Parents’ Participation in Care during Neonatal Intensive Care Unit Stay in COVID-19 Era: An Observational Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample and Setting
2.2. Data Collection
2.3. Statistical Analysis
3. Results
3.1. Barriers Related to Parental Background
3.2. Barriers Related to Neonates’ Features
3.3. Multiple Linear Regression
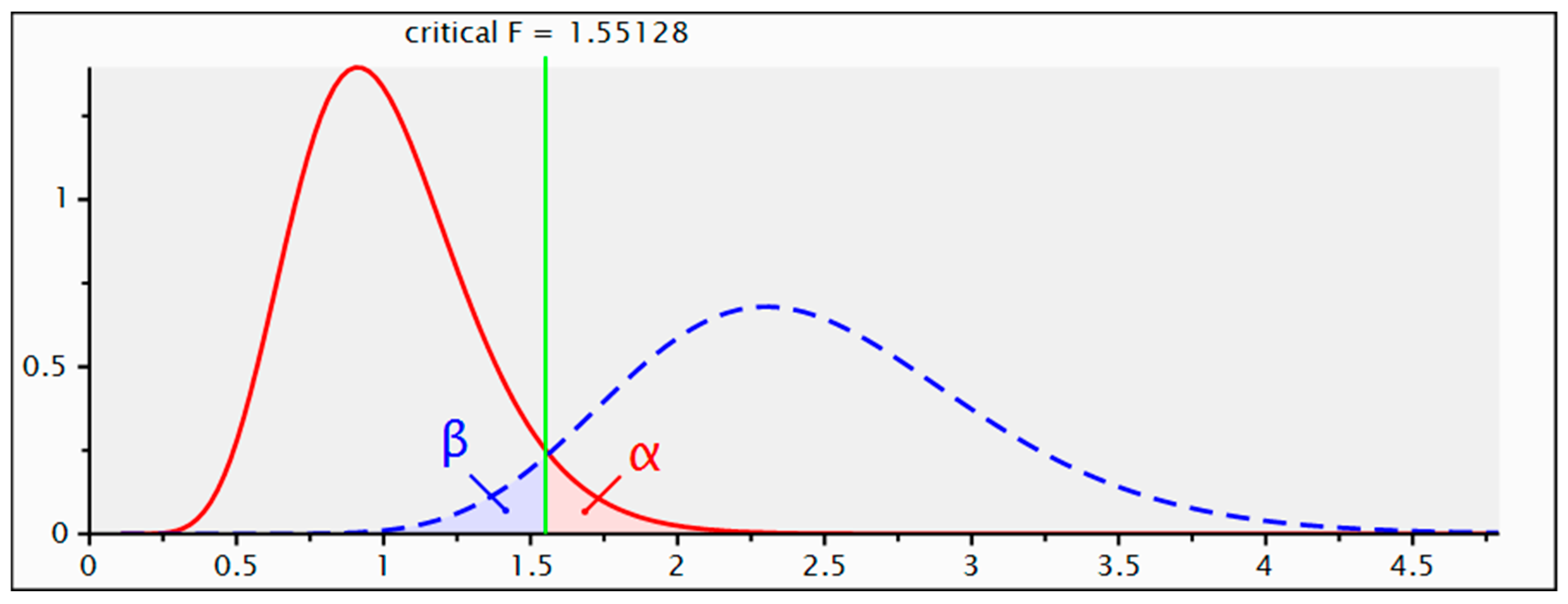
3.4. Sensitivity Power Analysis of Multiple Linear Regression
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public Involvement Statement
Guidelines and Standards Statement
Use of Artificial Intelligence
Conflicts of Interest
References
- van Veenendaal, N.R.; Labrie, N.H.M.; Mader, S.; van Kempen, A.A.M.W.; van der Schoor, S.R.D.; van Goudoever, J.B.; CROWN Study Group; Bertino, E.; Bhojnagarwala, B.; Bodrogi, E.; et al. An International Study on Implementation and Facilitators and Barriers for Parent-infant Closeness in Neonatal Units. Pediatr. Investig. 2022, 6, 179–188. [Google Scholar] [CrossRef]
- Bergman, N.J. Birth Practices: Maternal-neonate Separation as a Source of Toxic Stress. Birth Defects Res. 2019, 111, 1087–1109. [Google Scholar] [CrossRef]
- Walker, S.B. Neonatal Nurses’ Views on the Bamers to Parenting in the Intensive Care Nursery—A Pilot Study. Aust. Crit. Care 1997, 10, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Craig, J.W.; Glick, C.; Phillips, R.; Hall, S.L.; Smith, J.; Browne, J. Recommendations for Involving the Family in Developmental Care of the NICU Baby. J. Perinatol. 2015, 35, S5–S8. [Google Scholar] [CrossRef] [PubMed]
- Sundal, H.; Vatne, S. Parents’ and Nurses’ Ideal Collaboration in Treatment-Centered and Home-like Care of Hospitalized Preschool Children—A Qualitative Study. BMC Nurs. 2020, 19, 48. [Google Scholar] [CrossRef] [PubMed]
- Soni, R.; Tscherning, C. Family-Centred and Developmental Care on the Neonatal Unit. Paediatr. Child Health 2021, 31, 18–23. [Google Scholar] [CrossRef]
- Chen, H.; Dong, L. The Effect of Family Integrated Care on the Prognosis of Premature Infants. BMC Pediatr. 2022, 22, 668. [Google Scholar] [CrossRef]
- Montirosso, R.; Provenzi, L.; Calciolari, G.; Borgatti, R.; NEO-ACQUA Study Group. Measuring Maternal Stress and Perceived Support in 25 Italian NICUs: Maternal Stress and Perceived Support in NICUs Instead of Measuring Maternal Stress and Perceived Support. Acta Paediatr. 2012, 101, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Heidarzadeh, M.; Heidari, H.; Ahmadi, A.; Solati, K.; Sadeghi, N. Evaluation of Parental Stress in Neonatal Intensive Care Unit in Iran: A National Study. BMC Nurs 2023, 22, 41. [Google Scholar] [CrossRef]
- Okito, O.; Yui, Y.; Wallace, L.; Knapp, K.; Streisand, R.; Tully, C.; Fratantoni, K.; Soghier, L. Parental Resilience and Psychological Distress in the Neonatal Intensive Care Unit. J. Perinatol. 2022, 42, 1504–1511. [Google Scholar] [CrossRef]
- Caporali, C.; Pisoni, C.; Gasparini, L.; Ballante, E.; Zecca, M.; Orcesi, S.; Provenzi, L. A Global Perspective on Parental Stress in the Neonatal Intensive Care Unit: A Meta-Analytic Study. J. Perinatol. 2020, 40, 1739–1752. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.K.; O’Brien, K. Parents as Primary Caregivers in the Neonatal Intensive Care Unit. CMAJ 2014, 186, 845–847. [Google Scholar] [CrossRef] [PubMed]
- Polloni, L.; Cavallin, F.; Lolli, E.; Schiavo, R.; Bua, M.; Volpe, B.; Meneghelli, M.; Baraldi, E.; Trevisanuto, D. Psychological Wellbeing of Parents with Infants Admitted to the Neonatal Intensive Care Unit during SARS-CoV-2 Pandemic. Children 2021, 8, 755. [Google Scholar] [CrossRef] [PubMed]
- Muniraman, H.; Ali, M.; Cawley, P.; Hillyer, J.; Heathcote, A.; Ponnusamy, V.; Coleman, Z.; Hammonds, K.; Raiyani, C.; Gait-Carr, E.; et al. Parental Perceptions of the Impact of Neonatal Unit Visitation Policies during COVID-19 Pandemic. BMJ Paediatr. Open 2020, 4, e000899. [Google Scholar] [CrossRef]
- Darcy Mahoney, A.; White, R.D.; Velasquez, A.; Barrett, T.S.; Clark, R.H.; Ahmad, K.A. Impact of Restrictions on Parental Presence in Neonatal Intensive Care Units Related to Coronavirus Disease 2019. J. Perinatol. 2020, 40, 36–46. [Google Scholar] [CrossRef] [PubMed]
- Vance, A.J.; Malin, K.J.; Miller, J.; Shuman, C.J.; Moore, T.A.; Benjamin, A. Parents’ Pandemic NICU Experience in the United States: A Qualitative Study. BMC Pediatr. 2021, 21, 558. [Google Scholar] [CrossRef] [PubMed]
- Bua, J.; Dalena, P.; Mariani, I.; Girardelli, M.; Ermacora, M.; Manzon, U.; Plet, S.; Travan, L.; Lazzerini, M. Parental Stress, Depression, Anxiety and Participation in Care in Neonatal Intensive Care Unit: A Cross-Sectional Study in Italy Comparing Mothers versus Fathers. BMJ Paediatr. 2024, 8, e002429. [Google Scholar] [CrossRef] [PubMed]
- Erdei, C.; Feldman, N.; Koire, A.; Mittal, L.; Liu, C.H.J. COVID-19 Pandemic Experiences and Maternal Stress in Neonatal Intensive Care Units. Children 2022, 9, 251. [Google Scholar] [CrossRef] [PubMed]
- Curtis, E.; Jones, R.; Tipene-Leach, D.; Walker, C.; Loring, B.; Paine, S.-J.; Reid, P. Why Cultural Safety Rather than Cultural Competency Is Required to Achieve Health Equity: A Literature Review and Recommended Definition. Int. J. Equity Health 2019, 18, 174. [Google Scholar] [CrossRef]
- Bainter, J.; Fry, M.; Miller, B.; Miller, T.; Nyberg, A.; O’Dell, A.; Shaffer, G.; Vernon, L. Family Presence in the NICU: Constraints and Opportunities in the COVID-19 Era. Pediatr. Nurs. 2020, 46, 256–259. [Google Scholar]
- Ceylan, S.S.; Keskin, Z.; Yavaş, Z.; Özdemir, H.; Tosun, G.; Güner, E.; İzci, A. Developing the Scale of Parental Participation in Care: Neonatal Intensive Care Unit and Examining the Scale’s Psychometric Properties. Intensive Crit. Care Nurs. 2021, 65, 103037. [Google Scholar] [CrossRef]
- Scarponcini Fornaro, D.; Della Pelle, C.; Buccione, E. Parental Participation in Care during Neonatal Intensive Care Unit Stay: A Validation Study. Inferm. J. 2023, 1, 81–88. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical Power Analyses Using G*Power 3.1: Tests for Correlation and Regression Analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Selya, A.S.; Rose, J.S.; Dierker, L.C.; Hedeker, D.; Mermelstein, R.J. A Practical Guide to Calculating Cohen’s F2, a Measure of Local Effect Size, from PROC MIXED. Front. Psychol. 2012, 3, 111. [Google Scholar] [CrossRef] [PubMed]
- Dall’Oglio, I.; Fiori, M.; Tiozzo, E.; Mascolo, R.; Portanova, A.; Gawronski, O.; Ragni, A.; Amadio, P.; Cocchieri, A.; Fida, R.; et al. Neonatal Intensive Care Parent Satisfaction: A Multicenter Study Translating and Validating the Italian EMPATHIC-N Questionnaire. Ital. J. Pediatr. 2018, 44, 5. [Google Scholar] [CrossRef]
- Bua, J.; Mariani, I.; Girardelli, M.; Tomadin, M.; Tripani, A.; Travan, L.; Lazzerini, M. Parental Stress, Depression, and Participation in Care Before and during the COVID-19 Pandemic: A Prospective Observational Study in an Italian Neonatal Intensive Care Unit. Front. Pediatr. 2021, 9, 737089. [Google Scholar] [CrossRef]
- Ravi, D.; Iacob, A.; Profit, J. Unequal Care: Racial/Ethnic Disparities in Neonatal Intensive Care Delivery. Semin. Perinatol. 2021, 45, 151411. [Google Scholar] [CrossRef]
- Van McCrary, S.; Green, H.C.; Combs, A.; Mintzer, J.P.; Quirk, J.G. A Delicate Subject: The Impact of Cultural Factors on Neonatal and Perinatal Decision Making. J. Neonatal-Perinat. Med. 2014, 7, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Bracht, M.; Kandankery, A.; Nodwell, S.; Stade, B. Cultural Differences and Parental Responses to the Preterm Infant at Risk: Strategies for Supporting Families. Neonatal Netw. 2002, 21, 31–38. [Google Scholar] [CrossRef]
- Palau, M.A.; Meier, M.R.; Brinton, J.T.; Hwang, S.S.; Roosevelt, G.E.; Parker, T.A. The Impact of Parental Primary Language on Communication in the Neonatal Intensive Care Unit. J. Perinatol. 2019, 39, 307–313. [Google Scholar] [CrossRef]
- Schmid, S.V.; Arnold, C.; Jaisli, S.; Bubl, B.; Harju, E.; Kidszun, A. Parents’ and Neonatal Healthcare Professionals’ Views on Barriers and Facilitators to Parental Presence in the Neonatal Unit: A Qualitative Study. BMC Pediatr. 2024, 24, 268. [Google Scholar] [CrossRef]
- Kerr, S.; King, C.; Hogg, R.; McPherson, K.; Hanley, J.; Brierton, M.; Ainsworth, S. Transition to Parenthood in the Neonatal Care Unit: A Qualitative Study and Conceptual Model Designed to Illuminate Parent and Professional Views of the Impact of Webcam Technology. BMC Pediatr. 2017, 17, 158. [Google Scholar] [CrossRef]
- Richter, L.L.; Ku, C.; Mak, M.Y.Y.; Holsti, L.; Kieran, E.; Alonso-Prieto, E.; Ranger, M. Experiences of Mothers of Preterm Infants in the Neonatal Intensive Care Unit during the COVID-19 Pandemic. Adv. Neonatal Care 2023. Publish Ahead of Print. [Google Scholar] [CrossRef]
- Schappin, R.; Wijnroks, L.; Uniken Venema, M.M.A.T.; Jongmans, M.J. Rethinking Stress in Parents of Preterm Infants: A Meta-Analysis. PLoS ONE 2013, 8, e54992. [Google Scholar] [CrossRef]
- Bry, A.; Wigert, H. Psychosocial Support for Parents of Extremely Preterm Infants in Neonatal Intensive Care: A Qualitative Interview Study. BMC Psychol. 2019, 7, 76. [Google Scholar] [CrossRef]
- Yance, B.; Do, K.; Heath, J.; Fucile, S. Parental Perceptions of the Impact of NICU Visitation Policies and Restrictions Due to the COVID-19 Pandemic: A Qualitative Study. Adv. Neonatal Care 2023. Publish Ahead of Print. [Google Scholar] [CrossRef]
- Lantz, B.; Ottosson, C. Parental Interaction with Infants Treated with Medical Technology. Scand. Caring Sci. 2013, 27, 597–607. [Google Scholar] [CrossRef]
- Bembich, S.; Tripani, A.; Mastromarino, S.; Di Risio, G.; Castelpietra, E.; Risso, F.M. Parents Experiencing NICU Visit Restrictions Due to COVID-19 Pandemic. Acta Paediatr. 2021, 110, 940–941. [Google Scholar] [CrossRef]
- Adama, E.A.; Koliouli, F.; Provenzi, L.; Feeley, N.; van Teijlingen, E.; Ireland, J.; Thomson-Salo, F.; Khashu, M.; FINESSE Group. COVID-19 Restrictions and Psychological Well-being of Fathers with Infants Admitted to NICU—An Exploratory Cross-sectional Study. Acta Paediatr. 2022, 111, 1771–1778. [Google Scholar] [CrossRef]
- Merritt, L.; Maxwell, J.; Urbanosky, C. The Needs of NICU Fathers in Their Own Words: A Qualitative Descriptive Study. Adv. Neonatal Care 2022, 22, E94–E101. [Google Scholar] [CrossRef]
- Lee, J.W.; Lee, S. Perceptions of Fatherhood and Confidence Regarding Neonatal Care among Fathers of High-Risk Neonates in South Korea: A Descriptive Study. Child Health Nurs. Res. 2023, 29, 229–236. [Google Scholar] [CrossRef]
- Song, M.; Ishii, H.; Toda, M.; Tomimatsu, T.; Katsuyama, H.; Nakai, Y.; Shimoya, K. Maternal Depression and Mother-to-Infant Bonding: The Association of Delivery Mode, General Health and Stress Markers. OJOG 2017, 07, 155–166. [Google Scholar] [CrossRef]
- Zanardo, V.; Soldera, G.; Volpe, F.; Giliberti, L.; Parotto, M.; Giustardi, A.; Straface, G. Influence of Elective and Emergency Cesarean Delivery on Mother Emotions and Bonding. Early Hum. Dev. 2016, 99, 17–20. [Google Scholar] [CrossRef] [PubMed]
| Factor | Categories | N (%) | Median [IQR] I Assessment | p-Value | Median [IQR] II Assessment | p-Value |
|---|---|---|---|---|---|---|
| Gestational Age | Extremely Preterm | 8 (3.0%) | 31 [9] | <0.001 | 39.5 [9] | 0.033 † |
| Very Preterm | 32 (11.9%) | 35 [12] | 42 [10] | |||
| Moderate/Late preterm | 60 (22.2%) | 42.5 [7] | 46 [3] | |||
| Term | 170 (63.0%) | 42 [9] | 45 [7] | |||
| Parents’ Gender | Female | 136 (50.4%) | 42 [8] | 0.017 | 46 [6] | 0.003 |
| Male | 134 (49.6%) | 39 [11] | 44 [9] | |||
| First Child | No | 121 (44.8%) | 38 [12] | 0.005 | 44 [10] | 0.015 |
| Yes | 149 (55.2%) | 42 [8] | 46 [6] | |||
| Previous Abortions | No | 211 (78.1%) | 41 [9] | 0.325 | 45 [8] | 0.294 |
| Yes | 59 (21.9%) | 39 [12] | 47 [7] | |||
| Previous Deceased Children | No | 263 (97.4%) | 41 [10] | 0.070 | 46 [7] | 0.093 |
| Yes | 7 (2.6%) | 35 [6] | 40 [6] | |||
| Type of Delivery | Natural Birth | 128 (47.4%) | 43 [8] | <0.001 | 46 [6] | 0.006 |
| Elective Cesarean Section | 76 (28.1%) | 40.5 [10] | 44 [8] | |||
| Emergency Cesarean Section | 66 (24.4%) | 38 [12] | 46 [9] | |||
| Parents’ Ethnicity | Caucasian | 238 (88.1%) | 42 [8] | <0.001 | 46 [7] | <0.001 |
| African | 18 (6.7%) | 30.5 [15] | 38 [9] | |||
| Hispanic/Latino Americans | 10 (3.7%) | 45 [8] | 47.5 [4] | |||
| Asian * | 4 (1.5%) | 16 [0] | 16 [0] | |||
| Job | Unemployed | 60 (22.2%) | 42 [10] | 0.119 | 44 [8] | 0.126 |
| Employee | 200 (74.1%) | 41 [10] | 46 [7] | |||
| Student | 10 (3.7%) | 32 [24] | 42 [21] | |||
| Twins | No | 237 (87.8%) | 41 [11] | 0.981 | 45 [8] | 0.029 |
| Yes | 33 (12.2%) | 40 [7] | 47 [1] |
| Factor | Categories | N (%); Median (IQR) I Assessment | p-Value | N (%); Median (IQR) II Assessment | p-Value |
|---|---|---|---|---|---|
| Peripheric venous catheter | No | 119 (44.1%); 39 (11) | 0.062 | 89 (33.0%); 46 (9) | 0.663 |
| Yes | 151 (55.9%); 42 (9) | 181 (67.0%); 46 (6) | |||
| Central venous catheter | No | 238 (88.1%); 41.5 (9) | 0.011 | 212 (78.5%); 46 (7) | <0.001 |
| Yes | 32 (11.9%); 38 (17) | 58 (21.5%); 42 (9) | |||
| Umbilical venous catheter | No | 180 (66.7%); 42 (9) | 0.462 | 270 (100%); 46 (8) | - |
| Yes | 90 (33.3%); 39 (10) | - | |||
| Continuous infusions | No | 92 (34.1%); 38.5 (11) | 0.203 | 132 (48.9%); 46 (8) | 0.015 |
| Yes | 178 (65.9%); 42 (10) | 138 (51.1%); 45 (7) | |||
| Arterial catheter | No | 260 (96.3%); 41 (10) | 0.032 | 270 (100%); 46 (8) | - |
| Yes | 10 (3.7%); 34 (10) | - | |||
| High-flow nasal cannula | No | 226 (83.7%); 41 (11) | 0.679 | 226 (83.7%); 46 (8) | 0.713 |
| Yes | 44 (16.3%); 41 (10) | 44 (16.3%); 46 (5) | |||
| Non-invasive ventilation | No | 258 (95.6%); 41 (10) | 0.802 | 261 (96.7%); 46 (7) | 0.049 |
| Yes | 12 (4.4%); 41 (7) | 9(3.3%); 40 (6) | |||
| Endotracheal tube | No | 224 (86.0%); 42 (8) | 0.001 | 243 (90.0%); 46 (7) | 0.001 |
| Yes | 46 (17.0%); 35 (13) | 27 (10.0%); 41 (9) | |||
| High-frequency oscillatory ventilation | No | 258 (95.9%); 41.5 (9) | 0.005 | 266 (98.5%); 46 (8) | 0.140 |
| Yes | 12 (4.4%); 34 (10) | 4 (1.5%); 40 (10) | |||
| Gastric tube | No | 168 (62.2%); 42.5 (10) | 0.006 | 170 (63.0%); 46 (7) | 0.031 |
| Yes | 102 (37.8%); 39 (11) | 100 (37.0%); 44 (8) | |||
| Cerebral function monitoring | No | 252 (93.3%); 42 (10) | 0.100 | 264 (97.8%); 46 (8) | 0.074 |
| Yes | 18 (6.7%); 39.5 (9) | 6 (2.2%); 42 (9) | |||
| Bladder catheter | No | 250 (92.6%); 42 (9) | <0.001 | 252 (93.3%); 46 (7) | <0.001 |
| Yes | 20 (7.4%); 34 (17) | 18 (6.7%); 39 (11) | |||
| Stoma | No | 266 (98.5%); 41 (10) | - | 264 (97.8%); 46 (7) | 0.005 |
| Yes | 4 (1.5%); 16 (0) | 6 (2.2%); 22 (26) | |||
| Skin temperature probe | No | 183 (67.8%); 43 (9) | <0.001 | 208 (77.0%); 46 (7) | 0.010 |
| Yes | 87 (32.2%); 39 (11) | 62 (23.0%); 44 (8) | |||
| Phototherapy | No | 242 (89.6%); 42 (9) | 0.006 | 263 (97.4%); 46 (8) | 0.040 |
| Yes | 28 (10.4%); 36 (12) | 7 (2.6%); 41 (5) | |||
| Pulseoximeter sensor | Yes | 270 (100%); 41 (10) | - | 270 (100%); 46 (8) | - |
| Carbon-dioxide sensor | No | 228 (84.4%); 42 (8) | < 0.001 | 251 (93.0%); 46 (7) | 0.001 |
| Yes | 42 (15.6%); 35 (11) | 19 (7.0%); 41 (9) | |||
| PPS:NICU total score | Overall | 41 (10) | 46 (8) | <0.001 |
| Independent Variable | B | β | 95% CI | p Value | ||
|---|---|---|---|---|---|---|
| Birth weight | 0.003 | 0.284 | 0.001 | 0.005 | 0.002 | |
| Gestational age | Extremely preterm vs. term | −5.588 | −0.104 | −10.127 | −1.050 | 0.016 |
| Very preterm vs. term | −4.526 | −0.160 | −6.943 | −2.108 | <0.001 | |
| Late/Moderate preterm vs. term | −0.722 | −0.033 | −2.605 | 1.162 | 0.452 | |
| Peripheric venous catheter | 1.403 | 0.075 | −0.382 | 3.188 | 0.123 | |
| Central venous catheter | −0.384 | −0.016 | −3.150 | 2.382 | 0.785 | |
| Umbilical venous catheter | −0.851 | −0.035 | −3.698 | 1.997 | 0.557 | |
| Continuous infusions | 1.739 | 0.094 | −0.350 | 3.828 | 0.103 | |
| Arterial catheter | −2.864 | −0.042 | −9.338 | 3.609 | 0.385 | |
| Ventilatory support | Non-invasive ventilation vs. High-flow nasal cannula | −0.371 | −0.008 | −4.361 | 3.619 | 0.855 |
| Invasive ventilation vs. High-flow nasal cannula | −3.028 | −0.113 | −5.541 | −0.514 | 0.018 | |
| High-frequency oscillatory ventilation vs. High-flow nasal cannula | −2.251 | −0.042 | −7.307 | 2.804 | 0.382 | |
| Gastric tube | 0.967 | 0.051 | −0.927 | 2.861 | 0.316 | |
| Cerebral function monitoring | −2.302 | −0.052 | −5.857 | 1.253 | 0.204 | |
| Bladder catheter | −4.849 | −0.136 | −8.734 | −0.963 | 0.015 | |
| Stoma | −13.942 | −0.206 | −19.459 | −8.425 | <0.001 | |
| Skin temperature probe | 1.331 | 0.065 | −1.217 | 3.880 | 0.305 | |
| Phototherapy | −3.372 | −0.091 | −6.741 | −0.002 | 0.050 | |
| Carbon-dioxide sensor | −0.669 | −0.023 | −3.813 | 2.474 | 0.676 | |
| Parents’ gender | −0.364 | −0.199 | −0.524 | −0.205 | <0.001 | |
| Parents’ age | 0.037 | 0.030 | −0.061 | 0.135 | 0.458 | |
| First child | 1.361 | 0.074 | −0.190 | 2.911 | 0.085 | |
| Previous abortions | 2.055 | 0.093 | 0.259 | 3.850 | 0.025 | |
| Previous deceased children | 0.625 | 0.011 | −3.880 | 5.151 | 0.782 | |
| Type of delivery | Elective cesarean section vs. Natural birth | −2.838 | −0.140 | −4.660 | −1.016 | 0.002 |
| Emergency cesarean section vs. Natural birth | −3.031 | −0.142 | −4.937 | −1.125 | 0.002 | |
| Parents’ ethnicity | African vs. Caucasian | −8.579 | −0.234 | −11.598 | −5.560 | <0.001 |
| Hispanic/Latin American vs. Caucasian | 2.910 | 0.060 | −1.077 | 6.897 | 0.152 | |
| Twins | 2.112 | 0.075 | −0.631 | 4.855 | 0.131 | |
| Parents’ employment status | Unemployed vs. Employed | 0.836 | 0.038 | −1.086 | 2.759 | 0.393 |
| Student vs. Employed | 4.007 | 0.183 | 2.101 | 5.913 | <0.001 | |
| R2 | 0.263 | |||||
| Adjusted R2 | 0.229 | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Buccione, E.; Scarponcini Fornaro, D.; Pieragostino, D.; Natale, L.; D’Errico, A.; Chiavaroli, V.; Rasero, L.; Bambi, S.; Della Pelle, C.; Di Valerio, S. Parents’ Participation in Care during Neonatal Intensive Care Unit Stay in COVID-19 Era: An Observational Study. Nurs. Rep. 2024, 14, 1212-1223. https://doi.org/10.3390/nursrep14020092
Buccione E, Scarponcini Fornaro D, Pieragostino D, Natale L, D’Errico A, Chiavaroli V, Rasero L, Bambi S, Della Pelle C, Di Valerio S. Parents’ Participation in Care during Neonatal Intensive Care Unit Stay in COVID-19 Era: An Observational Study. Nursing Reports. 2024; 14(2):1212-1223. https://doi.org/10.3390/nursrep14020092
Chicago/Turabian StyleBuccione, Emanuele, Davide Scarponcini Fornaro, Damiana Pieragostino, Luca Natale, Adelaide D’Errico, Valentina Chiavaroli, Laura Rasero, Stefano Bambi, Carlo Della Pelle, and Susanna Di Valerio. 2024. "Parents’ Participation in Care during Neonatal Intensive Care Unit Stay in COVID-19 Era: An Observational Study" Nursing Reports 14, no. 2: 1212-1223. https://doi.org/10.3390/nursrep14020092
APA StyleBuccione, E., Scarponcini Fornaro, D., Pieragostino, D., Natale, L., D’Errico, A., Chiavaroli, V., Rasero, L., Bambi, S., Della Pelle, C., & Di Valerio, S. (2024). Parents’ Participation in Care during Neonatal Intensive Care Unit Stay in COVID-19 Era: An Observational Study. Nursing Reports, 14(2), 1212-1223. https://doi.org/10.3390/nursrep14020092








