Sleep Quality and Interoception Are Associated with Generalized Anxiety in Baccalaureate Nursing Students: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measures
2.2.1. Generalized Anxiety
2.2.2. Interoceptive Awareness
2.2.3. Sleep Quality
2.2.4. Physical Activity
2.2.5. Diet Quality
2.2.6. Perceived Health and Willingness to Change
2.2.7. Demographics and Anthropometrics
2.3. Statistical Analysis
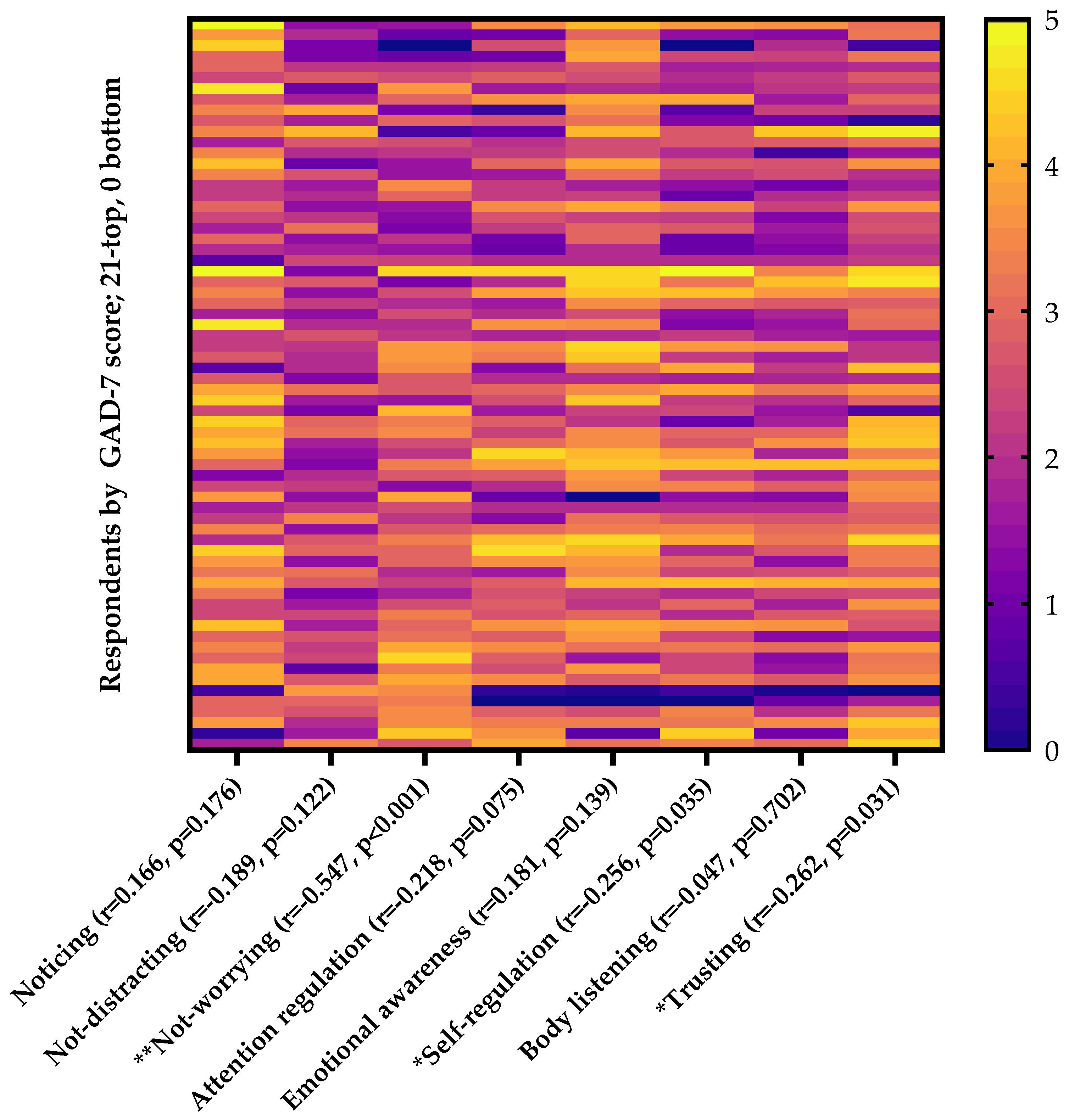
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public Involvement Statement
Guidelines and Standards Statement
Conflicts of Interest
References
- Anxiety Disorders. 2023. Available online: https://www.who.int/news-room/fact-sheets/detail/anxiety-disorders (accessed on 10 January 2024).
- Vos, T.; Allen, C.; Arora, M.; Barber, R.M.; Bhutta, Z.A.; Brown, A.; Carter, A.; Casey, D.C.; Charlson, F.J.; Chen, A.Z.; et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1545–1602. [Google Scholar] [CrossRef] [PubMed]
- American Psychological Association. Stress in America™ 2023 A National Mental Health Crisis. 2023. Available online: https://www.apa.org/news/press/releases/stress/2023/november-2023-topline-data.pdf (accessed on 10 January 2024).
- Center for Collegiate Mental Health. Center for Collegiate Mental Health 2022 Annual Report. 2023. Available online: https://ccmh.psu.edu/assets/docs/2022%20Annual%20Report.pdf (accessed on 10 January 2024).
- Barbayannis, G.; Bandari, M.; Zheng, X.; Baquerizo, H.; Pecor, K.W.; Ming, X. Academic stress and mental well-being in college students: Correlations, affected groups, and COVID-19. Front. Psychol. 2022, 13, 886344. [Google Scholar] [CrossRef] [PubMed]
- Kris-Etherton, P.M.; Petersen, K.S.; Hibbeln, J.R.; Hurley, D.; Kolick, V.; Peoples, S.; Rodriguez, N.; Woodward-Lopez, G. Nutrition and behavioral health disorders: Depression and anxiety. Nutr. Rev. 2021, 79, 247–260. [Google Scholar] [CrossRef] [PubMed]
- Alzayyat, A.; Al-Gamal, E. A review of the literature regarding stress among nursing students during their clinical education. Int. Nurs. Rev. 2014, 61, 406–415. [Google Scholar] [CrossRef] [PubMed]
- Pulido-Martos, M.; Augusto-Landa, J.M.; Lopez-Zafra, E. Sources of stress in nursing students: A systematic review of quantitative studies. Int. Nurs. Rev. 2012, 59, 15–25. [Google Scholar] [CrossRef]
- Ahmed, F.A.; Alrashidi, N.; Mohamed, R.A.; Asiri, A.; Al Ali, A.; Aly, K.H.; Nouh, W.G.; Demerdash, N.A.; Marzouk, S.A.; Omar, A.M.; et al. Satisfaction and anxiety level during clinical training among nursing students. BMC Nurs. 2023, 22, 187. [Google Scholar] [CrossRef] [PubMed]
- Karaman, M.A.; Lerma, E.; Vela, J.C.; Watson, J.C. Predictors of academic stress among college students. J. Coll. Couns. 2019, 22, 41–55. [Google Scholar] [CrossRef]
- Martínez-Vázquez, S.; Martínez-Galiano, J.M.; Peinado-Molina, R.A.; Hernández-Martínez, A. Magnitude of general anxiety disorder among nursing students and its associated factors. Health Sci. Rep. 2023, 6, e1405. [Google Scholar] [CrossRef] [PubMed]
- Casuso-Holgado, M.J.; Moreno-Morales, N.; Labajos-Manzanares, M.T.; Montero-Bancalero, F.J. The association between perceived health symptoms and academic stress in Spanish higher education students. Eur. J. Educ. Psychol. 2019, 12, 109–123. [Google Scholar] [CrossRef]
- Hill, D.; Conner, M.; Clancy, F.; Moss, R.; Wilding, S.; Bristow, M.; O’connor, D.B. Stress and eating behaviours in healthy adults: A systematic review and meta-analysis. Health Psychol. Rev. 2022, 16, 280–304. [Google Scholar] [CrossRef]
- Choi, J. Impact of stress levels on eating behaviors among college students. Nutrients 2020, 12, 1241. [Google Scholar] [CrossRef]
- Ling, J.; Zahry, N.R. Relationships among perceived stress, emotional eating, and dietary intake in college students: Eating self-regulation as a mediator. Appetite 2021, 163, 105215. [Google Scholar] [CrossRef] [PubMed]
- Bartschi, J.G.; Greenwood, L.-M. Food addiction as a mediator between depressive symptom severity and body mass index. Appetite 2023, 190, 107008. [Google Scholar] [CrossRef]
- Lipert, A.; Kozłowski, R.; Timler, D.; Marczak, M.; Musiał, K.; Rasmus, P.; Kamecka, K.; Jegier, A. Physical Activity as a Predictor of the Level of Stress and Quality of Sleep during COVID-19 Lockdown. Int. J. Environ. Res. Public Health 2021, 18, 5811. [Google Scholar] [CrossRef]
- Ye, J.; Jia, X.; Zhang, J.; Guo, K. Effect of physical exercise on sleep quality of college students: Chain intermediary effect of mindfulness and ruminative thinking. Front. Psychol. 2022, 13, 987537. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed]
- Johnson, S.U.; Ulvenes, P.G.; Øktedalen, T.; Hoffart, A. Psychometric properties of the general anxiety disorder 7-item (GAD-7) scale in a heterogeneous psychiatric sample. Front. Psychol. 2019, 10, 449461. [Google Scholar] [CrossRef]
- Mehling, W.E.; Acree, M.; Stewart, A.; Silas, J.; Jones, A. The multidimensional assessment of interoceptive awareness, version 2 (MAIA-2). PLoS ONE 2018, 13, e0208034. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F., III; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Rubenstein, J.H.; Morgenstern, H.; Kellenberg, J.; Kalish, T.; Donovan, J.; Inadomi, J.; McConnell, D.; Stojanovska, J.; Schoenfeld, P. Validation of a new physical activity questionnaire for a sedentary population. Dig. Dis. Sci. 2011, 56, 2678–2687. [Google Scholar] [CrossRef]
- Jetté, M.; Sidney, K.; Blümchen, G. Metabolic equivalents (METS) in exercise testing, exercise prescription, and evaluation of functional capacity. Clin. Cardiol. 1990, 13, 555–565. [Google Scholar] [CrossRef] [PubMed]
- Shingleton, J.; Buttrey, S.; Orendorff, F.; Wright, E. Global Assessment Tool (GAT) Trend Analysis; Army TRADOC Analysis Center: Austin, TX, USA, 2016. [Google Scholar]
- Purvis, D.L.; Lentino, C.V.; Jackson, T.K.; Murphy, K.J.; Deuster, P.A. Nutrition as a component of the performance triad: How healthy eating behaviors contribute to soldier performance and military readiness. US Army Med. Dep. J. 2013. Available online: https://pubmed.ncbi.nlm.nih.gov/24146244/ (accessed on 10 January 2024).
- Colby, S.; Zhou, W.; Allison, C.; Mathews, A.E.; Olfert, M.D.; Morrell, J.S.; Byrd-Bredbenner, C.; Greene, G.; Brown, O.; Kattelmann, K.; et al. Development and validation of the short healthy eating index survey with a college population to assess dietary quality and intake. Nutrients 2020, 12, 2611. [Google Scholar] [CrossRef] [PubMed]
- Ware, J., Jr.; Kosinski, M.; Keller, S.D. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Med. Care 1996, 34, 220–233. [Google Scholar] [CrossRef] [PubMed]
- Allison, K.R.; Dwyer, J.J.M.; Makin, S. Perceived Barriers to Physical Activity among High School Students. Prev. Med. 1999, 28, 608–615. [Google Scholar] [CrossRef] [PubMed]
- Saha, S.; Okafor, H.; Biediger-Friedman, L.; Behnke, A. Association between diet and symptoms of anxiety and depression in college students: A systematic review. J. Am. Coll. Health 2023, 71, 1270–1280. [Google Scholar] [CrossRef]
- Huberty, J.; Green, J.; Glissmann, C.; Larkey, L.; Puzia, M.; Lee, C. Efficacy of the mindfulness meditation mobile app “calm” to reduce stress among college students: Randomized controlled trial. JMIR mHealth uHealth 2019, 7, e14273. [Google Scholar] [CrossRef] [PubMed]
- Ghrouz, A.K.; Noohu, M.M.; Manzar, D.; Spence, D.W.; BaHammam, A.S.; Pandi-Perumal, S.R. Physical activity and sleep quality in relation to mental health among college students. Sleep Breath. 2019, 23, 627–634. [Google Scholar] [CrossRef] [PubMed]
- Du, C.; Zan, M.C.H.; Cho, M.J.; Fenton, J.I.; Hsiao, P.Y.; Hsiao, R.; Keaver, L.; Lai, C.-C.; Lee, H.; Ludy, M.-J.; et al. Increased resilience weakens the relationship between perceived stress and anxiety on sleep quality: A moderated mediation analysis of higher education students from 7 countries. Clocks Sleep 2020, 2, 334–353. [Google Scholar] [CrossRef] [PubMed]
- Price, C.J.; Hooven, C. Interoceptive Awareness Skills for Emotion Regulation: Theory and Approach of Mindful Awareness in Body-Oriented Therapy (MABT). Front. Psychol. 2018, 9, 798. [Google Scholar] [CrossRef]
- Fagioli, S.; Pallini, S.; Mastandrea, S.; Barcaccia, B. Effectiveness of a Brief Online Mindfulness-Based Intervention for University Students. Mindfulness 2023, 14, 1234–1245. [Google Scholar] [CrossRef]
- McMahon, S. Mindful Success: A Correlational Study on Mindfulness, Interoceptive Awareness, Thought Suppression, Perceived Stress, and Academic Success; California Institute of Integral Studies: San Francisco, CA, USA, 2021. [Google Scholar]
- Kabir, R.S. Interoceptive attention tendencies predict trait anxiety in undergraduate students and hospital nurses participating in stress management programs. Bull. Grad. Sch. Educ. Hiroshima Univ. 2019, 68, 111–120. [Google Scholar]
- Toqan, D.; Ayed, A.; Khalaf, I.A. Effect of progressive muscle relaxation exercise on anxiety among nursing students prior to critical care clinical training. J. Public Health Res. 2023, 12, 22799036231181668. [Google Scholar] [CrossRef] [PubMed]
- Almarcha, M.; González, I.; Balagué, N.; Javierre, C. Prescribing or co-designing exercise in healthy adults? Effects on mental health and interoceptive awareness. Front. Behav. Neurosci. 2022, 16, 944193. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Liu, J.; An, M.; Gu, H. The effect of time management training on time management and anxiety among nursing undergraduates. Psychol. Health Med. 2021, 26, 1073–1078. [Google Scholar] [CrossRef] [PubMed]
- Aloufi, M.A.; Jarden, R.J.; Gerdtz, M.F.; Kapp, S. Reducing stress, anxiety and depression in undergraduate nursing students: Systematic review. Nurse Educ. Today 2021, 102, 104877. [Google Scholar] [CrossRef] [PubMed]
- Ortega, R.H.; Pascual, J.L.G.; Araque, A.M.F. Impact of an intervention program with reinforcement on nursing students’ stress and anxiety levels in their clinical practices. Nurse Educ. Pract. 2021, 55, 103179. [Google Scholar] [CrossRef]
- Heeter, C.; Lehto, R.; Allbritton, M.; Day, T.; Wiseman, M. Effects of a Technology-Assisted Meditation Program on Healthcare Providers’ Interoceptive Awareness, Compassion Fatigue, and Burnout. J. Hosp. Palliat. Nurs. 2017, 19, 314–322. [Google Scholar] [CrossRef]

| N (%) | |
|---|---|
| Female gender | 64 (94.1%) |
| White race | 66 (97.1%) |
| Hispanic ethnicity | 2 (2.9%) |
| Age; median (range) | 21 (19–26) |
| Earned associate degree | 2 (2.9%) |
| Prior military service | 2 (2.9%) |
| Lifestyle factors | |
| MET hours/week; median (range) | 43 (24–78) |
| Diet Quality (HEI Score); median (range) | 60 (51–75) |
| Sleep Score (PSQI Global Score); median (range) | 7 (4–10) |
| BMI; mean (SD) | 23.2 (3.8) |
| GAD-7 | |
| Minimal anxiety | 25 (36.8%) |
| Mild anxiety | 16 (23.5%) |
| Moderate anxiety | 17 (25%) |
| Severe anxiety | 10 (14.7%) |
| General health status | |
| Fair or good | 31 (45.6%) |
| Very good or excellent | 37 (54.4%) |
| Willing to change | 67 (98.5%) |
| Barriers to change; median (range) | 4 (1–8) |
| Model | Dependent Variable: GAD-7 | Beta | t | Sig. |
|---|---|---|---|---|
| (Constant) | 3.135 | 0.003 | ||
| Sleep quality (PSQI) | 0.413 | 4.296 | <0.001 | |
| Perceived health | −0.159 | −1.715 | 0.091 | |
| Number of barriers to behavior change | 0.128 | 1.450 | 0.152 | |
| MAIA Not-Worrying | −0.361 | −3.868 | <0.001 | |
| MAIA Trusting | −0.045 | −0.477 | 0.635 | |
| 2 | (Constant) | 3.295 | <0.001 | |
| Sleep quality (PSQI) | 0.425 | 4.602 | <0.001 | |
| Perceived health | −0.173 | −1.954 | 0.055 | |
| Number of barriers to behavior change | 0.133 | 1.526 | 0.132 | |
| MAIA Not-Worrying | −0.357 | −3.865 | <0.001 | |
| 3 | (Constant) | 4.679 | <0.001 | |
| Sleep quality (PSQI) | 0.446 | 4.823 | <0.001 | |
| Perceived health | −0.168 | −1.887 | 0.064 | |
| MAIA Not-Worrying | −0.366 | −3.93 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Robinson, L.A.; Short, P.R.; Frugé, A.D. Sleep Quality and Interoception Are Associated with Generalized Anxiety in Baccalaureate Nursing Students: A Cross-Sectional Study. Nurs. Rep. 2024, 14, 1184-1192. https://doi.org/10.3390/nursrep14020090
Robinson LA, Short PR, Frugé AD. Sleep Quality and Interoception Are Associated with Generalized Anxiety in Baccalaureate Nursing Students: A Cross-Sectional Study. Nursing Reports. 2024; 14(2):1184-1192. https://doi.org/10.3390/nursrep14020090
Chicago/Turabian StyleRobinson, Laura A., Pamela R. Short, and Andrew D. Frugé. 2024. "Sleep Quality and Interoception Are Associated with Generalized Anxiety in Baccalaureate Nursing Students: A Cross-Sectional Study" Nursing Reports 14, no. 2: 1184-1192. https://doi.org/10.3390/nursrep14020090
APA StyleRobinson, L. A., Short, P. R., & Frugé, A. D. (2024). Sleep Quality and Interoception Are Associated with Generalized Anxiety in Baccalaureate Nursing Students: A Cross-Sectional Study. Nursing Reports, 14(2), 1184-1192. https://doi.org/10.3390/nursrep14020090









