Cancer Symptom Clusters in Children and Adolescents with Cancer Undergoing Chemotherapy: A Systematic Review
Abstract
1. Introduction
2. Method
2.1. Study Design
2.2. Research Question
2.3. Eligibility Criteria
2.4. Search Strategy
2.5. Screening of Articles
2.6. Data Extraction
2.7. Methodological Quality Assessment
3. Results
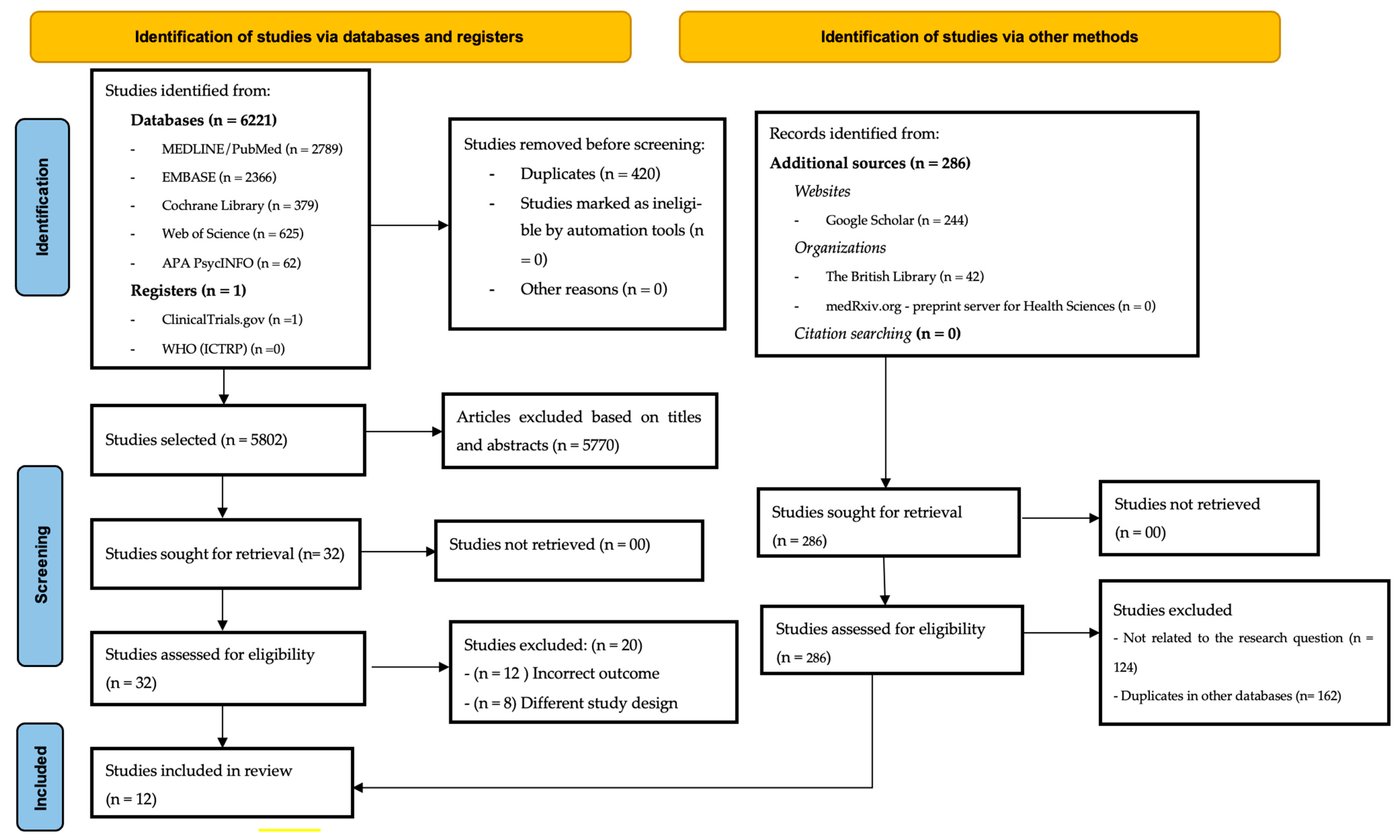
3.1. Study Selection
3.2. Characterization of Included Studies
- 1.
- Gastrointestinal Cluster
- The gastrointestinal cluster was one of the most frequently reported across multiple studies, encompassing symptoms such as nausea and vomiting (commonly associated with chemotherapy); diarrhea and constipation; taste alterations and dry mouth; and loss of appetite and weight loss. Studies by Li et al. [37,40,42], Wang et al. [41], and Atay et al. [33] emphasized the significance of this cluster, linking it to specific phases of chemotherapy and its adverse impact on quality of life.
- 2.
- Emotional and Psychosocial Cluster
- Another widely reported cluster involved emotional and psychological symptoms, including anxiety, worry, and nervousness; irritability and sadness; depression; and altered self-perception. This cluster was identified in several studies [31,33,35,37,39], highlighting the importance of psychological support throughout cancer treatment.
- 3.
- Fatigue and Sleep Disturbance Cluster
- Fatigue-related symptoms were highly prevalent, significantly affecting patients’ physical and emotional well-being. Key symptoms included severe and persistent fatigue; sleep disturbances and insomnia (or psychological stress); and reduced physical activity levels. This cluster was highlighted by Hockenberry et al. [31,35], Lopes-Júnior et al. [36,38], and Hooke et al. [39], with greater severity observed in adolescents diagnosed with solid tumors and those undergoing chemotherapy.
- 4.
- Somatic and Neurological Cluster
- This cluster comprised physical symptoms associated with cancer treatment, such as muscle pain and tingling sensations; headache and dizziness; and fever and excessive sweating. Studies by Li et al. [37,40,42], and Wang et al. [41] identified this cluster primarily in patients diagnosed with acute lymphoblastic leukemia (ALL).
- 5.
- Self-Image and Dermatological Cluster
- Several studies reported symptoms associated with treatment-related changes in physical appearance, including hair loss (alopecia); skin changes (dryness, itching); and swelling in the extremities. This cluster was reported by Li et al. [37,40,42], and Atay et al. [33], emphasizing the psychosocial impact of self-image alterations on pediatric oncology patients.
3.3. Internal Validity of Included Studies
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public Involvement Statement:
Guidelines and Standards Statement:
Use of Artificial Intelligence:
Conflicts of Interest
References
- Wu, Y.; Deng, Y.; Wei, B.; Xiang, D.; Hu, J.; Zhao, P.; Lin, S.; Zheng, Y.; Yao, J.; Zhai, Z.; et al. Global burden of childhood cancer in 2019 and its annualized change in rates from 1990 to 2019. J. Adv. Res. 2022, 40, 233–247. [Google Scholar] [CrossRef] [PubMed]
- Organización Mundial de la Salud. WHO Global Initiative for Childhood with Cancer: An Overview. [Internet] Ginebra: OMS. 2020. [Cited 14 August 2023]. Available online: https://www.who.int/docs/default-source/documents/health-topics/cancer/who-childhood-cancer-overview-booklet.pdf (accessed on 15 February 2025).
- Organización Panamericana de la Salud (OPAS). La Práctica de la Enfermería Oncológica Pediátrica en América Latina y el Caribe; OPAS: Washington, DC, USA, 2022. [Google Scholar]
- Lima, R.A.G.; Lopes-Júnior, L.C.; Maia, E.B.S.; Fuentes-Alabi, S.; Ponce, M.L.V. Global Initiative for Childhood Cancer Control: Increasing access, improving quality, saving lives. Rev. Lat. Am. Enfermagem. 2023, 31, e3998. [Google Scholar] [CrossRef] [PubMed]
- Magrath, I.; Steliarova-Foucher, E.; Epelman, S.; Ribeiro, R.C.; Harif, M.; Li, C.K.; Kebudi, R.; Macfarlane, S.D.; Howard, S.C. Paediatric cancer in low-income and middle-income countries. Lancet Oncol. 2013, 14, e104–e116. [Google Scholar] [CrossRef] [PubMed]
- Day, S.; Challinor, J.; Hollis, R.; Abramovitz, L.; Hanaratri, Y.; Punjwani, R. Paediatric Oncology Nursing Care in Low-And Middle-Income Countries: A Need for Baseline Standards. [Cited 14 May 2023]. Cancer Control [Internet]. 2015, pp. 111–116. Available online: http://www.cancercontrol.info/wp-content/uploads/2015/07/111-116-Day_cc2015.pdf (accessed on 30 January 2025).
- Rodgers, C.C.; Hooke, M.C.; Taylor, O.A.; Koerner, K.M.; Mitby, P.A.; Moore, I.M.; Scheurer, M.E.; Hockenberry, M.J.; Pan, W. Childhood Cancer Symptom Cluster: Leukemia and Health-Related Quality of Life. Oncol. Nurs. Forum. 2019, 46, 228–237. [Google Scholar] [CrossRef]
- Kelley, K.W.; Bluthé, R.M.; Dantzer, R.; Zhou, J.H.; Shen, W.H.; Johnson, R.W.; Broussard, S.R. Cytokine-induced sickness behavior. Brain Behav. Immun. 2003, 17 (Suppl. S1), S112–S118. [Google Scholar] [CrossRef]
- Bhatia, S.; Landier, W. Symptom Clusters in Childhood Cancer Survivors. J. Clin. Oncol. 2023, 41, 439–442. [Google Scholar] [CrossRef]
- Dodd, M.J.; Miaskowski, C.; Lee, K.A. Occurrence of symptom clusters. J. Natl. Cancer Inst. Monogr. 2004, 2004, 76–78. [Google Scholar] [CrossRef]
- Kim, H.J.; Barsevick, A.M.; Fang, C.Y.; Miaskowski, C. Common biological pathways underlying the psychoneurological symptom cluster in cancer patients. Cancer Nurs. 2012, 35, E1–E20. [Google Scholar] [CrossRef]
- Kent, S.; Bluthé, R.M.; Kelley, K.W.; Dantzer, R. Sickness behavior as a new target for drug development. Trends Pharmacol. Sci. 1992, 13, 24–28. [Google Scholar] [CrossRef]
- Dantzer, R.; Meagher, M.W.; Cleeland, C.S. Translational approaches to treatment-induced symptoms in cancer patients. Nat. Rev. Clin. Oncol. 2012, 9, 414–426. [Google Scholar] [CrossRef]
- Rodgers, C.; Hooke, M.C.; Ward, J.; Linder, L.A. Symptom clusters in children and adolescents with cancer. Semin. Oncol. Nurs. 2016, 32, 394–404. [Google Scholar] [CrossRef]
- Dong, S.T.; Butow, P.N.; Costa, D.S.; Lovell, M.R.; Agar, M. Symptom clusters in patients with advanced cancer: A systematic review of observational studies. J. Pain. Symptom Manag. 2014, 48, 411–450. [Google Scholar] [CrossRef] [PubMed]
- Harris, C.S.; Kober, K.M.; Conley, Y.P.; Dhruva, A.A.; Hammer, M.J.; Miaskowski, C.A. Symptom clusters in patients receiving chemotherapy: A systematic review. BMJ Support. Palliat. Care 2022, 12, 10–21. [Google Scholar] [CrossRef] [PubMed]
- Silva, R.J.G.; Grippa, W.R.; Pessanha, R.M.; Marcarini, J.A.C.; Silva Neto, L.C.B.; D’Agostini, N.S.; Lopes-Júnior, L.C. Cancer symptom cluster in hospitalized women with breast cancer: A descriptive observational study. Rev. Bras. Enferm. 2025, 78, e20240091. [Google Scholar] [CrossRef] [PubMed]
- Kamkhoad, D.; Judge Santacroce, S.; Phonyiam, R.; Wang, M. Symptom Clusters That Included Gastrointestinal Symptoms Among Children Receiving Cancer Treatments: A Scoping Review. Oncol. Nurs. Forum. 2023, 50, 381–395. [Google Scholar] [CrossRef]
- Tomlinson, D.; Tigelaar, L.; Hyslop, S.; Lazor, T.; Dupuis, L.L.; Griener, K.; Oliveria, J.; Sung, L. Self-report of symptoms in children with cancer younger than 8 years of age: A systematic review. Support. Care Cancer 2017, 25, 2663–2670. [Google Scholar] [CrossRef]
- Erickson, J.M.; Macpherson, C.F.; Ameringer, S.; Baggott, C.; Linder, L.; Stegenga, K. Symptoms and symptom clusters in adolescents receiving cancer treatment: A review of the literature. Int. J. Nurs. Stud. 2013, 50, 847–869. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Grassi, J.; Freitas, M.B.; Trigo, F.E.S.; Nunes, K.Z.; Lopes-Júnior, L.C. Cancer symptom clusters in pediatric patients with cancer undergoing chemotherapy: Systematic review protocol. RSD 2023, 12, e22912240188. [Google Scholar] [CrossRef]
- Methley, A.M.; Campbell, S.; Chew-Graham, C.; McNally, R.; Cheraghi-Sohi, S. PICO, PICOS and SPIDER: A comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv. Res. 2014, 14, 579. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [PubMed]
- Lopes-Júnior, L.C.; Bomfim, E.; Olson, K.; Neves, E.T.; Silveira, D.S.C.; Nunes, M.D.R.; Nascimento, L.C.; Pereira-Da-Silva, G.; Lima, R.A.G. Effectiveness of hospital clowns for symptom management in paediatrics: Systematic review of randomised and non-randomised controlled trials. BMJ 2020, 371, m4290. [Google Scholar] [CrossRef] [PubMed]
- Lopes-Júnior, L.C.; Ferrarini, T.; Pires, L.B.C.; Rodrigues, J.G.; Salaroli, L.B.; Nunes, K.Z. Cancer symptom clusters in adult patients undergoing chemotherapy: A systematic review and meta-analysis protocol. PLoS ONE 2022, 17, e0273411. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions Version 6.5 (Updated August 2024); Cochrane: London, UK, 2024; Available online: www.training.cochrane.org/handbook (accessed on 1 April 2025).
- Centre for Evidence-Based Medicine. 2020 [Internet]. The Centre for Evidence-Based Medicine. [Cited 14 August 2023]. Available online: http://www.cebm.net (accessed on 1 April 2025).
- Sterne, J.A.C.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed]
- Joanna Briggs Institute. Critical Appraisal Tools—JBI [Internet]. Joannabriggs.org. 2017 [Cited 14 August 2023]. Available online: https://jbi.global/critical-appraisal-tools (accessed on 13 March 2025).
- Hockenberry, M.J.; Hooke, M.C.; Gregurich, M.; McCarthy, K.; Sambuco, G.; Krull, K. Symptom clusters in children and adolescents receiving cisplatin, doxorubicin, or ifosfamide. Oncol. Nurs. Forum. 2010, 37, E16–E27. [Google Scholar] [CrossRef]
- Atay, S. Symptom characteristics and clustering in children and adolescents undergoing or being off cancer chemotherapy. J. BUON 2011, 16, 751–758. [Google Scholar] [PubMed]
- Atay, S.; Conk, Z.; Bahar, Z. Identifying symptom clusters in paediatric cancer patients using the Memorial Symptom Assessment Scale. Eur. J. Cancer Care 2012, 21, 460–468. [Google Scholar] [CrossRef]
- Baggott, C.; Cooper, B.A.; Marina, N.; Matthay, K.K.; Miaskowski, C. Symptom cluster analyses based on symptom occurrence and severity ratings among pediatric oncology patients during myelosuppressive chemotherapy. Cancer Nurs. 2012, 35, 19–28. [Google Scholar] [CrossRef]
- Hockenberry, M.J.; Hooke, M.C.; McCarthy, K.; Gregurich, M.A. Sickness behavior clustering in children with cancer. J. Pediatr. Oncol. Nurs. 2011, 28, 263–272. [Google Scholar] [CrossRef]
- Lopes-Junior, L.C.; Pereira-Da-Silva, G.; Silveira, D.S.C.; Veronez, L.C.; Santos, J.C.; Alonso, J.B.; Lima, R.A.G. The Effect of clown intervention on self-report and biomarker measures of stress and fatigue in pediatric osteosarcoma inpatients: A pilot study. Integr. Cancer Ther. 2018, 17, 928–940. [Google Scholar] [CrossRef]
- Li, R.; Ma, J.; Chan, Y.; Yang, Q.; Zhang, C. Symptom Clusters and Influencing Factors in Children With Acute Leukemia During Chemotherapy. Cancer Nurs. 2020, 43, 411–418. [Google Scholar] [CrossRef] [PubMed]
- Lopes-Junior, L.C.; Silveira, D.S.C.; Olson, K.; Bomfim, E.O.; Veronez, L.C.; Santos, J.C.; Alonso, J.B.; Nascimento, L.C.; Pereira-Da-Silva, G.; Lima, R.A.G. Clown intervention on psychological stress and fatigue in pediatric patients with cancer undergoing chemotherapy. Cancer Nurs. 2020, 43, 290–299. [Google Scholar] [CrossRef] [PubMed]
- Hooke, M.C.P.; Mathiason, M.A.; Blommer, A.B.; Hutter, J.B.; Mitby, P.; Taylor, O.; Scheurer, M.E.; Kunin-Batson, A.S.; Pan, W.; Hockenberry, M.J.P. Symptom clusters, physical activity, and quality of life. Cancer Nurs. 2022, 45, 113–119. [Google Scholar] [CrossRef]
- Li, R.M.; Yao, W.M.; Chan, Y.M.; Shen, M.M.; Wang, X.M.; Wen, F.M.; Yang, Q.M. Correlation between symptom clusters and quality of life in children with acute leukemia during chemotherapy. Cancer Nurs. 2022, 45, 96–104. [Google Scholar] [CrossRef]
- Wang, Y.; Xie, H.; Jiang, H.; Chen, M.; Ren, L.; Dong, C. Analyzing the symptom clusters among children with acute lymphoblastic leukemia during chemotherapy based on electronic nursing records. Cancer Nurs. 2025, 48, 138–146. [Google Scholar] [CrossRef]
- Li, R.; Shen, X.M.; Yang, Q.M.; Zhang, L.M.; Li, H.; Yao, W.M.; Chan, Y.M. Stability of symptom clusters in children with acute lymphoblastic leukemia undergoing chemotherapy. Cancer Nurs. 2024, 47, 48–59. [Google Scholar] [CrossRef]
- Hockenberry-Eaton, M.; Hinds, P.S. Fatigue in children and adolescents with cancer: Evolution of a program of study. Semin. Oncol. Nurs. 2000, 16, 261–272; discussion 272–278. [Google Scholar] [CrossRef]
- Thong, M.S.Y.; van Noorden, C.J.F.; Steindorf, K.; Arndt, V. Cancer-Related Fatigue: Causes and Current Treatment Options. Curr. Treat. Options Oncol. 2020, 21, 17. [Google Scholar] [CrossRef]
- Al Maqbali, M. Cancer-related fatigue: An overview. Br. J. Nurs. 2021, 30, S36–S43. [Google Scholar] [CrossRef]
- Levesque, A.; Caru, M.; Duval, M.; Laverdière, C.; Sultan, S. Contributors to cancer-related fatigue in childhood cancer survivors and the use of non-pharmacological interventions: A scoping review protocol. JBI Evid. Synth. 2021, 19, 2423–2433. [Google Scholar] [CrossRef]
- Kelada, L.; Wakefield, C.; Heathcote, L.; Jaaniste, T.; Signorelli, C.; Fardell, J.; Donoghoe, M.; McCarthy, M.; Gabriel, M.; Cohn, R. Perceived cancer-related pain and fatigue, information needs, and fear of cancer recurrence among adult survivors of childhood cancer. Patient Educ. Couns. 2019, 102, 2270–2278. [Google Scholar] [CrossRef] [PubMed]
- Fabi, A.; Bhargava, R.; Fatigoni, S.; Guglielmo, M.; Horneber, M.; Roila, F.; Weis, J.; Jordan, K.; Ripamonti, C.I.; ESMO Guidelines Committee. Cancer-related fatigue: ESMO Clinical Practice Guidelines for diagnosis and treatment. Ann. Oncol. 2020, 31, 713–723. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; He, B.; Jiang, M.; Yang, Y.; Wang, C.; Huang, C.; Han, L. Prevalence and risk factors of cancer-related fatigue: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2020, 111, 103707. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y.E.; Yoon, J.H.; Park, N.H.; Ahn, Y.C.; Lee, E.J.; Son, C.G. Prevalence of cancer-related fatigue based on severity: A systematic review and meta-analysis. Sci. Rep. 2023, 13, 12815. [Google Scholar] [CrossRef]
- Kestler, S.A.; LoBiondo-Wood, G. Review of symptom experiences in children and adolescents with cancer. Cancer Nurs. 2012, 35, E31–E49. [Google Scholar] [CrossRef]
- Nowe, E.; Stöbel-Richter, Y.; Sender, A.; Leuteritz, K.; Friedrich, M.; Geue, K. Cancer-related fatigue in adolescents and young adults: A systematic review of the literature. Crit. Rev. Oncol. Hematol. 2017, 118, 63–69. [Google Scholar] [CrossRef]
- Spathis, A.; Booth, S.; Grove, S.; Hatcher, H.; Kuhn, I.; Barclay, S. Teenage and Young Adult Cancer-Related Fatigue Is Prevalent, Distressing, and Neglected: It Is Time to Intervene. A Systematic Literature Review and Narrative Synthesis. J. Adolesc. Young Adult Oncol. 2015, 4, 3–17. [Google Scholar] [CrossRef]
- Tomlinson, D.; Zupanec, S.; Jones, H.; O’Sullivan, C.; Hesser, T.; Sung, L. The lived experience of fatigue in children and adolescents with cancer: A systematic review. Support. Care Cancer 2016, 24, 3623–3631. [Google Scholar] [CrossRef]
- Hooke, M.C.; Linder, L.A. Symptoms in Children Receiving Treatment for Cancer-Part I: Fatigue, Sleep Disturbance, and Nausea/Vomiting. J. Pediatr. Oncol. Nurs. 2019, 36, 244–261. [Google Scholar] [CrossRef]
- Antill Keener, T. Childhood Cancer-Related Fatigue and Day-to-Day Quality of Life. J. Pediatr. Oncol. Nurs. 2019, 36, 74–85. [Google Scholar] [CrossRef]
- Dsilva, F.; Singh, P.; Javeth, A. Determinants of Cancer-Related Fatigue among Cancer Patients: A Systematic Review. J. Palliat. Care 2023, 38, 432–455. [Google Scholar] [CrossRef] [PubMed]
- Wang, A.B.; Housley, S.N.; Flores, A.M.; Kircher, S.M.; Perreault, E.J.; Cope, T.C. A review of movement disorders in chemotherapy-induced neurotoxicity. J. Neuroeng. Rehabil. 2021, 18, 16. [Google Scholar] [CrossRef] [PubMed]
- Vichaya, E.G.; Chiu, G.S.; Ekrukowski, K.; Lacourt, T.E.; Ekavelaars, A.; Dantzer, R.; Heijnen, C.J.; Walker, A.K. Mechanisms of chemotherapy-induced behavioral toxicities. Front. Neurosci. 2015, 9, 131. [Google Scholar] [CrossRef] [PubMed]
- Stubbs, B.; Vancampfort, D.; Veronese, N.; Kahl, K.G.; Mitchell, A.J.; Lin, P.-Y.; Tseng, P.-T.; Mugisha, J.; Solmi, M.; Carvalho, A.F.; et al. Depression and physical health multimorbidity: Primary data and country-wide meta-analysis of population data from 190 593 people across 43 low- and middle-income countries. Psychol. Med. 2017, 47, 2107–2117. [Google Scholar] [CrossRef]
- Hartung, T.; Brähler, E.; Faller, H.; Härter, M.; Hinz, A.; Johansen, C.; Keller, M.; Koch, U.; Schulz, H.; Weis, J.; et al. The risk of being depressed is significantly higher in cancer patients than in the general population: Prevalence and severity of depressive symptoms across major cancer types. Eur. J. Cancer 2017, 72, 46–53. [Google Scholar] [CrossRef]
- Yardeni, M.; Campino, G.A.; Hasson-Ohayon, I.; Basel, D.; Hertz-Palmor, N.; Bursztyn, S.; Weisman, H.; Pessach, I.M.; Toren, A.; Gothelf, D. Trajectories and risk factors for anxiety and depression in children and adolescents with cancer: A 1-year follow-up. Cancer Med. 2021, 10, 5653–5660. [Google Scholar] [CrossRef]
- Lazor, T.; Pole, J.D.; De Souza, C.; Schechter, T.; Grant, R.; Davis, H.; Duong, N.; Stein, E.; Cook, S.; Tigelaar, L.; et al. Severity, change over time, and risk factors of anxiety in children with cancer depend on anxiety instrument used. Psychooncology 2019, 28, 710–717. [Google Scholar] [CrossRef]
- Riedl, D.; Schüßler, G. Factors associated with and risk factors for depression in cancer patients—A systematic literature review. Transl. Oncol. 2022, 16, 101328. [Google Scholar] [CrossRef]
- Daniel, L.C.; Aggarwal, R.; Schwartz, L.A. Sleep in Adolescents and Young Adults in the Year After Cancer Treatment. J. Adolesc. Young Adult Oncol. 2017, 6, 560–567. [Google Scholar] [CrossRef]
- Tucker, P.; Loew, M.; Russell, K.; Tynes, B.L.; Mandrell, B.N.; Witcraft, S.M.; Schwartz, L.E.; Crabtree, V.M. Sleep health behaviors in pediatric patients with newly diagnosed cancer. J. Psychosom. Res. 2023, 172, 111413. [Google Scholar] [CrossRef]
- Sheikh, I.N.; Roth, M.; Stavinoha, P.L. Prevalence of Sleep Disturbances in Pediatric Cancer Patients and Their Diagnosis and Management. Children 2021, 8, 1100. [Google Scholar] [CrossRef] [PubMed]
- Clanton, N.R.; Klosky, J.L.; Li, C.; Jain, N.; Srivastava, D.K.; Mulrooney, D.; Zeltzer, L.; Stovall, M.; Robison, L.L.; Krull, K.R. Fatigue, vitality, sleep, and neurocognitive functioning in adult survivors of childhood cancer: A report from the Childhood Cancer Survivor Study. Cancer 2011, 117, 2559–2568. [Google Scholar] [CrossRef] [PubMed]
- Xavier, W.D.S.; Abreu, M.P.; Nunes, M.D.R.; Silva-Rodrigues, F.M.; da Silva, L.F.; de Araújo, B.B.M.; De Bortoli, P.S.; Neris, R.R.; Nascimento, L.C. The Sleep Patterns of Children and Adolescents with Chronic Conditions and Their Families: An Integrative Literature Review. Children 2024, 11, 207. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Narendran, G.; Tomfohr-Madsen, L.; Schulte, F. A systematic review of sleep in hospitalized pediatric cancer patients. Psychooncology 2017, 26, 1059–1069. [Google Scholar] [CrossRef]
- Chandwani, K.D.; Ryan, J.L.; Peppone, L.J.; Janelsins, M.M.; Sprod, L.K.; Devine, K.; Trevino, L.; Gewandter, J.; Morrow, G.R.; Mustian, K.M. Cancer-related stress and complementary and alternative medicine: A review. Evid. Based Complement. Altern. Med. 2012, 2012, 979213. [Google Scholar] [CrossRef]
- Amjad, M.T.; Chidharla, A.; Kasi, A. Cancer Chemotherapy. 3 March 2022. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2022; [Cited 14 August 2023]. Available online: https://pubmed.ncbi.nlm.nih.gov/33232037/ (accessed on 1 April 2025).
- Johnston, D.L.; Hyslop, S.; Tomlinson, D.; Baggott, C.; Gibson, P.; Orsey, A.; Dix, D.; Price, V.; Vanan, M.; Portwine, C.; et al. Describing symptoms using the Symptom Screening in Pediatrics Tool in hospitalized children with cancer and hematopoietic stem cell transplant recipients. Cancer Med. 2018, 7, 1750–1755. [Google Scholar] [CrossRef]
- Linder, L.A.; Al-Qaaydeh, S.; Donaldson, G. Symptom Characteristics Among Hospitalized Children and Adolescents With Cancer. Cancer Nurs. 2018, 41, 23–32. [Google Scholar] [CrossRef]
- Collins, J.J.; Byrnes, M.E.; Dunkel, I.J.; Lapin, J.; Nadel, T.; Thaler, H.T.; Polyak, T.; Rapkin, B.; Portenoy, R.K. The measurement of symptoms in children with cancer. J. Pain. Symptom Manag. 2000, 19, 363–377. [Google Scholar] [CrossRef]
- Williams, P.D.P.; Williams, A.R.P.; Kelly, K.P.P.; Dobos, C.P.; Gieseking, A.B.; Connor, R.M.; Ridder, L.M.; Potter, N.M.; Del Favero, D.M. A symptom checklist for children with cancer: The Therapy-Related Symptom Checklist-Children. Cancer Nurs. 2012, 35, 89–98. [Google Scholar] [CrossRef]
- Green, R.; Horn, H.; Erickson, J.M. Eating experiences of children and adolescents with chemotherapy-related nausea and mucositis. J. Pediatr. Oncol. Nurs. 2010, 27, 209–216. [Google Scholar] [CrossRef]
- Loeffen, E.A.; Brinksma, A.; Miedema, K.G.; de Bock, G.H.; Tissing, W.J. Clinical implications of malnutrition in childhood cancer patients--infections and mortality. Support. Care Cancer 2015, 23, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Chui, P.L. Cancer- and Chemotherapy-Related Symptoms and the Use of Complementary and Alternative Medicine. Asia Pac. J. Oncol. Nurs. 2019, 6, 4–6. [Google Scholar] [CrossRef] [PubMed]
- Hariyanto, T.I.; Kurniawan, A. Appetite problem in cancer patients: Pathophysiology, diagnosis, and treatment. Cancer Treat. Res. Commun. 2021, 27, 100336. [Google Scholar] [CrossRef]
- Baratieri, T.; Marcon, S.S. Longitudinality of care: Perceptions of the nurses that work at the family health strategy. Esc. Anna Nery. 2011, 15, 802–810. [Google Scholar] [CrossRef]
- Miaskowski, C. Future Directions in Symptom Cluster Research. Semin. Oncol. Nurs. 2016, 32, 405–415. [Google Scholar] [CrossRef]
- Yeh, C.H.; Chiang, Y.C.; Chien, L.C.; Lin, L.; Yang, C.P.; Chuang, H.L. Symptom clustering in older Taiwanese children with cancer. Oncol. Nurs. Forum. 2008, 35, 273–281. [Google Scholar] [CrossRef]
- Lopes-Júnior, L.C. Cancer symptom clusters: From the lab bench to clinical practice. Rev. Bras. Enferm. 2022, 75, e2022v75n5inov. [Google Scholar] [CrossRef]
- Kwekkeboom, K.L. Cancer Symptom Cluster Management. Semin. Oncol. Nurs. 2016, 32, 373–382. [Google Scholar] [CrossRef]
- Tanaka, H.; Medeiros, G.; Giglio, A. Multidisciplinary teams: Perceptions of professionals and oncological patients. Rev. Assoc. Med. Bras. 2020, 66, 419–423. [Google Scholar] [CrossRef]
- Al-Motlaq, M.A.; Carter, B.; Neill, S.; Hallstrom, I.K.; Foster, M.; Coyne, I.; Arabiat, D.; Darbyshire, P.; Feeg, V.D.; Shields, L. Toward developing consensus on family-centred care: An international descriptive study and discussion. J. Child. Health Care 2019, 23, 458–467. [Google Scholar] [CrossRef]
- Enskär, K.; Darcy, L.; Björk, M.; Knutsson, S.; Huus, K. Experiences of Young Children with Cancer and Their Parents with Nurses’ Caring Practices During the Cancer Trajectory. J. Pediatr. Oncol. Nurs. 2020, 37, 21–34. [Google Scholar] [CrossRef] [PubMed]
- Cheng, L.; Wang, L.; He, M.; Feng, S.; Zhu, Y.; Rodgers, C. Perspectives of children, family caregivers, and health professionals about pediatric oncology symptoms: A systematic review. Support. Care Cancer 2018, 26, 2957–2971. [Google Scholar] [CrossRef]
- Vitorino, L.M.; Lopes-Júnior, L.C.; de Oliveira, G.H.; Tenaglia, M.; Brunheroto, A.; Cortez, P.J.O.; Lucchetti, G. Spiritual and religious coping and depression among family caregivers of pediatric cancer patients in Latin America. Psychooncology 2018, 27, 1900–1907. [Google Scholar] [CrossRef] [PubMed]
| Database | Search Strategy |
|---|---|
| MEDLINE/PubMed | #1 (“Infant, Newborn” [MeSH Terms] OR “Infants, Newborn” [Title/Abstract] OR “Newborn Infant” [Title/Abstract] OR “Newborn Infants” [Title/Abstract] OR “Newborns” [Title/Abstract] OR “Newborn” [Title/Abstract] OR “Neonate” [Title/Abstract] OR “Neonates” [Title/Abstract] OR “Infant” [MeSH Terms] OR “Infants” [Title/Abstract] OR “Child” [MeSH Terms] OR “Children” [Title/Abstract] OR “Child, Preschool” [MeSH Terms] OR “Preschool Child” [Title/Abstract] OR “Children, Preschool” [Title/Abstract] OR “Preschool Children” [Title/Abstract] OR “Adolescent” [MeSH Terms] OR “Adolescents” [Title/Abstract] OR “Teens” [Title/Abstract] OR “Teenagers” [Title/Abstract] OR “Teenager” [Title/Abstract] OR “Youth” [Title/Abstract] OR “Youths” [Title/Abstract]) #2 (“Neoplasms” [MeSH Terms] OR “Neoplasia” [Title/Abstract] OR “Neoplasias” [Title/Abstract] OR “Neoplasm” [Title/Abstract] OR “Tumors” [Title/Abstract] OR “Tumor” [Title/Abstract] OR “Cancer” [Title/Abstract] OR “Cancers” [Title/Abstract] OR “Malignancy” [Title/Abstract] OR “Malignancies” [Title/Abstract] OR “Malignant Neoplasms” [Title/Abstract] OR “Malignant Neoplasm” [Title/Abstract] OR “Neoplasm, Malignant” [Title/Abstract] OR “Neoplasms, Malignant” [Title/Abstract]) #3 #1 AND #2 #4 (“Chemotherapy” [Title/Abstract] OR “Induction Chemotherapy” [MeSH Terms] OR “Chemotherapy, Induction” OR “Induction Chemotherapies” [Title/Abstract] OR “Consolidation Chemotherapy” [MeSH Terms] OR “Chemotherapy, Consolidation” [Title/Abstract] OR “Consolidation Chemotherapies” [Title/Abstract] OR “Maintenance Chemotherapy” [MeSH Terms] OR “Chemotherapy, Maintenance” [Title/Abstract] OR “Maintenance Chemotherapies” [Title/Abstract] NOT “Radiotherapy” [MeSH Terms] NOT “Surgery” [Subheading]) #5 (“Signs and Symptoms” [MeSH Terms] OR “Symptoms and Signs” [Title/Abstract] OR “Symptom Cluster” [Title/Abstract] OR “Cluster, Symptom” [Title/Abstract] OR “Clusters, Symptom” [Title/Abstract] OR “Symptom Clusters” [Title/Abstract] OR “Cancer Symptom Clusters” [Title/Abstract] OR “Symptom Constellation” [Title/Abstract] OR “Symptom Management” [Title/Abstract]) #6 #3 AND #4 AND #5 |
| Cochrane Library | #1 (Infant, Newborn) OR (Infants, Newborn) OR (Newborn Infant) OR (Newborn Infants) OR (Newborns) OR (Newborn) OR (Neonate) OR (Neonates) OR (Infant) OR (Infants) OR (Child) OR (Children) OR (Child, Preschool) OR (Preschool Child) OR (Children, Preschool) OR (Preschool Children) OR (Adolescent) OR (Adolescent) OR (Adolescents) OR (Teens) OR (Teenagers) OR (Teenager) OR (Youth) OR (Youths) #2 (Neoplasms) OR (Neoplasia) OR (Neoplasias) OR (Neoplasm) OR (Tumors) OR (Tumor) OR (Cancer) OR (Cancers) OR (Malignancy) OR (Malignancies) OR (Malignant Neoplasms) OR (Malignant Neoplasm) OR (Neoplasm, Malignant) OR (Neoplasms, Malignant) #3 #1 AND #2 #4 (Chemotherapy) OR (Induction Chemotherapy) OR (Chemotherapies, Induction) OR (Chemotherapy, Induction) OR (Induction Chemotherapies) OR (Consolidation Chemotherapy) OR (Chemotherapy, Consolidation) OR (Consolidation Chemotherapies) OR (Maintenance Chemotherapy) OR (Chemotherapy, Maintenance) OR (Maintenance Chemotherapies) NOT (Radiotherapy) NOT (Surgery) #5 (Signs and Symptoms) OR (Symptoms and Signs) OR (Symptom Cluster) OR (Cluster, Symptom) OR (Clusters, Symptom) OR (Symptom Clusters) OR (Cancer Symptom Clusters) OR (Symptom Constellation) OR (Symptom Management) #6 #3 AND #4 AND #5 |
| EMBASE | #1 (‘child’/exp OR ‘preschool child’/exp OR ‘child, preschool’ OR ‘pre-school child’ OR ‘pre-school going children’ OR ‘pre-schooler’ OR ‘pre-schoolers’ OR ‘preschool child institution’ OR ‘preschooler’ OR ‘adolescent’/exp OR ‘teenager’ OR ‘juvenile’ OR ‘youth’) #2 (‘neoplasm’/exp OR ‘tumor’ OR ‘tumour’ OR ‘tumors’ OR ‘malignant neoplasm’ OR ‘cancer’ OR ‘cancers’ OR ‘malignant neoplasia’ OR ‘malignant neoplastic disease’ OR ‘malignant tumor’ OR ‘malignant tumour’ OR ‘neoplasia, malignant’ OR ‘tumor, malignant’ OR ‘tumour, malignant’) #3 (‘chemotherapy’/exp OR ‘induction chemotherapy’/exp OR ‘consolidation chemotherapy’/exp OR ‘maintenance chemotherapy’ OR ‘chemotherapeutics’ OR ‘chemotherapy, induction’ OR ‘chemotherapeutic consolidation’ OR ‘ chemotherapy consolidation’) #4 (‘physical disease by body function’/exp OR ‘symptom’/exp) #5 #1 AND #2 AND #3 AND #4 |
| Web of Science | #1 ALL = ((Infant, Newborn) OR (Infants, Newborn) OR (Newborn Infant) OR (Newborn Infants) OR (Newborns) OR (Newborn) OR (Neonate) OR (Neonates) OR (Infant) OR (Infants) OR (Child) OR (Children) OR (Child, Preschool) OR (Preschool Child) OR (Children, Preschool) OR (Preschool Children) OR (Adolescent) OR (Adolescent) OR (Adolescents) OR (Teens) OR (Teenagers) OR (Teenager) OR (Youth) OR (Youths)) #2 ALL = ((Neoplasms) OR (Neoplasia) OR (Neoplasias) OR (Neoplasm) OR (Tumors) OR (Tumor) OR (Cancer) OR (Cancers) OR (Malignancy) OR (Malignancies) OR (Malignant Neoplasms) OR (Malignant Neoplasm) OR (Neoplasm, Malignant) OR (Neoplasms, Malignant)) #3 #1 AND #2 #4 ALL = ((Chemotherapy) OR (Chemotherapy, Adjuvant) OR (Induction Chemotherapy) OR (Consolidation Chemotherapy) OR (Maintenance Chemotherapy)) #5 ALL = ((Symptom Cluster) OR (Cluster, Symptom) OR (Clusters, Symptom) OR (Symptom Clusters) OR (Cancer Symptom Clusters) OR (Symptom Constellation) OR (Symptom Management)) #6 #3 AND #4 AND #5 |
| PsycINFO | #1 (Adolescent Health OR Preschool Students OR Child Health) #2 (Neoplasms OR Malignant Neoplasms OR Cancers OR Carcinomas OR Tumors) #3 (Chemotherapy OR Chemotherapeutics) #4 (Symptoms OR Symptoms Based Treatment OR Symptom Cluster OR Cancer Symptom Cluster) #5 #1 AND #2 AND #3 AND #4 |
| Clinicaltrial.gov | #1 (Child) OR (Children) OR (Adolescent) OR (Adolescents) #2 (Neoplasms) OR (Neoplasia) #3 (Chemotherapy) #4 (Symptom Cluster) OR (Symptom Management) #5 #1 AND #2 AND #3 AND #4 |
| WHO International Clinical Trials Registry Platform | (Child OR Children OR Adolescent OR Adolescents) AND (Neoplasms OR Neoplasia) AND (Chemotherapy) AND (Symptom Cluster OR Symptom Management) |
| The British Library (UK) | (Child OR Children OR Adolescent OR Adolescents) AND (Neoplasms OR Neoplasia) AND (Chemotherapy) AND (Symptom Cluster OR Symptom Management) |
| Google Scholar | (Children OR Adolescents) AND (Neoplasms OR Neoplasia) AND (Chemotherapy) AND (Symptom Cluster) |
| Preprints in Health Sciences (medRxiv) | (Children OR Adolescents) AND (Neoplasms OR Neoplasia) AND (Chemotherapy) AND (Symptom Cluster) |
| Reference/ Country | Design/ Level of Evidence | Objective | Sample | Symptom Assessed/ Instruments | Main Results |
|---|---|---|---|---|---|
| Hockenberry et al., 2010 [31] United States | Quasi-experimental 2B | To examine the influence of CSC fatigue, nausea/vomiting, and sleep disturbances on clinical outcomes and behavior in children and adolescents, before and after receiving chemotherapy | 67 children and teenagers Age: 7 to 18 years (average age: 12.3 years) | Symptoms: Fatigue, nausea/vomiting, performance status, depression and sleep disturbances Instruments: CFS/ AFS/PFS/wrist actigraph/CDI/BASC/LPPS/KPS | When analyzed as a symptom cluster, fatigue, sleep disturbances, nausea, and vomiting had a negative impact on depressive symptoms and behavioral changes in adolescents after chemotherapy. In children, however, fatigue alone influenced depressive symptoms and behavioral changes. Fatigue was a significant predictor of depressive symptoms in children (F[1,67] = 18.427, p < 0.001). Additionally, higher parental perception of fatigue in their children was associated with greater reported behavioral and emotional difficulties (F[1,89] = 12.535, p = 0.001). |
| Atay 2011 [32] Turkey | Cross-sectional 3B | To describe the prevalence of CSC symptoms that occur in children and adolescents receiving chemotherapy or who have completed treatment | 164 children and adolescents (79 boys and 85 girls) Age: 10 to 18 years (mean age: 13.9 ± 2.1 years) | Symptoms: 30 cancer symptoms Instrument: MSAS | 5 CSC were identified: Cluster 1: trouble urinating, diarrhea, difficulty swallowing, constipation. Cluster 2: dyspnea, dizziness, mouth sores, taste changes, weight loss, dry mouth. Cluster 3: lack of concentration, skin changes, numbness/tingling, swelling of arms/legs, itching, insomnia, sweating, coughing. Cluster 4: worried, irritated, “I don’t look like myself”, hair loss. Cluster 5: nausea, vomiting, fatigue. The most prevalent CSC included nervousness, sadness, and fatigue. The most distressing symptoms in patients aged 10 to 18 y.o. were nausea/vomiting and alopecia. |
| Atay et al. 2012 [33] Turkey | Cross-sectional 3B | To determine the prevalence of CSC in children at 3, 6, and 12 months after cancer diagnosis | 44 adolescents and children (30 boys and 24 girls) Mean age: 14 years | Symptoms: 30 symptoms were assessed for severity and distress Instrument: MSAS | Four CSC were identified within the first month after diagnosis: Cluster 1: Dizziness, changes in food taste, and worry. Cluster 2: Feeling irritable, sad, and nervous. Cluster 3: Vomiting, nausea, and lack of energy. Cluster 4: Sweating, diarrhea, and insomnia. |
| Baggott et al., 2012 [34] United States | Cross-sectional 3B | To compare the number and types of CSC identified through patient ratings of symptoms | 131 children and adolescents Age: 10 to 18 years | Symptoms: Chemotherapy sequelae, mood disorders and neuropsychological distress Instruments: MSAS/KPS | Most symptoms contributed similarly to the chemotherapy sequelae cluster. For mood disturbance cluster, feeling irritable made the weakest contribution. In the neuropsychological distress cluster, feeling irritable, altered self-perception, and skin changes were the weakest contributors (χ2 = 322.7, p < 0.01). |
| Hockenberry et al., 2011 [35] United States | Quasi-experimental 2B | To examine the effects of synergistic symptoms experienced by pediatric patients during cancer therapy | 67 children and adolescents (38 boys and 29 girls) Age: 7 to 18 years (average age: 12.3 years) | Symptoms: Fatigue, nausea and vomiting, depression, and performance status symptoms Instruments: CFS/ AFS/PFS/wrist actigraph/CDI/BASC/LPPS/KPS | In Cluster 1 (fatigue, functional status, mood disturbances, and depression), the prevalence of moderate to severe symptoms one week after chemotherapy was: fatigue: 60.3%; impaired functional status: 47.6%; mood disturbances: 36.5%; depression: 18.5%. Adolescents diagnosed with solid tumors and those who had received prior chemotherapy were more likely to experience fatigue and depression (p < 0.01). In Cluster 2 (vomiting, nausea, sleep disturbance, and performance status), the prevalence of moderate to severe symptoms was: nausea: 42.4%; vomiting: 20.6%; altered performance status: 13.8%. |
| Lopes-Junior et al., 2018 [36] Brazil | Quasi-experimental 2B | To examine the feasibility of longitudinal testing of stress and fatigue in pediatric patients with osteosarcoma under chemotherapy who underwent clown intervention | 6 children/adolescents with osteosarcoma (12.33 ± 3.32) | Symptoms: Cancer-related fatigue and psychological stress Instruments: CSS/ PedsQL MFS (self and proxy version) | Cortisol levels exhibited a decreasing trend over time in all six pediatric osteosarcoma patients. A similar trend was observed for tumor necrosis factor-α (TNF-α) levels across all six patients. In patients with metastatic osteosarcoma, metalloproteinase-9 levels showed a linear decrease between 1 and 9 h after the clown intervention. |
| Li et al., 2020 [37] China | Cross-sectional 3B | To investigate CSC in children with acute lymphoblastic leukemia receiving chemotherapy and their predictors | 159 patients (97 boys and 62 girls) Mean age: 8.92 ± 3.33 years | Symptoms: Gastrointestinal, emotional, cognitive-related, self-image disorder symptoms, skin irritation cluster and somatic cluster Instrument: MSAS | Six CSC were identified, including the following: (i) gastrointestinal cluster; (ii) emotional cluster; (iii) cognitive cluster; (iv) self-image disorder cluster; (v) skin irritation cluster; and (vi) somatic cluster. Multiple linear regression analysis revealed that “chemotherapy phase, sex, and age were significantly associated with cluster severity, explaining 9.1–28.7% of the variance across clusters”. |
| Lopes-Junior et al., 2020 [38] Brazil | Quasi-experimental 2B | To evaluate the effect of clown theater art intervention on levels of stress and fatigue in pediatric cancer patients undergoing chemotherapy | 16 children/adolescents with cancer | Symptoms: Cancer-related fatigue and psychological stress Instruments: CSS/ PedsQL MFS (self and proxy version) | Compared to baseline measurements, total psychological stress and cancer-related fatigue levels showed significant improvement following the clown intervention (p = 0.003 and p = 0.04, respectively). Additionally, salivary cortisol levels significantly decreased after the intervention at +1, +9, and +13 h (p < 0.05). In contrast, α-amylase levels remained unchanged. |
| Hooke et al., 2022 [39] United States | Longitudinal study 2A | To examine differences between CSC and quality of life (QoL) throughout the course of maintenance therapy for ALL | 42 children and adolescents with cancer | Symptoms: Fatigue, sleep disturbance, and depression Instruments: CFS/AFS PROMIS/ GLTEQ | Two latent CSC classes (low and high) showed significant differences in symptoms and QoL at the start and end of maintenance therapy (p < 0.01), though both remained stable over time. Children with lower symptom burden and higher physical activity at baseline had better QoL outcomes post-treatment (p < 0.01). |
| Li et al., 2022 [40] China | Cross-sectional 3B | To examine CSC that children with ALL undergoing chemotherapy have which impact on their QoL | 184 children, with the mean age of 10.38 (2.22) years | Symptoms: Gastrointestinal, emotional, neurological, skin mucosal, self-image disorder, and somatic cluster Instruments:MSAS/PedsQL | The severity of all 6 CSC was negatively correlated with QoL in children with ALL. Gastrointestinal, emotional, and somatic symptom clusters were the primary factors impacting QoL in children with ALL undergoing chemotherapy. |
| Wang et al., 2025 [41] China | Cross-sectional 3B | To explore the dynamic changes in symptom clusters among children with ALL during chemotherapy using electronic nursing records | 75 children with ALL with an average age of 6.2 years | Symptoms: Cough, vomiting, fatigue, and fever Instruments: MSAS/PedsQL Generic Core Module v. 4.0) | The most common symptoms reported were bleeding, cough, and vomiting. Notably, upper gastrointestinal, respiratory, lower gastrointestinal, and skin-related symptom clusters persisted throughout both the consolidation and maintenance periods. Additionally, neurological and other discomfort-related symptom clusters were observed exclusively during the consolidation phase. |
| Li et al., 2024 [42] China | Longitudinal study 2A | To assess the stability of CSC in children with ALL during chemotherapy | 134 children (8–16 years old), mean age 10.53 (±2.18) years | Symptoms: Gastrointestinal, emotional, neurological, skin mucosal, self-image disorder, and somatic cluster Instrument: MSAS | Six CSCs were identified. Emotional and somatic clusters were consistently present across all dimensions and time points. Gastrointestinal and self-image disorder clusters appeared at most time points, while neurological and skin–mucosa clusters were observed primarily at T2 and T3. |
| ROBINS-I * Domains | Overall Judgment ROBINS-I * | |||||||
|---|---|---|---|---|---|---|---|---|
| Study | Confounding Bias | Selection Bias | Intervention Classification Bias | Bias Due to Intervention Deviations | Incomplete Data Bias | Outcome Measurement Bias | Selective Outcome Reporting Bias | |
| Hockenberry et al., 2010 [31] | Low | Low | Low | Low | Low | Low | Low | Low |
| Hockenberry et al., 2011 [35] | Low | Low | Low | Low | Low | Low | Low | Low |
| Lopes-Junior et al., 2018 [36] | Low | Low | Low | Low | Low | Low | Low | Low |
| Lopes-Junior et al., 2020 [38] | Low | Moderate | Low | Low | Low | Low | Low | Moderate |
| JBI Critical Appraisal Checklist | Were the Inclusion Criteria for the Sample Clearly Defined? | Were the Study Participants and the Study Location Described in Detail? | Was the Exposure Measured Reliably and Validly? | Were Objective and Standardized Criteria Used to Assess Health Status? | Were Confounding Factors Identified and Addressed? | Have Strategies Been Established to Manage Confounding Factors? | Were the Outcomes Measured Reliably and Validly? | Was the Appropriate Statistical Analysis Applied? |
|---|---|---|---|---|---|---|---|---|
| Atay, 2011 [30] | Yes | Yes | Yes | Yes | No | No | Yes | Yes |
| Atay, 2012 [31] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Baggott et al., 2012 [34] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Li et al., 2020 [37] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hooke et al., 2022 [39] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Rongrong Li et al., 2022 [40] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Wang et al., 2025 [41] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Rongrong Li et al., 2024 [42] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lopes-Júnior, L.C.; Grassi, J.; Freitas, M.B.; Trigo, F.E.S.; Jardim, F.A.; Nunes, K.Z.; Vasconcelos, K.A.d.; Lima, R.A.G.d. Cancer Symptom Clusters in Children and Adolescents with Cancer Undergoing Chemotherapy: A Systematic Review. Nurs. Rep. 2025, 15, 163. https://doi.org/10.3390/nursrep15050163
Lopes-Júnior LC, Grassi J, Freitas MB, Trigo FES, Jardim FA, Nunes KZ, Vasconcelos KAd, Lima RAGd. Cancer Symptom Clusters in Children and Adolescents with Cancer Undergoing Chemotherapy: A Systematic Review. Nursing Reports. 2025; 15(5):163. https://doi.org/10.3390/nursrep15050163
Chicago/Turabian StyleLopes-Júnior, Luís Carlos, Jonathan Grassi, Marcela Bortoleto Freitas, Fernanda Ercília Souza Trigo, Fabrine Aguilar Jardim, Karolini Zuqui Nunes, Karla Anacleto de Vasconcelos, and Regina Aparecida Garcia de Lima. 2025. "Cancer Symptom Clusters in Children and Adolescents with Cancer Undergoing Chemotherapy: A Systematic Review" Nursing Reports 15, no. 5: 163. https://doi.org/10.3390/nursrep15050163
APA StyleLopes-Júnior, L. C., Grassi, J., Freitas, M. B., Trigo, F. E. S., Jardim, F. A., Nunes, K. Z., Vasconcelos, K. A. d., & Lima, R. A. G. d. (2025). Cancer Symptom Clusters in Children and Adolescents with Cancer Undergoing Chemotherapy: A Systematic Review. Nursing Reports, 15(5), 163. https://doi.org/10.3390/nursrep15050163










