Effects of an Intensive 6-Week Rehabilitation Program with the HUBER Platform in the Treatment of Non-Specific Chronic Low Back Pain: A Pilot Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Measurements
2.3. Rehabilitation Program
2.4. Research Plan/Design
2.5. Statistical Analysis
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Knezevic, N.N.; Candido, K.D.; Vlaeyen, J.W.S.; Van Zundert, J.; Cohen, S.P. Low back pain. Lancet 2021, 398, 78–92. [Google Scholar] [CrossRef]
- Maher, C.; Underwood, M.; Buchbinder, R. Non-specific low back pain. Lancet 2017, 389, 736–747. [Google Scholar] [CrossRef] [Green Version]
- DePalma, M.J.; Ketchum, J.M.; Saullo, T. What is the source of chronic low back pain and does age play a role? Pain Med. 2011, 12, 224–233. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hartvigsen, J.; Hancock, M.J.; Kongsted, A.; Louw, Q.; Ferreira, M.L.; Genevay, S.; Hoy, D.; Karppinen, J.; Pransky, G.; Sieper, J.; et al. What low back pain is and why we need to pay attention. Lancet 2018, 391, 2356–2367. [Google Scholar] [CrossRef] [Green Version]
- Cho, K.H.; Beom, J.W.; Lee, T.S.; Lim, J.H.; Lee, T.H.; Yuk, J.H. Trunk muscles strength as a risk factor for nonspecific low back pain: A pilot study. Ann. Rehabil. Med. 2014, 38, 234–240. [Google Scholar] [CrossRef] [Green Version]
- Radebold, A.; Cholewicki, J.; Panjabi, M.M.; Patel, T.C. Muscle response pattern to sudden trunk loading in healthy individuals and in patients with chronic low back pain. Spine 2000, 25, 947–954. [Google Scholar] [CrossRef]
- Hancock, M.J.; Maher, C.G.; Latimer, J.; Spindler, M.F.; McAuley, J.H.; Laslett, M.; Bogduk, N. Systematic review of tests to identify the disc, SIJ or facet joint as the source of low back pain. Eur. Spine J. 2007, 16, 1539–1550. [Google Scholar] [CrossRef] [Green Version]
- O’Sullivan, P. It’s time for change with the management of non-specific chronic low back pain. Br. J. Sports Med. 2012, 46, 224–227. [Google Scholar] [CrossRef] [Green Version]
- Hayden, J.A.; Ellis, J.; Ogilvie, R.; Malmivaara, A.; van Tulder, M.W. Exercise therapy for chronic low back pain. Cochrane Database Syst. Rev. 2021, 9, CD009790. [Google Scholar] [CrossRef]
- Foster, N.E.; Anema, J.R.; Cherkin, D.; Chou, R.; Cohen, S.P.; Gross, D.P.; Ferreira, P.H.; Fritz, J.M.; Koes, B.W.; Peul, W.; et al. Prevention and treatment of low back pain: Evidence, challenges, and promising directions. Lancet 2018, 391, 2368–2383. [Google Scholar] [CrossRef]
- Hayden, J.A.; Ellis, J.; Ogilvie, R.; Stewart, S.A.; Bagg, M.K.; Stanojevic, S.; Yamato, T.P.; Saragiotto, B.T. Some types of exercise are more effective than others in people with chronic low back pain: A network meta-analysis. J. Physiother 2021, 67, 252–262. [Google Scholar] [CrossRef] [PubMed]
- Hayden, J.A.; van Tulder, M.W.; Malmivaara, A.; Koes, B.W. Exercise therapy for treatment of non-specific low back pain. Cochrane Database Syst. Rev. 2005, CD000335. [Google Scholar] [CrossRef] [PubMed]
- Verbrugghe, J.; Agten, A.; Stevens, S.; Hansen, D.; Demoulin, C.B.O.E.; Vandenabeele, F.; Timmermans, A. Exercise Intensity Matters in Chronic Nonspecific Low Back Pain Rehabilitation. Med. Sci. Sports Exerc. 2019, 51, 2434–2442. [Google Scholar] [CrossRef] [PubMed]
- Couillandre, A.; Duque Ribeiro, M.J.; Thoumie, P.; Portero, P. Changes in balance and strength parameters induced by training on a motorised rotating platform: A study on healthy subjects. Ann. Readapt. Med. Phys. 2008, 51, 59–73. [Google Scholar] [CrossRef] [PubMed]
- Fabre, J.B.; Martin, V.; Borelli, G.; Fritsch, N.; Theurel, J. Effects of a whole-body strength training program on metabolic responses and body composition. Gazz. Med. Ital. Arch. Per Le Sci. Med. 2014, 173, 47–56. [Google Scholar]
- Markovic, G.; Sarabon, N.; Greblo, Z.; Krizanic, V. Effects of feedback-based balance and core resistance training vs. Pilates training on balance and muscle function in older women: A randomized-controlled trial. Arch. Gerontol. Geriatr. 2015, 61, 117–123. [Google Scholar] [CrossRef]
- Greblo Jurakic, Z.; Krizanic, V.; Sarabon, N.; Markovic, G. Effects of feedback-based balance and core resistance training vs. Pilates training on cognitive functions in older women with mild cognitive impairment: A pilot randomized controlled trial. Aging Clin. Exp. Res. 2017, 29, 1295–1298. [Google Scholar] [CrossRef]
- Guiraud, T.; Labrunee, M.; Besnier, F.; Senard, J.M.; Pillard, F.; Riviere, D.; Richard, L.; Laroche, D.; Sanguignol, F.; Pathak, A.; et al. Whole-body strength training with Huber Motion Lab and traditional strength training in cardiac rehabilitation: A randomized controlled study. Ann. Phys. Rehabil. Med. 2017, 60, 20–26. [Google Scholar] [CrossRef]
- Guiraud, T.; Labrunee, M.; Pillard, F.; Granger, R.; Bousquet, M.; Richard, L.; Boned, A.; Pathak, A.; Gayda, M.; Gremeaux, V. Whole-body strength training using a Huber Motion Lab in coronary heart disease patients: Safety, tolerance, fuel selection, and energy expenditure aspects and optimization. Am. J. Phys. Med. Rehabil. 2015, 94, 385–394. [Google Scholar] [CrossRef]
- Letafatkar, A.; Nazarzadeh, M.; Hadadnezhad, M.; Farivar, N. The efficacy of a HUBER exercise system mediated sensorimotor training protocol on proprioceptive system, lumbar movement control and quality of life in patients with chronic non-specific low back pain. J. Back Musculoskelet. Rehabil. 2017, 30, 767–778. [Google Scholar] [CrossRef]
- Kim, S.; Jee, Y. Effects of 3D Moving Platform Exercise on Physiological Parameters and Pain in Patients with Chronic Low Back Pain. Medicina 2020, 56, 351. [Google Scholar] [CrossRef] [PubMed]
- Moussa, A.Z.B.; Zouita, S.B.S.F.; Salah, F.B.; Behm, D.G.; Chaouachi, A. Isokinetic Trunk Strength, Validity, Reliability, Normative Data and Relation to Physical Performance and Low Back Pain: A Review of the Literature. Int. J. Sports Phys. Ther. 2020, 15, 160–174. [Google Scholar] [CrossRef]
- Delitto, A.; Rose, S.J.; Crandell, C.E.; Strube, M.J. Reliability of isokinetic measurements of trunk muscle performance. Spine 1991, 16, 800–803. [Google Scholar] [CrossRef] [PubMed]
- Estrazulas, J.A.; Estrazulas, J.A.; de Jesus, K.; de Jesus, K.; da Silva, R.A.; Libardoni Dos Santos, J.O. Evaluation isometric and isokinetic of trunk flexor and extensor muscles with isokinetic dynamometer: A systematic review. Phys. Ther. Sport 2020, 45, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Guilhem, G.; Giroux, C.; Couturier, A.; Maffiuletti, N.A. Validity of trunk extensor and flexor torque measurements using isokinetic dynamometry. J. Electromyogr. Kinesiol. 2014, 24, 986–993. [Google Scholar] [CrossRef]
- Waddell, G.; Newton, M.; Henderson, I.; Somerville, D.; Main, C.J. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain 1993, 52, 157–168. [Google Scholar] [CrossRef]
- Fairbank, J.C.; Pynsent, P.B. The Oswestry Disability Index. Spine 2000, 25, 2940–2952; discussion 2952. [Google Scholar] [CrossRef]
- Jette, M.; Campbell, J.; Mongeon, J.; Routhier, R. The Canadian Home Fitness Test as a predictor for aerobic capacity. Can. Med. Assoc. J. 1976, 114, 680–682. [Google Scholar]
- Frizziero, A.; Pellizzon, G.; Vittadini, F.; Bigliardi, D.; Costantino, C. Efficacy of Core Stability in Non-Specific Chronic Low Back Pain. J. Funct. Morphol. Kinesiol. 2021, 6, 37. [Google Scholar] [CrossRef]
- Slade, S.C.; Keating, J.L. Trunk-strengthening exercises for chronic low back pain: A systematic review. J. Manip. Physiol. Ther. 2006, 29, 163–173. [Google Scholar] [CrossRef]
- Melo Filho, J.; Eduardo, F.M.C.; Moser, A.D.D.L. Isokinetic performance, functionality, and pain level before and after lumbar and pelvic estabilization exercise in individuals with chronic low back pain. Fisioter. Mov. 2014, 27, 447–455. [Google Scholar] [CrossRef]
- Olivier, N.; Lepretre, A.; Caby, I.; Dupuis, M.A.; Prieur, F. Does exercise therapy for chronic lower-back pain require daily isokinetic reinforcement of the trunk muscles? Ann. Readapt. Med. Phys. 2008, 51, 284–291. [Google Scholar] [CrossRef] [PubMed]
- Owen, P.J.; Miller, C.T.; Mundell, N.L.; Verswijveren, S.; Tagliaferri, S.D.; Brisby, H.; Bowe, S.J.; Belavy, D.L. Which specific modes of exercise training are most effective for treating low back pain? Network meta-analysis. Br. J. Sports Med. 2020, 54, 1279–1287. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Hoshino, Y.; Nakamura, K.; Kariya, Y.; Saita, K.; Ito, K. Trunk muscle weakness as a risk factor for low back pain. A 5-year prospective study. Spine 1999, 24, 54–57. [Google Scholar] [CrossRef] [PubMed]
- Shirado, O.; Ito, T.; Kaneda, K.; Strax, T.E. Concentric and eccentric strength of trunk muscles: Influence of test postures on strength and characteristics of patients with chronic low-back pain. Arch. Phys. Med. Rehabil. 1995, 76, 604–611. [Google Scholar] [CrossRef]
- Steele, J.; Fisher, J.; Perrin, C.; Conway, R.; Bruce-Low, S.; Smith, D. Does change in isolated lumbar extensor muscle function correlate with good clinical outcome? A secondary analysis of data on change in isolated lumbar extension strength, pain, and disability in chronic low back pain. Disabil. Rehabil. 2019, 41, 1287–1295. [Google Scholar] [CrossRef]
- Sheng, Y.; Duan, Z.; Qu, Q.; Chen, W.; Yu, B. Kinesio taping in treatment of chronic non-specific low back pain: A systematic review and meta-analysis. J. Rehabil. Med. 2019, 51, 734–740. [Google Scholar] [CrossRef] [Green Version]
- Yamato, T.P.; Maher, C.G.; Saragiotto, B.T.; Hancock, M.J.; Ostelo, R.W.; Cabral, C.M.; Menezes Costa, L.C.; Costa, L.O. Pilates for low back pain. Cochrane Database Syst. Rev. 2015, CD010265. [Google Scholar] [CrossRef]
- Saragiotto, B.T.; Maher, C.G.; Yamato, T.P.; Costa, L.O.P.; Costa, L.C.M.; Ostelo, R.; Macedo, L.G. Motor Control Exercise for Nonspecific Low Back Pain: A Cochrane Review. Spine 2016, 41, 1284–1295. [Google Scholar] [CrossRef]
- Gomes-Neto, M.; Lopes, J.M.; Conceicao, C.S.; Araujo, A.; Brasileiro, A.; Sousa, C.; Carvalho, V.O.; Arcanjo, F.L. Stabilization exercise compared to general exercises or manual therapy for the management of low back pain: A systematic review and meta-analysis. Phys. Ther. Sport 2017, 23, 136–142. [Google Scholar] [CrossRef]
- Verbrugghe, J.; Agten, A.; Stevens, S.; Hansen, D.; Demoulin, C.; Eijnde, B.O.; Vandenabeele, F.; Timmermans, A. High Intensity Training to Treat Chronic Nonspecific Low Back Pain: Effectiveness of Various Exercise Modes. J. Clin. Med. 2020, 9, 2401. [Google Scholar] [CrossRef] [PubMed]
- Borisovskaya, A.; Chmelik, E.; Karnik, A. Exercise and Chronic Pain. Adv. Exp. Med. Biol. 2020, 1228, 233–253. [Google Scholar] [CrossRef] [PubMed]
- Meints, S.M.; Wang, V.; Edwards, R.R. Sex and Race Differences in Pain Sensitization among Patients with Chronic Low Back Pain. J. Pain 2018, 19, 1461–1470. [Google Scholar] [CrossRef] [PubMed]

| HUB n = 12 | p | Cohen’s d | ||
|---|---|---|---|---|
| Pre | Post | |||
| Age | 42.92 ± 9.17 | |||
| Sex; n female (%) | 3 (25%) | |||
| Weight (kg) | 89.00 ± 23.78 | |||
| Heigh (cm) | 175.33 ± 6.85 | |||
| Body mass index (kg·m2) | 29.08 ± 8.07 | |||
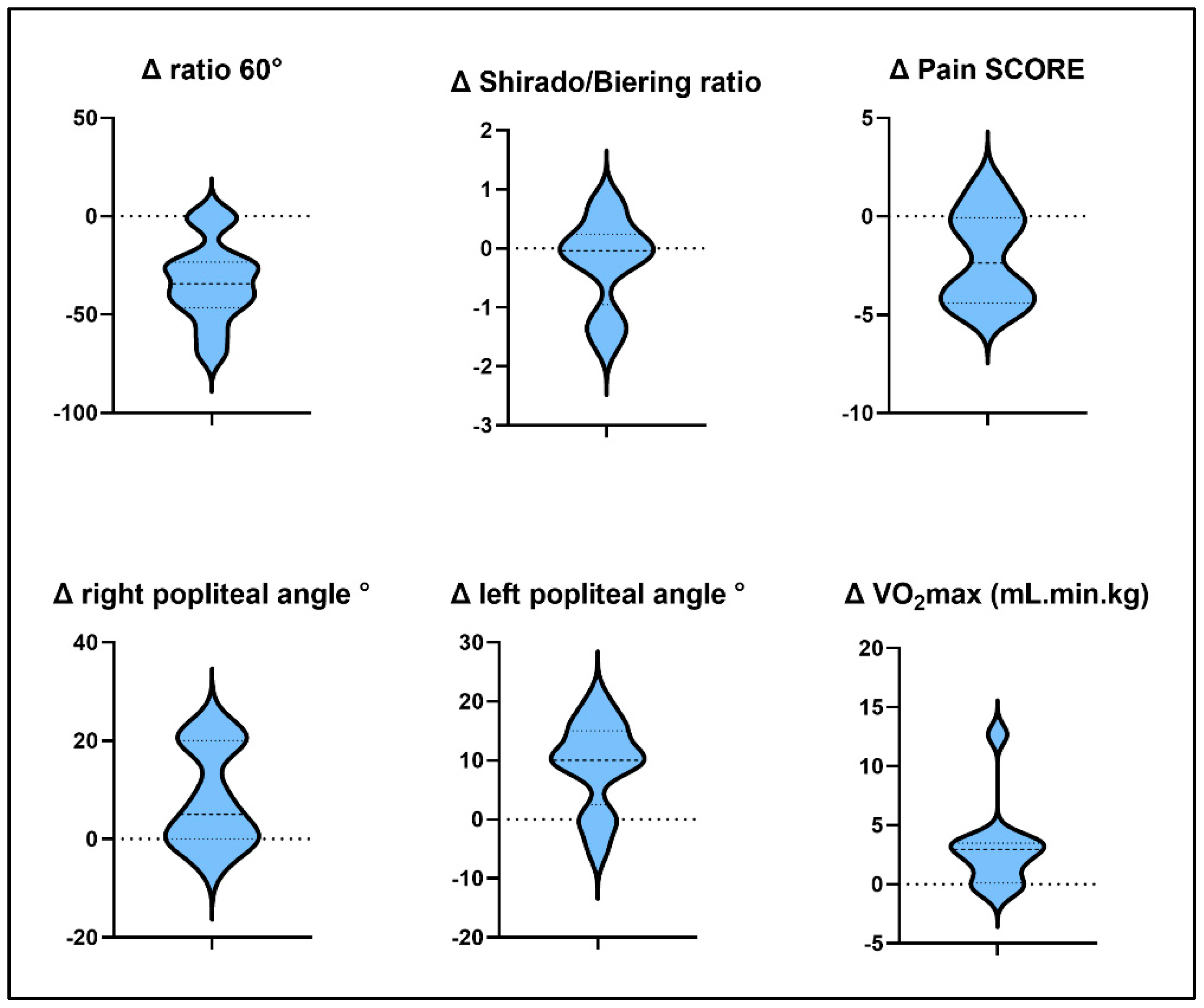
| Pain visual analog scale (/10) | 3.70 ± 1.92 | 1.65 ± 1.28 | 0.0110 | 1.26 |
| Oswestry Disability Index | 29.83 ± 9.32 | 14.00 ± 8.36 | 0.0000 | 1.79 |
| FABQ * work | 73.11 ± 18.58 | 50.63 ± 32.04 | 0.0244 | 0.86 |
| FABQ * physical activity | 54.12 ± 23.06 | 27.43 ± 15.74 | 0.0275 | 1.35 |
| Iso Fr 60 (Nm) | 197.77 ± 99.81 | 209.17 ± 64.46 | 0.1823 | 0.14 |
| Iso Exr 60 (Nm) | 209.03 ± 114.12 | 301.33 ± 99.85 | 0.0000 | 0.86 |
| Ratio 60 | 104.70 ± 25.03 | 71.25 ± 14.72 | 0.0002 | 1.63 |
| Peak Torque moy./kg 60 (Nm/kg) | 2.12 ± 0.95 | 3.27 ± 0.92 | 0.0000 | 1.24 |
| Iso Fr 120 | 177.83 ± 80.90 | 212.43 ± 82.52 | 0.0006 | 0.42 |
| Iso Exr 120 | 210.76 ± 112.48 | 267.32 ± 76.60 | 0.0149 | 0.59 |
| Ratio 120 | 89.78 ± 23.68 | 78.25 ± 11.27 | 0.1487 | 0.62 |
| Peak Torque moy./kg 120 (Nm/kg) | 2.32 ± 0.98 | 3.01 ± 0.77 | 0.0090 | 0.78 |
| VO2max (mL. kg. min) | 31.80 ± 5.00 | 34.80 ± 5.23 | 0.0076 | 0.59 |
| Lumbar mobility and flexibility | Pre | Post | p | Cohen’s d |
| Dual Inclinometry Flex° (°) | 23.33 ± 8.88 | 19.17 ± 5.57 | 0.0854 | - |
| Dual Inclinometry Ext° (°) | 18.25 ± 12.59 | 23.33 ± 13.54 | 0.147 | - |
| DI Inclination Right (°) | 14.17 ± 7.93 | 17.92 ± 6.56 | 0.095 | - |
| DI Inclination Left (°) | 14.08 ± 8.32 | 17.92 ± 5.82 | 0.1499 | - |
| Modified Thomas test Right (°) | 18.06 ± 10.58 | 13.75 ± 9.32 | 0.1485 | - |
| Modified Thomas test Left (°) | 13.89 ± 7.73 | 13.75 ± 11.10 | 0.9647 | - |
| Popliteal angle test Right (°) | 138.06 ± 11.99 | 146.25 ± 9.56 | 0.0166 | 0.76 |
| Popliteal angle test Left (°) | 136.53 ± 12.28 | 145.83 ± 8.75 | 0.0012 | 0.87 |
| Distance heel–buttocks Right (cm) | 10.67 ± 6.95 | 4.42 ± 4.03 | 0.0012 | 1.10 |
| Distance heel–buttocks Left (cm) | 9.67 ± 7.88 | 5.58 ± 4.91 | 0.0278 | 0.62 |
| Biering–Sorensen test (s) | 67.67 ± 38.49 | 113.83 ± 56.33 | 0.0102 | 0.96 |
| Shirado–Ito test (s) | 66.67 ± 37.00 | 106.33 ± 59.71 | 0.0051 | 0.80 |
| Shirado/Biering ratio | 1.28 ± 1.12 | 1.05 ± 0.64 | 0.3228 | |
| Killy test (s) | 38.50 ± 22.89 | 225.92 ± 229.21 | 0.0022 | 1.15 |
| Pharmacological treatments (number of patients concerned with each class of therapy) | ||||
| Analgesic step 1/2/3 * | 6/3/3 | 4/1/1 | ||
| Antidepressant | 2 | 2 | ||
| Antiepileptic | 1 | 1 | ||
| ACE * inhibitors | 1 | 0 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tantot, M.; Le Moal, V.; Mévellec, É.; Nouy-Trollé, I.; Lemoine-Josse, E.; Besnier, F.; Guiraud, T. Effects of an Intensive 6-Week Rehabilitation Program with the HUBER Platform in the Treatment of Non-Specific Chronic Low Back Pain: A Pilot Study. Clin. Pract. 2022, 12, 609-618. https://doi.org/10.3390/clinpract12040064
Tantot M, Le Moal V, Mévellec É, Nouy-Trollé I, Lemoine-Josse E, Besnier F, Guiraud T. Effects of an Intensive 6-Week Rehabilitation Program with the HUBER Platform in the Treatment of Non-Specific Chronic Low Back Pain: A Pilot Study. Clinics and Practice. 2022; 12(4):609-618. https://doi.org/10.3390/clinpract12040064
Chicago/Turabian StyleTantot, Mélanie, Vincent Le Moal, Éric Mévellec, Isabelle Nouy-Trollé, Emmanuelle Lemoine-Josse, Florent Besnier, and Thibaut Guiraud. 2022. "Effects of an Intensive 6-Week Rehabilitation Program with the HUBER Platform in the Treatment of Non-Specific Chronic Low Back Pain: A Pilot Study" Clinics and Practice 12, no. 4: 609-618. https://doi.org/10.3390/clinpract12040064
APA StyleTantot, M., Le Moal, V., Mévellec, É., Nouy-Trollé, I., Lemoine-Josse, E., Besnier, F., & Guiraud, T. (2022). Effects of an Intensive 6-Week Rehabilitation Program with the HUBER Platform in the Treatment of Non-Specific Chronic Low Back Pain: A Pilot Study. Clinics and Practice, 12(4), 609-618. https://doi.org/10.3390/clinpract12040064






