L.M., and T.I.; software, O.A.M.; validation, A.B. (Anamaria Bechir), O.A.M., and T.I.; formal analysis, A.B. (Alexandru Burcea), L.L.M., O.A.M., and T.I.; investigation, A.B. (Anamaria Bechir), E.S.B., L.L.M., and T.I.; data curation, A.B. (Alexandru Burcea), A.B. (Anamaria Bechir), and O.A.M.; writing—original draft preparation, B.C.C. and A.B. (Anamaria Bechir); writing—review and editing, A.B. (Anamaria Bechir) and E.S.B.; visualization, A.B., L.L.M., and T.I.; supervision, E.S.B., A.B. (Anamaria Bechir), and L.L.M.; project administration, B.C.C. and O.A.M. All authors have read and agreed to the published version of the manuscript. All authors contributed equally to this study.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was accomplished by the implementation of the ethical principles of the Declaration of Helsinki and of the good clinical practice. The protocol was authorized by the Ethics Committee of Dental Medicine Faculty, Titu Maiorescu University of Bucharest (No. 7 of 14.01.2019).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patients to publish this paper.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Bănuț Oneț, D.; Barbu Tudoran, L.; Delean, A.G.; Șurlin, P.; Ciurea, A.; Roman, A.; Bolboacă, S.D.; Gasparik, C.; Muntean, A.; Soancă, A. Adhesion of Flowable Resin Composites in Simulated Wedge-Shaped Cervical Lesions: An In Vitro Pilot Study. Appl. Sci. 2021, 11, 3173. [Google Scholar] [CrossRef]
- Nascimento, M.M.; Dilbone, D.A.; Pereira, P.N.; Duarte, W.R.; Geraldeli, S.; Delgado, A.J. Abfraction lesions: Etiology, diagnosis, and treatment options. Clin. Cosmet. Investig. Dent. 2016, 8, 79–87. [Google Scholar] [CrossRef]
- Nguyen, K.-C.T.; Yan, Y.; Kaipatur, N.R.; Major, P.W.; Lou, E.H.; Punithakumar, K.; Le, L.H. Computer-Assisted Detection of Cemento-Enamel Junction in Intraoral Ultrasonographs. Appl. Sci. 2021, 11, 5850. [Google Scholar] [CrossRef]
- Koju, S.; Maharjan, N.; Yadav, D.K.; Bajracharya, D.; Baral, R.; Ojha, B. Morphological analysis of cementoenamel junction in permanent dentition based on gender and arches. J. Kantipur Dent. Coll. 2021, 2, 24–28. [Google Scholar]
- Goldberg, M. Non-carious cervical lesions (NCCL). J. Dent. Health Oral Disord Ther. 2021, 12, 67–72. [Google Scholar] [CrossRef]
- Zuza, A.; Racic, M.; Ivkovic, N.; Krunic, J.; Stojanovic, N.; Bozovic, D.; Bankovic-Lazarevic, D.; Vujaskovic, M. Prevalence of non-carious cervical lesions among the general population of the Republic of Srpska, Bosnia and Herzegovina. Int. Dent. J. 2019, 69, 281–288. [Google Scholar] [CrossRef]
- Medeiros, T.L.M.; Mutran, S.C.A.N.; Espinosa, D.G.; do Carmo Freitas Faial, K.; Pinheiro, H.H.C.; D’Almeida Couto, R.S. Prevalence and risk indicators of non-carious cervical lesions in male footballers. BMC Oral Health 2020, 20, 215. [Google Scholar] [CrossRef]
- Warreth, A.; Abuhijleh, E.; Almaghribi, M.A.; Mahwal, G.; Ashawish, A. Tooth surface loss: A review of literature. Saudi Dent. J. 2020, 32, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Bhullar, K.K.; Malhotra, S.; Bhagat, G.; Handa, A.; Kaur, R. Non- Carious Cervical Lesions: A Review. Sci. Prog. Res. 2021, 4, 391–399. [Google Scholar] [CrossRef]
- Peliz Senos Tróia, P.M.B.; Spuldaro, T.R.; Barroso da Fonseca, P.A.; de Oliveira Fernandes, G.V. Presence of Gingival Recession or Noncarious Cervical Lesions on Teeth under Occlusal Trauma: A Systematic Review. Eur. J. Gen. Dent. 2021, 10, 50–59. [Google Scholar] [CrossRef]
- Stănuşi, A.; Mercuţ, V.; Scrieciu, M.; Popescu, M.S.; Crăiţoiu Iacob, M.M.; Dăguci, L.; Castravete, S.; Vintilă, D.D.; Vătu, M. Effects of occlusal loads in the genesis of non-carious cervical lesions—A finite element study. Rom. J. Oral Rehabil. RJOR 2019, 11, 73–81. [Google Scholar]
- El-Marakby, A.M.; Al-Sabri, F.A.; Alharbi, S.A.; Halawani, S.M.; Yousef, M.T.B. Noncarious Cervical Lesions as Abfraction: Etiology, Diagnosis, and Treatment Modalities of Lesions: A Review Article. Dentistry 2017, 7, 438–442. [Google Scholar] [CrossRef]
- Trushkowsky, R.D. Esthetic Oral Rehabilitation with Veneers: A Guide to Treatment Preparation and Clinical Concepts; Springer International Publishing: Cham, Switzerland, 2020; pp. 336–339. Available online: https://books.google.ro/books?id=xqrdDwAAQBAJ&pg=PA336&lpg=PA336&dq=abfraction+Present+a+multifactorial+etiology+and+may+be+associated+with+the+pathological+wear+(abrasion,+erosion)&source=bl&ots=GW9FMEuG5J&sig=ACfU3U1H595jeLE5hw6wv0zaP0nuzTFklg&hl=ro&sa=X&ved=2ahUKEwj1nL2o58L2AhWat6QKHdXPAN4Q6AF6BAgqEAM#v=onepage&q=abfraction%20Present%20a%20multifactorial%20etiology%20and%20may%20be%20associated%20with%20the%20pathological%20wear%20(abrasion%2C%20erosion)&f=false (accessed on 13 March 2021).
- Badavannavar, A.N.; Anjari, S.; Nayak, K.; Khijmatgar, S. Abfraction: Etiopathogenesis, clinical aspect, and diagnostic-treatment modalities: A review. Indian J. Dent. Res. 2020, 31, 305–311. [Google Scholar] [PubMed]
- Mercut, V.; Popescu, S.M.; Scrieciu, M.; Amărăscu, M.O.; Vătu, M.; Diaconu, O.A.; Osiac, E.; Ghelase, Ş.M. Optical coherence tomography applications in tooth wear diagnosis. Rom. J. Morphol. Embryol. 2017, 58, 99–106. [Google Scholar]
- Tamgadge, S.; Pereira, T.; Tamgadge, A. Visualization of enamel rods in hunter-schreger bands and enamel in incipient lesion under polarized and light microscopy. Saudi J. Oral Sci. 2020, 7, 76–79. [Google Scholar] [CrossRef]
- Roberts, W.E.; Mangum, J.E.; Schneider, P.M. Pathophysiology of Demineralization, Part I: Attrition, Erosion, Abfraction, and Noncarious Cervical Lesions. Curr. Osteoporos. Rep. 2022, 20, 90–105. [Google Scholar] [CrossRef] [PubMed]
- Peumans, M.; Politano, G.; Van Meerbeek, B. Treatment of noncarious cervical lesions: When, why, and how. Int. J. Esthet. Dent. 2020, 15, 16–42. [Google Scholar]
- Rusu Olaru, A.; Popescu, M.R.; Dragomir, L.P.; Rauten, A.M. Clinical Study on Abfraction Lesions in Occlusal Dysfunction. Curr. Health Sci. J. 2019, 45, 390–397. [Google Scholar] [CrossRef]
- Demjaha, G.; Kapusevska, B.; Pejkovska-Shahpaska, B. Bruxism Unconscious Oral Habit in Everyday Life. Open Access Maced. J. Med. Sci. 2019, 7, 876–881. [Google Scholar] [CrossRef]
- Winocur-Arias, O.; Winocur, E.; Shalev-Antsel, T.; Reiter, S.; Levratovsky, S.; Emodi-Perlman, A.; Friedman-Rubin, P. Painful Temporomandibular Disorders, Bruxism and Oral Parafunctions before and during the COVID-19 Pandemic Era: A Sex Comparison among Dental Patients. J. Clin. Med. 2022, 11, 589. [Google Scholar] [CrossRef] [PubMed]
- Bustos, A.J.; Al-Talib, T.; Abubakr, N. Retrospective Analysis of the Association of Non-Carious Cervical Lesions with Bruxism. Open J. Stomatol. 2020, 10, 11–18. [Google Scholar] [CrossRef]
- Thanathornwong, B.; Suebnukarn, S. Clinical Decision Support Model to Predict Occlusal Force in Bruxism Patients. Healthc. Inform. Res. 2017, 23, 255–261. [Google Scholar] [CrossRef]
- Ladino, L.G.; Vargas, M.; Rodriguez, J.; López, E. Bruxism Management: A Comprehensive Review. Clin. Med. Rev. Case Rep 2020, 7, 316. [Google Scholar] [CrossRef]
- Beddis, H.; Pemberton, M.; Davies, S. Sleep bruxism: An overview for clinicians. Br. Dent. J. 2018, 225, 497–501. [Google Scholar] [CrossRef]
- Available online: https://www.Sensodyne.In/Blogs/Tooth-Brushing-Techniques.html (accessed on 12 April 2021).
- Perera, D.; Yu, S.C.H.; Zeng, H.; Meyers, I.A.; Walsh, L.J. Acid Resistance of Glass Ionomer Cement Restorative Materials. Bioengineering 2020, 7, 150. [Google Scholar] [CrossRef]
- Available online: https://www.gcaustralasia.com/Upload/product/pdf/1/BROCHURE_FUJI_BULK.pdf (accessed on 20 March 2019).
- Sharma, N.; Singh Samant, P. Omnichroma: The See-It -To-Believe -It Technology. EAS J. Dent. Oral Med. 2021, 3, 100–104. [Google Scholar]
- Available online: https://www.shofu.com/wp-content/uploads/Giomer-BRO-US.pdf (accessed on 22 June 2021).
- Takahashi, M.; Bando, Y. Effective thermoforming method for maintaining mouthguards thickness with a circular sheet using a circular frame. Dent. Traumatol. 2022, 38, 325–331. [Google Scholar] [CrossRef] [PubMed]
- Cavalheiro, C.P.; Souza, P.S.; Rocha, R.O.; Mendes, F.M.; Braga, M.M.; Raggio, D.P.; Lenzi, T.L. Choosing the criteria for clinical evaluation of composite restorations: An analysis of impact on reliability and treatment decision. Pesqui. Bras. Odontopediatria Clín Integr. 2020, 20, e5088. [Google Scholar] [CrossRef]
- Marquillier, T.; Doméjean, S.; Le Clerc, J.; Chemla, F.; Gritsch, K.; Maurin, J.-C.; Millet, P.; Perard, M.; Grosgogeat, B.; Dursun, E. The use of FDI criteria in clinical trials on direct dental restorations: A scoping review. Am. J. Dent. 2018, 68, 1–9. [Google Scholar] [CrossRef]
- Nicholson, J.W. Maturation processes in glass-ionomer dental cements. Acta Biomater. Odontol. Scand. 2018, 4, 63–71. [Google Scholar] [CrossRef]
- Roberts, H.; Berzins, D.; Nicholson, J. Long-Term Water Balance Evaluation in Glass Ionomer Restorative Materials. Materials 2022, 15, 807. [Google Scholar] [CrossRef] [PubMed]
- Özcan, M.; Garcia, L.F.R.; Volpato, C.A.M. Bioactive Materials for Direct and Indirect Restorations: Concepts and Applications. Front. Dent. Med. 2021, 2, 647267. [Google Scholar] [CrossRef]
- Faridi, M.A.; Khabeer, A.; Haroon, S. Flexural Strength of Glass Carbomer Cement and Conventional Glass Ionomer Cement Stored in Different Storage Media over Time. Med. Princ. Pract. 2018, 27, 372–377. [Google Scholar] [CrossRef] [PubMed]
- Rolim, F.G.; de Araújo Lima, A.D.; Lima Campos, I.C.; de Sousa Ferreira, R.; da Cunha Oliveira-Júnior, C.; Gomes Prado, V.L.; Vale, G.C. Fluoride Release of Fresh and Aged Glass Ionomer Cements after Recharging with High-Fluoride Dentifrice. Int. J. Dent. 2019, 2019, 9785364. [Google Scholar] [CrossRef] [PubMed]
- Ching, H.S.; Luddin, N.; Kannan, T.P.; Ab Rahman, I.; Abdul Ghani, N.R.N. Modification of glass ionomer cements on their physical-mechanical and antimicrobial properties. J. Esthet. Restor. Dent. 2018, 30, 557–571. [Google Scholar] [CrossRef] [PubMed]
- Leão, I.F.; Araújo, N.; Scotti, C.K.; Mondelli, R.F.L.; de Amoêdo Campos Velo, M.M.; Bombonatti, J.F.S. The Potential of a Bioactive, Pre-reacted, Glass-Ionomer Filler Resin Composite to Inhibit the Demineralization of Enamel in Vitro. Oper. Dent. 2021, 46, E11–E20. [Google Scholar] [CrossRef]
- Kim, H.J.; Bae, H.E.; Lee, J.E. Effects of bioactive glass incorporation into glass ionomer cement on demineralized dentin. Sci. Rep. 2021, 11, 7016. [Google Scholar] [CrossRef]
- Singh, S.; Patil, A.; Mali, S.; Jaiswal, H. Bioglass: A New Era in Modern Dentistry. Eur. J. General. Dent. 2022, 11, 1–6. [Google Scholar] [CrossRef]
- Skallevold, H.E.; Rokaya, D.; Khurshid, Z.; Zafar, M.S. Bioactive Glass Applications in Dentistry. Int. J. Mol. Sci. 2019, 20, 5960. [Google Scholar] [CrossRef]
- Sesiliana, M.; Riyanti, E. Giomer S-PRG Technology as an Alternative Restoration in Early Childhood Caries. World J. Dent. 2021, 12, 241–246. [Google Scholar] [CrossRef]
- Mayumi, K.; Miyaji, H.; Miyata, S.; Nishida, E.; Furihata, T.; Kanemoto, Y.; Sugaya, T.; Shitomi, K.; Akasaka, T. Antibacterial coating of tooth surface with ion-releasing pre-reacted glass-ionomer (S-PRG) nanofillers. Heliyon 2021, 7, e06147. [Google Scholar] [CrossRef] [PubMed]
- Colceriu Burtea, L.; Prejmerean, C.; Prodan, D.; Baldea, I.; Vlassa, M.; Filip, M.; Moldovan, M.; Moldovan, M.L.; Antoniac, A.; Prejmerean, V.; et al. New Pre-reacted Glass Containing Dental Composites (giomers) with Improved Fluoride Release and Biocompatibility. Materials 2019, 12, 4021. [Google Scholar] [CrossRef] [PubMed]
- Rusnac, M.E.; Gasparik, C.; Irimie, A.I.; Grecu, A.G.; Mesaroş, A.Ş.; Dudea, D. Giomers in dentistry—At the boundary between dental composites and glass-ionomers. Med. Pharm. Rep. 2019, 92, 123–128. [Google Scholar] [CrossRef]
- Francois, P.; Fouquet, V.; Attal, J.-P.; Dursun, E. Commercially Available Fluoride-Releasing Restorative Materials: A Review and a Proposal for Classification. Materials 2020, 13, 2313. [Google Scholar] [CrossRef]
- Pratap, B.; Gupta, R.K.; Bhardwaj, B.; Nag, M. Resin based restorative dental materials: Characteristics and future perspectives. Jpn. Dent. Sci. Rev. 2019, 55, 126–138. [Google Scholar] [CrossRef]
- Francisconi-Dos-Rios, L.F.; Tavares, J.; Oliveira, L.; Moreira, J.C.; Nahsan, F. Functional and aesthetic rehabilitation in posterior tooth with bulk-fill resin composite and occlusal matrix. Restor. Dent. Endod. 2020, 45, e9. [Google Scholar] [CrossRef]
- Baroudi, K.; Rodrigues, J.C. Flowable Resin Composites: A Systematic Review and Clinical Considerations. J. Clin. Diagn. Res. 2015, 9, ZE18–ZE24. [Google Scholar] [CrossRef]
- Omnichroma Flow. Available online: https://www.tokuyama-us.com/omnichroma-flow-dental-composite/ (accessed on 14 May 2019).
- Lai, Y.-J.; Takahashi, R.; Lin, P.-Y.; Kuo, L.; Zhou, Y.; Matin, K.; Chiang, Y.-C.; Shimada, Y.; Tagami, J. Anti-Demineralization Effects of Dental Adhesive-Composites on Enamel–Root Dentin Junction. Polymers 2021, 13, 3327. [Google Scholar] [CrossRef]
- Bezerra, I.M.; Brito, A.; de Sousa, S.A.; Santiago, B.M.; Cavalcanti, Y.W.; de Almeida, L. Glass ionomer cements compared with composite \resin in restoration of noncarious cervical lesions: A systematic review and meta-analysis. Heliyon 2020, 6, e03969. [Google Scholar] [CrossRef] [PubMed]
- Yeo, H.W.; Loo, M.Y.; Alkhabaz, M.; Li, K.C.; Choi, J.J.E.; Barazanchi, A. Bulk-Fill Direct Restorative Materials: An In Vitro Assessment of Their Physio-Mechanical Properties. Oral 2021, 1, 75–87. [Google Scholar] [CrossRef]
- Boing, T.F.; de Geus, J.L.; Wambier, L.M.; Loguercio, A.D.; Reis, A.; Gomes, O.M.M. Are Glass-Ionomer Cement Restorations in Cervical Lesions More Long-Lasting than Resin-based Composite Resins? A Systematic Review and Meta-Analysis. J. Adhes. Dent. 2018, 20, 435–452. [Google Scholar] [CrossRef] [PubMed]
- Heintze, S.D.; Loguercio, A.D.; Hanzen, T.A.; Reis, A.; Rousson, V. Clinical efficacy of resin-based direct posterior restorations and glass-ionomer restorations—An updated meta-analysis of clinical outcome parameters. Dent. Mater. 2022, 38, e109–e135. [Google Scholar] [CrossRef] [PubMed]
- Ferracane, J.L. Models of Caries Formation around Dental Composite Restorations. J. Dent. Res. 2017, 96, 364–371. [Google Scholar] [CrossRef] [PubMed]
- Serin-Kalay, T. Discoloration of Bulk-Fill Versus Conventional Composites: A Spectrophotometric Evaluation. Odovtos Int. J. Dent. Sci. 2021, 23, 63–72. [Google Scholar] [CrossRef]
- Murariu, A.; Dinu, C.; Agop Forna, D.; Stefanescu, V.; Topor, G.; Forna, N.C.; Fotea, S.; Gurau, G.; Iordache, C. Composite Resins—Multifunctional Restorative Material and Practical Approaches in Dental Field. Mater. Plast. 2020, 57, 276–284. [Google Scholar] [CrossRef]
- Teixeira, N.; Webber, M.B.F.; Nassar, C.A.; Camilotti, V.; Mendonça, M.J.; Sinhoreti, M.A.C. Influence of Different Composites and Polishing Techniques on Periodontal Tissues near Noncarious Cervical Lesions: A Controlled, Randomized, Blinded Clinical Trial. Eur. J. Dent. 2019, 13, 635–641. [Google Scholar] [CrossRef]
- Nassar, C.A.; Nassar, P.O.; Secundes, M.B.; Ribeiro Busato, P.D.M.; Camilotti, V. Composite resin restorations of non-carious cervical lesions in patients with diabetes mellitus and periodontal disease: Pilot study. Acta Odontológica Latinoam. 2012, 25, 279–286. [Google Scholar]
- Sedghi, L.M.; Bacino, M.; Kapila, Y.L. Periodontal Disease: The Good, The Bad, and The Unknown. Front. Cell. Infect. Microbiol. 2021, 11, 766944. [Google Scholar] [CrossRef]
- Kahon, C.; Sachin, S.S.; Darsha, J. Dimensions of Periodontium (Biotype Versus Phenotype)—A Literature Review. RGUHS J. Dent. Sci. 2022, 14, 24–30. [Google Scholar]
- Malpartida-Carrillo, V.; Tinedo-Lopez, P.L.; Guerrero, M.E.; Amaya-Pajares, S.P.; Özcan, M.; Rösing, C.K. Periodontal phenotype: A review of historical and current classifications evaluating different methods and characteristics. J. Esthet. Restor. Dent. 2021, 33, 432–445. [Google Scholar] [CrossRef]
- Purushotham, S.; Manjunath, N.; D’Souza, M.L.; Shetty, R. An interdisciplinary approach for the management of noncarious lesions. J. Indian Soc. Periodontol. 2016, 20, 211–215. [Google Scholar] [CrossRef] [PubMed]
- Srimaneepong, V.; Heboyan, A.; Zafar, M.S.; Khurshid, Z.; Marya, A.; Fernandes, G.V.O.; Rokaya, D. Fixed Prosthetic Restorations and Periodontal Health: A Narrative Review. J. Funct. Biomater. 2022, 13, 15. [Google Scholar] [CrossRef] [PubMed]
- Bechir, F.; Bataga, S.M.; Tohati, A.; Ungureanu, E.; Cotrut, C.M.; Bechir, E.S.; Suciu, M.; Vranceanu, D.M. Evaluation of the Behavior of Two CAD/CAM Fiber-Reinforced Composite Dental Materials by Immersion Tests. Materials 2021, 14, 7185. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).