Clinical Research in Prehospital Care: Current and Future Challenges
Abstract
1. Introduction
2. Research in Prehospital Care: State of the Art
3. Research in Prehospital Care: Major Challenges
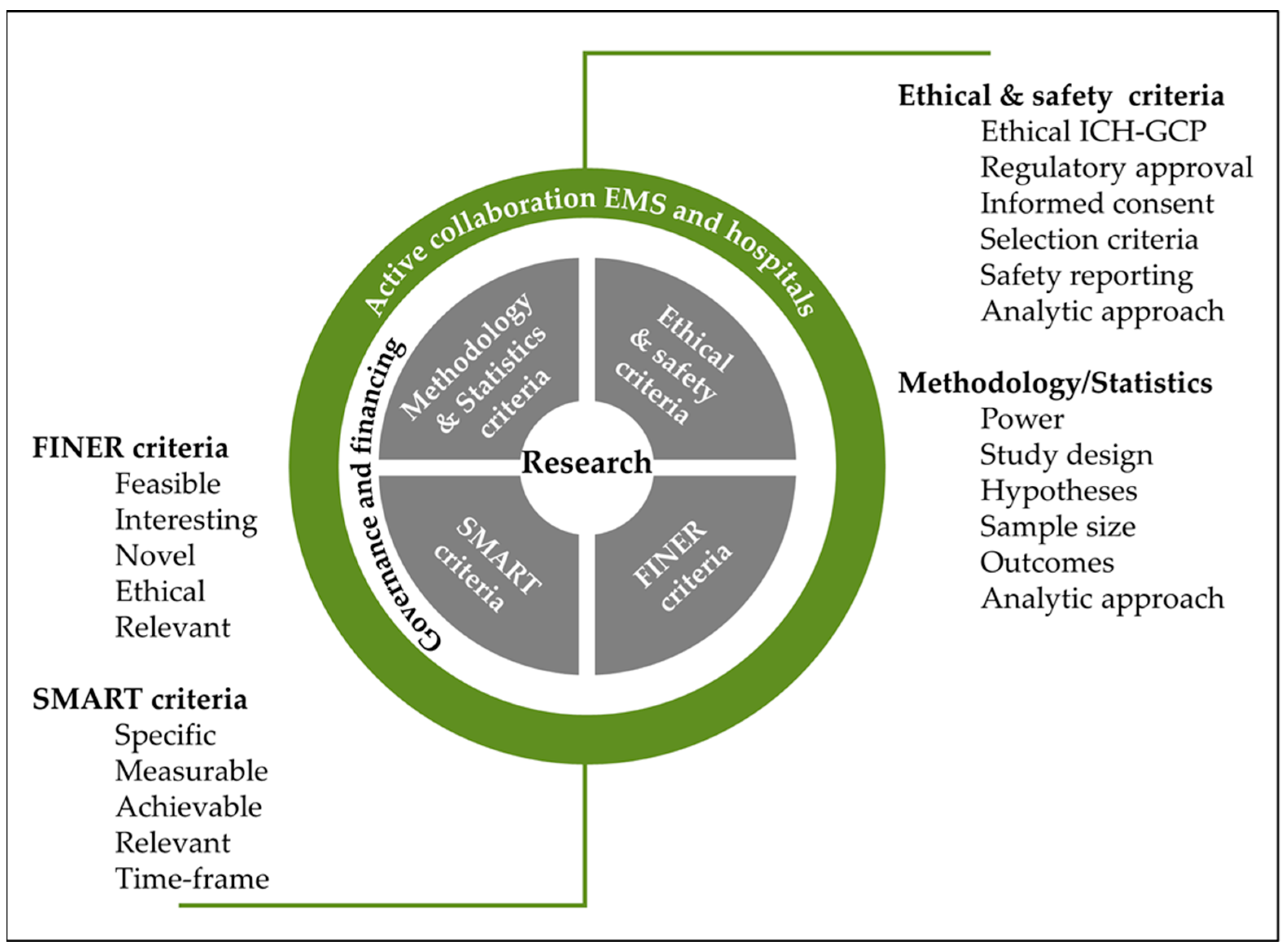
- “What are the aims of the study?”, which encompasses the SMART (Specific, Measurable, Achievable, Relevant, and Time-frame) criteria (Figure 1) and are linked to methodology/statistics.
- “Why, Where and How should the study be conducted?”, which encompasses the FINER (feasible, interesting, novel, ethical, relevant) criteria (Figure 1) and are linked to ethical/safety criteria.
3.1. Limited Resources and Infrastructure
3.2. Ethical Considerations
3.3. Impact of Time Constraints
3.4. Safety Concerns
3.5. Data Collection and Analysis
| Findings | Target Population | Study Design |
|---|---|---|
| Rottman et al. (1997) compared on-scene time, appropriateness of therapy, and accuracy of paramedic clinical assessments when prehospital care was provided with the use of on-line medical control (OLMC) by EMS-certified nurses from a single base station or by paramedics using chief complaint-based protocols. The use of protocols resulted in small improvements in both on-scene time and the appropriateness of therapeutic decisions, without a change in agreement between paramedic and physician [82]. | EMS call center | Prospective cohort |
| Holstein et al. (2003) found that training of the emergency team is an effective and efficient intervention to improve quality of treatment and prognosis outcome for patients with type 1 diabetic emergencies [83]. | Diabetic patients | Prospective population-based study |
| Watts et al. (2004) found that providers who were able to learn and implement the Brain Trauma Foundation (BTF) Guidelines and outcomes in traumatic brain injury patients were significantly improved [84]. | Traumatic brain injury patients | Prospective observational study |
| Combes et al. (2006) determined the rate of difficult intubations and the factors associated with prehospital difficult airways when a standard protocol for sedation and intubation was applied [85]. | Tracheal intubation patients | Observational et prospective study |
| Sasson et al. (2009) discussed the operational issues within local EMS systems that may serve as barriers or facilitators to full acceptance of national guidelines for prehospital termination of resuscitation in appropriate circumstances [86]. | Termination of resuscitation | Qualitative and focus groups study |
| Atary et al. (2010) showed that a standardized regional acute myocardial infarction treatment protocol achieved optimal and uniformly distributed pre-hospital performance in the region ‘Hollands-Midden’, resulting in minimal time delays regardless of area of residence [87]. | Myocardial injuries patients | Standardized pre-hospital care guidelines applied in practice |
| Rognas et al. (2013) reported a prospective quality control study of the effect on pre-hospital critical care anesthesiologists’ behavior of implementing a standard operating procedure for pre-hospital controlled ventilation [88]. | Airway management patients | Prospective registry |
| Brandler et al. (2015) found that EMS care providers missed more than a third of stroke cases. Seizures and other atypical presentations contribute significantly to stroke misdiagnosis [89]. | Prehospital stroke identification methods | Retrospective report |
| Osborne et al. (2015) summarized the United Kingdom (UK) Ambulance Service guidelines for the management of seizures and explored the extent to which these guidelines are evidence-based [90]. | Management of seizures | Guidelines report |
| Kerner et al. (2017) evaluated how the use of checklists for prehospital emergency care may help to improve adherence to treatment guidelines [91]. | Checklists in prehospital emergency care | Standard operating procedures study |
| Lenssen et al. (2017) suggested that routine, remote, physician-based, telemedically-delegated (opioid-based) analgesia in trauma and non-trauma emergencies, as applied by paramedics, shows comparable efficacy to analgesia administered by on-scene prehospital EMS physicians [92]. | Analgesia management patients | Retrospective observational study |
| Pride et al. (2017) discussed the importance of prehospital care delivery and triage in cases of stroke with emergent large vessel occlusion (ELVO) [93]. | Stroke patients | Guidelines report |
| Rodríguez et al. (2020) found that the use of early warning scores can help the EMS to differentiate traumatic brain injury patients with a high risk of deterioration [94]. | Traumatic brain injury patients | Prospective cohort |
3.6. Selection of a Homogeneous Study Group
4. Discussion
4.1. What Are the Solutions to Implement?
4.2. What Are the Future Opportunities and Perspectives?
| Findings | Target Population | Study Design |
|---|---|---|
| Liu et al. (2014) highlighted the potential for machine learning algorithms to improve the accuracy of predicting the need for life-saving interventions in trauma patients, enabling faster and more appropriate treatment for these patients. The hybrid system developed in this study may also serve as a model for integrating machine learning algorithms into clinical decision-making processes [123]. | Analgesia management patients | Retrospective and prospective cohort study |
| Desautels et al. (2016) highlighted the potential for machine learning models to improve sepsis prediction in the ICU using minimal EHR data, which may be particularly useful in resource-limited settings. However, the study also acknowledges the limitations of using retrospective data and the need for prospective validation of the models in clinical practice [124]. | Sepsis prediction | Retrospective study |
| Cheng et al. (2021) highlighted the potential for deep learning algorithms to assist sonographers in the detection of abdominal free fluid in Morison’s pouch during sonography in trauma, potentially enabling faster and more accurate diagnosis of abdominal trauma. However, the study also acknowledges the limitations of using retrospective data and the need for prospective validation in clinical practice [125]. | Abdominal trauma patients | Observational study |
| Fontanellaz et al. (2021) highlighted the potential for deep learning algorithms to assist radiologists in the detection of COVID-19 using chest radiographs, potentially enabling faster and more accurate diagnosis of the disease. However, the study also acknowledges the limitations of using retrospective data and the need for prospective validation of the deep learning diagnostic support system in clinical practice [126]. | COVID-19 patients | Retrospective study |
| Uchida et al. (2021) demonstrated the feasibility and effectiveness of using machine learning algorithms as a diagnostic support tool in the prediction of stroke probability and type at the prehospital stage, potentially leading to improved stroke care and patient outcomes [127]. | Stroke-management patients | Retrospective and prospective cohort study |
| Shahi et al. (2021) highlighted the potential for deep learning algorithms to improve decision-making in pediatric blunt solid organ injury, enabling faster and more accurate predictions of the need for massive transfusion, need for operative management, and mortality risk. The use of deep learning algorithms in trauma care may also reduce healthcare costs and improve patient outcomes [128]. | Pediatric blunt solid organ injury | Retrospective study |
| Chen et al. (2022) highlighted the potential for AI-assisted systems to improve prehospital care by enabling faster and more accurate detection of ST-elevation myocardial infarction, which is crucial for timely intervention and improved patient outcomes. The use of a mini-12-lead ECG device also makes the system more accessible for use in resource-limited settings [129]. | Myocardial injury patients | Retrospective study |
5. Limitations
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Wibring, K.; Magnusson, C.; Axelsson, C.; Lundgren, P.; Herlitz, J.; Andersson Hagiwara, M. Towards definitions of time-sensitive conditions in prehospital care. Scand. J. Trauma Resusc. Emerg. Med. 2020, 28, 7. [Google Scholar] [CrossRef]
- World Health Organization. Classification and Minimum Standards for Emergency Medical Teams; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Patiño, A.M.; Chen, J.; DeVos, E.L.; Lee, J.A.; Anderson, K.; Banks, M.; Arbelaez, C. Emergency medicine around the world: Analysis of the 2019 American College of emergency physicians international Ambassador country reports. J. Am. Coll. Emerg. Physicians Open 2022, 3, e12681. [Google Scholar] [CrossRef] [PubMed]
- Moore, M.R.; Archer, M.L. Red cross and red crescent health information system (RCHIS): Functional design and usability testing protocol. Prehosp. Disaster Med. 2019, 34, s86–s87. [Google Scholar] [CrossRef]
- Debenham, S.; Fuller, M.; Stewart, M.; Price, R.R. Where there is no EMS: Lay providers in Emergency Medical Services care-EMS as a public health priority. Prehospital Disaster Med. 2017, 32, 593–595. [Google Scholar] [CrossRef]
- Martin-Gill, C.; Brown, K.M.; Cash, R.E.; Haupt, R.M.; Potts, B.T.; Richards, C.T.; Prehospital Guidelines Consortium. 2022 systematic review of evidence-based guidelines for prehospital care. Prehospital Emerg. Care 2023, 27, 131–143. [Google Scholar] [CrossRef] [PubMed]
- Jobé, C.; Carron, P.N.; Métrailler, P.; Bellagamba, J.M.; Briguet, A.; Zurcher, L.; Dami, F. Introduction of Telemedicine in a Prehospital Emergency Care Setting: A Pilot Study. Int. J. Telemed. Appl. 2023, 2023, 1171401. [Google Scholar] [CrossRef]
- Metelmann, B.; Metelmann, C. Mobile Health Applications in Prehospital Emergency Medicine. In Mobile Health Applications for Quality Healthcare Delivery; IGI Global: Hershey, PA, USA, 2019; pp. 117–135. [Google Scholar]
- Kunz, A.; Ebinger, M.; Geisler, F.; Rozanski, M.; Waldschmidt, C.; Weber, J.E.; Wendt, M.; Winter, B.; Zieschang, K.; Fiebach, J.B.; et al. Functional outcomes of pre-hospital thrombolysis in a mobile stroke treatment unit compared with conventional care: An observational registry study. Lancet Neurol. 2016, 15, 1035–1043. [Google Scholar] [CrossRef]
- Plummer, V.; Boyle, M. EMS systems in lower-middle income countries: A literature review. Prehospital Disaster Med. 2017, 32, 64–70. [Google Scholar]
- Sudantha, B.H.; Warnakulasooriya, K.M.H.K.; Jayasuriya, Y.P.; Ratnayaka, G.R.; Mahanama, P.K.S.; Warusavitharana, E.J.; Weerasinghe, S.N. Open-source implementation of an integrated low-cost environmental monitoring system (EMS) for developing countries. Bhumi Plan. Res. J. 2018, 6, 23–29. [Google Scholar] [CrossRef]
- Rathore, N.; Jain, P.K.; Parida, M. A sustainable model for emergency medical services in developing countries: A novel approach using partial outsourcing and machine learning. Risk Manag. Healthc. Policy 2022, 15, 193–218. [Google Scholar] [CrossRef]
- El Sayed, M.; Al Assad, R.; Abi Aad, Y.; Gharios, N.; Refaat, M.M.; Tamim, H. Measuring the impact of emergency medical services (EMS) on out-of-hospital cardiac arrest survival in a developing country: A key metric for EMS systems’ performance. Medicine 2017, 96, e7570. [Google Scholar] [CrossRef]
- Bhandari, D.; Yadav, N.K. Developing an integrated emergency medical services in a low-income country like Nepal: A concept paper. Int. J. Emerg. Med. 2020, 13, 7. [Google Scholar] [CrossRef]
- Thygerson, S.; Memmott, G.; Chaney, R. A Global Emergency: Identifying Priorities for Reforming International Emergency Medical Systems. Med. Res. Arch. 2023, 11, 3922. [Google Scholar] [CrossRef]
- Miskimins, R.; Pati, S.; Schreiber, M. Barriers to clinical research in trauma. Transfusion 2019, 59 (Suppl. 1), 846–853. [Google Scholar] [CrossRef] [PubMed]
- Cimino, J.; Braun, C. Building a competitive infrastructure to support clinical research in healthcare institution. Eur. J. Clin. Investig. 2021, 51, e13641. [Google Scholar] [CrossRef]
- Steg, P.G.; Bonnefoy, E.; Chabaud, S.; Lapostolle, F.; Dubien, P.Y.; Cristofini, P.; Touboul, P. Impact of time to treatment on mortality after prehospital fibrinolysis or primary angioplasty: Data from the CAPTIM randomized clinical trial. Circulation 2003, 108, 2851–2856. [Google Scholar] [CrossRef]
- Bernard, S.A.; Nguyen, V.; Cameron, P.; Masci, K.; Fitzgerald, M.; Cooper, D.J.; Walker, T.; Std, B.P.; Myles, P.; Murray, L.; et al. Prehospital rapid sequence intubation improves functional outcome for patients with severe traumatic brain injury: A randomized controlled trial. Ann. Surg. 2010, 252, 959–965. [Google Scholar] [CrossRef] [PubMed]
- El-Menyar, A.; Sathian, B.; Asim, M.; Latifi, R.; Al-Thani, H. Efficacy of prehospital administration of tranexamic acid in trauma patients: A meta-analysis of the randomized controlled trials. Am. J. Emerg. Med. 2018, 36, 1079–1087. [Google Scholar] [CrossRef]
- Martín-Rodríguez, F.; Del Pozo Vegas, C.; Mohedano-Moriano, A.; Polonio-López, B.; Miquel, C.M.; Viñuela, A.; Fernández, C.D.; Correas, J.G.; López-Izquierdo, R.; Martín-Conty, J.L. Role of Biomarkers in the Prediction of Serious Adverse Events after Syncope in Prehospital Assessment: A Multi-Center Observational Study. J. Clin. Med. 2020, 9, 651. [Google Scholar] [CrossRef]
- Misra, D.P.; Ravindran, V. An overview of the functionalities of PubMed. J. R. Coll. Physicians Edinb. 2022, 52, 8–9. [Google Scholar] [CrossRef]
- Berkowitz, J.; Cotarelo, A.; Washko, J.; Levinsky, B. Emergency Medical Services and the Elderly Patient: Prehospital Management. In Acute Care Surgery in Geriatric Patients; Springer International Publishing: Cham, Switzerland, 2023; pp. 107–113. [Google Scholar]
- Ramage, L.; McLachlan, S.; Williams, K. Determining the top research priorities in UK prehospital critical care: A modified delphi study. Emerg. Med. J. 2023, 40, 271–276. [Google Scholar] [CrossRef]
- Delgado, R.C.; Gonzalez, K.A.; Martinez, J.A.C.; Alvarez, T.C.; Gonzalez, P.A. Top research priorities in prehospital care in Spain. Prehospital Disaster Med. 2023, 38, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Ali, J.; Howard, M.R.; Stedman, M.R.; Miller, P.P.M.; Winn, J.R.; Butler, K.A.M.; Gonsalves, D.R.; Chang, H.M.; Adam, R.M.; Williams, J. The Advanced Trauma Life Support (ATLS) program improves trauma patient outcome in a developing country. J. Trauma Acute Care Surg. 1992, 33, 149. [Google Scholar] [CrossRef]
- Søreide, K. Three decades (1978–2008) of Advanced Trauma Life Support (ATLS™) practice revised and evidence revisited. Scand. J. Trauma Resusc. Emerg. Med. 2008, 16, 19. [Google Scholar] [CrossRef] [PubMed]
- Cummins, R.O.; Eisenberg, M.S.; Hallstrom, A.P.; Litwin, P.E. Survival of out-of-hospital cardiac arrest with early initiation of cardiopulmonary resuscitation. Am. J. Emerg. Med. 1985, 3, 114–119. [Google Scholar] [CrossRef]
- Bickell, W.H.; Wall, M.J., Jr.; Pepe, P.E.; Martin, R.R.; Ginger, V.F.; Allen, M.K.; Mattox, K.L. Immediate versus delayed fluid resuscitation for hypotensive patients with penetrating torso injuries. N. Engl. J. Med. 1994, 331, 1105–1109. [Google Scholar] [CrossRef]
- Sampalis, J.S.; Denis, R.; Lavoie, A.; Fréchette, P.; Boukas, S.; Nikolis, A.; Benoit, D.; Fleiszer, D.; Brown, R.; Churchill-Smith, M.; et al. Trauma care regionalization: A process-outcome evaluation. J. Trauma Acute Care Surg. 1999, 46, 565–581. [Google Scholar] [CrossRef]
- Gausche, M.; Lewis, R.J.; Stratton, S.J.; Haynes, B.E.; Gunter, C.S.; Goodrich, S.M.; Poore, P.D.; McCollough, M.D.; Henderson, D.P.; Pratt, F.D.; et al. Effect of out-of-hospital pediatric endotracheal intubation on survival and neurological outcome: A controlled clinical trial. JAMA 2000, 283, 783–790. [Google Scholar] [CrossRef]
- Davis, D.P.; Peay, J.; Sise, M.J.; Vilke, G.M.; Kennedy, F.; Eastman, A.B.; Brent, A.; Velky, T.; Hoyt, D.B. The impact of prehospital endotracheal intubation on outcome in moderate to severe traumatic brain injury. J. Trauma Acute Care Surg. 2005, 58, 933–939. [Google Scholar] [CrossRef]
- Richard, J.; Osmond, M.H.; Nesbitt, L.; Stiell, I.G. Management and outcomes of pediatric patients transported by emergency medical services in a Canadian prehospital system. Can. J. Emerg. Med. 2006, 8, 6–12. [Google Scholar] [CrossRef]
- Ortolani, P.; Marzocchi, A.; Marrozzini, C.; Palmerini, T.; Saia, F.; Baldazzi, F.; Silenzi, S.; Taglieri, N.; Bacchi-Reggiani, M.; Branzi, A.; et al. Usefulness of prehospital triage in patients with cardiogenic shock complicating ST-elevation myocardial infarction treated with primary percutaneous coronary intervention. Am. J. Cardiol. 2007, 100, 787–792. [Google Scholar] [CrossRef] [PubMed]
- Kragh, J.F., Jr.; Walters, T.J.; Baer, D.G.; Fox, C.J.; Wade, C.E.; Salinas, J.; Holcomb, J.B. Survival with emergency tourniquet use to stop bleeding in major limb trauma. Ann. Surg. 2009, 249, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Nassif, A.; Ostermayer, D.G.; Hoang, K.B.; Claiborne, M.K.; Camp, E.A.; Shah, M.I. Implementation of a prehospital protocol change for asthmatic children. Prehospital Emerg. Care 2018, 22, 457–465. [Google Scholar] [CrossRef] [PubMed]
- Dracup, K.; McKinley, S.; Riegel, B.; Moser, D.K.; Meischke, H.; Doering, L.V.; Davidson, P.; Paul, S.; Baker, H.; Pelter, M. A randomized clinical trial to reduce patient prehospital delay to treatment in acute coronary syndrome. Circ. Cardiovasc. Qual. Outcomes 2009, 2, 524–532. [Google Scholar] [CrossRef] [PubMed]
- Bergs, J.; Sabbe, M.; Moons, P. Prehospital stroke scales in a Belgian prehospital setting: A pilot study. Eur. J. Emerg. Med. 2010, 17, 2–6. [Google Scholar] [CrossRef]
- Monsieurs, K.G.; De Regge, M.; Vansteelandt, K.; De Smet, J.; Annaert, E.; Lemoyne, S.; Kalmar, A.; Calle, P.A. Excessive chest compression rate is associated with insufficient compression depth in prehospital cardiac arrest. Resuscitation 2012, 83, 1319–1323. [Google Scholar] [CrossRef]
- Meretoja, A.; Kaste, M. Pre-and in-hospital intersection of stroke care. Ann. N. Y. Acad. Sci. 2012, 1268, 145–151. [Google Scholar] [CrossRef]
- Brown, J.B.; Sperry, J.L.; Fombona, A.; Billiar, T.R.; Peitzman, A.B.; Guyette, F.X. Pre-trauma center red blood cell transfusion is associated with improved early outcomes in air medical trauma patients. J. Am. Coll. Surg. 2015, 220, 797–808. [Google Scholar] [CrossRef]
- Lockey, D.J.; Healey, B.; Crewdson, K.; Chalk, G.; Weaver, A.E.; Davies, G.E. Advanced airway management is necessary in prehospital trauma patients. Br. J. Anaesth. 2015, 114, 657–662. [Google Scholar] [CrossRef]
- Crewdson, K.; Lockey, D.J.; Røislien, J.; Lossius, H.M.; Rehn, M. The success of pre-hospital tracheal intubation by different pre-hospital providers: A systematic literature review and meta-analysis. Crit. Care 2017, 21, 31. [Google Scholar] [CrossRef]
- Wang, H.E.; Schmicker, R.H.; Daya, M.R.; Stephens, S.W.; Idris, A.H.; Carlson, J.N.; Colella, M.; Herren, H.; Hansen, M.; Richmond, N.; et al. Effect of a strategy of initial laryngeal tube insertion vs endotracheal intubation on 72-hour survival in adults with out-of-hospital cardiac arrest: A randomized clinical trial. JAMA 2018, 320, 769–778. [Google Scholar] [CrossRef] [PubMed]
- Guyette, F.X.; Brown, J.B.; Zenati, M.S.; Early-Young, B.J.; Adams, P.W.; Eastridge, B.J.; Nirula, R.; Vercruysse, G.; O’Keeffe, T.; Joseph, B.; et al. Tranexamic acid during prehospital transport in patients at risk for hemorrhage after injury: A double-blind, placebo-controlled, randomized clinical trial. JAMA Surg. 2021, 156, 11–20. [Google Scholar] [CrossRef]
- Scquizzato, T.; Imbriaco, G.; Moro, F.; Losiggio, R.; Cabrini, L.; Consolo, F.; Zangrillo, A. Non-invasive ventilation in the prehospital emergency setting: A systematic review and meta-analysis. Prehospital Emerg. Care 2023, 27, 566–574. [Google Scholar] [CrossRef]
- Carney, N.; Totten, A.M.; Cheney, T.; Jungbauer, R.; Neth, M.R.; Weeks, C.; Davis-O’Reilly, C.; Fu, R.; Yu, Y.; Chou, R.; et al. Prehospital airway management: A systematic review. Prehospital Emerg. Care 2021, 26, 716–727. [Google Scholar] [CrossRef]
- McMullan, J.; Droege, C.; Strilka, R.; Hart, K.; Lindsell, C. Intranasal ketamine as an adjunct to fentanyl for the prehospital treatment of acute traumatic pain: Design and rationale of a randomized controlled trial. Prehospital Emerg. Care 2021, 25, 519–529. [Google Scholar] [CrossRef] [PubMed]
- Helwig, S.A.; Ragoschke-Schumm, A.; Schwindling, L.; Kettner, M.; Roumia, S.; Kulikovski, J.; Keller, I.; Manitz, M.; Martens, D.; Fassbender, K.; et al. Prehospital stroke management optimized by use of clinical scoring vs mobile stroke unit for triage of patients with stroke: A randomized clinical trial. JAMA Neurol. 2019, 76, 1484–1492. [Google Scholar] [CrossRef]
- Ehlers, J.; Fisher, B.; Peterson, S.; Dai, M.; Larkin, A.; Bradt, L.; Mann, N.C. Description of the 2020 NEMSIS public-release research dataset. Prehospital Emerg. Care 2022, 27, 473–481. [Google Scholar] [CrossRef]
- Perkins, G.D.; Ji, C.; Deakin, C.D.; Quinn, T.; Nolan, J.P.; Scomparin, C.; Regan, S.; Long, J.; Slowther, A.; Lall, R.; et al. A randomized trial of epinephrine in out-of-hospital cardiac arrest. N. Engl. J. Med. 2018, 379, 711–721. [Google Scholar] [CrossRef] [PubMed]
- Delano, M.J.; Rizoli, S.B.; Rhind, S.G.; Cuschieri, J.; Junger, W.; Baker, A.J.; Bulger, E.M. Prehospital resuscitation of traumatic hemorrhagic shock with hypertonic solutions worsens hypocoagulation and hyperfibrinolysis. Shock 2015, 44, 25. [Google Scholar] [CrossRef]
- Sikka, N.; Margolis, G. Understanding diversity among prehospital care delivery systems around the world. Emerg. Med. Clin. 2005, 23, 99–114. [Google Scholar] [CrossRef]
- Bounes, V.; Dehours, E.; Houze-Cerfon, V.; Vallé, B.; Lipton, R.; Ducassé, J.L. Quality of publications in emergency medicine. Am. J. Emerg. Med. 2013, 31, 297–301. [Google Scholar] [CrossRef] [PubMed]
- Charzyńska, E.; Habibi Soola, A.; Mozaffari, N.; Mirzaei, A. Patterns of work-related stress and their predictors among emergency department nurses and emergency medical services staff in a time of crisis: A latent profile analysis. BMC Nurs. 2023, 22, 98. [Google Scholar] [CrossRef] [PubMed]
- Stratman, E.G.; Boutilier, J.J.; Albert, L.A. Uncertainty in Facility Location Models for Emergency Medical Services. In Uncertainty in Facility Location Problems; Springer: Berlin/Heidelberg, Germany, 2023; pp. 213–250. [Google Scholar]
- Lerner, E.B.; Weik, T.; Edgerton, E.A. Research in prehospital care: Overcoming the barriers to success. Prehospital Emerg. Care 2016, 20, 448–453. [Google Scholar] [CrossRef]
- Kim, J.H. Data integration using information and communication technology for emergency medical services and systems. Clin. Exp. Emerg. Med. 2023, 10, 129–131. [Google Scholar] [CrossRef]
- Sandman, L.; Nordmark, A. Ethical conflicts in prehospital emergency care. Nurs. Ethics 2006, 13, 592–607. [Google Scholar] [CrossRef] [PubMed]
- Moscati, R. Protection of human subjects in prehospital research. Prehospital Emerg. Care 2002, 6 (Suppl. 2), S18–S23. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.T.; Spivey, W.H. A retrospective analysis of institutional review board and informed consent practices in EMS research. Ann. Emerg. Med. 1994, 23, 70–74. [Google Scholar] [CrossRef]
- Jensen, A.S.R.; Valentin, J.B.; Mulvad, M.G.; Hagenau, V.H.V.; Skaarup, S.H.; Johnsen, S.P.; VæggemoseGude, U.; Gude, M.F. Standard vs. Targeted Oxygen Therapy Prehospitally for Chronic Obstructive Pulmonary Disease (STOP-COPD); study protocol for a randomised controlled trial. Res. Square 2023. [Google Scholar]
- Saver, J.L.; Kidwell, C.; Eckstein, M.; Ovbiagele, B.; Starkman, S. Physician-investigator phone elicitation of consent in the field: A novel method to obtain explicit informed consent for prehospital clinical research. Prehospital Emerg. Care 2006, 10, 182–185. [Google Scholar] [CrossRef]
- Abelsson, A.; Lindwall, L. What is dignity in prehospital emergency care? Nurs. Ethics 2017, 24, 268–278. [Google Scholar] [CrossRef]
- Roule, V.; Ardouin, P.; Blanchart, K.; Lemaitre, A.; Wain-Hobson, J.; Legallois, D.; Beygui, F. Prehospital fibrinolysis versus primary percutaneous coronary intervention in ST-elevation myocardial infarction: A systematic review and meta-analysis of randomized controlled trials. Crit. Care 2016, 20, 359. [Google Scholar] [CrossRef]
- Boersma, E. Does time matter? A pooled analysis of randomized clinical trials comparing primary percutaneous coronary intervention and in-hospital fibrinolysis in acute myocardial infarction patients. Eur. Heart J. 2006, 27, 779–788. [Google Scholar] [CrossRef] [PubMed]
- Van der Velden, M.W.A.; Ringburg, A.N.; Bergs, E.A.; Steyerberg, E.W.; Patka, P.; Schipper, I.B. Prehospital interventions: Time wasted or time saved? An observational cohort study of management in initial trauma care. Emerg. Med. J. 2008, 25, 444–449. [Google Scholar] [CrossRef] [PubMed]
- Pedley, D.K.; Bissett, K.; Connolly, E.M.; Goodman, C.G.; Golding, I.; Pringle, T.H.; Jones, M.C. Prospective observational cohort study of time saved by prehospital thrombolysis for ST elevation myocardial infarction delivered by paramedics. BMJ 2003, 327, 22–26. [Google Scholar] [CrossRef] [PubMed]
- Fladt, J.; Ospel, J.M.; Singh, N.; Saver, J.L.; Fisher, M.; Goyal, M. Optimizing Patient-Centered Stroke Care and Research in the Prehospital Setting. Stroke 2023, 54, 2453–2460. [Google Scholar] [CrossRef]
- Cimino, J.; Braun, C. Design a Clinical Research Protocol: Influence of Real-World Setting. Healthcare 2023, 11, 2254. [Google Scholar] [CrossRef]
- Jarvis, S.; Salottolo, K.; Berg, G.M.; Carrick, M.; Caiafa, R.; Hamilton, D.; Banton, K.; Lieser, M.; Bar-Or, D. Examining emergency medical services’ prehospital transport times for trauma patients during COVID-19. Am. J. Emerg. Med. 2021, 44, 33–37. [Google Scholar] [CrossRef]
- Sucov, A.; Verdile, V.P.; Garettson, D.; Paris, P.M. The outcome of patients refusing prehospital transportation. Prehospital Disaster Med. 1992, 7, 365–371. [Google Scholar] [CrossRef]
- Wallace, D.J.; Kahn, J.M.; Angus, D.C.; Martin-Gill, C.; Callaway, C.W.; Rea, T.D.; Chhatwal, J.; Kurland, K.; Seymour, C.W. Accuracy of prehospital transport time estimation. Acad. Emerg. Med. 2014, 21, 9–16. [Google Scholar] [CrossRef]
- Quake, S.Y.L.; Khoda, F.; Arjomandi Rad, A.; Subbiah Ponniah, H.; Vardanyan, R.; Frisoni, P.; Arjomandi Rad, H.; Brasesco, M.; Mustoe, S.; Godfrey, J.; et al. The current status and challenges of prehospital trauma care in low-and middle-income countries: A systematic review. Prehospital Emerg. Care 2023, 1–11. [Google Scholar] [CrossRef]
- Jamshidi, H.; Jazani, R.K.; Khani Jeihooni, A.; Alibabaei, A.; Alamdari, S.; Kalyani, M.N. Facilitators and barriers to collaboration between pre-hospital emergency and emergency department in traffic accidents: A qualitative study. BMC Emerg. Med. 2023, 23, 58. [Google Scholar] [CrossRef] [PubMed]
- Drayna, P.C.; Browne, L.R.; Guse, C.E.; Brousseau, D.C.; Lerner, E.B. Prehospital pediatric care: Opportunities for training, treatment, and research. Prehospital Emerg. Care 2015, 19, 441–447. [Google Scholar] [CrossRef]
- Kim, H.; Kim, S.W.; Park, E.; Kim, J.H.; Chang, H. The role of fifth-generation mobile technology in prehospital emergency care: An opportunity to support paramedics. Health Policy Technol. 2020, 9, 109–114. [Google Scholar] [CrossRef]
- Ångerman, S.; Kirves, H.; Nurmi, J. Multifaceted implementation and sustainability of a protocol for prehospital anaesthesia: A retrospective analysis of 2115 patients from helicopter emergency medical services. Scand. J. Trauma Resusc. Emerg. Med. 2023, 31, 21. [Google Scholar] [CrossRef] [PubMed]
- McManamny, T.; Ortega, M.; Munro, S.; Jennings, P.; Whitley, G.A. A pre-hospital mixed methods systematic review protocol. Br. Paramed. J. 2023, 8, 38–43. [Google Scholar] [CrossRef]
- Finn, Z.; Carter, P.; Rogers, D.; Burnett, A. Prehospital COVID-19-Related Encounters Predict Future Hospital Utilization. Prehospital Emerg. Care 2023, 27, 297–302. [Google Scholar] [CrossRef]
- Li, T.; Koloden, D.; Berkowitz, J.; Luo, D.; Luan, H.; Gilley, C.; Kurgansky, G.; Barbara, P. Prehospital transport and termination of resuscitation of cardiac arrest patients: A review of prehospital care protocols in the United States. Resusc. Plus 2023, 14, 100397. [Google Scholar] [CrossRef]
- Rottman, S.J.; Schriger, D.L.; Charlop, G.; Salas, J.H.; Lee, S. On-line medical control versus protocol-based prehospital care. Ann. Emerg. Med. 1997, 30, 62–68. [Google Scholar] [CrossRef]
- Holstein, A.; Plaschke, A.; Vogel, M.Y.; Egberts, E.H. Prehospital management of diabetic emergencies—A population-based intervention study. Acta Anaesthesiol. Scand. 2003, 47, 610–615. [Google Scholar] [CrossRef]
- Watts, D.D.; Hanfling, D.; Waller, M.A.; Gilmore, C.; Fakhry, S.M.; Trask, A.L. An evaluation of the use of guidelines in prehospital management of brain injury. Prehospital Emerg. Care 2004, 8, 254–261. [Google Scholar] [CrossRef]
- Combes, X.; Jabre, P.; Jbeili, C.; Leroux, B.; Bastuji-Garin, S.; Margenet, A.; Adnet, F.; Dhonneur, G. Prehospital standardization of medical airway management: Incidence and risk factors of difficult airway. Acad. Emerg. Med. 2006, 13, 828–834. [Google Scholar] [CrossRef]
- Sasson, C.; Forman, J.; Krass, D.; Macy, M.; Hegg, A.J.; McNally, B.F.; Kellermann, A.L. A qualitative study to understand barriers to implementation of national guidelines for prehospital termination of unsuccessful resuscitation efforts. Prehospital Emerg. Care 2010, 14, 250–258. [Google Scholar] [CrossRef]
- Atary, J.Z.; de Visser, M.; van den Dijk, R.; Bosch, J.; Liem, S.S.; Antoni, M.L.; Bootsma, M.; Viergever, E.P.; Kirchhof, C.J.; Padmos, I.; et al. Standardised pre-hospital care of acute myocardial infarction patients: MISSION! guidelines applied in practice. Neth. Heart J. 2010, 18, 408–415. [Google Scholar] [CrossRef]
- Rognås, L.; Hansen, T.M.; Kirkegaard, H.; Tønnesen, E. Standard operating procedure changed pre-hospital critical care anaesthesiologists’ behaviour: A quality control study. Scand. J. Trauma Resusc. Emerg. Med. 2013, 21, 84. [Google Scholar] [CrossRef][Green Version]
- Brandler, E.S.; Sharma, M.; McCullough, F.; Ben-Eli, D.; Kaufman, B.; Khandelwal, P.; Helzner, E.; Sinert, R.H.; Levine, S.R. Prehospital stroke identification: Factors associated with diagnostic accuracy. J. Stroke Cerebrovasc. Dis. 2015, 24, 2161–2166. [Google Scholar] [CrossRef] [PubMed]
- Osborne, A.; Taylor, L.; Reuber, M.; Grünewald, R.A.; Parkinson, M.; Dickson, J.M. Pre-hospital care after a seizure: Evidence base and United Kingdom management guidelines. Seizure 2015, 24, 82–87. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kerner, T.; Schmidbauer, W.; Tietz, M.; Marung, H.; Genzwuerker, H.V. Use of checklists improves the quality and safety of prehospital emergency care. Eur. J. Emerg. Med. 2017, 24, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Lenssen, N.; Krockauer, A.; Beckers, S.K.; Rossaint, R.; Hirsch, F.; Brokmann, J.C.; Bergrath, S. Quality of analgesia in physician-operated telemedical prehospital emergency care is comparable to physician-based prehospital care-a retrospective longitudinal study. Sci. Rep. 2017, 7, 1536. [Google Scholar] [CrossRef]
- Pride, G.L.; Fraser, J.F.; Gupta, R.; Alberts, M.J.; Rutledge, J.N.; Fowler, R.; Ansari, S.; Abruzzo, T.; Albani, B.; Jayaraman, M.V.; et al. Prehospital care delivery and triage of stroke with emergent large vessel occlusion (ELVO): Report of the Standards and Guidelines Committee of the Society of Neurointerventional Surgery. J. Neurointerv. Surg. 2017, 9, 802–812. [Google Scholar] [CrossRef]
- Martín-Rodríguez, F.; López-Izquierdo, R.; Mohedano-Moriano, A.; Polonio-López, B.; Maestre Miquel, C.; Viñuela, A.; Durantez Fernandez, C.; Correas, J.; Marques, G.; Martín-Conty, J.L. Identification of serious adverse events in patients with traumatic brain injuries, from prehospital care to Intensive-Care Unit, using Early Warning Scores. Int. J. Environ. Res. Public Health 2020, 17, 1504. [Google Scholar] [CrossRef]
- Johnson, M.; O’Hara, R.; Hirst, E.; Weyman, A.; Turner, J.; Mason, S.; Siriwardena, A.N. Multiple triangulation and collaborative research using qualitative methods to explore decision making in pre-hospital emergency care. BMC Med. Res. Methodol. 2017, 17, 11. [Google Scholar] [CrossRef] [PubMed]
- Oanesa, R.D.; Su, T.W.-H.; Weissman, A. Evidence for Use of Validated Sepsis Screening Tools in the Prehospital Population: A Scoping Review. Prehospital Emerg. Care 2023, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Tuerxun, K.; Eklund, D.; Wallgren, U.; Dannenberg, K.; Repsilber, D.; Kruse, R.; Särndahl, E.; Kurland, L. Predicting sepsis using a combination of clinical information and molecular immune markers sampled in the ambulance. Sci. Rep. 2023, 13, 14917. [Google Scholar] [CrossRef] [PubMed]
- Janerka, C.; Leslie, G.D.; Mellan, M.; Arendts, G. Prehospital telehealth for emergency care: A scoping review. Emerg. Med. Australas. 2023, 35, 540–552. [Google Scholar] [CrossRef]
- Jaeger, L.R.; McCartin, M.P.; Haamid, A.; Weber, J.M.; Tataris, K.L. TeleEMS: An EMS Telemedicine Pilot Program Barriers to Implementation: (Preliminary Investigation). Prehospital Emerg. Care 2023, 1–6. [Google Scholar] [CrossRef]
- Katz, B.S.; McMullan, J.T.; Sucharew, H.; Adeoye, O.; Broderick, J.P. Design and validation of a prehospital scale to predict stroke severity: Cincinnati Prehospital Stroke Severity Scale. Stroke 2015, 46, 1508–1512. [Google Scholar] [CrossRef]
- Weerts, J.O.; Schier, L.; Schmidt, H.; Kreinest, M. Review of existing measurement tools to assess spinal motion during prehospital immobilization. Eur. J. Emerg. Med. 2018, 25, 161–168. [Google Scholar] [CrossRef]
- Wu, X.; Dunne, R.; Yu, Z.; Shi, W. STREMS: A smart real-time solution toward enhancing EMS prehospital quality. In Proceedings of the 2017 IEEE/ACM International Conference on Connected Health: Applications, Systems and Engineering Technologies (CHASE), Philadelphia, PA, USA, 17–19 July 2017; pp. 365–372. [Google Scholar]
- Brown, N. Should the Kendrick Extrication Device have a place in pre-hospital care? J. Paramed. Pract. 2015, 7, 300–304. [Google Scholar] [CrossRef]
- Ayub, E.M.; Sampayo, E.M.; Shah, M.I.; Doughty, C.B. Prehospital providers’ perceptions on providing patient and family centered care. Prehospital Emerg. Care 2017, 21, 233–241. [Google Scholar] [CrossRef]
- Farcas, A.M.; Zaidi, H.Q.; Wleklinski, N.P.; Tataris, K.L. Implementing a Patient Tracking System in a Large EMS System. Prehospital Emerg. Care 2022, 26, 305–310. [Google Scholar] [CrossRef]
- Denecke, K.; Meier, L.; Bauer, J.G.; Bender, M.; Lueg, C. Information capturing in pre-hospital emergency medical settings (EMS). Stud. Health Technol. Inform. 2020, 270, 613–617. [Google Scholar] [PubMed]
- Davidson, T.J.; Waxenegger, H.; Mohamed, I.; McConnell, D.S.; Sanderson, P.M. SPECTRa: An Online Tool for Simulating Prehospital Patient Care. HERD Health Environ. Res. Des. J. 2022, 15, 375–394. [Google Scholar] [CrossRef]
- Walsh, K.B. Non-invasive sensor technology for prehospital stroke diagnosis: Current status and future directions. Int. J. Stroke 2019, 14, 592–602. [Google Scholar] [CrossRef]
- Amaral, C.B.; Ralston, D.C.; Becker, T.K. Prehospital point-of-care ultrasound: A transformative technology. SAGE Open Med. 2020, 8, 2050312120932706. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, M.A.; Hanna, N.; Rodrigo, M.E.; Satler, L.F.; Waksman, R. Reliability of prehospital real-time cellular video phone in assessing the simplified National Institutes of Health Stroke Scale in patients with acute stroke: A novel telemedicine technology. Stroke 2011, 42, 1522–1527. [Google Scholar] [CrossRef]
- Ahmad, M.; Page, M.; Goodsman, D. What is simulation-based medical education (SBME) debriefing in prehospital medicine? A qualitative, ethnographic study exploring SBME debriefing in prehospital medical education. BMC Med. Educ. 2023, 23, 625. [Google Scholar] [CrossRef]
- Lowrie, L.N.; Duncan, L.; Samuels, D.A.; Ablah, E.; Ofei-Dodoo, S. Prehospital Clinical Decision-Making for Medication Administration for Behavioral Emergencies. Kans. J. Med. 2023, 16, 189. [Google Scholar] [CrossRef]
- Kang, D.Y.; Cho, K.J.; Kwon, O.; Kwon, J.M.; Jeon, K.H.; Park, H.; Lee, Y.; Park, J.; Oh, B.H. Artificial intelligence algorithm to predict the need for critical care in prehospital emergency medical services. Scand. J. Trauma Resusc. Emerg. Med. 2020, 28, 17. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; You, S.; So, S.; Lee, J.; Yook, S.; Jang, D.P.; Young Kim, I.; Park, E.; Cho, K.; Park, H.K.; et al. A data-driven artificial intelligence model for remote triage in the prehospital environment. PLoS ONE 2018, 13, e0206006. [Google Scholar] [CrossRef]
- Simionescu, C.; Insuratelu, M.; Herscovici, R. Prehospital cerebrovascular accident detection using artificial intelligence powered mobile devices. Procedia Comput. Sci. 2020, 176, 2773–2782. [Google Scholar] [CrossRef]
- Koceska, N.; Komadina, R.; Simjanoska, M.; Koteska, B.; Strahovnik, A.; Jošt, A.; Maček, R.; Madevska-Bogdanova, A.; Trajkovik, V.; Tasič, J.F.; et al. Mobile wireless monitoring system for prehospital emergency care. Euro. J. Trauma Emerg. Surg. 2020, 46, 1301–1308. [Google Scholar] [CrossRef]
- Spangler, D.; Hermansson, T.; Smekal, D.; Blomberg, H. A validation of machine learning-based risk scores in the prehospital setting. PLoS ONE 2019, 14, e0226518. [Google Scholar] [CrossRef] [PubMed]
- Carlson, J.N.; Das, S.; De la Torre, F.; Frisch, A.; Guyette, F.X.; Hodgins, J.K.; Yealy, D.M. A novel artificial intelligence system for endotracheal intubation. Prehospital Emerg. Care 2016, 20, 667–671. [Google Scholar] [CrossRef] [PubMed]
- Hasan, M.; Bath, P.A.; Marincowitz, C.; Sutton, L.; Pilbery, R.; Hopfgartner, F.; Mazumdar, S.; Campbell, R.; Stone, T.; Goodacre, S.; et al. Pre-hospital prediction of adverse outcomes in patients with suspected COVID-19: Development, application and comparison of machine learning and deep learning methods. Comput. Biol. Med. 2022, 151, 106024. [Google Scholar] [CrossRef]
- Choi, A.; Kim, M.J.; Sung, J.M.; Kim, S.; Lee, J.; Hyun, H.; Kim, H.C.; Kim, J.H.; Chang, H.J. Development of Prediction Models for Acute Myocardial Infarction at Prehospital Stage with Machine Learning Based on a Nationwide Database. J. Cardiovasc. Dev. Dis. 2022, 9, 430. [Google Scholar] [CrossRef]
- Desai, M.D.; Tootooni, M.S.; Bobay, K.L. Can Prehospital Data Improve Early Identification of Sepsis in Emergency Department? An Integrative Review of Machine Learning Approaches. Appl. Clin. Inform. 2022, 13, 189–202. [Google Scholar] [CrossRef]
- Abe, D.; Inaji, M.; Hase, T.; Takahashi, S.; Sakai, R.; Ayabe, F.; Tanaka, Y.; Otomo, Y.; Maehara, T. A prehospital triage system to detect traumatic intracranial hemorrhage using machine learning algorithms. JAMA Netw. Open 2022, 5, e2216393. [Google Scholar] [CrossRef]
- Liu, N.T.; Holcomb, J.B.; Wade, C.E.; Batchinsky, A.I.; Cancio, L.C.; Darrah, M.I.; Salinas, J. Development and validation of a machine learning algorithm and hybrid system to predict the need for life-saving interventions in trauma patients. Med. Biol. Eng. Comput. 2014, 52, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Desautels, T.; Calvert, J.; Hoffman, J.; Jay, M.; Kerem, Y.; Shieh, L.; Shimabukuro, D.; Chettipally, U.; Feldman, M.; Das, R.; et al. Prediction of sepsis in the intensive care unit with minimal electronic health record data: A machine learning approach. JMIR Med. Inform. 2016, 4, e5909. [Google Scholar] [CrossRef]
- Cheng, C.Y.; Chiu, I.M.; Hsu, M.Y.; Pan, H.Y.; Tsai, C.M.; Lin, C.H.R. Deep learning assisted detection of abdominal free fluid in Morison’s pouch during focused assessment with sonography in trauma. Front. Med. 2021, 8, 707437. [Google Scholar] [CrossRef]
- Fontanellaz, M.; Ebner, L.; Huber, A.; Peters, A.; Löbelenz, L.; Hourscht, C.; Klaus, J.; Munz, J.; Ruder, T.; Christe, A.; et al. A deep-learning diagnostic support system for the detection of COVID-19 using chest radiographs: A multireader validation study. Investig. Radiol. 2021, 56, 348–356. [Google Scholar] [CrossRef]
- Uchida, K.; Kouno, J.; Yoshimura, S.; Kinjo, N.; Sakakibara, F.; Araki, H.; Morimoto, T. Development of Machine Learning Models to Predict Probabilities and Types of Stroke at Prehospital Stage: The Japan Urgent Stroke Triage Score Using Machine Learning (JUST-ML). Transl. Stroke Res. 2021, 13, 370–381. [Google Scholar] [CrossRef] [PubMed]
- Shahi, N.; Shahi, A.K.; Phillips, R.; Shirek, G.; Bensard, D.; Moulton, S.L. Decision-making in pediatric blunt solid organ injury: A deep learning approach to predict massive transfusion, need for operative management, and mortality risk. J. Pediatr. Surg. 2021, 56, 379–384. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.W.; Wang, Y.C.; Liu, M.H.; Tsai, B.Y.; Wu, M.Y.; Hsieh, P.H.; Wei, J.-T.; Shi, E.; Shiao, Y.-T.; Chang, K.C.; et al. Artificial intelligence-assisted remote detection of ST-elevation myocardial infarction using a mini-12-lead electrocardiogram device in prehospital ambulance care. Front. Cardiovasc. Med. 2022, 9, 1001982. [Google Scholar] [CrossRef] [PubMed]
| Findings | Target Population | Study Design |
|---|---|---|
| Cummins et al. (1985) examined the records of 1297 people with witnessed out-of-hospital cardiac arrest caused by heart disease and treated by both emergency medical technicians (EMTs) and paramedics, to determine early cardiopulmonary resuscitation (CPR) improved survival [28]. | Cardiac arrest patients | Observational |
| Bickell et al. (1994) found that prehospital intravenous fluid replacement therapy improved survival in hypotensive trauma patients, highlighting the importance of aggressive fluid resuscitation in this population [29]. | Hypotensive trauma patients | Prospective cohort |
| Sampalis et al. (1999) showed that tertiary trauma centers and reduced prehospital times are the essential components of an efficient trauma care system [30]. | Traumatic injury patients | Prospective cohort |
| Gausche et al. (2000) found that out-of-hospital pediatric endotracheal intubation did not improve survival or neurological outcomes compared to bag–mask ventilation, highlighting the challenges of airway management in pediatric patients [31]. | Endotracheal intubation in pediatric patients | Controlled clinical trial |
| Davis et al. (2005) found that prehospital oxygen therapy did not improve mortality in severe traumatic brain injury patients, challenging the previous standard of care [32]. | Brain injury patients | Retrospective registry |
| Richard et al. (2006) shed light on the management and outcomes of pediatric patients transported by EMS in a Canadian prehospital system. Through an analysis of a prospective cohort, the research provides valuable insights into the characteristics, interventions, and outcomes of pediatric patients in the prehospital setting [33]. | Pediatric emergency medicine | Prospective cohort |
| Ortolani et al. (2007) demonstrated the significant benefit of prehospital triage in identifying patients with cardiogenic shock complicating ST-elevation myocardial infarction (STEMI) who would benefit from primary percutaneous coronary intervention (PCI). The results indicate that patients who received prehospital triage had a significantly lower mortality rate compared to those who did not undergo prehospital triage. Furthermore, the study reveals that prehospital triage was associated with a higher likelihood of achieving optimal revascularization [34]. | Prehospital cardiogenic shock | Prospective registry |
| Kragh et al. (2009) evaluated the use of tourniquets in trauma patients in war areas. The study found that tourniquet use when shock was absent was strongly associated with saved lives, and prehospital use was also strongly associated with life-saving outcomes [35]. | Traumatic injury patients | Prospective survey |
| Nassif et al. (2009) found that prehospital protocol change for asthmatic children is associated with shorter total hospital and total care times. This protocol change was also associated with decreased hospitalization rates and less need for critical care in those hospitalized. Further study is necessary to determine if other factors also contributed. [36]. | Children with minor head trauma | Prospective cohort |
| Dracup et al. (2009) demonstrated the effectiveness of a targeted educational intervention in reducing prehospital delay to treatment in acute coronary syndrome (ACS) patients. The study emphasizes the importance of patient education and empowerment in promoting timely medical care-seeking behavior. The findings suggest that interventions aimed at improving symptom recognition, knowledge of ACS symptoms, and overcoming barriers can contribute to better outcomes for ACS patients by facilitating early access to appropriate treatments [37]. | Acute coronary syndrome patients | Randomized clinical trial |
| Bergs et al. (2010) demonstrated the feasibility and reliability of prehospital stroke scales in the Belgian prehospital setting. The results indicate that EMS personnel were able to effectively administer and interpret the stroke scales, leading to accurate identification and triage of potential stroke patients. The study also reveals a high level of inter-rater reliability among EMS providers in using the stroke scales [38]. | Stroke patients | Prospective cohort |
| Monsieurs et al. (2012) showed an association between higher compression rates and lower compression depths. Avoiding excessive compression rates may lead to more compressions of sufficient depth [39]. | Myocardial infarction patients | Observational |
| Meretoja et al. (2012) found that the implementation of a prehospital stroke protocol by emergency medical services improved stroke outcomes, emphasizing the importance of early recognition and treatment of stroke symptoms [40]. | Stroke patients | Observational |
| Brown et al. (2015) found that prehospital blood product transfusion improved mortality and functional outcomes in trauma patients during medical evacuation, highlighting the potential benefits of this intervention [41]. | Traumatic injury patients | Retrospective cohort |
| Lockey et al. (2015) found that prehospital advanced life support improved outcomes for major trauma patients, highlighting the importance of early and effective interventions in this population [42]. | Major trauma patients | Prospective observational |
| Crewdson et al. (2017) conducted a systematic review and meta-analysis and found that prehospital rapid sequence intubation was associated with improved outcomes for trauma patients, highlighting the importance of effective airway management in this population [43]. | Injury patients | Systematic review and meta-analysis |
| Wang et al. (2018) compared the effectiveness of two methods of airway management in adults with out-of-hospital cardiac arrest: laryngeal tube (LT) and endotracheal intubation (ETI). Based on these findings, the authors concluded that initial LT insertion may be considered as an alternative to ETI for airway management in adults with out-of-hospital cardiac arrest [44]. | Cardiac arrest patients | Randomized clinical trial |
| Guyette et al. (2021) found that prehospital administration of tranexamic acid after injury did not result in a higher incidence of thrombotic complications or adverse events. Tranexamic acid given to injured patients at risk for hemorrhage in the prehospital setting is safe and associated with survival benefit in specific subgroups of patients [45]. | Trauma patients with hypovolemic shock | Randomized clinical trial |
| Scquizzato et al. (2023) demonstrated that adults with acute respiratory failure treated in the prehospital setting with noninvasive ventilation had a lower risk of intubation than those managed with standard oxygen therapy, with similar risk of death, intensive care admission, and length of hospital stay. [46]. | Prehospital respiratory failure | Retrospective cohort |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cimino, J.; Braun, C. Clinical Research in Prehospital Care: Current and Future Challenges. Clin. Pract. 2023, 13, 1266-1285. https://doi.org/10.3390/clinpract13050114
Cimino J, Braun C. Clinical Research in Prehospital Care: Current and Future Challenges. Clinics and Practice. 2023; 13(5):1266-1285. https://doi.org/10.3390/clinpract13050114
Chicago/Turabian StyleCimino, Jonathan, and Claude Braun. 2023. "Clinical Research in Prehospital Care: Current and Future Challenges" Clinics and Practice 13, no. 5: 1266-1285. https://doi.org/10.3390/clinpract13050114
APA StyleCimino, J., & Braun, C. (2023). Clinical Research in Prehospital Care: Current and Future Challenges. Clinics and Practice, 13(5), 1266-1285. https://doi.org/10.3390/clinpract13050114





