Blepharoconjunctivitis and Otolaryngological Disease Trends in the Context of Mask Wearing during the COVID-19 Pandemic
Abstract
:1. Introduction
2. Materials and Methods
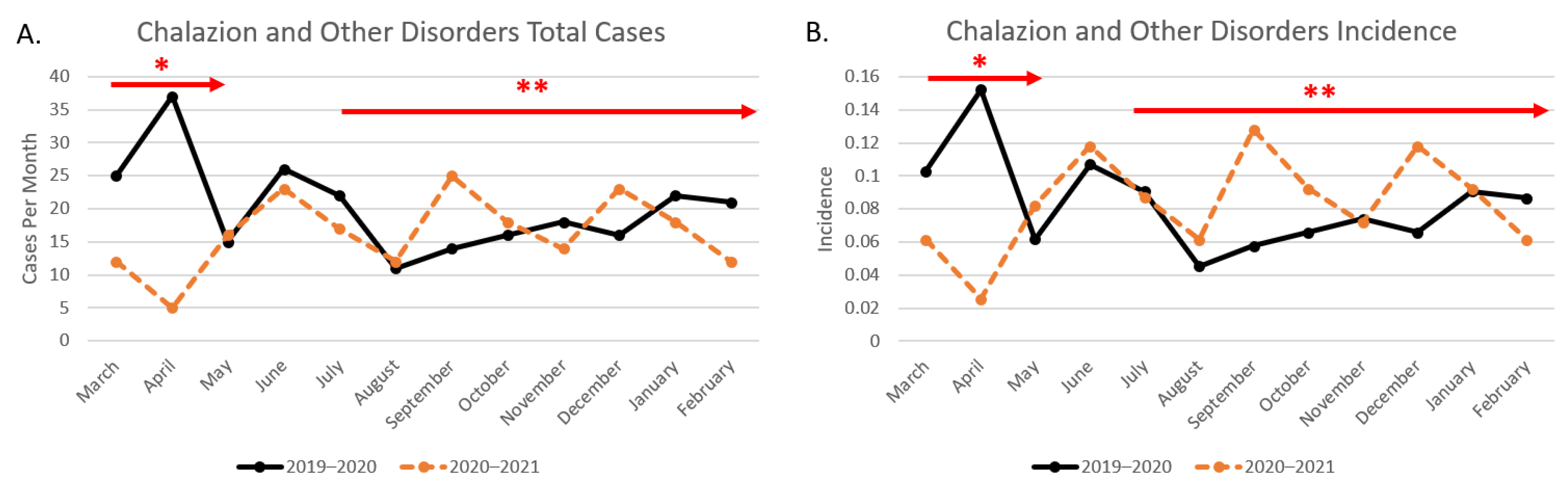
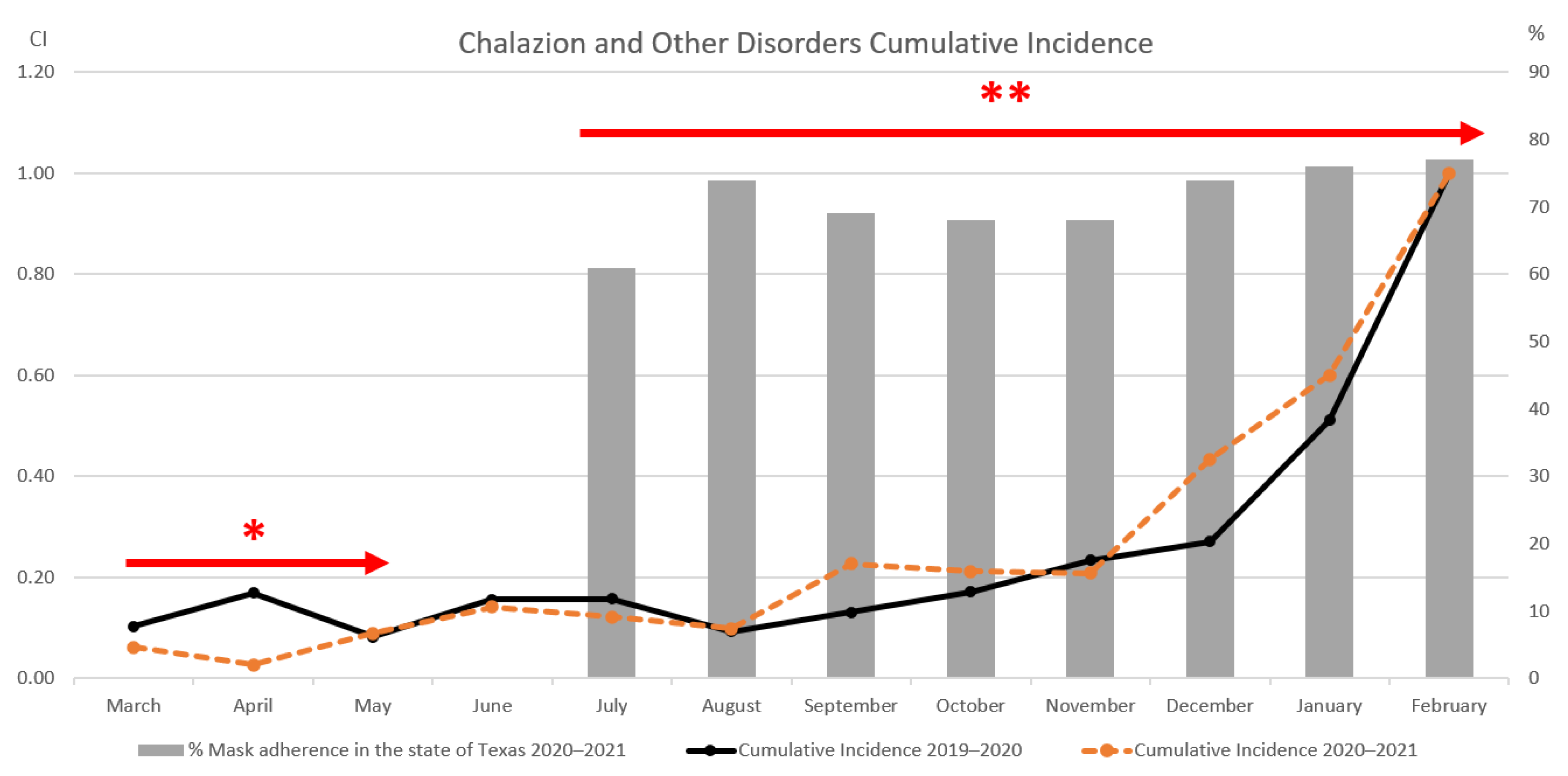
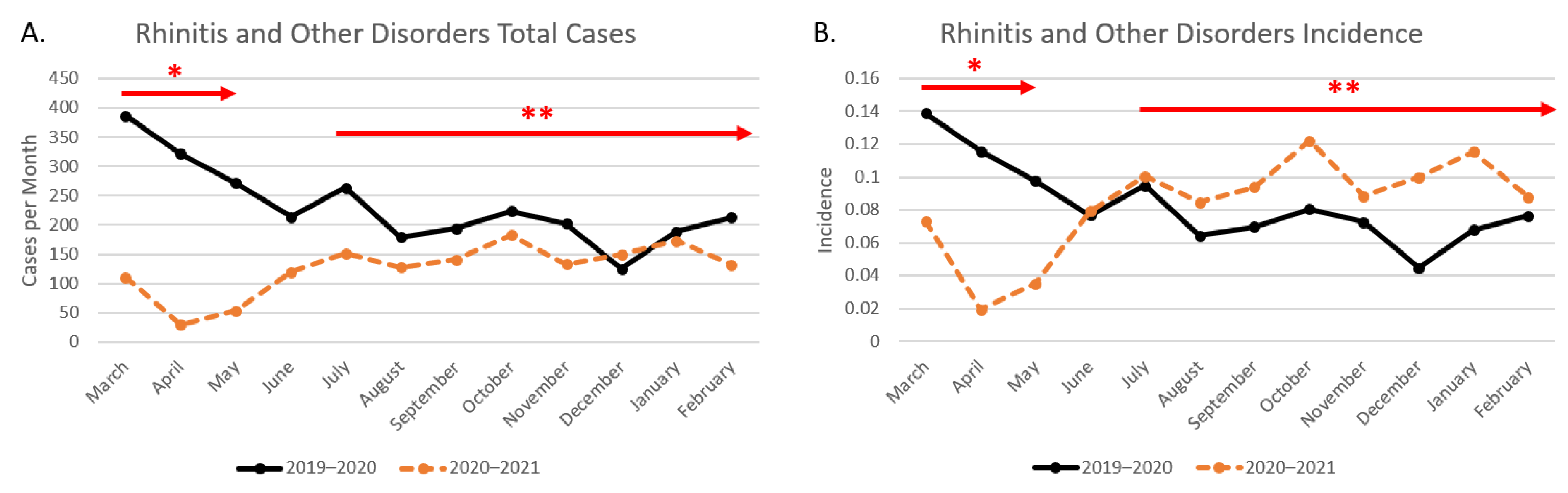
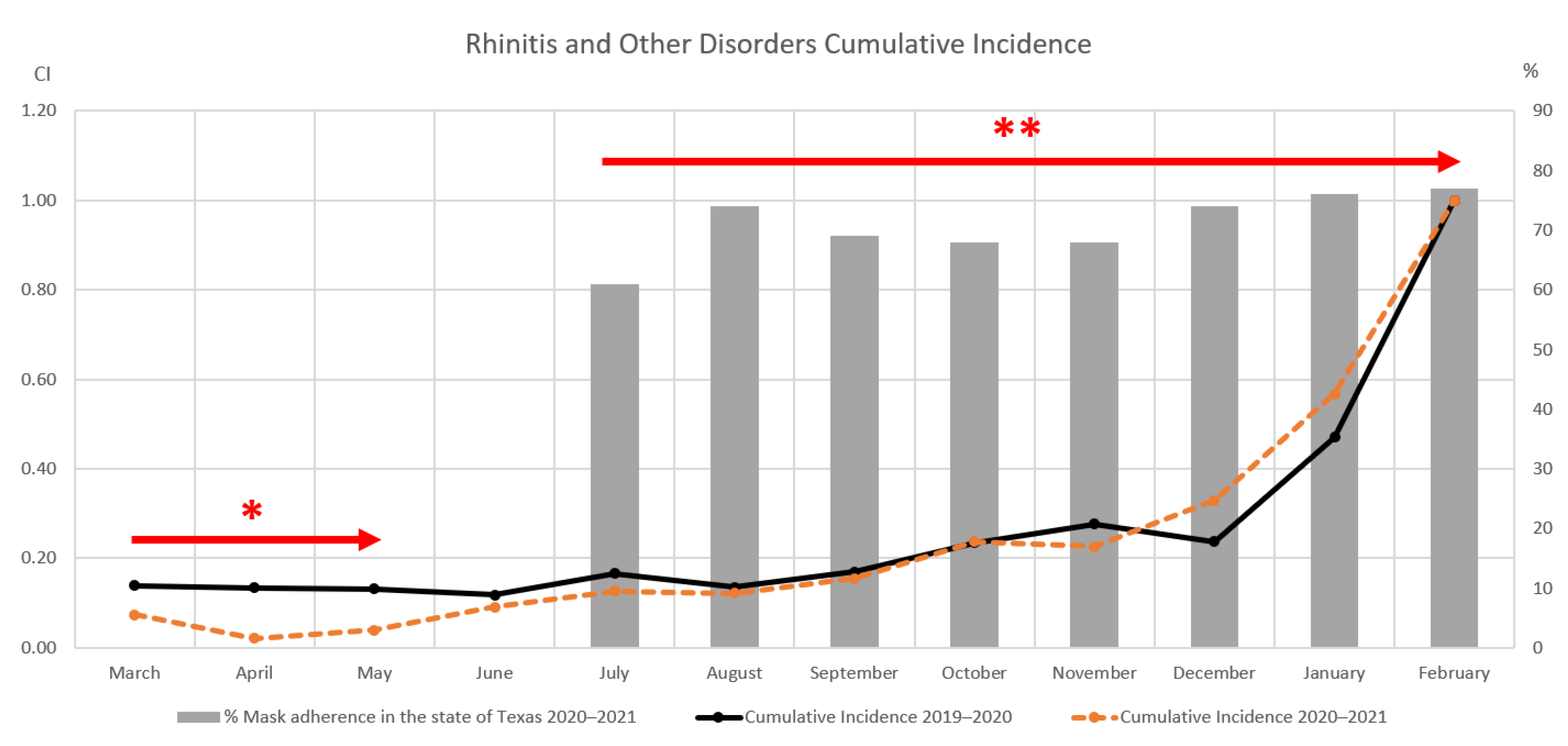
3. Results
3.1. Ophthalmology Results
Otolaryngology Results
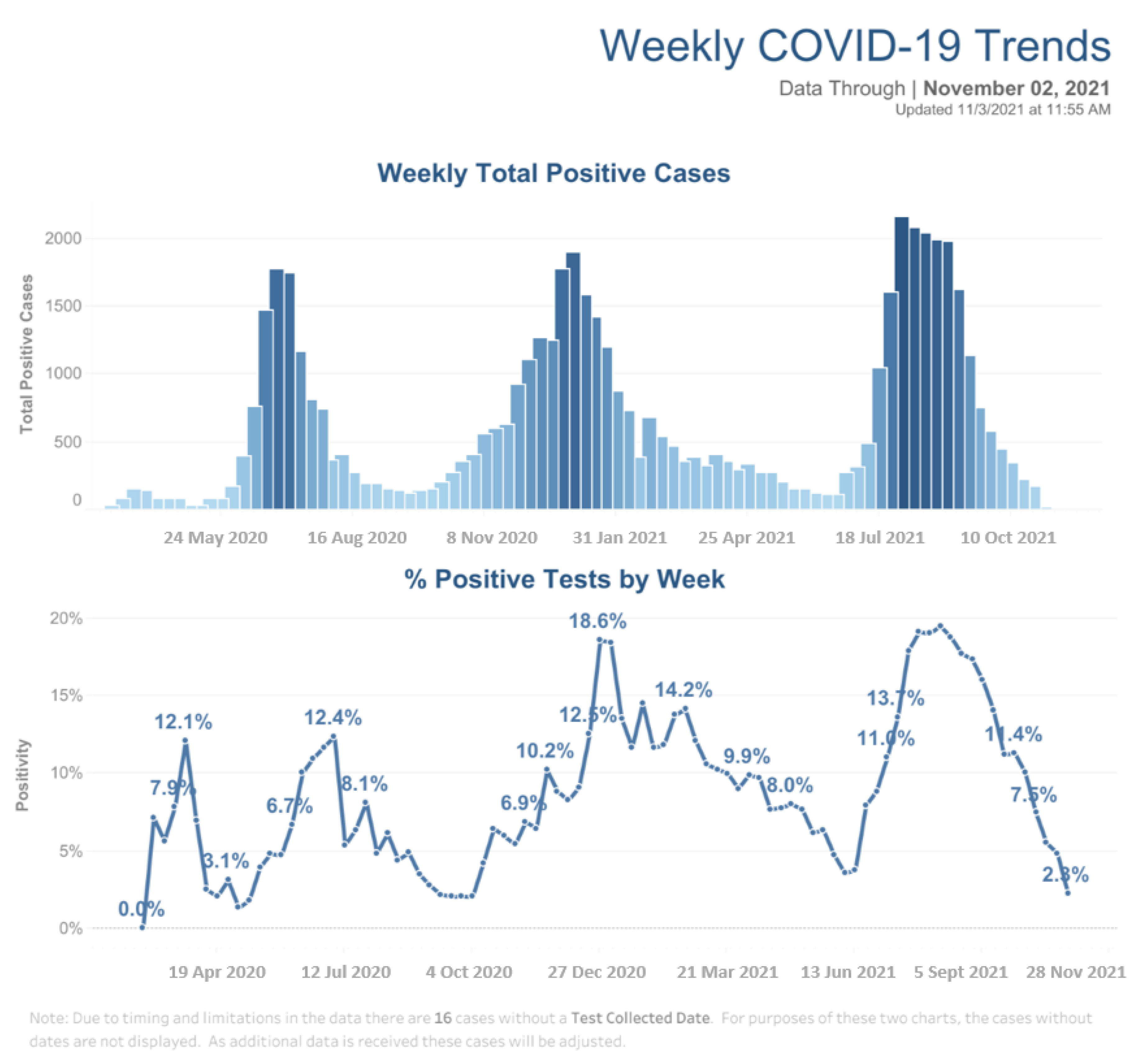
3.2. Galveston County Health District COVID-19 Data
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| COVID-19 | 2019 coronavirus disease |
| SARS-COV-2 | Severe acute respiratory syndrome coronavirus 2 |
| CDC | Center for Disease Control |
| WHO | World Health Organization |
| UTMB | University of Texas Medical Branch |
| ENT | Ears, nose, and throat |
| GCHD | Galveston County Health District |
| MDPI | Multidisciplinary Digital Publishing Institute |
| DOAJ | Directory of open access journals |
| TLA | Three letter acronym |
| LD | Linear dichroism |
References
- Office of Texas Government. Available online: https://gov.texas.gov/news/post/governor-abbott-establishes-statewide-face-covering-requirement-issues-proclamation-to-limit-gatherings (accessed on 4 April 2022).
- Ueki, H.; Furusawa, Y.; Iwatsuki-Horimoto, K.; Imai, M.; Kabata, H.; Nishimura, H.; Kawaoka, Y. Effectiveness of Face Masks in Preventing Airborne Transmission of SARS-CoV-2. mSphere 2020, 5, e00637-20. [Google Scholar] [CrossRef]
- Klimek, L.; Huppertz, T.; Alali, A.; Spielhaupter, M.; Hörmann, K.; Matthias, C.; Hagemann, J. A new form of irritant rhinitis to filtering facepiece particle (FFP) masks (FFP2/N95/KN95 respirators) during COVID-19 pandemic. World Allergy Organ J. 2020, 13, 100474. [Google Scholar] [CrossRef]
- Dror, A.A.; Eisenbach, N.; Marshak, T.; Layous, E.; Zigron, A.; Shivatzki, S.; Morozov, N.G.; Taiber, S.; Alon, E.E.; Ronen, O.; et al. Reduction of allergic rhinitis symptoms with face mask usage during the COVID-19 pandemic. J. Allergy Clin. Immunol. Pract. 2020, 8, 3590–3593. [Google Scholar] [CrossRef] [PubMed]
- Dayal, A.K.; Sinha, V. Trend of Allergic Rhinitis Post COVID-19 Pandemic: A Retrospective Observational Study. Indian J. Otolaryngol. Head Neck Surg. 2020, 20, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Silkiss, R.Z.; Paap, M.K.; Ugradar, S. Increased incidence of chalazion associated with face mask wear during the COVID-19 pandemic. Am. J. Ophthalmol. Case Rep. 2021, 22, 101032. [Google Scholar] [CrossRef]
- Moshirfar, M.; West, W.B., Jr.; Marx, D.P. Face Mask-Associated Ocular Irritation and Dryness. Ophthalmol. Ther. 2020, 9, 397–400. [Google Scholar] [CrossRef] [PubMed]
- Mégarbane, B.; Tadayoni, R. Cluster of chalazia in nurses using eye protection while caring for critically ill patients with COVID-19 in intensive care. Occup. Environ. Med. 2020, 77, 584–585. [Google Scholar] [CrossRef] [PubMed]
- Giannaccare, G.; Vaccaro, S.; Mancini, A.; Scorcia, V. Dry eye in the COVID-19 era: How the measures for controlling pandemic might harm ocular surface. Graefes Arch. Clin. Exp. Ophthalmol. 2020, 258, 2567–2568. [Google Scholar] [CrossRef] [PubMed]
- Galveston County COVID-19 Cases. Available online: https://www.gchd.org/public-health-services/covid-19/covid-19-dashboard (accessed on 2 November 2021).
- Darby, S.; Chulliyallipalil, K.; Przyjalgowski, M.; McGowan, P.; Jeffers, S.; Giltinan, A.; Lewis, L.; Smith, N.; Sleator, R.D. COVID-19: Mask efficacy is dependent on both fabric and fit. Future Microbiol. 2021, 16, 5–11. [Google Scholar] [CrossRef] [PubMed]
- Lima, M.M.S.; Cavalcante, F.M.L.; Macêdo, T.S.; Galindo Neto, N.M.; Caetano, J.Á.; Barros, L.M. Cloth face masks to prevent Covid-19 and other respiratory infections. Rev. Lat. Am. Enferm. 2020, 28, e3353. [Google Scholar] [CrossRef] [PubMed]
- Hong, N.; Yu, W.; Xia, J.; Shen, Y.; Yap, M.; Han, W. Evaluation of ocular symptoms and tropism of SARS-CoV-2 in patients confirmed with COVID-19. Acta Ophthalmol. 2020, 10, 1111. [Google Scholar] [CrossRef] [PubMed]
- Kasting, M.L.; Head, K.J.; Hartsock, J.A.; Sturm, L.; Zimet, G.D. Public perceptions of the effectiveness of recommended non-pharmaceutical intervention behaviors to mitigate the spread of SARS-CoV-2. PLoS ONE 2020, 15, e0241662. [Google Scholar] [CrossRef]
- Teasdale, E.; Santer, M.; Geraghty, A.W.; Little, P.; Yardley, L. Public perceptions of non pharmaceutical interventions for reducing transmission of respiratory infection: Systematic review and synthesis of qualitative studies. BMC Public Health 2014, 14, 589. [Google Scholar] [CrossRef]
- Al-Hasan, A.; Yim, D.; Khuntia, J. Citizens’ Adherence to COVID-19 Mitigation Recommendations by the Government: A 3-Country Comparative Evaluation Using Web-Based Cross-Sectional Survey Data. J. Med. Internet Res. 2020, 22, e20634. [Google Scholar] [CrossRef] [PubMed]
- Fischer, C.B.; Adrien, N.; Silguero, J.J.; Hopper, J.J.; Chowdhury, A.I.; Werler, M.M. Mask adherence and rate of COVID-19 across the United States. PLoS ONE 2021, 16, e0249891. [Google Scholar] [CrossRef] [PubMed]
- Prather, K.A.; Wang, C.C.; Schooley, R.T. Reducing transmission of SARS-CoV-2. Science 2020, 368, 1422–1424. [Google Scholar] [CrossRef]
- Chiu, N.C.; Chi, H.; Tai, Y.L.; Peng, C.C.; Tseng, C.Y.; Chen, C.C.; Tan, B.F.; Lin, C.Y. Impact of Wearing Masks, Hand Hygiene, and Social Distancing on Influenza, Enterovirus, and All-Cause Pneumonia During the Coronavirus Pandemic: Retrospective National Epidemiological Surveillance Study. J. Med. Internet Res. 2020, 22, e21257. [Google Scholar] [CrossRef] [PubMed]
- Rosner, E. Adverse Effects of Prolonged Mask Use among Healthcare Professionals during COVID-19. J. Infect. Dis. Epidemiol. 2020, 6, 130. [Google Scholar] [CrossRef]
- Kisielinski, K.; Giboni, P.; Prescher, A.; Klosterhalfen, B.; Graessel, D.; Funken, S.; Kempski, O.; Hirsch, O. Is a Mask That Covers the Mouth and Nose Free from Undesirable Side Effects in Everyday Use and Free of Potential Hazards? Int. J. Environ. Res. Public Health 2021, 18, 4344. [Google Scholar] [CrossRef] [PubMed]
- Gomułka, K.; Panaszek, B. Contact urticaria syndrome caused by haptens. Postepy Dermatol. Alergol. 2014, 31, 108–112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Parent ICD-10 Code | Diagnosis |
|---|---|
| H00.0 | Hordeolum |
| H00.1 | Chalazion |
| H01.0 | Blepharitis |
| H04.12 | Dry Eye |
| H10 | Conjunctivitis |
| H92.09 | Otalgia |
| J30.0 | Vasomotor Rhinitis |
| J30.9 | Allergic Rhinitis |
| J31.0 | Chronic Rhinitis |
| J34 Nasal | Irritation/Mucositis |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koshevarova, V.A.; Westenhaver, Z.K.; Schmitz-Brown, M.; McKinnon, B.J.; Merkley, K.H.; Gupta, P.K. Blepharoconjunctivitis and Otolaryngological Disease Trends in the Context of Mask Wearing during the COVID-19 Pandemic. Clin. Pract. 2022, 12, 619-627. https://doi.org/10.3390/clinpract12040065
Koshevarova VA, Westenhaver ZK, Schmitz-Brown M, McKinnon BJ, Merkley KH, Gupta PK. Blepharoconjunctivitis and Otolaryngological Disease Trends in the Context of Mask Wearing during the COVID-19 Pandemic. Clinics and Practice. 2022; 12(4):619-627. https://doi.org/10.3390/clinpract12040065
Chicago/Turabian StyleKoshevarova, Victoria A., Zack K. Westenhaver, Mary Schmitz-Brown, Brian J. McKinnon, Kevin H. Merkley, and Praveena K. Gupta. 2022. "Blepharoconjunctivitis and Otolaryngological Disease Trends in the Context of Mask Wearing during the COVID-19 Pandemic" Clinics and Practice 12, no. 4: 619-627. https://doi.org/10.3390/clinpract12040065
APA StyleKoshevarova, V. A., Westenhaver, Z. K., Schmitz-Brown, M., McKinnon, B. J., Merkley, K. H., & Gupta, P. K. (2022). Blepharoconjunctivitis and Otolaryngological Disease Trends in the Context of Mask Wearing during the COVID-19 Pandemic. Clinics and Practice, 12(4), 619-627. https://doi.org/10.3390/clinpract12040065






